Abstract
Background
There has been limited research considering the effects of prenatal exposure to multiple heavy metals on early childhood size and growth.
Objective
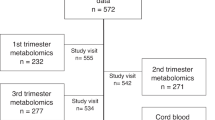
We evaluated prenatal exposures to 15 heavy metals in association with measures of weight, length, and head circumference (HC) measured at birth, and 1, 3 and 6 months of age in a study of 358 mother-child pairs.
Methods
Urinary concentrations were measured in the first and third trimesters of pregnancy and examined, using sex-stratified general linear models, in association with average standardized size and changes in size (growth) over the first 6 months of life. Confounding effects among metals were explored.
Results
Increased first trimester Hg and V were associated with decreased average HC among males and weight among females, respectively. Increased first trimester V was associated with a decline in weight among females over time. Increased third trimester Cs, Rb and Tl were associated with increased average weight and HC among males. Increased third trimester Se was associated with increased HC among females over time. Evidence for confounding was observed between Cs, Rb and Tl in association with weight and HC.
Significance
We observed multiple biologically plausible associations between prenatal heavy metal exposures and postnatal size and growth.
Impact
We have taken a comprehensive and novel approach to evaluating the impacts of prenatal heavy metal exposures on size and growth during early childhood. Our detailed analyses consider exposures to 15 different heavy metals at two time points during pregnancy, as well as multiple metrics of size and growth collected at birth and 1, 3 and 6 months of age.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 6 print issues and online access
$259.00 per year
only $43.17 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
Data availability
Access to data and code will require approval by the Guangdong Province Hospital for Occupational Disease Prevention and Treatment and the Chinese Center for Disease Control and Prevention. Contact the corresponding author for further details.
References
Wright RO. Environment, susceptibility windows, development and child health. Curr Opin Pediatr. 2017;29:211–7.
Huang S, Kuang J, Zhou F, Jia Q, Lu Q, Feng C, et al. The association between prenatal cadmium exposure and birth weight: a systematic review and meta-analysis of available evidence. Environ Pollut Barking Essex. 2019;251:699–707.
Baldewsingh GK, Wickliffe JK, van Eer ED, Shankar A, Hindori-Mohangoo AD, Harville EW, et al. Prenatal mercury exposure in pregnant women from suriname’s interior and its effects on birth outcomes. Int J Environ Res Public Health. 2020;17. https://doi.org/10.3390/ijerph17114032.
Gonzalez-Nahm S, Nihlani K, House SJ, Maguire LR, Skinner GH, Hoyo C. Associations between maternal cadmium exposure with risk of preterm birth and low after birth weight effect of Mediterranean diet adherence on affected prenatal outcomes. Toxics. 2020;8. https://doi.org/10.3390/toxics8040090.
Cheng L, Zhang B, Zheng T, Hu J, Zhou A, Bassig BA, et al. Critical windows of prenatal exposure to cadmium and size at birth. Int J Environ Res Public Health. 2017;14. https://doi.org/10.3390/ijerph14010058.
Wai KM, Mar O, Kosaka S, Umemura M, Watanabe C. Prenatal heavy metal exposure and adverse birth outcomes in Myanmar: a birth-cohort study. Int J Environ Res Public Health. 2017;14. https://doi.org/10.3390/ijerph14111339.
Laine JE, Bailey KA, Rubio-Andrade M, Olshan AF, Smeester L, Drobná Z, et al. Maternal arsenic exposure, arsenic methylation efficiency, and birth outcomes in the Biomarkers of Exposure to ARsenic (BEAR) pregnancy cohort in Mexico. Environ Health Perspect. 2015;123:186–92.
Sun H, Chen W, Wang D, Jin Y, Chen X, Xu Y. The effects of prenatal exposure to low-level cadmium, lead and selenium on birth outcomes. Chemosphere. 2014;108:33–9.
Hu J, Peng Y, Zheng T, Zhang B, Liu W, Wu C, et al. Effects of trimester-specific exposure to vanadium on ultrasound measures of fetal growth and birth size: a longitudinal prospective prenatal cohort study. Lancet Planet Health. 2018;2:e427–37.
Hu J, Wu C, Zheng T, Zhang B, Xia W, Peng Y, et al. Critical windows for associations between manganese exposure during pregnancy and size at birth: a longitudinal cohort study in Wuhan, China. Environ Health Perspect. 2018;126:127006.
Bermúdez L, García-Vicent C, López J, Torró MI, Lurbe E. Assessment of ten trace elements in umbilical cord blood and maternal blood: association with birth weight. J Transl Med. 2015;13:291.
Harari F, Langeén M, Casimiro E, Bottai M, Palm B, Nordqvist H, et al. Environmental exposure to lithium during pregnancy and fetal size: a longitudinal study in the Argentinean Andes. Environ Int. 2015;77:48–54.
