Abstract
Background
Glucagon-like peptide-1 (GLP-1) analogs are approved for the treatment of obesity in adults and adolescents. Reports have emerged that the weight loss effect of these medications may be related to changes in food preferences and ingestive behaviors following the treatment. Understanding the mechanisms which impact ingestive behavior could expand opportunities to develop more refined and personalized treatment options for obesity.
Methods
Recent studies investigating the relationship between GLP-1 analogs and ingestive behaviors were retrieved from PubMed using the search terms: “obesity,” “food preference,” “taste,” “ingestive behavior,” “weight loss medication,” “anti-obesity medication,” “GLP-1 analog,” “tirzepatide,” “liraglutide,” “semaglutide.” Measurement tools were studied to compare variables used to assess food intake behavior. The main outcomes from each study were analyzed to evaluate the current standing and future directions of appetitive, ingestive, and consummatory behaviors and their association with GLP-1 analogs.
Results
Thus far, studies have primarily explored the weight loss phase and report decreased short-term appetite and food intake upon treatment. However, research during the weight maintenance phase and objective measurements of food intake are notably sparse. Additionally, verbal reports have been primarily used to examine food intake, which can be susceptible to subjectivity.
Conclusions
Elucidating the relationship between GLP-1 analogs and ingestive behavior could reveal additional parameters which contribute to their anti-obesity effects. To better understand these mechanisms, it is imperative to consider objective measurements of food intake in future studies. Several measurement tools have been adapted to measure variables of food behavior in humans, and each must be carefully considered with their strengths and limitations to develop optimal investigations.
Similar content being viewed by others
Introduction
Obesity is currently managed through three primary methods: lifestyle changes (e.g., diet modifications), surgical intervention (e.g., gastric bypass, gastric banding, sleeve gastrectomy), and pharmacotherapy using anti-obesity medications. Pharmacological intervention is increasingly utilized due to promising weight loss effects, minimal invasiveness, and sustainability. There are currently seven medications approved for the treatment of obesity: orlistat, naltrexone-bupropion, phentermine-topiramate, setmelanotide, tirzepatide, liraglutide, and semaglutide. In recent years, the latter two, belonging to a class of medications known as glucagon-like-peptide 1 (GLP-1) analogs, are prescribed more frequently. Weight loss efficacy while resulting in relatively few adverse events are major attractions to their use. This prompts further investigation and clarification of the mechanisms promoting weight loss, including their effect on ingestive behavior and food preference. Leveraging this understanding could help refine anti-obesity treatment to benefit clinicians and patients. Therefore, this review focuses on semaglutide and liraglutide and aims to explore current discoveries of their effect on ingestive behavior. We also evaluate the tools and techniques used to study these dimensions, and recommend future directions for further research.
Endogenous GLP-1 is synthesized by L-cells of the distal small intestine and is released in response to carbohydrate consumption. GLP-1 receptors are expressed in the gastrointestinal tract, pancreas, hypothalamus, heart, kidney, and lungs [1, 2]. Acute GLP-1 infusions promote insulin secretion, inhibit glucagon secretion, delay gastric emptying, and promote satiety [3, 4].
Food-intake is a result of behaviors and not a behavior in its own right. Thus, understanding the neurobiological mechanisms that alter behaviors to determine food intake is fundamental to understanding the association between appetitive behaviors and consummatory behaviors. Additionally, it is important to consider food preference as a separate variable which describes a subject’s food choice based on their personal enjoyment and satisfaction. These behaviors can be studied in both humans and animals and can yield important insights that assist clinicians in managing patient expectations when using anti-obesity treatments.
Verbal reports as a means of gathering information on ingestive behaviors are often used [1]; however, verbal report comes with an array of challenges that reduce the validity and reliability of the data obtained. For instance, verbal reporting relies heavily on the participant’s ability to accurately remember the parameters being studied [5]. Additionally, participants could be influenced by a social desirability bias and respond by altering their reports to reflect behaviors that are deemed more socially acceptable [6]. Verbal reports are also subjective by nature and thus participants might perceive and express their experiences differently.
Measuring food-intake directly, without relying on verbal reports, is an objective means of collecting ingestive behavior data, but there are practical challenges. Precise measurements may require the use of expensive devices that are complex to use, while also making long-term data collection particularly difficult. This could add significant cost and complexity to a study. Additionally, the act of directly measuring food intake can be invasive by nature, making subjects feel uncomfortable and subsequently risking the introduction of reactivity bias [7]. Direct observation of ingestive behaviors may also introduce social desirability bias by unintentionally causing participants to alter their normal activity in a conscious or subconscious effort to align with social norms regarding food intake [7].
Overall, while each tool has their associated strength, results obtained from techniques such as verbal reports run a greater risk of subjectivity due to individual interpretation, while direct measurements of food intake are more likely to provide objective and quantifiable data [5, 7].
Due to the prevalence of post-operative weight regain, anti-obesity medications are often prescribed to supplement the effects of bariatric surgery [8]. The link between anti-obesity medications and bariatric surgery, particularly gastric bypass, is strengthened by evidence of gastric bypass increasing gut hormone secretion and activity. Notably, GLP-1 and peptide YY secretion is accelerated upon gastric bypass, both of which are known to play key roles in appetite regulation and hunger reduction [9, 10]. This connection supports the feasibility of using investigations of ingestive behavior following gastric bypass surgery as models for similar studies upon anti-obesity medication treatment.
