Abstract
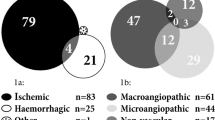
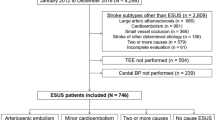
We aimed to evaluate brachial and central blood pressure (BP) estimates and biomarker levels in lacunar ischemic stroke (IS) and other IS subtypes (nonlacunar stroke). We studied 70 functionally independent subjects consecutively admitted to our institution after a first episode of IS. Subjects with previous heart failure were excluded. BP was measured at admission and during the subacute phase of stroke (5–7 days after stroke onset). Aortic pulse wave velocity (aPWV), augmentation index (AIx), and 24 h brachial and central BP (24h-ABPM) were measured by means of a Mobil-O-Graph device during the subacute phase of stroke. Determination of N-terminal prohormone of brain natriuretic peptide (NT-proBNP), urinary albumin excretion, and echocardiography were performed in all subjects. After adjusting for age and clinical severity, lacunar IS had significantly higher levels of BP at admission (systolic BP 173 ± 37 vs 153 ± 28 mmHg, p = 0.006; diastolic BP: 97 ± 21 vs 86 ± 16 mmHg, p = 0.035) and during the subacute phase of stroke (systolic BP 152 ± 23 vs 134 ± 19 mmHg, p = 0.001; diastolic BP: 84 ± 14 and 77 ± 10 mmHg, respectively; p = 0.038) but lower NT-proBNP levels (median: 36,277 vs 274 pg/mL, p = 0.009) than nonlacunar IS. Central BP, aPWV, and AIx were not different between lacunar and nonlacunar IS, neither the rate of target organ damage. In conclusion, patients with a first episode of lacunar IS have higher BP values at admission and during the subacute phase of stroke and lower levels of NT-proBNP, suggesting a closer relationship with hypertension of this IS subtype.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 digital issues and online access to articles
$119.00 per year
only $9.92 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Georgianou E, Georgianos PI, Petidis K, Athyros VG, Serafidis PA, Karagiannis A. Antihypertensive therapy in acute ischemic stroke: where do we stand? J Hum Hypertens. 2018;32:799–807.
Armario P, Martin-Baranera M, Ceresuela LM, Hernández-del-Rey R, Iribarnegaray E, Pintado S, et al. Blood pressure in the initial phase of acute stroke: evolution and its role as an independent prognosis factors at discharge and after 3 months of follow-up. Blood Press. 2008;17:284–90.
Powers WJ, Rabinstein AA, Ackerson T, Adeoye OM, Bambakidis NC, Becker K, et al. on behalf of the American Heart Association Stroke Council. 2018 Guidelines for the early management of patients with acute ischemis stroke. A guideline for Healthcare Professionals from the American Heart Association/American Stroke Association. Stroke. 2018;49:e46–e110. https://doi.org/10.1161/STR.0000000000000158.
Vemmos KN, Spengos K, Tsivgoulis G, Zakapoulus N, Manios E, Kotsis V, et al. Factors influencing acute blood pressure values in stroke subtypes. J Hum Hypertens. 2004;28:253–9.
Altmann M, Thommessen B, Ronning OM, Reichbach AS, Fure B. Blood pressure differences between patients with lacunar and non lacunar infarcts. Brain Behav. https://doi.org/10.1002/brb3.353.
Wardlaw JM, Doubal F, Armitage P, Chappell F, Carpenter T, Muñoz Maniega S, et al. Lacunar stroke is associated with diffuse blood-brain barrier dysfunction. Ann Neurol. 2009;65:194–202.
Wardlaw JM. What causes lacunar stroke? J Neurol Neurosurg Psychiatry. 2005;76:617–9.
Sico JJ, Phipps MS, Yaggi HK, Burrus N, Ferguson J, McClain V, et al. Ambulatory blood pressure monitoring among patients with cerebrovascular disease. Blood Press Monit. 2011;16:211–7.