Shirai S, Suzuki Y, Yoshinaga J, Mizumoto Y. Maternal exposure to low-level heavy metals during pregnancy and birth size. J Environ Sci Health Part A Tox Hazard Subst Environ Eng. 2010;45:1468–74.
Luo Y, McCullough LE, Tzeng J-Y, Darrah T, Vengosh A, Maguire RL, et al. Maternal blood cadmium, lead and arsenic levels, nutrient combinations, and offspring birthweight. BMC Public Health. 2017;17:354.
Kobayashi S, Kishi R, Saijo Y, Ito Y, Oba K, Araki A, et al. Association of blood mercury levels during pregnancy with infant birth size by blood selenium levels in the Japan environment and children’s study: a prospective birth cohort. Environ Int. 2019;125:418–29.
Schoenwolf GC, Bleyl SB, Brauer PR, Francis-West PH, Larsen WJ. Larsen’s human embryology. 2015 https://www.clinicalkey.com/dura/browse/bookChapter/3-s2.0-C20100689383.
Lin C-M, Doyle P, Wang D, Hwang Y-H, Chen P-C. Does prenatal cadmium exposure affect fetal and child growth? Occup Environ Med. 2011;68:641–6.
Liu L, Yao L, Dong M, Liu T, Lai W, Yin X, et al. Maternal urinary cadmium concentrations in early pregnancy in relation to prenatal and postpartum size of offspring. J Trace Elem Med Biol Organ Soc Min Trace Elem GMS. 2021;68:126823.
Villar J, Cheikh Ismail L, Victora CG, Ohuma EO, Bertino E, Altman DG, et al. International standards for newborn weight, length, and head circumference by gestational age and sex: the Newborn Cross-Sectional Study of the INTERGROWTH-21st Project. Lancet. 2014;384:857–68.
Hornung RW, Reed LD. Estimation of average concentration in the presence of nondetectable values. Appl Occup Environ Hyg. 1990;5:46–51.
Sikorski R, Paszkowski T, Szprengier-Juszkiewicz T. Mercury in neonatal scalp hair. Sci Total Environ. 1986;57:105–10.
Lederman SA, Jones RL, Caldwell KL, Rauh V, Sheets SE, Tang D, et al. Relation between cord blood mercury levels and early child development in a World Trade Center cohort. Environ Health Perspect. 2008;116:1085–91.
Gundacker C, Fröhlich S, Graf-Rohrmeister K, Eibenberger B, Jessenig V, Gicic D, et al. Perinatal lead and mercury exposure in Austria. Sci Total Environ. 2010;408:5744–9.
Ding G, Cui C, Chen L, Gao Y, Zhou Y, Shi R, et al. Prenatal low-level mercury exposure and neonatal anthropometry in rural northern China. Chemosphere. 2013;92:1085–9.
Murcia M, Ballester F, Enning AM, Iñiguez C, Valvi D, Basterrechea M, et al. Prenatal mercury exposure and birth outcomes. Environ Res. 2016;151:11–20.
Wells EM, Herbstman JB, Lin YH, Jarrett J, Verdon CP, Ward C, et al. Cord blood methylmercury and fetal growth outcomes in Baltimore newborns: potential confounding and effect modification by omega-3 fatty acids, selenium, and sex. Environ Health Perspect. 2016;124:373–9.
Berglund M, Lind B, Björnberg KA, Palm B, Einarsson Ö, Vahter M. Inter-individual variations of human mercury exposure biomarkers: a cross-sectional assessment. Environ Health. 2005;4:20.
Gade M, Comfort N, Re DB. Sex-specific neurotoxic effects of heavy metal pollutants: Epidemiological, experimental evidence and candidate mechanisms. Environ Res. 2021;201:111558.
Fortoul TI, Rojas-Lemus M, Rodriguez-Lara V, Gonzalez-Villalva A, Ustarroz-Cano M, Cano-Gutierrez G, et al. Overview of environmental and occupational vanadium exposure and associated health outcomes: an article based on a presentation at the 8th International Symposium on Vanadium Chemistry, Biological Chemistry, and Toxicology, Washington DC, August 15–18, 2012. J Immunotoxicol. 2014;11:13–18.
Poggioli R, Arletti R, Bertolini A, Frigeri C, Benelli A. Behavioral and developmental outcomes of prenatal and postnatal vanadium exposure in the rat. Pharm Res. 2001;43:341–7.
Usende IL, Olopade JO, Emikpe BO, Oyagbemi AA, Adedapo AA. Oxidative stress changes observed in selected organs of African giant rats (Cricetomys gambianus) exposed to sodium metavanadate. Int J Vet Sci Med. 2018;6:80–9.
Diaz-Castro J, Pulido-Moran M, Moreno-Fernandez J, Kajarabille N, de Paco C, Garrido-Sanchez M, et al. Gender specific differences in oxidative stress and inflammatory signaling in healthy term neonates and their mothers. Pediatr Res. 2016;80:595–601.
