Abstract
Malocclusion, identified by the World Health Organization (WHO) as one of three major oral diseases, profoundly impacts the dental-maxillofacial functions, facial esthetics, and long-term development of ~260 million children in China. Beyond its physical manifestations, malocclusion also significantly influences the psycho-social well-being of these children. Timely intervention in malocclusion can foster an environment conducive to dental-maxillofacial development and substantially decrease the incidence of malocclusion or reduce the severity and complexity of malocclusion in the permanent dentition, by mitigating the negative impact of abnormal environmental influences on the growth. Early orthodontic treatment encompasses accurate identification and treatment of dental and maxillofacial morphological and functional abnormalities during various stages of dental-maxillofacial development, ranging from fetal stages to the early permanent dentition phase. From an economic and societal standpoint, the urgency for effective early orthodontic treatments for malocclusions in childhood cannot be overstated, underlining its profound practical and social importance. This consensus paper discusses the characteristics and the detrimental effects of malocclusion in children, emphasizing critical need for early treatment. It elaborates on corresponding core principles and fundamental approaches in early orthodontics, proposing comprehensive guidance for preventive and interceptive orthodontic treatment, serving as a reference for clinicians engaged in early orthodontic treatment.
Similar content being viewed by others

Introduction
Malocclusion ranks among the top three oral diseases as identified by the World Health Organization. This condition profoundly impacts the dental-maxillofacial functions, facial esthetics, and the growth and development of ~260 million children in China.1,2 Beyond its physical manifestations, malocclusion also significantly influences the psycho-social well-being of these children. The emergence of malocclusion is influenced by both genetic and environmental factors. Timely intervention in malocclusion can foster a conducive environment for dental-maxillofacial development, thereby mitigating the negative impact of abnormal environmental and genetic influences on dental-maxillofacial growth. Such early interventions can substantially decrease the incidence of malocclusion in children, thereby enhancing their overall physical and mental health. From an economic and societal standpoint, the urgency for effective early orthodontic treatments for malocclusion in children cannot be overstated, underlining its profound practical and social importance. This consensus paper outlines the detrimental effects of malocclusion, underscores the critical need for early treatment, and introduces core principles and fundamental approaches. It proposes guidance for preventive and interceptive orthodontic interventions across various stages of dental-maxillofacial growth and development, from fetal stages to the early permanent dentition phase. This paper emphasizes the necessity of a systematic approach to promote and standardize early orthodontic treatment, underscoring its significance in improving children’s health outcomes. Early intervention for malocclusion in childhood involves timely identification and treatment of dental-maxillofacial morphological and functional abnormalities during various stages of development. Through effective and rational intervention, this approach aims to eliminate oral and systemic environmental factors that adversely affect dental-maxillofacial development. It also seeks to reduce the severity and complexity of malocclusion, thereby achieving harmonious and esthetically pleasing dental-maxillofacial structures and functions with greater efficiency. This consensus paper will elaborate on the characteristics of childhood malocclusion and the corresponding principles of preventive treatment. It proposes guidelines and fundamental principles for early intervention, serving as a reference for clinicians engaged in early orthodontic treatment.
Definition and risk of malocclusion
Malocclusion is a multi-factorial condition in children characterized by abnormal growth and development, influenced by genetic and environmental factors including dental and pulp diseases, trauma, oral habits, dental replacement disorders, among others. This condition leads to misalignment of teeth, abnormalities in the relationship between the upper and lower dental arches, morphological and positional abnormalities in jaw size, and facial deformities, among other manifestations.
Oral functions
Malocclusion seriously affects children’s oral functions, including mastication, swallowing, speech and temporomandibular joint functions. Occlusion characterized by deep overbite, open bite, or occlusal interference results in deviations in the range and trajectory of mandibular movements during opening, protrusion, and lateral movements. This may induce perioral muscle fatigue and/or degeneration, subsequently affecting the temporomandibular joint function and potentially resulting in organic pathology.3,4,5,6,7,8,9,10,11 Atypical tongue posture and swallowing patterns often contribute to the onset and progression of malocclusion, acting as predisposing factors rather than merely being correlated with it.12,13,14,15,16,17,18 Moreover, malocclusion can impact articulation, as exemplified by individuals presenting skeletal Class III malocclusion who may experience speech impairments.19,20,21,22,23 Malocclusion, characterized by misalignment, along with abnormalities in the size, shape, and number of teeth can reduce the functional contact area of the maxillary and mandibular teeth and result in reduced masticatory efficiency.24,25,26
Oral health
The accumulation of food debris, plaque, and the subsequent increased formation in calculus resulting from dental crowding and misalignment poses challenges in effective oral hygiene maintenance. Such conditions can give rise to caries, gingival periodontal diseases, and periapical disease, among other oral health concerns.27,28,29 In other cases, occlusal trauma caused by premature contact has the potential to exacerbate periodontal disorders,30,31 while the anterior protrusion of upper incisors heightens the susceptibility to dental trauma.32,33,34,35,36,37,38,39
Dental-maxillofacial growth
In the context of children’s growth and development, malocclusion affects dental and maxillofacial development, impacting both soft and hard tissues. For instance, an anterior crossbite compounded by a potential abnormally anterior positioning of the mandible may impede the sagittal growth of the maxilla and stimulate excessive mandibular growth, consequently disrupting the balance of the sagittal relationship between the maxilla and mandible. In the other case, excessive narrowing of the upper dental arch or upright upper anterior teeth may restrict mandibular protrusion, impeding its development. Additionally, unilateral posterior crossbite or occlusal interferences will result in asymmetric facial development.40,41
Physical and mental health
Malocclusion is correlated with general development of children’s whole body. Impaired chewing function resulting from malocclusion may lead to a reduction in nutrition intake.42 Mandibular retrusion is one of the contributing factors to obstructive sleep apnea, also called obstructive sleep apnea hypopnea syndrome, whose associated consequences include sleep disturbances, neurocognitive issues, and attention deficits.43 Apart from physical health, malocclusion, especially those leading to a poor facial appearance, affects children’s psychological health, forming low self-esteem. Increased overjet and deep bite, space between anterior teeth, and extremely misaligned teeth are potential reasons for children to be teased,44,45,46 causing the affected person isolated from the social activities and difficult to interact with others.
Mechanism of the occurrence of malocclusion
The etiology of malocclusion involves multi-factorial influences. One influential factor can cause different types of malocclusion, while a single malocclusion can be attributed to different influential factors acting in a complexity mode.47 Therefore, it is important to analyze the etiological mechanism during the diagnosis and treatment of malocclusion. More importantly, we need to provide proper solutions to eliminate the influential factor in early orthodontic interventions.48
Based on current understanding, it is believed that the development of children’s teeth and maxillofacial complex is affected by various factors, including genetics, environment, diseases, and injury.49 Genetic factors control craniofacial morphology, structure and size, whereas environmental factors exert a greater influence on the growth and development of alveolar and jawbones.50,51,52,53 In the genetic context, environmental factors exacerbate the malocclusion manifestation.54 At the systemic level, craniofacial congenital malformations and genetic diseases cause abnormal craniofacial morphology. Main localized environmental factors, such as abnormal respiratory and swallowing functions, inadequate mastication, poor oral habits, and oral health, affecting dental and maxillofacial growth and development at the local level.
Genetic factors
The genetic factors of malocclusion are closely correlated with racial evolution and personal growth. With the human evolution, dietary patterns have changed, leading to a gradual degeneration of chewing muscles, jawbone, and teeth. Given the inconsistent degree of jawbone and teeth degeneration, the lack of coordination between the mass of teeth and bone results in tooth crowding and malocclusion. Malocclusion, when inherited from parents. poses challenges to correction due to genetic factors.55 Therefore, clear and early diagnosis and treatment planning are demanded, aiming to compensate for the imbalanced craniofacial growth. Early orthodontic treatment should involve selecting appropriate methods and establishing reasonable staged treatment goals. It is important to ensure an extended period of maintenance and adhere to a long-term follow-up treatment regime after early orthodontic treatment.