Previous studies investigating ingestive behaviors after gastric bypass surgery have provided valuable insights into procedure-associated weight loss [5, 11, 12]. While the significantly decreased volume of food consumed by patients leads to decreased caloric intake, gastric bypass surgery also causes notable changes to gut hormone levels [5]. Plasma levels of gut hormones start rising within 15 min of starting a meal and typically peak around 30–90 min. Satiation (resulting in a meal being stopped) occurs much sooner than the peak of the plasma levels. Satiety (resulting in a delay of the onset of the next meal) often continues even after the plasma levels have started to return to baseline. The duration of satiety is associated with the height of the peak of the gut hormones and the duration before the gut hormones return to baseline [13]. These gut hormone changes contribute to reduced hunger and appetitive behavior [5]. Gastric bypass in rodents results in weight loss, reduced food-intake, reduction in preference for sucrose and intralipid during a two-bottle preference test, reduced consumption of fat, with a modest increase in protein intake [11, 12]. Whilst in humans, gastric bypass results in weight loss, reduced food intake, and reduction in rate of eating, but no change in food selection or frequency of eating [14]. However, conclusions regarding changes in food selection after gastric bypass continue to be evasive, with various studies reporting differing results depending on the technique employed [5]. Furthermore, during the weight loss phase in humans, the progressive ratio task (PRT), an operant measurement which requires participants to complete a varying amount of tasks to receive a reward, shows a reduction in appetitive behavior, whereas in rodents in the weight loss maintenance phase, there are no changes in appetitive behavior [15, 16]. In rodents, taste reactivity as a measure of consummatory behavior shows no change in the palatability of food at the start of the meal, but an increase in aversive behavior is observed when the meal has ended [17].
Appetitive behavior describes the effort the subject is willing to undertake to reach a reward such as food [18]. These responses can include food-seeking behaviors which lead to food consumption and can result in food foraging or food hoarding [18]. Food hoarding as an appetitive behavior has been extensively studied in non-human primates with laboratory animals exhibiting increased hoarding following food deprivation [19]. However, food intake does not necessarily increase, demonstrating a delineation between appetitive and ingestive behavior [19]. When translating this phenomenon to humans, studies of food hoarding and other appetitive behaviors as a result of fasting or food deprivation are relatively limited [10].
Appetitive behavior can be influenced by neuroendocrine mechanisms [18]. Siberian hamsters which were administered neuropeptide Y (NPY) injections to the hypothalamic paraventricular nucleus and perifornical area displayed marked increases in food hoarding, highlighting it as a key regulator of appetitive behavior [20]. Ghrelin, a hormone stimulating gastric emptying and appetite, increases upon fasting in animals such as hamsters [21]. Ghrelin injections in hamsters stimulate long-term food hoarding, highlighting a major neurochemical factor in appetitive behavior [22]. Moreover, studies conducted on gerbils have shown food hoarding to increase activation of cells containing tyrosine hydroxylase, which catalyzes rate-limited dopamine synthesis, in subcortical regions of the brain [18]. This suggests an element of reward and reinforcement driving appetitive behavior [18].
The PRT is a direct measure of appetitive behavior [15]. This technique is widely used to investigate the hedonic value reinforcers in animal models which can answer the question of how hard a subject is willing to work for a given reinforcer [23,24,25,26]. The method was built on previous studies that used PRTs in humans [27,28,29,30,31,32,33]. One of the key merits of the task is that the assessment is based on the actual behavior of the subject and is not burdened by the interpretive limitations associated with scaling procedures using verbal reports. The PRT uses simple computer software and requires participants to consume the reinforcer during the task rather than at the end. Thus, appetitive responsiveness is determined directly by the orosensory properties (e.g., taste) of the reward and is independent of the association between a stimulus such as a token, money, or images with the reward. The completion of the task is not dependent on the technological or intellectual skills of the participant. To minimize post-ingestive effects, reinforcers are of minimal volume and calories so that the ingestion of a food reward may not lead to premature satiety and interfere with the oral-based evaluation. This property makes PRT beneficial for studying changes in appetitive responsiveness in patients [5]. Participants are briefed about each experiment by an investigator who is not present during the task to minimize bias in responses. These methodologic features differentiate this paradigm from others used in humans in previous studies [10,11,12,13,14,15,16].
Consummatory behaviors occur when there is direct interaction between the taste buds and food and are thought to be highly regulated by neuroendocrine mechanisms [18]. Ghrelin, in addition to proteins of the hypothalamic-pituitary-adrenal and hypothalamic-pituitary-gonadal axes, has been shown to impact consummatory behavior in laboratory animals [18]. Quantitative studies on consummatory behavior following anti-obesity medication are relatively sparse, requiring further exploration.
When assessing consummatory behavior, it is important to consider the types of food that patients who undergo anti-obesity treatment choose to consume. When evaluating mechanisms of weight loss, sweet and fatty food consumption trends can be particularly informative. Previous works indicate that sugar and fat preferences decreased in rats that underwent gastric bypass surgery [16, 34]. These results have not been replicated in humans undergoing gastric bypass surgery [35]. Furthermore, food selection in the context of anti-obesity medications has not been studied extensively. Therefore, this study aims to shed light on current research regarding the effect of GLP-1 analog pharmacotherapy on food intake and behaviors, their limitations and opportunities to expand, and methods used to assess these dimensions.
Methods
This article reviews studies which shed light on the relationship between GLP-1 analogs and ingestive behaviors, while reviewing measurement tools utilized to obtain results. The following search terms were applied in PubMed to locate relevant articles: obesity, food preference, taste, ingestive behavior, weight loss medication, anti-obesity medication, GLP-1 analog, tirzepatide, liraglutide, semaglutide. Additional filters were applied to obtain studies inclusive of humans and/or rodent subjects. Age and language criteria were not accounted for as search criteria. Studies were included if they were published within the last 25 years to ensure the research is up to date but still ensure there were sufficient resources, given that it is an understudied field. Eligibility was also restricted to articles that discussed GLP-1 analogs and specifically analyzed taste preference along with ingestive behavior following treatment. For the scope of this review, articles which investigated GLP-1 analogs as treatments for obesity were primarily extracted, although their usage is also utilized in the treatment of type 2 diabetes. Titles and abstracts were reviewed for relevance and to determine if the study fit within the eligibility criteria. Articles were ensured to be current and relevant to the timeframe in which the study was conducted (July 2023 – October 2023). Selected articles were downloaded to and managed from Mendeley, which was also used for citation management. The following data were extracted from the studies: study type, year of publication, location of study, study population, methods, and key results. Further terms were then applied, including “universal eating monitor,” “drinkometer,” “visual analog scale,” “Leeds food preference task,” and “control of eating questionnaire” in conjunction with the aforementioned search terms to examine the various methods for assessing ingestive behavior. Relevant studies with both human and animal subjects were extracted and applied. The main outcomes analyzed from each study are the impact of GLP-1 analogs on ingestive behavior, cravings and craving control, and differential effects in the weight loss and weight maintenance phase. The measurement tools used for each outcome were also studied.
