Abstract
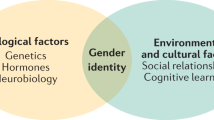
Transgender and gender diverse (TGD) adults are more likely to have obesity compared to cisgender peers. Based on surveys, the TGD population experiences disparities in healthy lifestyle behaviors (e.g., physical activity, screen time) compared to reference groups. They also face significant socioeconomic and healthcare barriers to accessing affirming care and gender minority stress, potentially contributing to increased weight. Gender-affirming hormone therapy is associated with changes in body composition and increased weight, which may impact cardiometabolic risk trajectory. Obesity can also be a barrier to gender-affirming surgeries, and affirming weight management services tailored to TGD patients are an important gap in healthcare to address. This Perspective briefly reviews current literature on the unique barriers experienced by TGD people and their identified needs regarding weight management interventions. It also suggests areas for future research to best fill this gap in healthcare and research while supporting the provision of lifesaving gender-affirming care.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
The Health of Lesbian, Gay, Bisexual, and Transgender People: Building a Foundation for Better Understanding. The National Academies Collection: Reports funded by National Institutes of Health. Washington (DC) 2011.
Brown GR, Jones KT. Mental health and medical health disparities in 5135 transgender veterans receiving healthcare in the veterans health administration: a case-control study. LGBT Health. 2016;3:122–31.
Dragon CN, Guerino P, Ewald E, Laffan AM. Transgender medicare beneficiaries and chronic conditions: exploring fee-for-service claims data. LGBT Health. 2017;4:404–11.
Nagata JM, Ganson KT, Austin SB. Emerging trends in eating disorders among sexual and gender minorities. Curr Opin Psychiatry. 2020;33:562–7.
Christian R, Mellies AA, Bui AG, Lee R, Kattari L, Gray C. Measuring the health of an invisible population: lessons from the Colorado Transgender health survey. J Gen Intern Med. 2018;33:1654–60.
Diamond LM, Alley J. Rethinking minority stress: a social safety perspective on the health effects of stigma in sexually-diverse and gender-diverse populations. Neurosci Biobehav Rev. 2022;138:104720.
VanKim NA, Erickson DJ, Eisenberg ME, Lust K, Simon Rosser BR, Laska MN. Weight-related disparities for transgender college students. Health Behav Policy Rev. 2014;1:161–71.
Newcomb ME, Hill R, Buehler K, Ryan DT, Whitton SW, Mustanski B. High burden of mental health problems, substance use, violence, and related psychosocial factors in transgender, non-binary, and gender diverse youth and young adults. Arch Sex Behav. 2020;49:645–59.
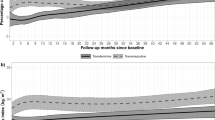
Klaver M, Dekker M, de Mutsert R, Twisk JWR, den Heijer M. Cross-sex hormone therapy in transgender persons affects total body weight, body fat and lean body mass: a meta-analysis. Andrologia. 2017;49:e12660.
Kyinn M, Banks K, Leemaqz SY, Sarkodie E, Goldstein D, Irwig MS. Weight gain and obesity rates in transgender and gender-diverse adults before and during hormone therapy. Int J Obes (Lond). 2021;45:2562–9.
Bigarella LG, Ballardin AC, Couto LS, de Avila ACP, Ballotin VR, Ingracio AR, et al. The impact of obesity on plastic surgery outcomes: a systematic review and meta-analysis. Aesthet Surg J. 2022;42:795–807.
Brownstone LM, DeRieux J, Kelly DA, Sumlin LJ, Gaudiani JL. Body mass index requirements for gender-affirming surgeries are not empirically based. Transgend Health. 2021;6:121–4.
Martinson TG, Ramachandran S, Lindner R, Reisman T, Safer JD. High body mass index is a significant barrier to gender-confirmation surgery for transgender and gender-nonbinary individuals. Endocr Pract. 2020;26:6–15.
Fisher AD, Castellini G, Ristori J, Casale H, Cassioli E, Sensi C, et al. Cross-sex hormone treatment and psychobiological changes in transsexual persons: two-year follow-up data. J Clin Endocrinol Metab. 2016;101:4260–9.
Silva ED, Fighera TM, Allgayer RM, Lobato MIR, Spritzer PM. Physical and sociodemographic features associated with quality of life among transgender women and men using gender-affirming hormone therapy. Front Psychiatry. 2021;12:621075.
Kirby SR, Linde JA. Understanding the nutritional needs of transgender and gender-nonconforming students at a large public midwestern university. Transgend Health. 2020;5:33–41.
van der Sluis WB, de Bruin RJM, Steensma TD, Bouman MB. Gender-affirmation surgery and bariatric surgery in transgender individuals in The Netherlands: Considerations, surgical techniques and outcomes. Int J Transgend Health. 2022;23:355–61.
Funding
JMT has no financial disclosures. SJI receives funding through a Eunice Kennedy Shriver National Institute of Child Health & Human Development grant (The Colorado Building Interdisciplinary Research Careers in Women’s Health [BIRCWH] Program; supported by 5K12HD057022, PIs: Regensteiner JG and Santoro NF).
Author information
Authors and Affiliations
Contributions
JMT and SJI made individual contributions to authorship. JMT wrote the first draft of the manuscript and created the figure. JMT and SJI made critical revisions to the manuscript and reviewed and approved the final version.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Taormina, J.M., Iwamoto, S.J. Filling a gap in care: addressing obesity in transgender and gender diverse patients. Int J Obes 47, 761–763 (2023). https://doi.org/10.1038/s41366-023-01334-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41366-023-01334-0