Disease factors
Throughout the growth and development process from embryonic period to childhood, various diseases can lead to the occurrence of malocclusion Maternal malnutrition or diseases during pregnancy can cause fetal dental and maxillofacial dysplasia or developmental abnormalities.56 Some acute and chronic diseases in childhood can affect teeth, jaw, and face growth, as well as total health.57 For example, vitamin D deficiency causes calcium and phosphorus metabolism disorders, hypothyroidism, pituitary gigantism and other diseases, which would lead to malformation of jawbone and dental arch development,58,59,60.
Localized environmental factors
Malocclusion is often caused by local disorders during tooth replacement in children. Early loss or retention of deciduous teeth can lead to succeeding permanent teeth eruption disorders and dislocation. Another common local environmental factor is deleterious oral habits. The unilateral chewing habit may result in posterior teeth crossbite on the chewing side, a shift in the midline of the upper and lower arches toward the chewing side, and ultimately, facial asymmetry.40,41 Non-nutritive sucking (NNS) such as finger-sucking, lead to anterior open bite and dental-arch narrowness.61,62,63,64,65 Thrusting the tongue and licking the anterior teeth during eruption may also contribute to localized anterior open bite. Additionally, biting the upper lip causes mandibular protrusion and anterior crossbite.66,67,68,69
Main contents of early orthodontic treatment
Malocclusion, a variation from normal occlusion, is not classified as a disease but a developmental condition that often manifests during the transition to permanent dentition. Early orthodontic treatment of malocclusion plays a crucial role in managing oral health and functions in children. The goal is to create a conducive environment for the dental and maxillofacial development of children based on the growth potential of the dentition and jaw. This involves targeted interventions aimed at the prevention, guidance, and interception of malocclusion during its early developmental stages, where various orthodontic techniques and methods are applied with the aim of mitigating the severity and complexity of malocclusion.70,71,72
Early correction of malformation in children mainly includes:
Management of oral functionality development: oral chewing, swallowing, breathing and speech, and correction of bad oral habits.
Management of occlusal development: management of dental developmental abnormalities (abnormal tooth eruption, number, or morphology), management of tooth replacement abnormalities (space management), orthopedic treatment of alveolar bone developmental abnormalities, and early correction of dental malocclusion that affects oral health, function and growth and development of children.
Management of maxillofacial growth and development: early treatment of abnormal muscle functionality and functional malocclusion such as occlusal interferences affecting craniofacial development, comprehensive treatment of craniofacial growth and development abnormalities caused by abnormal oral functionality, orthopedic treatment of mild, moderate, and severe disharmonies of jaws in children, control of hereditary craniofacial morphological abnormalities.
Management of general health and development: including children’s nutritional health maintaining, early treatment of children’s respiratory diseases, correction of children’s abnormal body and head posture, prevention and treatment of children’s craniofacial trauma (condylar and jaw fractures).73,74,75,76,77,78,79
Principals of early orthodontic treatment
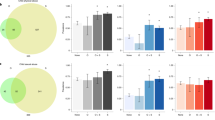
Early orthodontic treatment leverages the dental and jaw growth potentials in children to prevent and interrupt the development of malocclusion, achieving the staging treatment goals73 (Fig. 1).
The treatment purpose of early intervention of malocclusion in children must be clearly defined, with an emphasis on accurate diagnosis and reasonable treatment plan as fundamental aspects for early orthodontic treatments. It’s crucial for early orthodontic treatment to be both effective and efficient, with clinicians balancing the cost and benefits involved. Modern early intervention methods for malocclusion in children combine appliance treatments with training of oral and perioral muscle functions. The available orthodontic appliances are primarily categorized into removable and fixed appliances, along with segmental fixed multi-bracket braces and clear aligners. Their functions cover palatal expanders, functional regulators, space maintainers, and oral muscle trainers. The integrated method addresses both structural and functional aspects of malocclusion, reflecting advancements in pediatric orthodontic theory.
Early orthodontic treatment of malocclusion in children also carries certain limitations and risks, requiring careful consideration in clinical decision-making. Due to the active period of dental and maxillofacial growth and development, manifestations of malocclusion in children may not be fully expressed, with some skeletal deformities or growth patterns potentially remaining stationary until growth is completed. In addition, accurately predicting growth patterns and amounts still presents some difficulties, particularly in forecasting the prognosis of genetic and/or skeletal issues, hence caution is advised regarding prolonged treatments, sequential tooth extraction, and other irreversible interventions. Simultaneously, it is imperative to acknowledge the limitations inherent in dentofacial growth modification. Our current repertoire of techniques for restraining jaw growth or fostering mandibular ramus growth remains relatively restricted. In instances where evidence is insufficient to substantiate early intervention, a conservative stance is warranted.
Specific challenges also exist during the process of early orthodontic treatment. For instance, primary teeth may exhibit shorter crowns and greater occlusal tapering, posing challenges for the bonding or retaining of orthodontic appliances. Children’s immature mindset may also impede compliance with treatment, resulting in insufficient wearing time of removable appliances and poor orthodontic effects. Poor oral hygiene and habits can lead to relapse of malocclusions or complications, such as dental caries and periodontal issues. Moreover, children’s tooth roots and alveolar bone are currently in a developmental state. It is essential for clinicians to closely monitor them and be vigilant in preventing potential treatment complications.
During the transition from primary to mixed dentition, children may experience conditions such as mild incisor crowding of less than 2 mm, maxillary midline diastema of less than 2 mm, divergence of lateral and central incisor crowns, molar half cuspid distal relationship, and mild deep bite, owing to factors like incisor liability and Leeway Space, which essentially represent asynchronous adjustments between bone and tooth mass. These occurrences are typically normal and may resolve spontaneously to establish a normal occlusion, requiring no treatment.80 Unless requested by the patient for temporary esthetics, minimally invasive approaches should be favored during this period.81,82,83,84
Clinical examination and diagnosis of malocclusion in children
The clinical examination and diagnosis of early orthodontic treatment comprehend oral health and function, dental and maxillofacial morphology and structures, and general health development. Special attention should be given to evaluating occlusal development and relationships, as well as upper respiratory tract health85 (Fig. 2).
Oral occlusal development examination: tooth age, tooth eruption, occlusal relationship, and oral health examination. The number of deciduous permanent teeth and mandibular symmetry are examined by panoramic radiography.
Facial morphological function examination: facial symmetry, facial lateral appearance and growth type, breathing, swallowing, facial muscle function, jaw opening and closing movement.
Craniofacial morphological and structural examination: cephalometric analysis, cervical spine development analysis, tooth eruption and morphological abnormalities exam by cone-beam computed tomography (CBCT).
Oral Habits: through interviews and chairside observations, assess whether the child has oral habits such as lip biting, finger sucking, or tongue thrusting.
Children’s growth and development potentials: analysis of the second, third, and fourth cervical vertebrae morphology using lateral cephalometric films to determine the growth and development period of children.86,87,88
Upper respiratory tract examination in children: using lateral head films, check for hypertrophic adenoids and tonsils (whether they affect the patency of the upper respiratory tract) and, if necessary, consult an otolaryngologist.
General development and health checkup: For children with obvious systemic developmental abnormalities (growth hormone, shape abnormalities, craniofacial morphology, etc.), a consultation with a pediatrician is requested before starting early correction and treatment of systemic health developmental abnormalities.
Principals of malocclusion prevention in children
The general principles of child malocclusion prevention include:
Early orthodontic treatment in children begins with eugenics: The fetal period is an important stage of dental and maxillofacial development. Attention at this stage can avoid the occurrence of many congenital genetic diseases.89,90,91,92,93,94,95
Good oral hygiene habits: Maintaining good oral hygiene habits is effective in ensuring healthy and balanced oral soft and hard tissues in functions. Intact, healthy and functionally balanced oral soft and hard tissues are prerequisites for good child facial development.
Early detection and treatment of oral diseases: including caries, periapical disease, mucosal disease, abnormal tethering attachment soft and hard tissue diseases that affect oral function.
Good oral function habits: respiratory, swallowing, language and other neuromuscular habits.
