Abstract
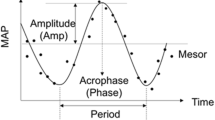
This study compares the effect of three diets on the circadian rhythm of blood pressure (BP). Hypertension and abnormal BP variability (BPV) are major risk factors leading to morbidity and mortality from cardiovascular disease. When detected early, a dietary approach may be preferred to medication. Data stemming from ambulatory BP monitoring (ABPM) from the Dietary Approaches to Stop Hypertension (DASH) study were re-analyzed from a chronobiologic perspective. Compared to the control diet (N = 112) that had no effect on BP (from 131.2/83.5 to 131.0/83.6 mmHg), both the Fruit and Vegetable (FV; N = 113) diet and the DASH (N = 113) diet were associated with a decrease in BP (FV: from 132.6/84.4 to 129.0/82.1 mmHg; DASH: from 131.9/83.6 to 127.2/80.9 mmHg). The decrease in BP was found to be circadian stage-dependent, and to differ between men and women. Nighttime BP was decreased to a larger extent with the DASH than with the FV diet, a difference observed in women but not in men. Study participants who had a higher BP during the reference stage were more likely to decrease their BP to a larger extent after the 8-week dietary intervention. The FV and DASH diets had different effects on BPV. In view of the relatively large day-to-day variability in BP in both normotensive and hypertensive people, it is recommended to monitor BP around the clock for longer than 24 h, and to individualize the optimization of dietary or other intervention.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 digital issues and online access to articles
$119.00 per year
only $9.92 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
References
Roth GA, Johnson C, Abajobir A, Abd-Allah F, Abera SF, Abyu G, et al. Global, regional, and national burden of cardiovascular diseases for 10 causes, 1990 to 2015. J Am College Cardiol. 2017; 70:1–25. https://doi.org/10.1016/j.jacc.2017.04.052.
Yu E, Rimm E, Qi L, Rexrode K, Albert CM, Sun Q, et al. Diet, lifestyle, biomarkers, genetic factors, and risk of cardiovascular disease in the Nurses’ Health Studies. Am J Public Health. 2016;106:1616–23.
Sacks FM, Obarzanek E, Windhauser MM, Svetkey LP, Vollmer WM, McCullough M, et al. Rationale and design of the Dietary Approaches to Stop Hypertension Trial (DASH): a multicenter controlled-feeding study of dietary patterns to lower blood pressure. Ann Epidemiol. 1995;5:108–18.
Appel LJ, Moore TJ, Obarzanek E, Vollmer WM, Svetkey LP, Sacks FM, et al. Clinical trial of the effects of dietary patterns on blood pressure. N. Engl J Med. 1997;336:1117–24.
Moore TJ, Vollmer WM, Appel LJ, Sacks FM, Svetkey LP, Vogt TM, et al. Effect of dietary patterns on ambulatory blood pressure. Results from the Dietary Approaches to Stop Hypertension (DASH) trial. Hypertension. 1999;34:472–7.
Cornelissen G. Cosinor-based rhythmometry. Theor Biol Med Modell. 2014;11:16. https://doi.org/10.1186/1742-4682-11-16.
Halberg F, Powell D, Otsuka K, Watanabe Y, Beaty LA, Rosch P, et al. Diagnosing vascular variability anomalies, not only MESOR-hypertension. Am J Physiol Heart Circ Physiol. 2013;305:H279–94.
Bingham C, Arbogast B, Cornelissen Guillaume G, Lee JK, Halberg F. Inferential statistical methods for estimating and comparing cosinor parameters. Chronobiologia. 1982;9:397–439.
Vasan RS, Larson MG, Leip EP, Evans JC, O’Donnell CJ, Kannel WB, et al. Impact of high-normal blood pressure on the risk of cardiovascular disease. N. Engl J Med. 2001;345:1291–7.
Márquez-Celedonio FG, Téxon-Fernández O, Chávez-Negrete A, Hernández-López S, Marín-Rendón S, Berlín-Lascurain S. Clinical effect of lifestyle modification on cardiovascular risk in prehypertensives: PREHIPER I study. Rev Esp Cardiol. 2009;62:86–90.
Anand SS, Hawkes C, de Souza RJ, Mente A, Dehghan M, Nugent R, et al. Food consumption and its impact on cardiovascular disease: importance of solutions focused on the globalized food system: a report from the workshop convened by the World Heart Federation. J Am Coll Cardiol. 2015;66:1590–614.
Otsuka K, Watanabe H, Cornelissen G, Shinoda M, Uezono K, Kawasaki T, et al. Gender, age and circadian blood pressure variation of apparently healthy rural vs. metropolitan Japanese. Chronobiologia. 1990;17:253–65.
Maas AH, Appelman YE. Gender differences in coronary heart disease. Neth Heart J. 2010;18:598–602.
Ingelsson E, Björklund-Bodegård K, Lind L, Arnlöv J, Sundström J. Diurnal blood pressure pattern and risk of congestive heart failure. JAMA. 2006;295:2859–66.
Yano Y, Kario K. Nocturnal blood pressure and cardiovascular disease: a review of recent advances. Hypertens Res. 2012;35:695–701.
Otsuka K, Cornelissen G, Halberg F. Predictive value of blood pressure dipping and swinging with regard to vascular disease risk. Clin Drug Investig. 1996;11:20–31.
Otsuka K, Cornelissen G, Halberg F, Oehlert G. Excessive circadian amplitude of blood pressure increases risk of ischemic stroke and nephropathy. J Med Eng Technol. 1997;21:23–30.
Watanabe Y, Halberg F, Otsuka K, Cornelissen G. Toward a personalized chronotherapy of high blood pressure and a circadian overswing. Clin Exp Hypertens. 2013;35:257–66.
Acknowledgements
The authors thank Professor Lloyd J. Edwards and the NIH for access to the data.
Funding
Halberg Chronobiology Fund (GC).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Saka, F., Cornelissen, G. Chronobiologic assessment of the effect of the DASH diet on blood pressure. J Hum Hypertens 35, 678–684 (2021). https://doi.org/10.1038/s41371-020-00408-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41371-020-00408-0