Results
In order to shed light on the suggested relationships between GLP-1 analogs, ingestive behavior, and food preference, this review primarily focuses on studies which treated adults with obesity and/or type 2 diabetes with semaglutide and liraglutide, and which recorded measurements of appetitive behavior, consummatory behavior, and food preferences.
Changes in ingestive behavior after treatment with GLP-1 analogs pharmacotherapy
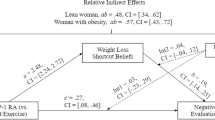
Patients who used the GLP-1 receptor agonist exenatide displayed decreased neuronal responses to pictures of food measured by functional magnetic resonance imaging (fMRI) in parts of the brain that relate to appetite and reward (insula, amygdala, putamen, and orbitofrontal cortex) [36]. The glucagon-like peptide 1 receptor (GLP-1R) analog semaglutide, a once-weekly injectable medication for type 2 diabetes mellitus and obesity [37], targets the circumventricular organs rather than permeating the blood-brain barrier. By binding to GLP-1R in the subcortical areas of the brain, semaglutide has been suggested to potentially affect taste preferences and food intake behaviors via interaction with proopiomelanocortin neurons and cocaine- and amphetamine-regulated transcripts [38].
Patients treated with semaglutide undergo an initial phase of weight loss for 12–18 months followed by a weight stabilization phase [39]. During the initial phase, patients are more likely to experience adverse gastrointestinal side effects such as nausea, vomiting diarrhea, and constipation [40]. However, these effects can be attenuated by starting with lower doses of the medication and gradually titrating to the recommended dose [41]. Semaglutide resulted in reduction of body weight of up to 15% over 12–18 months in adults and adolescents with obesity [40]. The STEP 5 study evaluated semaglutide over 2 years which captured both the initial weight loss and weight-loss maintenance phases [42]. STEP 5 used verbal reports in the form of the Control of Eating Questionnaire to measure changes in appetite compared to a placebo. The group receiving semaglutide verbally reported lower cravings for dairy and starchy foods and less desire to eat salty or spicy foods, along with less difficulty controlling eating and resisting cravings. The initial changes seen during the weight loss phase were attenuated during the weight-loss maintenance phase [42], suggesting that once the patients achieve a new homeostatic fat mass, the biological drive to lose weight diminishes. Without the biological drive to achieve a lower body fat mass, there appears to be no physiological demand for changes to appetitive behaviors.
During the weight loss phase of semaglutide treatment, energy intake substantially decreased [43,44,45,46,47]. Decreased meal size and decreased preference for energy-dense foods are thought to contribute to the reduced energy intake associated with GLP-1R analogs [45] (Table 1). The macronutrient profile of foods selected by individuals taking semaglutide may change as shown in a randomized trial by Blundell et al. [45]. While in the weight loss phase, patients had decreased preference for high-fat, non-sweet foods as directly measured by consumption of an evening ad libitum snack box [45]. Using similar methods, a trial including 15 patients with type 2 diabetes mellitus (T2D) treated with oral semaglutide conducted by Gibbons et al. verbally reported a decreased preference for both high-fat and sweet foods from the snack box [48]. Measures of food preference were determined using data from verbal reports. Contrary to these findings, a cross-over study conducted in 1998 by Näslund et al. found no significant differences in the macronutrient profiles of foods selected by the group administered GLP-1 analog as compared to placebo [43]. Ingestive behavior using direct and objective measures not contingent on verbal reporting has not yet been reported for patients in the weight-loss maintenance phase, which raises the question whether the patients may return to baseline (pre-intervention) food choices.
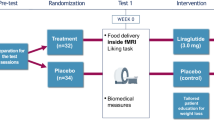
Liraglutide is a once-daily injectable GLP-1 receptor agonist also prescribed for the treatment of type-2 diabetes mellitus and obesity. Liraglutide initially reduces hunger and increases satiety [49]. Liraglutide similarly acts on GLP-1 receptors in the subcortical region of the brain and in the arcuate nucleus. Liraglutide also directly stimulates proopiomelanocortin neurons, and this has been postulated to result in reduced hunger and appetitive behavior [50, 51].
Liraglutide’s effect on slowing gastric emptying has been suggested as an explanation for higher satiety levels and decreased appetitive behavior, albeit the mechanism of this hypothesis has not been demonstrated [44]. Gastrointestinal side effects such as nausea were initially associated with weight loss in the phase 2 studies with liraglutide [52], but this observation was never confirmed, with all subsequent liraglutide studies showing nausea is not associated with weight loss [53].
Effects on food cravings
Five previous studies used verbal reports to show decreased intensity of food cravings as well as a change in the types of foods they crave after GLP-1 analog treatment [43, 45, 47, 48, 54]. Using the Leeds Food Preference Task, the Blundell group found participants taking semaglutide craved a smaller number of foods, with a decrease in the implicit preference for high-fat, non-sweet foods in particular [45]. Gibbons also found semaglutide decreased preference of high-fat, non-sweet foods [48]. Using the forced choice list method, Näslund found GLP-1 analogs reduced craving for foods [43]. Furthermore, Friedrichsen using verbal reports showed the semaglutide group craved sweet, savory, and dairy-containing foods significantly less than the placebo group after 20 weeks of treatment and while in the weight loss phase [47]. Finally, Kadouh, using verbal reports also showed GLP-1R analogs lower preference for sweet, salty, fatty, and savory foods [54]. Ingestive behavior using verbal reports has not yet been reported for patients in the weight-loss maintenance phase, which raises the question again whether the patients may return to baseline (pre-intervention) food choices.