Early detection and correction of abnormal oral functional habits: including abnormal breathing, swallowing, chewing, tongue thrusting, lip licking, finger sucking, cheek sucking, abnormal head and neck posture, abnormal full-body posture, etc.
Clinical practice of early orthodontic treatment in different growth stages
Orthodontic treatment in primary dentition (2.5/3–6 years of age)
Oral hygiene habits: Cultivating optimal oral hygiene practices should start with oral cleaning from birth. Parents should prioritize maintaining a proper feeding posture during this period, advocate breastfeeding, avoid bad bottle feeding posture, pay attention to chewing function training, and avoid too soft food.96,97,98
Oral functional habits: Parents should be vigilant in the timely detection and correction of various detrimental oral habits that may emerge after the oral appetite period, such as the continued use of the pacifier and thumb or finger sucking.61,99,100 It is important to introduce proper oral functions, such as lip closure training and tongue exercises. Additionally, preventing trauma to the deciduous teeth is essential.101,102,103
Crossbite correction: Crossbite in primary dentition should be corrected with orthodontic removable appliances, such as a removable appliance with recurved spring and a posterior bite plane, a bonded lower anterior acrylic slide plane for anterior crossbite, and removable or bonded Schwartz expanders with occlusal coverage for posterior crossbite. Chin caps can correct the bad habits of mandibular advancement during the primary dentition. For children with functional protruding mandible with tonsillar hypertrophy, otolaryngology should be consulted while correcting anterior crossbite, and the hypertrophied tonsils should be removed promptly if necessary to avoid secondary mandibular protrusion. For children with hereditary maxillary hypoplasia, maxillary expansion with anterior traction or Frankel III (functional regulator III, FR III) is feasible for early treatment to promote maxillary development.
Other dental malocclusion: During the primary dentition period, malocclusion, such as severe anterior deep overbite, significant arch narrowing, anterior protrusion of upper incisors, and posterior crossbite, combined with abnormal oral functions causing the child’s palatal mucosa injuries should be treated promptly. A common condition is anterior deep overbite causing the trauma of the palatal mucosa.
Periodically detection and correction of all kinds of bad oral habits are needed. The correction of habits such as abnormal sucking, biting, and incomplete lip closure should begin after 3.5 years of age.
Skeletal disorders: Children with abnormal facial growth patterns in the primary dentition, such as anterior maxillary protrusion, clockwise rotation of the lower jaw, and a noticeable acute mandibular angle, may be temporarily unable to undergo systematic orthopedic treatment. Instead, primary adjunctive therapy could involve oral functional training.
Space maintenance: In the case of premature loss of primary deciduous molars and mandibular primary canines, space maintenance is required104.
Other diseases: Clinicians should promptly detect and treat ear, nose, and throat (ENT) diseases, and other respiratory diseases, and treat oral soft and hard tissue diseases that may cause changes in the functional environment of the oral cavity.
Orthodontic treatment in mixed dentition (6–12 years of age)
Early orthodontic treatment in the mixed dentition should primarily focus on differentially diagnosing the physiological malocclusions of mixed dentition. Temporary malocclusion in mixed dentition should be observed without urgent orthodontic treatment:
-
(1)
maxillary midline diastema (<2 mm): mostly caused by the lateral incisor germ pressing the root of the central incisors, which can self-correct with the eruption of the lateral incisor.
-
(2)
distal tipping lateral incisors: mostly caused by the canine’s germ pressing the root of the lateral incisors.
-
(3)
mild to moderated anterior deep bite, characterized by minimal lingual inclination of upper incisors: can self-adjust with the growth of the mandible and the increase of alveolar bone height and molar crown height after the completion of tooth replacement.
-
(4)
mild crowding of incisors (incisor liability): typically resolved by the labial eruption of anterior teeth, utilization of the primate space, and natural growth of the arch width.
-
(5)
mild distal relationship of first permanent molars: can be adjusted with the replacement of the primary molars by premolars, in which upper and lower first permanent molars drift mesially differently (using Leeway Space) and differential growth of the maxilla and mandible (mandibular growth retardation).
The basic elements of early orthodontic treatment in children with mixed dentition include:
Anterior Cross Bite: Timely treatment of dental and functional anterior crossbite is crucial, which should be detected and addressed promptly. The main purpose of anterior crossbite correction is to interrupt functional mandibular advancement, preventing the progression of a dental problem to a skeletal problem. For skeletal Class III malocclusions caused by genetic factors, noticeable maxillary and mandibular discrepancy during this period. For children with predominantly genetic maxillary underdevelopment, early treatment with maxillary expansion with anterior traction or FR III orthodontic appliances can promote maxillary development,104,105,106 while efforts should be made to control mandibular overgrowth or allow slight compensation through mandibular rotation. In obviously severe hereditary skeletal anterior crossbite, early clinical controls of mandibular growth could be facilitated, but clinical efficacy is uncertain.
Tonsillar hypertrophy is a risk factor for the development of skeletal anterior crossbite in children. Children with anterior crossbite and oversized tonsils should be promptly referred to an ENT specialist for evaluation. If necessary, tonsillectomy should be considered along with functional orthodontic treatment to control mandibular advancement.
Anterior deep bite and deep overjet with labial inclination: Treatment involves uprighting proclined upper incisors, lingually tipping lower incisors, coordinating of upper and lower arch width, and timely correction of anterior deep overjet. This treatment should be complemented with lip competency improvement to alleviate the adverse effects of weak perioral muscle function on exacerbating deep overjet. Additionally, correct oral sucking habits if necessary. Early and timely bite opening can improve vertical growth of the jaws and increase the height of the lower third of the face, changing the horizontal growth pattern of the face.107 Early correction of deep overjet with labial tipped of the upper incisors can prevent incisor fractures in children.
Facial protruding profiles in children: For patients with Skeletal Class II malocclusion with the functional mandibular recession, the upper and lower arch widths are checked for their coordination, and the arch can be expanded early to release functional mandibular recession due to the narrow upper arch.
Functional orthodontic appliances of mandibular advancement are the main orthodontic appliances used during this period, and the timing of orthodontic treatment is during the pre- or during the peak of the pubertal growth spurt of the child.108
For skeletal maxillary protrusion, the growth of the protrusive maxilla should be suppressed as much as possible during the growth and functional appliances facilitated with extra-oral headgear should be used, and treatment time should start before the peak of pubertal growth.
Early orthodontic treatment of dental developmental abnormalities: Early detection and orthodontic treatments can alleviate occlusal interference and tooth transposition caused by abnormal tooth eruption, while also restoring chewing function and esthetic appearance of the front teeth.109,110,111,112,113,114,115,116,117,118 The early orthodontic tract aid eruption of the buried teeth, blocked teeth and curved root teeth will not cease the root development of the unerupted permanent teeth and cause the apical resorption, and even have the effect of reducing the severity of root curvature of curved teeth, but the biological light force (30–60 g) required.119,120
Timely space management: Timely space management is crucial in cases of premature loss of primary teeth. Except the premature loss of upper incisors, it is necessary to prevent space loss. This is especially important when the anticipated eruption of permanent successors is more than 6 months. Special attention should be paid to maintaining space after the premature loss of the upper and lower second deciduous molars and lower deciduous canines.114,121,122,123,124 For patients with already closed edentulous space, procedures to regain space may be necessary. This facilitates the normal replacement of deciduous and permanent teeth.