Koifman S, Koifman RJ, Ferreira J, Curado M. Health effects in a population cohort exposed to Cesium 137 in the Goiania radiological accident: offspring growth and development during childhood and adolescence. Epidemiology. 2008;19:S210.
Anke M, Angelow L, Müller R, Anke S. Recent progress in exploring the essentiality of the ultratrace element rubidium to the nutrition of animals and man. Biomed Res Trace Elem. 2005;16:203–7.
Yokoi K, Kimura M, Itokawa Y. Effect of low dietary rubidium on plasma biochemical parameters and mineral levels in rats. Biol Trace Elem Res. 1996;51:199–208.
Xia W, Du X, Zheng T, Zhang B, Li Y, Bassig BA, et al. A case-control study of prenatal thallium exposure and low birth weight in China. Environ Health Perspect. 2016;124:164–9.
Hanzel CE, Verstraeten SV. Thallium induces hydrogen peroxide generation by impairing mitochondrial function. Toxicol Appl Pharm. 2006;216:485–92.
Lozano M, Murcia M, Ballester F, Soler-Blasco R, Iñiguez C, Irizar A, et al. Prenatal selenium exposure and postnatal anthropometric effects in Spanish INMA cohorts. Environ Epidemiol. 2019;3:250–1.
Tariq U, Krupa C, Qamar H, Mahmud A, Ahmed T, Gernand A, et al. The association between maternal and umbilical cord selenium status and fetal and infant growth in a birth cohort in Dhaka. Bangladesh Curr Dev Nutr. 2020;4:1087.
Pieczyńska J, Grajeta H. The role of selenium in human conception and pregnancy. J Trace Elem Med Biol. 2015;29:31–8.
Hofstee P, Bartho LA, McKeating DR, Radenkovic F, McEnroe G, Fisher JJ, et al. Maternal selenium deficiency during pregnancy in mice increases thyroid hormone concentrations, alters placental function and reduces fetal growth. J Physiol. 2019;597:5597–617.
Geng X, Geng L, Zhang Y, Lu H, Shen Y, Chen R, et al. Fetal sex influences maternal fasting plasma glucose levels and basal β-cell function in pregnant women with normal glucose tolerance. Acta Diabetol. 2017;54:1131–8.
Vacchi-Suzzi C, Kruse D, Harrington J, Levine K, Meliker JR. Is urinary cadmium a biomarker of long-term exposure in humans? A review. Curr Environ Health Rep. 2016;3:450–8.
Iinuma T, Nagai T, Ishihara T, Watari K, Izawa M. Cesium turnover in man following single administration of 132CS: 1. Whole body retention and excretion pattern. J Radiat Res. 1965;6:73–81.
Couffignal C, Chevillard L, El Balkhi S, Cisternino S, Declèves X. The pharmacokinetics of lithium. In: Malhi GS, Masson M, Bellivier F, editors. The science and practice of lithium therapy. Cham: Springer International Publishing; 2017. p. 25–53.
Fieve RR, Meltzer HL, Taylor RM. Rubidium chloride ingestion by volunteer subjects: Initial experience. Psychopharmacologia. 1971;20:307–14.
Gad SC, Pham T. Thallium. In: Wexler P, editor. Encyclopedia of toxicology. 3rd ed. Oxford: Academic Press; 2014. p. 527–9.
Heinemann G, Fichtl B, Vogt W. Pharmacokinetics of vanadium in humans after intravenous administration of a vanadium containing albumin solution. Br J Clin Pharm. 2003;55:241–5.
Valentine JL, Kang HK, Spivey GH. Selenium levels in human blood, urine, and hair in response to exposure via drinking water. Environ Res. 1978;17:347–55.
Funding
National Institute of Environmental Health Sciences, National Institutes of Health (R01ES025796); National Natural Science Foundation of China (No. 81972990, LLiu); Guangdong Provincial Science and Technology Plan (2017B030314152, JC).
Author information
Authors and Affiliations
Contributions
LY, LLiu, JC, XS, SS and PB were responsible for the overall design of the study. LLiu, MD, JY and ZZ were responsible for generating heavy metal measurements. LLv, ZW, JW and XS oversaw participant recruitment and data and biospecimen collection. LLiu conducted all data analyses with oversight by LY and SS. LY, LLiu, SS and PB contributed to writing the report. All authors provided feedback on the report.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
The study was approved by the ethical committee of the Chinese Center for Disease Control and Prevention.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Yao, L., Liu, L., Dong, M. et al. Trimester-specific prenatal heavy metal exposures and sex-specific postpartum size and growth. J Expo Sci Environ Epidemiol 33, 895–902 (2023). https://doi.org/10.1038/s41370-022-00443-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41370-022-00443-8