Effects on control of eating
Verbal reports suggest that semaglutide improves short-term control of eating through decreased feelings of hunger associated with increased fullness and decreased severity of food within the first 12–24 weeks over 104-weeks [42]. The effect attenuated between 52 weeks and 104 weeks, but control of eating was still better than baseline.
Differential effects during the weight loss phase and the weight maintenance phase
Semaglutide has a dose-escalating protocol to achieve a chronic maintenance dose. This is done to minimize side effects of the medication like nausea and malaise [55]. Most human studies on ingestive behavior have only focused on the weight loss phase with one exception of a 104-week study which also used verbal reports to describe appetite [42].
Cawthon et al. compared the metabolic, behavioral, and neural consequences of acute and chronic semaglutide administration in rats [56]. They confirmed the reduction in energy intake and loss of fat mass while maintaining lean mass in rats. Ingestive behavior during the weight loss and weight-loss maintenance phase over the span of 42 days was directly measured and showed that meal size and rate of eating had been the main modulators of semaglutide-induced changes in food intake.
In acute dosing protocols in rodents, where GLP-1R analogs were not dose titrated, as is the convention in humans, the drug reduces reward pathways that reinforce sucrose ingestion, thereby decreasing the amount of high-sugar-containing food that the rats consumed before they stopped ingesting calories [56,57,58,59,60,61,62,63,64,65]. When semaglutide was dose-titrated, like what typically happens in humans, the rats reached the weight-stable phase after approximately 10 days [56]. In the weight-stable phase, ingestion of low to mid-range sucrose-containing liquids was increased [56]. Rats consumed more than 2.5 times as much of low to mid sucrose-containing liquids as compared to control groups. Cawthon et al. identify several factors that could possibly explain this phenomenon, including the energy density of the stimuli, the stimuli’s texture (liquid vs. solid), the effects of GLP-1 analogs on taste responses, or changes in neurohormonal responses to the stimuli [56]. In this study, energy density was measured as the amount of energy or calories in a particular weight of food (kcal/g). Foods with lower energy density provide fewer calories per gram than foods with higher energy density which typically contain more fat, refined carbohydrates, and less fiber [66]. A deeper understanding of this and other consequences of chronic dosing schedules of GLP-1R agonizts will provide a more complete understanding of the long-term limitations and benefits of the medication, especially as it pertains to humans.
Measurement tools
Tools to measure ingestive behaviors
From its initial development by Kissilef et al. in 1980, the Universal Eating Monitor (UEM) provided the novel ability to test rates of consumption for solid and liquid foods, thereby considering consistency as a satiating influence [7, 67]. The UEM consists of a plate resting upon a scale which is connected to a computer. The scale tracks the weight of the food, transmitting the information to a computer very frequently throughout the process [5]. This allows for almost continuous monitoring of ingestive behavior, tracking changes in consumption speed throughout the meal, and provides much more information than simply weighing the meal before and after eating occurs [48]. Since its inception, the UEM has been adapted for broader human or animal studies to assess food intake patterns related to GLP-1 analog treatment. Näslund et al. used the tool in 1998 to measure total consumption, duration, eating rate, and relative rate of consumption in humans, which they defined as “food intake during the first half of the meal minus food intake during the second half of the meal divided by total food intake” [43].
Another tool for measuring ingestive behavior is the drinkometer [68]. Originally used to study ingestive behavior after bariatric surgery in humans, the device uses a liquid meal and tracks the volume consumed, length of consumption, number of sucks, and burst (group of sucks) size while the participant is drinking from the device [69].
Most of the human studies done to date relied on verbal reports and used a 100 mm visual analog scale (VAS) to assess satiety and fullness [43, 45,46,47, 54]. This consists of a 100 mm scale where participants mark their answers in response to questions such as “How full do you feel?” and “How much do you think you can eat?” [54]. Although the VAS is less expensive and more readily available for assessing a participant’s feelings of fullness compared to more direct measurement tools such as UEM and the drinkometer, the direct measures of behavior can circumvent the limitations and biases induced by verbal reporting.
Measures of diet composition after use of GLP-1 analogs
Gibbons et al. directly measured behavior by weighing food [48]. Participants with T2D received a snack box containing 100 grams of each of the following four types of food: high-fat, sweet; low-fat, sweet; high-fat, non-sweet; low-fat, non-sweet. The snack boxes were weighed before and after consumption to determine the composition of the food consumed by the participants. The study showed a decreased preference for both high-fat and sweet foods after treatment with GLP-1 analog [48]. The mean energy intake for high-fat sweet foods was 38.8% lower in the semaglutide-treated group than in the placebo group. Overall high-fat food intake was 40.8% lower in the oral semaglutide group when compared to the placebo group. Both variables represented statistically significant differences.