Early maxillary expansion: Patients should undergo early orthodontic treatment for insufficient arch widths, abnormal arch length, uncoordinated upper and lower arch forms, as well as asymmetric left and right arch forms. Maxillary bony expansion should be performed before the mid-palatal suture is closed, and the best time for maxillary expansion is from 7 to 10 years old, in which time the bone effects of early expansion is better.116,125,126,127,128,129
Deleterious oral habits: In mixed dentition, early identification and intervention should be performed for all kinds of bad oral habits, including mouth breathing, atypical swallowing, tongue thrusting, functional mandibular advancement, NNS (thumb, finger, cheek, or a similarly shaped object), lip biting, soft diet, bottle-feeding incompetent lip closure, unilateral chewing habits, etc.98,130,131,132 Cooperating with early orthodontic treatment and actively carrying out functional training of maxillofacial muscles should be conducted.133,134,135,136,137,138 Orofacial myofunctional therapy (OMT) targets oral and oropharyngeal structures, aiming to improve muscle tone, endurance, and coordinated movements in the pharynx and surrounding areas. Clinically, OMT has shown positive outcomes in enhancing swallowing function, correcting tongue posture and muscle dysfunction, and reducing the likelihood of relapse from previous orthodontic treatments.139,140 At this stage, if a child is unable to self-correct bad habits after reminder and reward therapy, some orthodontic appliances can be used as habit breakers for auxiliary intervention. For instance, vestibular shields can be used to block habitual mouth breathing and for lip muscle training, frog-mouth appliances can correct immature swallowing patterns, and palatal bar or tongue crib can prevent tongue thrusting and NNS. Some prefabricated myofunctional appliances made of silicone materials can be used simultaneously for occlusal guidance, habit cessation, and muscle function training.141,142,143,144,145,146,147
Other diseases: It is needed to have timely detection and treatment of otolaryngological diseases and other respiratory diseases, and oral soft and hard tissue diseases that may cause changes in the functional and mechanical environment of the oral cavity in mixed dentition148 (Fig. 3).
Orthodontic treatment in early permanent dentition (after 12 years of age)
After the completion of the replacement of succeeding permanent teeth, the occlusal growth enters the early stages of permanent dentition. The second permanent molar is still to erupt, and the child is in the late stages of growth spurt of puberty. At the beginning of the permanent dentition, the speed of jaw growth and development slows down, but occlusion is not yet fully established, and growth modifications remain (especially in males).
Orthodontic treatment during this period still requires paying an attention to maintaining oral hygiene, good oral functions, and thorough correction of various oral malfunctions. Adjunctive oral muscle function training would help to stabilize the results of comprehensive orthodontic treatment of malocclusion.
Functional orthodontic treatment for anterior crossbite: Orthodontic functional therapy, such as FR III, may be beneficial in treating mild-to-moderate skeletal Class III malocclusions. It is recommended to track growth and development and conduct regular follow-up reviews. Due to the unpredictability of mandibular growth and development (especially in males), comprehensive orthodontic camouflage treatment in early permanent dentition should be postponed. Tooth exaction in the treatment plan for skeletal class III malocclusion should be approached with great caution to avoid complicating future orthodontic-orthognathic surgery to correct the jaw discrepancies in adulthood. For children with severe high-angle skeletal Class III malocclusion and a family history, combined orthodontic-orthognathic surgery is the appropriate treatment, eliminating the need for early intervention. Patients with maxillary hypoplasia of Class III malocclusion may benefit from anterior traction with palatal expansion or FR III orthodontic appliances in the early permanent dentition.
Orthodontic treatment of facial convex profile in early permanent dentition: At this stage, the mandible remains some growth potential (especially in males). For a retruded mandible, orthopedic treatment can still be performed firstly to address the sagittal discrepancy between maxilla and mandible. Note: For Class II malocclusion with maxillary width deficiency, a rapid expansion appliance to increase the maxillary arch base should be applied prior to the start of mandibular advancement or using a functional appliance with a maxillary expansion crew. Mild to moderate maxillary hypoplasia with an anteriorly protruding facial profile usually requires extraction to camouflage the skeletal protrusion. For severe skeletal maxillary protrusion, a combined orthodontic-orthognathic treatment should be chosen to correct the facial protrusion.
Orthodontic treatment of skeletal narrow upper arch: Due to the large variability of timing of the palatal suture closure, it is also possible to open the palatal suture during the early permanent dentition to correct skeletal width discrepancy. Most of the clinical methods are involved in fixed palatal rapid expansion and mini implant-assisted rapid palatal expansion.149
Orthodontic treatment of crowding: The appropriate orthodontic method is selected based on the analysis of tooth-sizes and alveolar bone volume. Clinical methods of space obtaining include tooth extraction, molar distalization, arch expansion, and use of Leeway Space. The amount of space gained by arch expansion in the early permanent dentition is limited and should be used with cautions. In patients of mild to moderate crowding with straight profile, non-extraction orthodontic treatment can be chosen to correct the crowding. In severe crowding, extraction should be chosen to align the teeth to maintain the normal profile.150,151
Clinical management of early orthodontic treatment
Children are in the immature stage of physiological and psychological development, early orthodontic treatment is different from adult orthodontic treatment in the aspects of the selection of orthodontic methods, orthodontic follow-up process, patient compliance.
Early orthodontic treatment of children with malocclusion requires patients and parents to fully understand the purpose and significance of early orthodontic treatment goals. Clinicians of early orthodontic treatments need to emphasize that early orthodontic treatment has a positive effect on craniofacial development, and that early orthodontic treatment of malocclusion in children is at the optimal time of growth and development. This necessitates the prevention and interception of abnormal dental and maxillofacial manifestations in children at different stages according to the genetic and environmental factors, as well as the etiological mechanisms of malocclusion. Additionally, it involves promoting coordinated and balanced dental and maxillofacial growth and development to reduce the severity and complexity of malocclusion. Early orthodontic treatment can reduce the possibility of orthognathic surgery needs for skeletal problems of patients in adult. Preoperative communication with the patient and their parents to obtain their consensus is fundamental for a successful early orthodontic treatment.
It should be emphasized that the nature of the staging and limitations of early orthodontic treatment in children, and the continuity between early orthodontic treatment and later comprehensive orthodontic treatment. The early orthodontic treatment is four-dimensional orthodontic treatment, incorporating a timeline of growth and development. It is also important to maintain a comprehensive oral health for normal dental and maxillofacial growth and development in the early orthodontic treatment for children.
Varied choices of early orthodontic treatment for children should be provided. Clinicians of early orthodontic treatments need to select the most suitable orthodontic appliance for the child based on the mechanism of child’s malocclusion, the principle of appliance design, and the patient’s compliancy to the appliance and patient’s financial ability. When multiple orthodontic methods are available to achieve the same desired effect, the orthodontist should select the method based on the patient’s and parents’ preferences, considering the effect and benefit ratio.
In addition to the expected results, the duration of treatment is also a major concern for children and their parents. Early orthodontic treatment should have a clear purpose. It is usually shorter than comprehensive orthodontic treatment. Time-consuming orthodontic treatment should be avoided in the staged treatment. In addition, since there is still time from the first phase of early orthodontic treatment to the completion of permanent dentition, efficacy of early orthodontic treatment should be emphasized. Communication before the start of treatment can allow patients and their parents to have an adequate psychological preparation.
Early orthodontic treatment requires the active cooperation of patients and their parents, and clinical compliance is an important factor in the success of early orthodontic treatment. Early orthodontic treatment focuses on problems that interfere with maxillofacial growth and development, oral health and oral functions, and the tooth alignment is not a priority to considerate, removable and functional appliances are mostly used in early orthodontic treatment. The removable orthodontic appliances require active patient cooperation to ensure accurate adaptation and secure retention otherwise the efficacy of the appliance can be compromised. In addition, early orthodontic treatment is concerned with oral function and perioral muscle activators and will also require the patient’s cooperation with appropriate oral function and perioral muscle training. The clinicians of early orthodontic treatment should also fully communicate with the patient and their parents prior to treatment regarding the need for cooperation and the lack of orthodontic effect due to poor-cooperation.
Notes on early orthodontic treatment
Timing of early orthodontic treatment
Early orthodontic treatment is treatment by using patient’s maxillary growth and development, correct and effective orthodontic treatment can change the abnormal dental and facial growth, and promote the coordinated development of dental and jaws. Early orthodontic treatment requires accurate timing to make a good use of growth (without delaying treatment), but also to quickly and effectively complete the staging of treatment (to avoid excessive clinical orthodontic time). For example, when addressing mandibular underdevelopment through functional treatments, initiating treatment during the pre-peak or peak of puberty growth and development can effectively correct the mandibular deficiency and reduce overall clinical treatment time.