Castilla-Guerra L, Fernández-Moreno MC. Ambulatory blood pressure monitoring in stroke survivors: do we really control our patients? Eur J Intern Med. 2009;20:760–3.
Castilla-Guerra L, Fernández-Moreno MC. Chronic management of hypertension after stroke: the role of ambulatory blood pressure monitoring. J Stroke. 2016;18:31–37.
Jain S, Namboodri KKN, Kumari S, Prabhakar S. Loss of circadian rhythm of blood pressure following acute stroke. BMC Neurol. 2004;4:1–6.
Kollias A, Lagou S, Zeniodi ME, Boubouchairopoulus N, Stergiou GS. Association of central versus brachial blood pressure with target organ damage. Syst Rev Meta-Anal Hypertens. 2016;67:183–90.
Llombart V, Antolin-Fontes A, Bustamante A, Giralt D, Rost NS, Furie K, et al. B-type natriuretic peptides help in cardioembolic stroke diagnosis. Pool data meta-Anal Stroke. 2015;46:1187–95.
Greisenegger S, Segal HC, Burges AI, Poole DL, Mehta Z, Rotwell PM. Biomarkers and mortality after transient ischemic attack and minor ischemicstroke. Population-based study. Stroke. 2015;46:659–66.
Kawase S, Kowa H, Suto Y, Fukuda H, Kusumi M, Nakayasu H, et al. Plama brain natriuretic peptide is a marker of prognostic functional outcome in non-cardioembolic infarction. J Stroke Cererbrovasc Dis. 2015;24:2285–90.
Gao M, Ma G, Ding W, Mu L. Copeptina and NT-proBNP as prognostic markers for recurrent ischemic cerebrovascular events in ischemic stroke patients. J Am Coll Cardiol. 2016;68:2710–1.
O’Brien E, Parati G, Stergiou G, Asmar R, Beilin L, Bilo G, et al. European Society of Hypertension Working Group on blood pressure monitoring. European Society of Hypertension position paper on ambulatory blood pressure monitoring. J Hypertens. 2013;31:1731–68.
Parati G, Stergiou G, O’Brien E, Asmar R, Beilin L, Bilo G, et al. European Society of Hypertension practice guidelines for ambulatory blood pressure monitoring. J Hypertens. 2014;32:1359–66.
Hametner B, Wassertheurer S, Kropf J, Mayer C, Eber B, Weber T. Oscillometrtic estimation of aortic pulse wave velocity: comparison with intra-aortic catheter measurements. Blood Press Monit. 2013;18:173–6.
Weber T, Wassertheurer S, Hametner B, Parragh S, Eber B. Noninvasive methods to assess pulse wave velocity. J Hypertens. 2015;33:1023–31.
Blanch P, Armario P, Oliveras A, Fernández-Llama P, Vázquez S, Calero F, et al. Association of left ventricular hypertrophy or diastolic dysfunction with 24-hour central and peripheral blood pressure. Am J Hypertens. 2018;31:1293–9.
Marwick TH, Gillebert TC, Aurigemma G, Chirinos J, Derumeaux G, Galderisi M, et al. Recommendations on the use of echocardiography in adult hypertension: a report from the European Association of cardiovascular imaging (EACVI) and the American Society of Echocardiography (ASE). J Am Soc Echocardiogr. 2015;28:727–54.
Devereux RB, Alonso DR, Lutas EM, Gottlieb CJ, Campo E, Sachs I, et al. Echocardiographic assessment of left ventricular hypertrophy: comparison to necropsy findings. Am J Cardiol. 1986;57:450–8.
Fernández-Llama P, Pareja J, Yun S, Vázquez S, Oliveras A, Armario P, et al. Cuff-based oscillometric central and brachial blood pressures obtained through ABPM are similarly associated with renal organ damage in arterial hypertension. Kidney Blood Press Res. 2017;42:1068–77.