Measures of food preference
Blundell et al. used verbal reports and the Leeds Food Preference Task (LFPT) to examine changes in the choice of diet composition of adult humans with obesity and without diabetes [45]. The authors measured both explicit liking and implicit wanting of certain types of food using photos of different foods that were either sweet or savory or high-fat or low-fat. In the LFPT, explicit liking is measured by having participants rate how pleasant the food in each photo is to them. To study implicit wanting, the authors employed forced choice. Participants were forced to choose between sets of photos from the four categories based on which they would want the most, with shorter response times corresponding to a stronger desire for the chosen photo. Similarly, Näslund et al. studied food preference of adult humans with obesity through a forced choice approach [43]. Participants had to choose from different groups of foods– high protein, high-fat, high-carbohydrate, and low energy– to determine which they preferred [43, 45]. In their study, Friedrichsen used the Control of Eating Questionnaire (COEQ) to assess different preferences of adult humans with obesity [47]. Finally, Kadouh et al. used a 100 mm VAS to measure preference for fatty, salty, sweet, and savory foods [54]. In a randomized controlled trial, Griffioen-Roose et al. compared the LFPT with other measurements of desire for different foods and sensory-specific satiety [70]. They use three measurements– LFPT, ad libitum intake (measured by giving participants bowls of different types of food and weighing the remaining food in each bowl), and willingness to work, where participants play a computer game and try to get enough points to win food (measured by mouse clicks until the game is stopped). The authors found no difference in results based on the measurement procedure used. LFPT/forced choice and COEQ all rely on verbal reporting, but the willingness to work and ad libitum intake are direct measures of behavior. It was reassuring that no major differences were found between the verbal report measures and the direct measures of behavior [45, 70, 71].
Measures of eating control
Along with preference, the COEQ was used by several researchers [42, 45, 47, 48]. These verbal reports showed that after GLP-1 analog treatment, in all four studies, control of eating became easier.
Discussion
Recent developments have introduced GLP-1 analogs as a highly viable option for the treatment of obesity, representing the newest generation of therapeutic models for weight management. Several studies have aimed to shed light on the mechanisms driving pharmacotherapy-induced weight loss by investigating their impact on ingestive behavior. Altered food preferences, decreased food cravings, and reduced food intake may contribute to long-term weight loss.
However, since the approval of GLP-1R analogs for the treatment of obesity, surprisingly few studies have been done to understand ingestive behavior. Studies are further complicated by the distinct and potentially unrelated natures of food intake (i.e., the consumption of food as a result of behaviors) and food preference (i.e., a subject’s food choices dependent on their preferences and personal enjoyment) as separate and potentially unrelated variables. Very little is known about appetitive behavior and almost nothing is known about consummatory behavior, especially in the weight maintenance phase. The studies done thus far mostly focused on the weight loss phase and predominantly used verbal reporting to understand appetite, cravings, and portion control. Moreover, the tools leveraged by these studies analyze multiple variables of food preference, which is undoubtedly imperative in understanding how they interplay to impact food behaviors. However, it is ultimately crucial to investigate objective measures of food intake to better clarify the effect of anti-obesity medications. Direct measurement of behavior is possible using new equipment which has been validated in the study of gastric bypass surgery. This may provide more reliable results.
While a variety of tools have been repurposed and refined to assess food behaviors, each measurement technique has accompanying limitations to account for. For instance, the UEM provides opportunities for dynamic consumption pattern measurements, but restricts investigators to a single set of food items under a laboratory setting. This not only limits the conditions under which food behavior can be explored, but also introduces a potentially confounding variable of the discomfort which may come with participants eating in a laboratory. The Drinkometer assesses multiple crucial variables of ingestive behavior, but the short duration between sucks and bursts limits opportunities to extract detailed analyses of interval measurements. Moreover, the relatively high expenses associated with the tool present limitations to research. Contrarily, the VAS is less expensive and accessible for most researchers. However, responses from study participants are subject to individual interpretation of scale ratings and introduce an element of subjectivity to acquired results. The LFPT is uniquely able to simultaneously measure explicit liking and implicit wanting of participants, but does not account for variation in food preferences which may present across different times in a day. While the CoEQ can measure food cravings over longer periods of time and is not limited to static points in a given day, this method does not allow for an objective, actual measurement of intake across participants. It is prudent to consider each of these strengths and limitations and accordingly design effective and optimal future investigations (Table 2).
The treatment options for obesity are rapidly improving, and more and better medications will become available. By understanding the behavioral mechanisms which explain how anti-obesity medications impact ingestive behavior, researchers can potentially refine treatment strategies and tailor interventions to individual patients. This may enhance the overall success of obesity management with these medications. With direct measures of ingestive behavior in animals now suggesting that low to mid-range sucrose intake may increase after semaglutide treatment, it is imperative to study ingestive behavior in humans using direct measures. The focus should also be on the weight maintenance phase, because the absence of such information risks the propagation of misinformation and the harboring of unrealistic expectations by both clinicians and patients, which can influence patients’ and clinicians’ willingness to use anti-obesity medications in the future.
References
Seino Y, Fukushima M, Yabe D. GIP and GLP-1, the two incretin hormones: Similarities and differences. J Diabetes Investig. 2010;1:8–23.
Yu M, Benjamin MM, Srinivasan S, Morin EE, Shishatskaya EI, Schwendeman SP, et al. Battle of GLP-1 delivery technologies. Adv Drug Deliv Rev. 2018;130:113–30.
Graaf Cde, Donnelly D, Wootten D, Lau J, Sexton PM, Miller LJ, et al. Glucagon-Like Peptide-1 and Its Class B G Protein-Coupled Receptors: A Long March to Therapeutic Successes. Pharmacol Rev. 2016;68:954–1013.
Ramracheya R, Chapman C, Chibalina M, Dou H, Miranda C, González A, et al. GLP-1 suppresses glucagon secretion in human pancreatic alpha-cells by inhibition of P/Q-type Ca2+ channels. Physiol Rep. 2018;6:e13852.
Mathes CM, Spector AC. Food selection and taste changes in humans after Roux-en-Y gastric bypass surgery: a direct-measures approach. Physiol Behav. 2012;107:476–83.
Nielsen MS, Christensen BJ, Ritz C, Rasmussen S, Hansen TT, Bredie WLP, et al. Roux-En-Y Gastric Bypass and Sleeve Gastrectomy Does Not Affect Food Preferences When Assessed by an Ad libitum Buffet Meal. Obes Surg. 2017;27:2599–605.
Kissileff HR. The Universal Eating Monitor (UEM): objective assessment of food intake behavior in the laboratory setting. Int J Obes. 2022;46:1114–21.