-
(1)
The different sequence of three-dimensional growth and development of the jaws and face determines the different timing for the start of early orthodontic treatment of malocclusion on different dimensions, and clinical early orthodontic treatment should be noted.
-
(2)
The correlation between tooth eruption and occlusal development to the jaw development is week, and the timing of orthodontic treatment of dental development abnormalities is different from the correction of jaw developmental abnormalities.
-
(3)
Early orthodontic treatment is not the final treatment, and most of the early orthodontic treatments also requires later phase comprehensive orthodontic treatments in the permanent dentition. Early orthodontic treatment is mostly two-phases treatment.
-
(4)
Treatments of abnormal facial growth patterns should be postponed, and worth to wait after the completion of child’s craniofacial growth and development to make the treatment choices. Individuals with skeletal class III malocclusion have large mandibular bones. Because mandibular development could continue until late adolescence or even 20 years old, and orthodontic treatment should be postponed. Individuals with skeletal class III malocclusion with hereditary high-angle mandibular over-development (especially for male high-angle patients) often require orthodontic-orthognathic combination therapy in adulthood. Underdevelopment of the mandibular ascending branch causes front open bite (over-erupted molars). early orthodontic treatment is prone to recurrence of open bite due to incomplete vertical development of the mandible, and clinical treatment should be postponed.
-
(5)
The pursuit of early orthodontic treatment is better dental and jaw coordination and esthetics, better oral function maintenance, and more stability of treatment results. Early orthodontic treatment that does not expect to achieve better results is not necessary.
Oral and systemic health management in children during early orthodontic treatment
Oral Health Management for Children (OHMC) refers to the comprehensive management of dental, jaw, and facial health growth and development, including early prevention, early diagnosis and early intervention, and early orthodontic treatment of malocclusion in children is the core of OHMC from embryo to adult. Since early orthodontic treatment of malocclusion in children coincides with the peak growth and development of children, the comprehensive management of children’s oral and general health cannot be neglected. It includes reasonable dietary balance, supplementation of calcium, phosphorus, and vitamins, etc.; cultivation and maintenance of good oral hygiene; timely correction of deleterious oral habits; early prevention of childhood caries, such as the use of fluoride, gutter closure, etc., to create an oral functional environment conducive to children’s health and to maintain normal growth and development of children.
References
Lin, M. et al. Prevalence of malocclusion in Chinese schoolchildren from 1991 to 2018: a systematic review and meta-analysis. Int. J. Paediatr. Dent. 30, 144–155 (2020).
Fu, M. et al. The prevalence of malocclusion in China-an investigation of 25,392 children. Zhonghua Kou Qiang Yi Xue Za Zhi 37, 371–373 (2002).
Zhao, Z. Orthodontics 7th edn, (People’s Medical Publishing House, 2020).
Biondi, M. & Picardi, A. Temporomandibular joint pain-dysfunction syndrome and bruxism: etiopathogenesis and treatment from a psychosomatic integrative viewpoint. Psychother. Psychosom. 59, 84–98 (1993).
Khayat, N. et al. The prevalence of temporomandibular disorders and dental attrition levels in patients with posterior crossbite and/or deep bite: a preliminary prospective study. Pain. Res. Manag. 2021, 8827895 (2021).
Liu, X. et al. Dental malocclusion stimulates neuromuscular circuits associated with temporomandibular disorders. Eur. J. Oral. Sci. 126, 466–475 (2018).
Celić, R., Jerolimov, V. & Pandurić, J. A study of the influence of occlusal factors and parafunctional habits on the prevalence of signs and symptoms of TMD. Int. J. Prosthodont. 15, 43–48 (2002).
D’Attilio, M. et al. Modification of condyle anatomy following a monolateral bite rise: a histological study in rat. Int. J. Immunopathol. Pharmacol. 20, 43–47 (2007).
Hirose, M. et al. Three-dimensional finite-element model of the human temporomandibular joint disc during prolonged clenching. Eur. J. Oral. Sci. 114, 441–448 (2006).
Al-Moraissi, E. A., Perez, D. & Ellis, E. 3rd Do patients with malocclusion have a higher prevalence of temporomandibular disorders than controls both before and after orthognathic surgery? A systematic review and meta-analysis. J. Craniomaxillofac. Surg. 45, 1716–1723 (2017).
Abrahamsson, C. et al. TMD before and after correction of dentofacial deformities by orthodontic and orthognathic treatment. Int. J. Oral. Maxillofac. Surg. 42, 752–758 (2013).
Maspero, C. et al. Atypical swallowing: a review. Minerva Stomatol. 63, 217–227 (2014).
Ekprachayakoon, I. et al. New application of dynamic magnetic resonance imaging for the assessment of deglutitive tongue movement. Prog. Orthod. 19, 45 (2018).
Sasaki, Y. et al. Relationship between dental occlusion and maximum tongue pressure in preschool children aged 4–6 years. Children 9, 141 (2022).
Partal, I. & Aksu, M. Changes in lips, cheeks and tongue pressures after upper incisor protrusion in Class II division 2 malocclusion: a prospective study. Prog. Orthod. 18, 29 (2017).
Hutchinson, E. F., Kieser, J. A. & Kramer, B. Morphometric growth relationships of the immature human mandible and tongue. Eur. J. Oral. Sci. 122, 181–189 (2014).
Gokce, S. M. et al. Relationship between Class III malocclusion and hyoid bone displacement during swallowing: a cine-magnetic resonance imaging study. Korean J. Orthod. 42, 190–200 (2012).
Gallerano, G., Ruoppolo, G. & Silvestri, A. Myofunctional and speech rehabilitation after orthodontic-surgical treatment of dento-maxillofacial dysgnathia. Prog. Orthod. 13, 57–68 (2012).
Doshi, U. H. & Bhad-Patil, W. A. Speech defect and orthodontics: a contemporary review. Orthodontics 12, 340–353 (2011).
Laitinen, J., Ranta, R., Pulkkinen, J. & Haapanen, M. L. Associations between dental occlusion and misarticulations of Finnish dental consonants in cleft lip/palate children. Eur. J. Oral. Sci. 107, 109–113 (1999).
Vallino, L. D. Speech, velopharyngeal function, and hearing before and after orthognathic surgery. J. Oral. Maxillofac. Surg. 48, 1274–1281 (1990).
Hu, W., Zhou, Y. & Fu, M. Effect of skeletal Class III malocclusion on speech articulation. Zhonghua Kou Qiang Yi Xue Za Zhi 32, 344–346 (1997).
Xue, S. A., Lam, C. W., Whitehill, T. L. & Samman, N. Effects of Class III malocclusion on young male adults’ vocal tract development: a pilot study. J. Oral. Maxillofac. Surg. 69, 845–852 (2011).
Häggman-Henrikson, B. & Eriksson, P. O. Head movements during chewing: relation to size and texture of bolus. J. Dent. Res. 83, 864–868 (2004).
Henrikson, T., Ekberg, E. C. & Nilner, M. Masticatory efficiency and ability in relation to occlusion and mandibular dysfunction in girls. Int. J. Prosthodont. 11, 125–132 (1998).
Abrahamsson, C., Henrikson, T., Bondemark, L. & Ekberg, E. Masticatory function in patients with dentofacial deformities before and after orthognathic treatment-a prospective, longitudinal, and controlled study. Eur. J. Orthod. 37, 67–72 (2015).
Alsulaiman, A. A. et al. Incisor malalignment and the risk of periodontal disease progression. Am. J. Orthod. Dentofac. Orthop. 153, 512–522 (2018).
Bernhardt, O. et al. New insights in the link between malocclusion and periodontal disease. J. Clin. Periodontol. 46, 144–159 (2019).
Liu, X. et al. The prevalence of gingivitis and related risk factors in schoolchildren aged 6-12 years old. BMC Oral. Health 22, 623 (2022).
Jiang, M. et al. Study on the role of pyroptosis in bone resorption induced by occlusal trauma with or without periodontitis. J. Periodontal Res. 57, 448–460 (2022).
