Abstract
Background
Ambient air pollution exposure increases the incidence and severity of pediatric asthma. Despite this, we lack effective therapies to protect patients from the impact of ambient air pollution exposure. A roadblock is the inability to identify patients that are affected by air pollution.
Objective
To examine the association between AAP sensitivity determined by individual exposure prior to asthma exacerbations and the severity of asthma in pediatric patients.
Methods
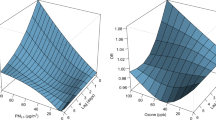
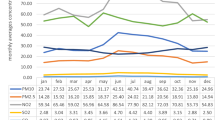
We assess the association between spikes in ambient air pollution and asthma exacerbations. Patients were considered sensitive to a specific pollutant if they experienced an asthma exacerbation immediately following a spike in the concentration of that pollutant. Cut off values for these spikes were determined as two standard deviations above the mean concentration two weeks prior and two weeks post the days leading up to an asthma exacerbation.
Results
We included 8129 pediatric patients with over 34,346 associated asthma exacerbations. In a multinomial log-linear logistic regression model comparing patients with mild asthma to patients with moderate or severe asthma, sensitivity to Ozone, SO2, PM2.5 and PM10 was significantly associated to severe as opposed to mild asthma (OR 1.39 with CI 1.08–1.78, 1.58 with CI 1.12–2.23, 1.37 with CI 1.07–1.76, and 1.63 with CI 1.12–2.37 respectively). Furthermore, moderate as opposed to mild asthma was significantly associated with sensitivity to SO2 and PM2.5 (OR 1.24 with CI 1.06–1.44 and 1.26 with CI 1.12–1.43, respectively).
Impact Statement
-
There is a subpopulation of pediatric asthma patients that experience asthma exacerbations just following spikes in ambient air pollution. This subgroup of patients has more severe asthma despite correction for significant confounders. The presented work is the first to reveal the clinically significant impact of variation in ambient air pollution sensitivity in pediatric asthma, highlighting the importance of accounting for variable sensitivity in the study of the effects of ambient air pollution exposure on pediatric asthma.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 6 print issues and online access
$259.00 per year
only $43.17 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
Data availability
The data that support the findings of this study are available from the corresponding author, JK, upon reasonable request.
References
Guarnieri M, Balmes JR. Outdoor air pollution and asthma. Lancet. 2014;383:1581–92.
Tiotiu AI, Novakova P, Nedeva D, Chong-Neto HJ, Novakova S, Steiropoulos P, et al. Impact of Air Pollution on Asthma Outcomes. Int J Environ Res Public Health. 2020;17:6212.
Perez L, Declercq C, Iñiguez C, Aguilera I, Badaloni C, Ballester F, et al. Chronic burden of near-roadway traffic pollution in 10 European cities (APHEKOM network). Eur Respiratory J. 2013;42:594–605.
Garcia E, Berhane KT, Islam T, McConnell R, Urman R, Chen Z, et al. Association of Changes in Air Quality With Incident Asthma in Children in California, 1993-2014. JAMA 2019;321:1906.
Guerriero C, Chatzidiakou L, Cairns J, Mumovic D. The economic benefits of reducing the levels of nitrogen dioxide (NO2) near primary schools: The case of London. J Environ Manag. 2016;181:615–22.
Cromar KR, Gladson LA, Ghazipura M, Ewart G. Estimated Excess Morbidity and Mortality Associated with Air Pollution above American Thoracic Society–recommended Standards, 2013–2015. American Thoracic Society and Marron Institute Report. Ann Am Thorac Soc. 2018;15:542–51.
Wendt JK, Symanski E, Stock TH, Chan W, Du XL. Association of short-term increases in ambient air pollution and timing of initial asthma diagnosis among medicaid-enrolled children in a metropolitan area. Environ Res. 2014;131:50–8.
Contreras M, Keys K, Magana J, Goddard P, Risse-Adams O, Zeiger AM, et al. Native American Ancestry and Air Pollution Interact to Impact Bronchodilator Response in Puerto Rican Children with Asthma. Ethnicity Dis. 2021;31:77–88.
Rancière F, Bougas N, Viola M, Momas I. Early Exposure to Traffic-Related Air Pollution, Respiratory Symptoms at 4 Years of Age, and Potential Effect Modification by Parental Allergy, Stressful Family Events, and Sex: A Prospective Follow-up Study of the PARIS Birth Cohort. Environ Health Perspect. 2017;125:737–45.
Air Quality System Data Mart [internet database] [Internet]. US Environmental Protection Agency. [cited 02, 2022.]. Available from: https://www.epa.gov/outdoor-air-quality-data.
Gottesman O, Kuivaniemi H, Tromp G, Faucett WA, Li R, Manolio TA, et al. The Electronic Medical Records and Genomics (eMERGE) Network: past, present, and future. Genet Med. 2013;15:761-71.