Redmond IP, Shukla AP, Aronne LJ. Use of Weight Loss Medications in Patients after Bariatric Surgery. Curr Obes Rep. 2021;10:81–9.
Holst JJ, Madsbad S, Bojsen-Møller KN, Svane MS, Jørgensen NB, Dirksen C, et al. Mechanisms in bariatric surgery: Gut hormones, diabetes resolution, and weight loss. Surg Obes Rel Dis. 2018;14:708–14.
Karra E, Chandarana K, Batterham RL. The role of peptide YY in appetite regulation and obesity. J Physiol. 2009;587:19–25.
Mathes CM, Letourneau C, Blonde GD, le Roux CW, Spector AC. Roux-en-Y gastric bypass in rats progressively decreases the proportion of fat calories selected from a palatable cafeteria diet. Am J Physiol. 2016;310:R952–9.
le Roux CW, Bueter M, Theis N, Werling M, Ashrafian H, Löwenstein C, et al. Gastric bypass reduces fat intake and preference. Am J Physiol. 2011;301:R1057–66.
Lean MEJ, Malkova D. Altered gut and adipose tissue hormones in overweight and obese individuals: cause or consequence? Int J Obes. 2016;40:622–32.
Livingstone MBE, Redpath T, Naseer F, Boyd A, Martin M, Finlayson G, et al. Food Intake Following Gastric Bypass Surgery: Patients Eat Less but Do Not Eat Differently. J Nutr. 2022;152:2319–32.
Miras AD, Jackson RN, Jackson SN, Goldstone AP, Olbers T, Hackenberg T, et al. Gastric bypass surgery for obesity decreases the reward value of a sweet-fat stimulus as assessed in a progressive ratio task. Am J Clin Nutr. 2012;96:467–73.
Mathes CM, Bohnenkamp RA, Blonde GD, Letourneau C, Corteville C, Bueter M, et al. Gastric bypass in rats does not decrease appetitive behavior towards sweet or fatty fluids despite blunting preferential intake of sugar and fat. Physiol Behav. 2015;142:179–88.
Blonde GD, Mathes CM, Inui T, Hamel EA, Price RK, Livingstone MBE, et al. Oromotor and somatic taste reactivity during sucrose meals reveals internal state and stimulus palatability after gastric bypass in rats. Am J Physiol. 2022;322:R204–18.
Keen-Rhinehart E, Ondek K, Schneider JE. Neuroendocrine regulation of appetitive ingestive behavior. Front Neurosci. 2013;7:213.
Bartness TJ, Keen-Rhinehart E, Dailey MJ, Teubner BJ. Neural and hormonal control of food hoarding. Am J Physiol Regul Integr Comp Physiol. 2011;301:R641–55.
Dailey MJ, Bartness TJ. Appetitive and consummatory ingestive behaviors stimulated by PVH and perifornical area NPY injections. Am J Physiol Regul Integr Comp Physiol. 2009;296:R877–92.
Higgins SC, Gueorguiev M, Korbonits M. Ghrelin, the peripheral hunger hormone. Ann Med. 2007;39:116–36.
Keen-Rhinehart E, Bartness TJ. Peripheral ghrelin injections stimulate food intake, foraging, and food hoarding in Siberian hamsters. Am J Physiol Regul Integr Comp Physiol. 2005;288:R716–22.
Reilly S. Reinforcement value of gustatory stimuli determined by progressive ratio performance. Pharmacol Biochem Behav. 1999;63:301–11.
Hodos W, Kalman G. Effects of increment size and reinforcer volume on progressive ratio performance. J Exp Anal Behav. 1963;6:387–92.
Stafford D, LeSage MG, Glowa JR. Progressive-ratio schedules of drug delivery in the analysis of drug self-administration: a review. Psychopharmacology. 1998;139:169–84.
Richardson NR, Roberts DC. Progressive ratio schedules in drug self-administration studies in rats: a method to evaluate reinforcing efficacy. J Neurosci Methods. 1996;66:1–11.
Lappalainen R, Epstein LH. A behavioral economics analysis of food choice in humans. Appetite. 1990;14:81–93.
Nasser JA, Evans SM, Geliebter A, Pi-Sunyer FX, Foltin RW. Use of an operant task to estimate food reinforcement in adult humans with and without BED. Obesity. 2008;16:1816–20.
Willner P, Benton D, Brown E, Cheeta S, Davies G, Morgan J, et al. “Depression” increases “craving” for sweet rewards in animal and human models of depression and craving. Psychopharmacology. 1998;136:272–83.
Kissileff HR, Nally SJM, Gordon R, Gondek-Brown M, Farkas J, Sclafani A. Measuring food reward value in humans. Appetite. 2007;49:304.
Ouwehand C, de Ridder DTD. Effects of temptation and weight on hedonics and motivation to eat in women. Obesity. 2008;16:1788–93.
Bulik CM, Brinded EC. The effect of food deprivation on the reinforcing value of food and smoking in bulimic and control women. Physiol Behav. 1994;55:665–72.
Cameron JD, Goldfield GS, Cyr MJ, Doucet E. The effects of prolonged caloric restriction leading to weight-loss on food hedonics and reinforcement. Physiol Behav. 2008;94:474–80.
Bueter M, Miras AD, Chichger H, Fenske W, Ghatei MA, Bloom SR, et al. Alterations of sucrose preference after Roux-en-Y gastric bypass. Physiol Behav. 2011;104:709–21.
Spector AC, Kapoor N, Price RK, Pepino MY, Livingstone MBE, Le Roux CW. Proceedings from the 2018 Association for Chemoreception Annual Meeting Symposium: Bariatric Surgery and Its Effects on Taste and Food Selection. Chem Senses. 2019;44:155–63.
van Bloemendaal L, IJzerman RG, Ten Kulve JS, Barkhof F, Konrad RJ, Drent ML, et al. GLP-1 receptor activation modulates appetite- and reward-related brain areas in humans. Diabetes. 2014;63:4186–96.