Inchingolo, A. D. et al. Correlation between occlusal trauma and oral microbiota: a microbiological investigation. J. Biol. Regul. Homeost. Agents 35, 295–302 (2021).
Yaman Dosdogru, E. et al. Maxillary incisor trauma in patients with class II division 1 dental malocclusion: associated factors. J. Istanb. Univ. Fac. Dent. 51, 34–41 (2017).
Dua, R. & Sharma, S. Prevalence, causes, and correlates of traumatic dental injuries among seven-to-twelve-year-old school children in Dera Bassi. Contemp. Clin. Dent. 3, 38–41 (2012).
Thiruvenkatachari, B., Harrison, J., Worthington, H. & O’Brien, K. Early orthodontic treatment for Class II malocclusion reduces the chance of incisal trauma: results of a Cochrane systematic review. Am. J. Orthod. Dentofac. Orthop. 148, 47–59 (2015).
Arraj, G. P., Rossi-Fedele, G. & Doğramacı, E. J. The association of overjet size and traumatic dental injuries-a systematic review and meta-analysis. Dent. Traumatol. 35, 217–232 (2019).
Primo-Miranda, E. F. et al. Association between occlusal characteristics and the occurrence of dental trauma in preschool children: a case-control study. Dent. Traumatol. 35, 95–100 (2019).
Mostafa, N. Z., McCullagh, A. P. G. & Kennedy, D. B. Management of a Class I malocclusion with traumatically avulsed maxillary central and lateral incisors. Angle Orthod. 89, 661–671 (2019).
da Silva, R. M. et al. Association between malocclusion and the severity of dental trauma in primary teeth. Dent. Traumatol. 37, 275–281 (2021).
Baccetti, T. et al. Diagnostic performance of increased overjet in Class II division 1 malocclusion and incisor trauma. Prog. Orthod. 11, 145–150 (2010).
Sollenius, O. et al. Three-dimensional evaluation of forced unilateral posterior crossbite correction in the mixed dentition: a randomized controlled trial. Eur. J. Orthod. 42, 415–425 (2020).
Bukhari, A. et al. Dimensional changes in the palate associated with slow maxillary expansion for early treatment of posterior crossbite. Angle Orthod. 88, 390–396 (2018).
Togawa, R. et al. Gastroesophageal reflux symptoms in adults with skeletal Class III malocclusion examined by questionnaires. Am. J. Orthod. Dentofac. Orthop. 136, 10.e11–16 (2009).
Hansen, C., Markström, A. & Sonnesen, L. Specific dento-craniofacial characteristics in non-syndromic children can predispose to sleep-disordered breathing. Acta Paediatr. 111, 473–477 (2022).
Kilpeläinen, P. V., Phillips, C. & Tulloch, J. F. Anterior tooth position and motivation for early treatment. Angle Orthod. 63, 171–174 (1993).
Tristão, S. et al. Is there a relationship between malocclusion and bullying? A systematic review. Prog. Orthod. 21, 26 (2020).
Ramos, I. T. M. et al. Correlation between malocclusion and history of bullying in vulnerable adolescents. Angle Orthod. 92, 677–682 (2022).
Proffit, W. R., Fields, H., Larson, B. E., & Sarver, D. M. Contemporary Orthodontics 6 edn, 130–167 (Mosby, 2018).
Sabuncuoglu, O. Understanding the relationships between breastfeeding, malocclusion, ADHD, sleep-disordered breathing and traumatic dental injuries. Med. Hypotheses 80, 315–320 (2013).
Bjork, A. & Skeller, V. Postnatal growth and development of the maxillary complex. (Center for Human Growth/Dev, University of Michigan, 1976).
Küchler, E. C. et al. Potential interactions among single nucleotide polymorphisms in bone- and cartilage-related genes in skeletal malocclusions. Orthod. Craniofac. Res. 24, 277–287 (2021).
Zohud, O. et al. Towards genetic dissection of skeletal class III malocclusion: a review of genetic variations underlying the phenotype in humans and future directions. J. Clin. Med. 12, 3212 (2023).
Xue, F., Wong, R. W. & Rabie, A. B. Genes, genetics, and Class III malocclusion. Orthod. Craniofac. Res. 13, 69–74 (2010).
Gershater, E. et al. Genes and pathways associated with skeletal sagittal malocclusions: a systematic review. Int. J. Mol. Sci. 22, 13037 (2021).
Graber, L. W., Katherine, W. L. V., Greg, J. H. & Fleming, P. S. Orthodontics: Current Principles and Techniques 7 edn, 992 (Elsevier, 2022).
Dehesa-Santos, A., Iber-Diaz, P. & Iglesias-Linares, A. Genetic factors contributing to skeletal class III malocclusion: a systematic review and meta-analysis. Clin. Oral. Investig. 25, 1587–1612 (2021).
Wang, X., Feng, X. & Li, Z. The Fourth National Oral Health Epidemiological Survey Report (People’s Medical Publishing House Co. Ltd, 2018).
Zou, J. et al. Common dental diseases in children and malocclusion. Int. J. Oral. Sci. 10, 7 (2018).
Souza, M. A., Soares Junior, L. A., Santos, M. A. & Vaisbich, M. H. Dental abnormalities and oral health in patients with Hypophosphatemic rickets. Clinics 65, 1023–1026 (2010).
Ronay, V., Miner, R. M., Will, L. A. & Arai, K. Mandibular arch form: the relationship between dental and basal anatomy. Am. J. Orthod. Dentofac. Orthop. 134, 430–438 (2008).
Braun, S., Hnat, W. P., Fender, D. E. & Legan, H. L. The form of the human dental arch. Angle Orthod. 68, 29–36 (1998).
Paolantonio, E. G. et al. Association between oral habits, mouth breathing and malocclusion in Italian preschoolers. Eur. J. Paediatr. Dent. 20, 204–208 (2019).
Doğramacı, E. J. & Rossi-Fedele, G. Establishing the association between nonnutritive sucking behavior and malocclusions: A systematic review and meta-analysis. J. Am. Dent. Assoc. 147, 926–934.e926 (2016).
Bishara, S. E., Warren, J. J., Broffitt, B. & Levy, S. M. Changes in the prevalence of nonnutritive sucking patterns in the first 8 years of life. Am. J. Orthod. Dentofac. Orthop. 130, 31–36 (2006).
Schmid, K. M. et al. The effect of pacifier sucking on orofacial structures: a systematic literature review. Prog. Orthod. 19, 8 (2018).
Warren, J. J. et al. Effects of nonnutritive sucking habits on occlusal characteristics in the mixed dentition. Pediatr. Dent. 27, 445–450 (2005).
Agarwal, S. S. et al. Association between breastfeeding duration, non-nutritive sucking habits and dental arch dimensions in deciduous dentition: a cross-sectional study. Prog. Orthod. 15, 59 (2014).
Matsumoto, H. et al. Real-Time Continuous Monitoring of Oral Soft Tissue Pressure with a Wireless Mouthguard Device for Assessing Tongue Thrusting Habits. Sensors 23, 5027 (2023).
Kieser, J. A. et al. The role of oral soft tissues in swallowing function: what can tongue pressure tell us? Aust. Dent. J. 59, 155–161 (2014).
Giannini, L., Galbiati, G., Cressoni, P. & Esposito, L. Bad oral habits: a review of the literature. J. Biol. Regul. Homeost. Agents 35, 403–406 (2021).
Majorana, A. et al. Timetable for oral prevention in childhood-developing dentition and oral habits: a current opinion. Prog. Orthod. 16, 39 (2015).
Keski-Nisula, K. et al. Orthodontic intervention in the early mixed dentition: a prospective, controlled study on the effects of the eruption guidance appliance. Am. J. Orthod. Dentofac. Orthop. 133, 254–260 (2008). quiz 328.e252.
Bahreman, A. Early Age Orthodontic Treatment 1 edn, (Quintessence Publishing, 2013).
Musich, D. & Busch, M. J. Early orthodontic treatment: current clinical perspectives. Alpha Omega. 100, 17–24 (2007).