Lau KK, Li L, Simoni M, Mehta Z, Küker W, Rothwell PM. for the Oxford Vascular Study. Long-term premorbid blood pressure and cerebral small vessel disease burden on imaging in transient ischemic attack and ischemic stroke. Population-based study. Stroke. 2018;49:2053–60.
Klarenbeek P, Van Oostenbrugge J, Rouhl RPW, Knottnerus ILH, Staals J. Ambulatory blood pressure in patients with lacunar stroke. Association with total MRI burden of cerebral small vessel disease. Stroke. 2013;44:2995–9.
Yan B, Peng L, Dong Q, Zheng F, Yang P, Sun L, et al. Reverse-dipper pattern of blood pressure may predict lacunar infarction in patients with essential hypertension. Eur J Neurol. 2015;22:1022–5.
Zhang WW, Cadilac DA, Churilov L, Donnan GA, O’Callaghan C, Dewey HM. Does abnormal circadian blood pressure pattern really matter in patients with transient ischemic attack or minor stroke? Stroke. 2014;45:865–7.
Yamamoto Y, Akiguchi I, Oiwa K, Hayashi M, Kimura J. Adverse effect of night-time blood pressure on the outcome of lacunar infarct patients. Stroke. 1998;29:570–6.
Yamamoto Y, Akiguchi I, Oiwa K, Hayashi M, Kasai T, Ozasa K. Twenty-four-hour blood pressure and MRI as predictive factors for different outcomes in patients with lacunar infarct. Stroke. 2002;33:297–305.
Weber T, Wassertheurer S, Schmidt-Truckäss A, Rodilla E, Ablaser C, Jankowski P, et al. Relationship between 24.hour ambulatory central systolic blood pressure and left ventricular mass. A prospective multicenter study. Hypertension. 2017;70:1157–64.
Henskens LHG, Kroon AA, Oostenbrugge Van, HBM Gronenschild, MMJJ Fuss-Lejeune, Hofman PAM, et al. Increased aortic pulse wave velocity is associated with silent cerebral small-vessel disease in hypertensive patients. Hypertension. 2008;52:1120–6.
Gasecki D, Kwarciany M, Kowalczyk K, Rojerj A, Nowicki T, Skrzypek-Czerco M, et al. Aortic stiffness is an independent biomarker of subclinical brain damage in acute ischemic stroke. J Hypertens. 2015;33. https://doi.org/10.1097/01.hjh.0000467502.75589.a8.
Byun DS, Han SW, Park JH, Kim JY, Baik JS, Park JH. Relationship between augmentation index and acute ischemic stroke subtype. J Clin Neuroscience. 2014;21:1220–4.
Di Castelnuovo A, Veronesi G, Constanzo S, Zeller T, Schnabel RB, de Curtis A, et al. On behalf of the BiomarCARE Investigators. Stroke. 2019. https://doi.org/10.1161/STROKEAHA.118.023218.
Heuschmann PU, Kircher J, Nowe T, Dittich R, Reiner Z, Cifkova R, et al. Control of main risk factors after stroke across Europe: data from the stroke-specific module of the EUROASPIRE III survey. Eur J Prev Cardiol. 2015;22:1354–62.
Kohok DD, Sico JJ, Baye F, Myers L, Coffing J, Kamalesh M, et al. Post-stroke hypertension control and receipt of healthy care services among veterans. J Clin Hypertens. 2018;20:382–87.
Acknowledgements
We thank Kathryn O’Connor for reviewing the manuscript. The current study was supported by a grant of the Catalan Society of Hypertension.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Gómez-Choco, M., García-Sánchez, S.M., Font, M.À. et al. Biomarkers levels and brachial and central blood pressure during the subacute phase of lacunar stroke and other ischemic stroke subtypes. J Hum Hypertens 34, 404–410 (2020). https://doi.org/10.1038/s41371-019-0233-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41371-019-0233-8