Chao AM, Tronieri JS, Amaro A, Wadden TA. Semaglutide for the treatment of obesity. Trends Cardiovasc Med. 2023;33:159–66.
Gabery S, Salinas CG, Paulsen SJ, Ahnfelt-Rønne J, Alanentalo T, Baquero AF, et al. Semaglutide lowers body weight in rodents via distributed neural pathways. JCI Insight. 2020;5:e133429.
Garcia de Lucas MD, Miramontes-González JP, Avilés-Bueno B, Jiménez-Millán AI, Rivas-Ruiz F, Pérez-Belmonte LM. Real-world use of once-weekly semaglutide in patients with type 2 diabetes at an outpatient clinic in Spain. Front Endocrinol. 2022;13:995646.
Wilding JPH, Batterham RL, Calanna S, Davies M, Van Gaal LF, Lingvay I, et al. Once-Weekly Semaglutide in Adults with Overweight or Obesity. N Engl J Med. 2021;384:989–1002.
Shiomi M, Takada T, Tanaka Y, Yajima K, Isomoto A, Sakamoto M, et al. Clinical factors associated with the occurrence of nausea and vomiting in type 2 diabetes patients treated with glucagon-like peptide-1 receptor agonists. J Diabetes Investig. 2019;10:408–17.
Wharton S, Batterham RL, Bhatta M, Buscemi S, Christensen LN, Frias JP, et al. Two-year effect of semaglutide 2.4 mg on control of eating in adults with overweight/obesity: STEP 5. Obesity. 2023;31:703–15.
Näslund E, Gutniak M, Skogar S, Rössner S, Hellström PM. Glucagon-like peptide 1 increases the period of postprandial satiety and slows gastric emptying in obese men. Am J Clin Nutr. 1998;68:525–30.
van Can J, Sloth B, Jensen CB, Flint A, Blaak EE, Saris WHM. Effects of the once-daily GLP-1 analog liraglutide on gastric emptying, glycemic parameters, appetite and energy metabolism in obese, non-diabetic adults. Int J Obes. 2014;38:784–93.
Blundell J, Finlayson G, Axelsen M, Flint A, Gibbons C, Kvist T, et al. Effects of once-weekly semaglutide on appetite, energy intake, control of eating, food preference and body weight in subjects with obesity. Diabetes Obes Metab. 2017;19:1242–51.
Tronieri JS, Wadden TA, Walsh O, Berkowitz RI, Alamuddin N, Gruber K, et al. Effects of liraglutide on appetite, food preoccupation, and food liking: results of a randomized controlled trial. Int J Obes. 2020;44:353–61.
Friedrichsen M, Breitschaft A, Tadayon S, Wizert A, Skovgaard D. The effect of semaglutide 2.4 mg once weekly on energy intake, appetite, control of eating, and gastric emptying in adults with obesity. Diabetes Obes Metab. 2021;23:754–62.
Gibbons C, Blundell J, Tetens Hoff S, Dahl K, Bauer R, Baekdal T. Effects of oral semaglutide on energy intake, food preference, appetite, control of eating and body weight in subjects with type 2 diabetes. Diabetes Obes Metab. 2021;23:581–8.
Rubino DM, Greenway FL, Khalid U, O’Neil PM, Rosenstock J, Sørrig R, et al. Effect of Weekly Subcutaneous Semaglutide vs Daily Liraglutide on Body Weight in Adults With Overweight or Obesity Without Diabetes: The STEP 8 Randomized Clinical Trial. JAMA. 2022;327:138–50.
Secher A, Jelsing J, Baquero AF, Hecksher-Sørensen J, Cowley MA, Dalbøge LS, et al. The arcuate nucleus mediates GLP-1 receptor agonist liraglutide-dependent weight loss. J Clin Invest. 2014;124:4473–88.
Holst JJ. The physiology of glucagon-like peptide 1. Physiol Rev. 2007;87:1409–39.
Armstrong MJ, Gaunt P, Aithal GP, Barton D, Hull D, Parker R, et al. Liraglutide safety and efficacy in patients with non-alcoholic steatohepatitis (LEAN): a multicentre, double-blind, randomised, placebo-controlled phase 2 study. Lancet. 2016;387:679–90.
Pi-Sunyer X, Astrup A, Fujioka K, Greenway F, Halpern A, Krempf M, et al. A Randomized, Controlled Trial of 3.0 mg of Liraglutide in Weight Management. N Engl J Med. 2015;373:11–22.
Kadouh H, Chedid V, Halawi H, Burton DD, Clark MM, Khemani D, et al. GLP-1 Analog Modulates Appetite, Taste Preference, Gut Hormones, and Regional Body Fat Stores in Adults with Obesity. J Clin Endocrinol Metab. 2020;105:1552–63.
Wharton S, Calanna S, Davies M, Dicker D, Goldman B, Lingvay I, et al. Gastrointestinal tolerability of once-weekly semaglutide 2.4 mg in adults with overweight or obesity, and the relationship between gastrointestinal adverse events and weight loss. Diabetes Obes Metab. 2022;24:94–105.
Cawthon CR, Blonde GD, Nisi AV, Bloomston HM, Krubitski B, le Roux CW, et al. Chronic Semaglutide Treatment in Rats Leads to Daily Excessive Concentration-Dependent Sucrose Intake. J Endocr Soc. 2023;7:bvad074.
Colvin KJ, Killen HS, Kanter MJ, Halperin MC, Engel L, Currie PJ. Brain Site-Specific Inhibitory Effects of the GLP-1 Analogue Exendin-4 on Alcohol Intake and Operant Responding for Palatable Food. Int J Mol Sci. 2020;21:9710.