Milani, R. S., De Perière, D. D., Lapeyre, L. & Pourreyron, L. Relationship between dental occlusion and posture. Cranio 18, 127–134 (2000).
Andrew, T. W., Morbia, R. & Lorenz, H. P. Pediatric facial trauma. Clin. Plast. Surg. 46, 239–247 (2019).
Chandra, S. R. & Zemplenyi, K. S. Issues in pediatric craniofacial trauma. Facial Plast. Surg. Clin. North Am. 25, 581–591 (2017).
Grippaudo, C. et al. Early orthodontic treatment: a new index to assess the risk of malocclusion in primary dentition. Eur. J. Paediatr. Dent. 15, 401–406 (2014).
Alyahya, A. et al. Mandibular condylar fracture: a systematic review of systematic reviews and a proposed algorithm for management. Br. J. Oral. Maxillofac. Surg. 58, 625–631 (2020).
Khiabani, K., Zinhaghayegh, B. & Amirzade-Iranaq, M. H. Does dynamic intermaxillary fixation with elastics improve outcomes following unilateral condylar fracture? J. Oral. Maxillofac. Surg. 79, 192–199 (2021).
Dos Santos, C. C. O. et al. Spontaneous changes in mandibular incisor crowding from mixed to permanent dentition: a systematic review. Prog. Orthod. 24, 15 (2023).
Araújo, C. et al. Should midline diastema in mixed dentition be an aesthetic concern? Orthod. Craniofac. Res. 26, 331–337 (2023).
Carneiro, D. P. A. et al. Esthetic impact of maxillary midline diastema and mandibular crowding in children in the mixed dentition. Am. J. Orthod. Dentofac. Orthop. 161, 390–395 (2022).
Chaves, P. R. B., Karam, A. M. & Machado, A. W. Does the presence of maxillary midline diastema influence the perception of dentofacial esthetics in video analysis? Angle Orthod. 91, 54–60 (2021).
Nuvvula, S. et al. Etiological factors of the midline diastema in children: a systematic review. Int. J. Gen. Med. 14, 2397–2405 (2021).
Grippaudo, M. M. et al. Orthodontic treatment need and timing: assessment of evolutive malocclusion conditions and associated risk factors. Eur. J. Paediatr. Dent. 21, 203–208 (2020).
McNamara, J. A. Jr & Franchi, L. The cervical vertebral maturation method: a user’s guide. Angle Orthod. 88, 133–143 (2018).
Baccetti, T., Franchi, L. & McNamara, J. A. Jr An improved version of the cervical vertebral maturation (CVM) method for the assessment of mandibular growth. Angle Orthod. 72, 316–323 (2002).
Cericato, G. O., Bittencourt, M. A. & Paranhos, L. R. Validity of the assessment method of skeletal maturation by cervical vertebrae: a systematic review and meta-analysis. Dentomaxillofac. Radiol. 44, 20140270 (2015).
Daley, R., Hill, M. & Chitty, L. S. Non-invasive prenatal diagnosis: progress and potential. Arch. Dis. Child. Fetal Neonatal Ed. 99, F426–F430 (2014).
Levy, B. & Wapner, R. Prenatal diagnosis by chromosomal microarray analysis. Fertil. Steril. 109, 201–212 (2018).
Nishimura, G. et al. Prenatal diagnosis of bone dysplasias. Br. J. Radiol. 96, 20221025 (2023).
Gaunt, T. Prenatal imaging advances: physiology and function to motion correction and AI-introductory editorial. Br. J. Radiol. 96, 0 (2023).
Lim, K. M. X., Mahyuddin, A. P., Gosavi, A. T. & Choolani, M. Genetics in prenatal diagnosis. Singap. Med. J. 64, 27–36 (2023).
Grosse, S. D. et al. Population screening for genetic disorders in the 21st century: evidence, economics, and ethics. Public Health Genom. 13, 106–115 (2010).
Pan, Z. et al. Treacher Collins syndrome: clinical report and retrospective analysis of Chinese patients. Mol. Genet. Genom. Med. 9, e1573 (2021).
Hermont, A. P. et al. Breastfeeding, bottle feeding practices and malocclusion in the primary dentition: a systematic review of cohort studies. Int. J. Environ. Res. Public Health 12, 3133–3151 (2015).
Narbutytė, I., Narbutytė, A. & Linkevičienė, L. Relationship between breastfeeding, bottle-feeding and development of malocclusion. Stomatologija 15, 67–72 (2013).
Abate, A. et al. Relationship between breastfeeding and malocclusion: a systematic review of the literature. Nutrients 12, 3688 (2020).
Borrie, F. R., Bearn, D. R., Innes, N. P. & Iheozor-Ejiofor, Z. Interventions for the cessation of non-nutritive sucking habits in children. Cochrane Database Syst. Rev. 2015, Cd008694 (2015).
Melink, S., Vagner, M. V., Hocevar-Boltezar, I. & Ovsenik, M. Posterior crossbite in the deciduous dentition period, its relation with sucking habits, irregular orofacial functions, and otolaryngological findings. Am. J. Orthod. Dentofac. Orthop. 138, 32–40 (2010).
Flores, M. T. & Onetto, J. E. How does orofacial trauma in children affect the developing dentition? Long-term treatment and associated complications. Dent. Traumatol. 35, 312–323 (2019).
Nowak, A. J., Christensen, J. R., Mabry, T. R., Townsend, J. A. & Wells, M. H. Pediatric Dentistry 6 edn, 394–398 (Saunders, 2019).
Flores, M. T. & Onetto, J. E. How does orofacial trauma in children affect the developing dentition? Long-term treatment and associated complications. J. Endod. 45, S1–S12 (2019).
Al-Mozany, S. A. et al. A novel method for treatment of Class III malocclusion in growing patients. Prog. Orthod. 18, 40 (2017).
Liu, Y. et al. Relative effectiveness of facemask therapy with alternate maxillary expansion and constriction in the early treatment of Class III malocclusion. Am. J. Orthod. Dentofac. Orthop. 159, 321–332 (2021).
Lin, Y. et al. Stability of maxillary protraction therapy in children with Class III malocclusion: a systematic review and meta-analysis. Clin. Oral. Investig. 22, 2639–2652 (2018).
Liu, W., Zhou, S., Yen, E. & Zou, B. Comparison of changes in the nasal cavity, pharyngeal airway, and maxillary sinus volumes after expansion and maxillary protraction with two protocols: Rapid palatal expansion versus alternate rapid maxillary expansion and constriction. Korean J. Orthod. 53, 175–184 (2023).
Ball, R. L., Miner, R. M., Will, L. A. & Arai, K. Comparison of dental and apical base arch forms in Class II Division 1 and Class I malocclusions. Am. J. Orthod. Dentofac. Orthop. 138, 41–50 (2010).
Naoumova, J., Kurol, J. & Kjellberg, H. A systematic review of the interceptive treatment of palatally displaced maxillary canines. Eur. J. Orthod. 33, 143–149 (2011).
Baccetti, T., Mucedero, M., Leonardi, M. & Cozza, P. Interceptive treatment of palatal impaction of maxillary canines with rapid maxillary expansion: a randomized clinical trial. Am. J. Orthod. Dentofac. Orthop. 136, 657–661 (2009).
Benson, P. E. et al. Interventions for promoting the eruption of palatally displaced permanent canine teeth, without the need for surgical exposure, in children aged 9 to 14 years. Cochrane Database Syst. Rev. 12, Cd012851 (2021).
Leonardi, M., Armi, P., Franchi, L. & Baccetti, T. Two interceptive approaches to palatally displaced canines: a prospective longitudinal study. Angle Orthod. 74, 581–586 (2004).
Bedoya, M. M. & Park, J. H. A review of the diagnosis and management of impacted maxillary canines. J. Am. Dent. Assoc. 140, 1485–1493 (2009).
Christensen, R. T. et al. The effects of primary canine loss on permanent lower dental midline stability. Pediatr. Dent. 40, 279–284 (2018).
Ericson, S. & Kurol, J. Early treatment of palatally erupting maxillary canines by extraction of the primary canines. Eur. J. Orthod. 10, 283–295 (1988).