Lyam Vazquez, Connolly. J. Chop. Asthma. PheKB; 2013 [Available from: https://phekb.org/phenotype/146.
Rozzi GC. zipcodeR: Advancing the analysis of spatial data at the ZIP code level in R. Softw Impacts. 2021;9:100099.
Agency USEP. [Available from: https://aqs.epa.gov/aqsweb/airdata/download_files.html#AQI.
Kelchtermans J, Mentch F, Hakonarson H, editors. Facilitating Case-Crossover Studies Using Environmental Protection Agency 2022: American Thoracic Society.
2021-2022 Air Monitoring Network Plan. In: City of Philadelphia DoPH, Air Management Services, editor. 2021.
Peng RD, Dominici F, Pastor-Barriuso R, Zeger SL, Samet JM. Seasonal analyses of air pollution and mortality in 100 US cities. Am J Epidemiol. 2005;161:585–94.
Yamazaki S, Shima M, Yoda Y, Oka K, Kurosaka F, Shimizu S, et al. Exposure to air pollution and meteorological factors associated with children’s primary care visits at night due to asthma attack: case-crossover design for 3-year pooled patients. BMJ Open. 2015;5:e005736-e.
Yu-Ni H, Fu-Jen C, Ming-Ta T, Chih-Min T, Po-Chun C, Chi-Yung C. Fine particulate matter constituents associated with emergency room visits for pediatric asthma: a time-stratified case–crossover study in an urban area. 2021.
Zhang Z. Model building strategy for logistic regression: purposeful selection. Ann Transl Med 2016;4:111-.
Choi H, Tabashidze N, Rossner P, Dostal M, Pastorkova A, Kong SW, et al. Altered vulnerability to asthma at various levels of ambient Benzo[a]Pyrene by CTLA4, STAT4 and CYP2E1 polymorphisms. Environ Pollut. 2017;231:1134–44.
Gref A, Merid SK, Gruzieva O, Ballereau S, Becker A, Bellander T, et al. Genome-Wide Interaction Analysis of Air Pollution Exposure and Childhood Asthma with Functional Follow-up. Am J Respiratory Crit Care Med. 2017;195:1373–83.
Ierodiakonou D, Coull BA, Zanobetti A, Postma DS, Boezen HM, Vonk JM, et al. Pathway analysis of a genome-wide gene by air pollution interaction study in asthmatic children. J Exposure Sci Environ Epidemiol. 2019;29:539–47.
Lin M. Effect of short-term exposure to gaseous pollution on asthma hospitalisation in children: a bi-directional case-crossover analysis. J Epidemiol Community Health. 2003;57:50–5.
Ueda K, Nitta H, Odajima H. The effects of weather, air pollutants, and Asian dust on hospitalization for asthma in Fukuoka. Environ Health Preventive Med. 2010;15:350–7.
Iskandar A, Andersen ZJ, Bønnelykke K, Ellermann T, Andersen KK, Bisgaard H. Coarse and fine particles but not ultrafine particles in urban air trigger hospital admission for asthma in children. Thorax 2012;67:252–7.
Kim J, Kim H, Kweon J. Hourly differences in air pollution on the risk of asthma exacerbation. Environ Pollut (Barking, Essex: 1987) 2015;203:15–21.
Byrwa-Hill BM, Venkat A, Presto AA, Rager JR, Gentile D, Talbott E. Lagged Association of Ambient Outdoor Air Pollutants with Asthma-Related Emergency Department Visits within the Pittsburgh Region. Int J Environ Res Public Health. 2020;17:8619.
Funding
This work was supported by Institutional Development Funds and the Endowed Chair in Genomic Research grant from The Children’s Hospital of Philadelphia. Research reported in this publication was supported by the National Center for Advancing Translational Sciences of the National Institutes of Health under award number TL1TR001880. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. This publication was made possible by grant number P30 ES013508 from the National Institute of Environmental Health Sciences (NIEHS), NIH. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the NIEHS, NIH.
Author information
Authors and Affiliations
Contributions
JK: Conceptualization, Investigation, Writing- Original draft preparation, Visualization. FM: Conceptualization, Investigation, Writing- Reviewing and Editing. HH.: Conceptualization, Supervision, Writing- Reviewing and Editing.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
Relevant ethical approval for this study was obtained.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kelchtermans, J., Mentch, F. & Hakonarson, H. Ambient air pollution sensitivity and severity of pediatric asthma. J Expo Sci Environ Epidemiol (2023). https://doi.org/10.1038/s41370-023-00573-7
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41370-023-00573-7
Keywords
This article is cited by
-
Recent Insights into the Environmental Determinants of Childhood Asthma
Current Allergy and Asthma Reports (2024)