Dickson SL, Shirazi RH, Hansson C, Bergquist F, Nissbrandt H, Skibicka KP. The glucagon-like peptide 1 (GLP-1) analogue, exendin-4, decreases the rewarding value of food: a new role for mesolimbic GLP-1 receptors. J Neurosci. 2012;32:4812–20.
Ghidewon M, Wald HS, McKnight AD, De Jonghe BC, Breen DM, Alhadeff AL, et al. Growth differentiation factor 15 (GDF15) and semaglutide inhibit food intake and body weight through largely distinct, additive mechanisms. Diabetes Obes Metab. 2022;24:1010–20.
Konanur VR, Hsu TM, Kanoski SE, Hayes MR, Roitman MF. Phasic dopamine responses to a food-predictive cue are suppressed by the glucagon-like peptide-1 receptor agonist Exendin-4. Physiol Behav. 2020;215:112771.
López-Ferreras L, Richard JE, Noble EE, Eerola K, Anderberg RH, Olandersson K, et al. Lateral hypothalamic GLP-1 receptors are critical for the control of food reinforcement, ingestive behavior and body weight. Mol Psychiatry. 2018;23:1157–68.
Richard JE, Anderberg RH, Göteson A, Gribble FM, Reimann F, Skibicka KP. Activation of the GLP-1 receptors in the nucleus of the solitary tract reduces food reward behavior and targets the mesolimbic system. PLoS One. 2015;10:e0119034.
Treesukosol Y, Moran TH. Administration of Exendin-4 but not CCK alters lick responses and trial initiation to sucrose and intralipid during brief-access tests. Chem Senses. 2022;47:bjac004.
Ong ZY, Liu JJ, Pang ZP, Grill HJ. Paraventricular Thalamic Control of Food Intake and Reward: Role of Glucagon-Like Peptide-1 Receptor Signaling. Neuropsychopharmacology. 2017;42:2387–97.
Vogel H, Wolf S, Rabasa C, Rodriguez-Pacheco F, Babaei CS, Stöber F, et al. GLP-1 and estrogen conjugate acts in the supramammillary nucleus to reduce food-reward and body weight. Neuropharmacology. 2016;110:396–406.
Rolls BJ. Dietary energy density: Applying behavioural science to weight management. Nutr Bull. 2017;42:246–53.
Kissileff HR, Klingsberg G, Van Itallie TB. Universal eating monitor for continuous recording of solid or liquid consumption in man. Am J Physiol. 1980;238:R14–22.
Alceste D, Serra M, Raguz I, Gero D, Thalheimer A, Widmer J, et al. Association between microstructure of ingestive behavior and body weight loss in patients one year after Roux-en-Y gastric bypass. Physiol Behav. 2022;248:113728.
Serra M, File B, Alceste D, Raguz I, Gero D, Thalheimer A, et al. Burst-pause criterion derivation for drinkometer measurements of ingestive behavior. MethodsX. 2022;9:101726.
Griffioen-Roose S, Finlayson G, Mars M, Blundell JE, de Graaf C. Measuring food reward and the transfer effect of sensory specific satiety. Appetite. 2010;55:648–55.
Dalton M, Finlayson G, Hill A, Blundell J. Preliminary validation and principal components analysis of the Control of Eating Questionnaire (CoEQ) for the experience of food craving. Eur J Clin Nutr. 2015;69:1313–7.
Näslund E, King N, Mansten S, Adner N, Holst JJ, Gutniak M, et al. Prandial subcutaneous injections of glucagon-like peptide-1 cause weight loss in obese human subjects. Brit J Nutr. 2004;91:439–46.
Klimek L, Bergmann KC, Biedermann T, Bousquet J, Hellings P, Jung K, et al. Visual analogue scales (VAS): Measuring instruments for the documentation of symptoms and therapy monitoring in cases of allergic rhinitis in everyday health care. Allergo J Int. 2017;26:16–24.
Alkahtni SA, Dalton M, Abuzaid O, Obeid O, Finlayson G. Validation of the Leeds Food Preference Questionnaire in Arabs. Asia Pac J Clin Nutr. 2016;25:257–64.
Dalton M, Finlayson G, Walsh B, Halseth AE, Duarte C, Blundell JE. Early improvement in food cravings are associated with long-term weight loss success in a large clinical sample. Int J Obes. 2017;41:1232–6.
Funding
Open Access funding provided by the IReL Consortium.
Author information
Authors and Affiliations
Contributions
All authors made substantial contributions to designing and drafting of the article. SB, KD, and KJ equally contributed to writing and reviewing the article. All authors reviewed and approved the final version to be submitted.
Corresponding author
Ethics declarations
Competing interests
The first four authors have no conflict of interest to declare. ClR reports grants from the Irish Research Council, Science Foundation Ireland, Anabio, and the Health Research Board. He serves on advisory boards and speakers panels of Novo Nordisk, Herbalife, GI Dynamics, Eli Lilly, Johnson & Johnson, Glia, Irish Life Health, and Boehringer Ingelheim, Currax, Zealand Pharma, and Rhythm Pharma. ClR is a member of the Irish Society for Nutrition and Metabolism outside the area of work commented on here. He was the chief medical officer and director of the Medical Device Division of Keyron in 2021. Both of these are unremunerated positions. ClR was a previous investor in Keyron, which develops endoscopically implantable medical devices intended to mimic the surgical procedures of sleeve gastrectomy and gastric bypass. No patients have been included in any of Keyron’s studies and they are not listed on the stock market. ClR was gifted stock holdings in September 2021 and divested all stock holdings in Keyron in September, 2021. He continues to provide scientific advice to Keyron for no remuneration. ClR provides obesity clinical care in the Beyond BMI clinic and is a shareholder in the clinic.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Bettadapura, S., Dowling, K., Jablon, K. et al. Changes in food preferences and ingestive behaviors after glucagon-like peptide-1 analog treatment: techniques and opportunities. Int J Obes (2024). https://doi.org/10.1038/s41366-024-01500-y
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41366-024-01500-y