Almasoud, N. N. Extraction of primary canines for interceptive orthodontic treatment of palatally displaced permanent canines: A systematic review. Angle Orthod. 87, 878–885 (2017).
Sigler, L. M., Baccetti, T. & McNamara, J. A. Jr Effect of rapid maxillary expansion and transpalatal arch treatment associated with deciduous canine extraction on the eruption of palatally displaced canines: a 2-center prospective study. Am. J. Orthod. Dentofac. Orthop. 139, e235–e244 (2011).
Limme, M. The need of efficient chewing function in young children as prevention of dental malposition and malocclusion. Arch. Pediatr. 17, S213–S219 (2010).
Ciftci, V., Uguz, H. N. & Ozcan, M. Laser-assisted management of ectopic eruption of permanent incisors. Niger. J. Clin. Pract. 22, 276–280 (2019).
Crawford, L. B. Impacted maxillary central incisor in mixed dentition treatment. Am. J. Orthod. Dentofac. Orthop. 112, 1–7 (1997).
Kupietzky, A. Clinical technique: removable appliance therapy for space maintenance following early loss of primary molars. Eur. Arch. Paediatr. Dent. 8, 30–34 (2007).
Holan, G. & Needleman, H. L. Premature loss of primary anterior teeth due to trauma-potential short- and long-term sequelae. Dent. Traumatol. 30, 100–106 (2014).
Nadelman, P. et al. Premature loss of primary anterior teeth and its consequences to primary dental arch and speech pattern: A systematic review and meta-analysis. Int. J. Paediatr. Dent. 30, 687–712 (2020).
Kupietzky, A. & Tal, E. The transpalatal arch: an alternative to the Nance appliance for space maintenance. Pediatr. Dent. 29, 235–238 (2007).
Baccetti, T., Franchi, L., Cameron, C. G. & McNamara, J. A. Jr Treatment timing for rapid maxillary expansion. Angle Orthod. 71, 343–350 (2001).
Nimkarn, Y., Miles, P. G., O’Reilly, M. T. & Weyant, R. J. The validity of maxillary expansion indices. Angle Orthod. 65, 321–326 (1995).
Sari, Z., Uysal, T., Usumez, S. & Basciftci, F. A. Rapid maxillary expansion. Is it better in the mixed or in the permanent dentition? Angle Orthod. 73, 654–661 (2003).
Grassia, V. et al. Comparison between rapid and mixed maxillary expansion through an assessment of arch changes on dental casts. Prog. Orthod. 16, 20 (2015).
Bishara, S. E., Jakobsen, J. R., Treder, J. & Nowak, A. Arch width changes from 6 weeks to 45 years of age. Am. J. Orthod. Dentofac. Orthop. 111, 401–409 (1997).
Rodríguez-Olivos, L. H. G. et al. Deleterious oral habits related to vertical, transverse and sagittal dental malocclusion in pediatric patients. BMC Oral. Health 22, 88 (2022).
Abreu, L. G., Paiva, S. M., Pordeus, I. A. & Martins, C. C. Breastfeeding, bottle feeding and risk of malocclusion in mixed and permanent dentitions: a systematic review. Braz. Oral Res. 30, e22 (2016).
Paglia, L. Interceptive orthodontics: awareness and prevention is the first cure. Eur. J. Paediatr. Dent. 24, 5 (2023).
Zhao, T. & He, H. Pediatric mouth breathing and malocclusion. Zhong Hua Kou Qiang Zheng Ji Xue 26, 195–198 (2019).
Koletsi, D., Makou, M. & Pandis, N. Effect of orthodontic management and orofacial muscle training protocols on the correction of myofunctional and myoskeletal problems in developing dentition. A systematic review and meta-analysis. Orthod. Craniofac. Res. 21, 202–215 (2018).
DiBiase, A. T., Cobourne, M. T. & Lee, R. T. The use of functional appliances in contemporary orthodontic practice. Br. Dent. J. 218, 123–128 (2015).
Cozza, P. et al. Mandibular changes produced by functional appliances in Class II malocclusion: a systematic review. Am. J. Orthod. Dentofac. Orthop. 129, 599.e591–512 (2006).
Zhao, T., Hua, F. & He, H. Rapid maxillary expansion may increase the upper airway volume of growing patients with maxillary transverse deficiency. J. Evid. Based Dent. Pract. 21, 101579 (2021).
Zhao, T. et al. Effects of Maxillary Skeletal Expansion on Upper Airway Airflow: A Computational Fluid Dynamics Analysis. J. Craniofac. Surg. 31, e6–e10 (2020).
Koka, V. et al. Orofacial myofunctional therapy in obstructive sleep apnea syndrome: a pathophysiological perspective. Medicina 57, 323 (2021).
Van Dyck, C. et al. The effect of orofacial myofunctional treatment in children with anterior open bite and tongue dysfunction: a pilot study. Eur. J. Orthod. 38, 227–234 (2016).
Simsuchin, C., Chen, Y. & Mallineni, S. K. Clinical effectiveness of vestibular shields in orthodontic treatment: a scoping review. Children 10, 16 (2022).
Di Vecchio, S., Manzini, P., Candida, E. & Gargari, M. Froggy mouth: a new myofunctional approach to atypical swallowing. Eur. J. Paediatr. Dent. 20, 33–37 (2019).
Quinzi, V. et al. Short-term effects of a myofunctional appliance on atypical swallowing and lip strength: a prospective study. J. Clin. Med. 9, 2652 (2020).
Taslan, S., Biren, S. & Ceylanoglu, C. Tongue pressure changes before, during and after crib appliance therapy. Angle Orthod. 80, 533–539 (2010).
Chen, L. R. et al. Evaluation of skeletal and dentoalveolar changes in class II division I pediatric patients receiving myofunctional appliance therapy: A preliminary study. J. Formos. Med. Assoc. 121, 2028–2034 (2022).
Mohammed, H., Čirgić, E., Rizk, M. Z. & Vandevska-Radunovic, V. Effectiveness of prefabricated myofunctional appliances in the treatment of Class II division 1 malocclusion: a systematic review. Eur. J. Orthod. 42, 125–134 (2020).
Wishney, M., Darendeliler, M. A. & Dalci, O. Myofunctional therapy and prefabricated functional appliances: an overview of the history and evidence. Aust. Dent. J. 64, 135–144 (2019).
Hua, F. et al. Effects of adenotonsillectomy on the growth of children with obstructive sleep apnoea-hypopnea syndrome (OSAHS): protocol for a systematic review. BMJ Open 9, e030866 (2019).
Björk, A. The use of metallic implants in the study of facial growth in children: method and application. Am. J. Phys. Anthropol. 29, 243–254 (1968).
Bondemark, L. & Tsiopa, J. Prevalence of ectopic eruption, impaction, retention and agenesis of the permanent second molar. Angle Orthod. 77, 773–778 (2007).
Ngan, P., Alkire, R. G. & Fields, H. Jr. Management of space problems in the primary and mixed dentitions. J. Am. Dent. Assoc. 130, 1330–1339 (1999).
Acknowledgements
The study was supported by the National Natural Science Foundation of China (82171001, 82222015), Research Funding from West China School/Hospital of Stomatology Sichuan University (RCDWJS2023-1), and Align Technology Specialized Scientific Research Fund (21H0922).
Author information
Authors and Affiliations
Contributions
Conceptualization and Investigation, C.C.Z.; Supervision, X.B.L. and S.J.Z.; Original draft, C.C.Z., P.P.D. and H.H.; Review and editing, J.L.S., M.H, Y.H.L., Y.L., J.G., F.J., Y.C., L.Y.J., Q.S.Y., M.Z., B.Z.J., W.H.R, X.Y., H.L., R.Z., Y.L.T., L.G., R.S., J.W.C., and R.K.L.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Zhou, C., Duan, P., He, H. et al. Expert consensus on pediatric orthodontic therapies of malocclusions in children. Int J Oral Sci 16, 32 (2024). https://doi.org/10.1038/s41368-024-00299-8
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41368-024-00299-8