Abstract
Background
Behavioral processes through which lifestyle interventions influence risk factors for type 2 diabetes (T2DM), e.g., body weight, are not well-understood. We examined whether changes in psychological dimensions of eating behavior during the first year of lifestyle intervention would mediate the effects of intervention on body weight during a 9-year period.
Methods
Middle-aged participants (38 men, 60 women) with overweight and impaired glucose tolerance (IGT) were randomized to an intensive, individualized lifestyle intervention group (n = 51) or a control group (n = 47). At baseline and annually thereafter until nine years body weight was measured and the Three Factor Eating Questionnaire assessing cognitive restraint of eating with flexible and rigid components, disinhibition and susceptibility to hunger was completed. This was a sub-study of the Finnish Diabetes Prevention Study, conducted in Kuopio research center.
Results
During the first year of the intervention total cognitive (4.6 vs. 1.7 scores; p < 0.001), flexible (1.7 vs. 0.9; p = 0.018) and rigid (1.6 vs. 0.5; p = 0.001) restraint of eating increased, and body weight decreased (−5.2 vs. −1.2 kg; p < 0.001) more in the intervention group compared with the control group. The difference between the groups remained significant up to nine years regarding total (2.6 vs. 0.1 scores; p = 0.002) and rigid restraint (1.0 vs. 0.4; p = 0.004), and weight loss (−3.0 vs. 0.1 kg; p = 0.046). The first-year increases in total, flexible and rigid restraint statistically mediated the impact of intervention on weight loss during the 9-year study period.
Conclusions
Lifestyle intervention with intensive and individually tailored, professional counselling had long-lasting effects on cognitive restraint of eating and body weight in middle-aged participants with overweight and IGT. The mediation analyses suggest that early phase increase in cognitive restraint could have a role in long-term weight loss maintenance. This is important because long-term weight loss maintenance has various health benefits, including reduced risk of T2DM.
Similar content being viewed by others
Introduction
Type 2 diabetes mellitus (T2DM) is preventable by lifestyle interventions targeting weight reduction by changes in diet and physical activity [1, 2]. Meta-analyses of randomized controlled trials (RCTs) have, however, shown that a large proportion of people are unable to maintain achieved weight loss [3, 4]. Body weight is a result of a variety of factors, some of which are more and some less modifiable [5]. Therefore, to improve long-term weight loss maintenance, it is important to understand especially the modifiable factors and their role as potential mediators of successful weight loss maintenance. Such potential factors include psychological dimensions of eating behavior [6, 7].
As a distinction of eating habits describing actual food intake, we refer here by the term eating behavior to its psychological dimensions related to motivation to eat [7]. These eating behavior dimensions could influence food intake through choices about what, when and where to eat [7,8,9]. Different dimensions of eating behavior have been identified, such as cognitive restraint of eating, disinhibition and susceptibility to hunger [10]. Cognitive restraint of eating refers to tendency to restrict food intake to lose weight or prevent weight gain. It can be further divided to flexible restraint (a more graduated approach to eating, dieting, and weight) and rigid restraint (a more dichotomous, “all-or-nothing” approach to eating, dieting, and weight) [11]. Disinhibition refers to tendency to eat opportunistically in an obesogenic environment in response to a variety of food and eating stimuli (e.g. emotions, food cues), and susceptibility to hunger to extent of experiencing feelings of hunger and food cravings in different situations.
Longitudinal weight management intervention studies have shown that an increase in cognitive restraint of eating is associated with successful weight loss in participants with overweight or obesity [12,13,14] and with long-term (≥1.5 year) weight maintenance after weight loss [15,16,17]. Increases in both rigid and flexible restraint have been associated with weight loss [18]. Components of restraint of eating may also have divergent associations with health-related outcomes [19] and especially an increase in flexible restraint has been associated with larger weight loss and/or better weight loss maintenance [20, 21]. A reduction in disinhibition [12, 21] and susceptibility to hunger [22] have also predicted weight loss, at least short-term.
Studies that have investigated eating behavior dimensions among people with impaired glucose tolerance (IGT) are still few. The non-controlled Delay of Impaired Glucose Tolerance by a Healthy Lifestyle Trial (DELIGHT) showed that enhancing flexible control and decreasing disinhibition seemed beneficial to control central adiposity and blood glucose in a 1-year follow-up [23]. Increased dietary restraint measured by DEBQ (Dutch Eating Behavior Questionnaire) [24] predicted better long-term weight loss among people with IGT and elevated fasting plasma glucose after a mean follow-up of 2.8 years according to a non-controlled sub-study of the US Diabetes Prevention Program (DPP) [25, 26]. Only one previous intervention study has investigated eating behavior dimensions as mediators of weight loss and weight loss maintenance, although not specifically in those with IGT [27]. It used mediation models to identify mediators of 12-month weight loss and 24-month weight loss maintenance in women with overweight/obesity who underwent a 1-year behavioral treatment program. An increase in flexible, but not rigid, restraint mediated a greater 24-month weight loss.
Thus, more evidence is needed about the role of eating behavior dimensions in long-term weight loss maintenance among people at risk of T2DM. The aim of the present study was to investigate how lifestyle intervention to prevent T2DM affects eating behavior dimensions (cognitive restraint of eating with flexible and rigid components, disinhibition, and susceptibility to hunger) among people with IGT as well as whether changes in eating behavior dimensions during the early phase (i.e. first year) of the lifestyle intervention mediate the long-term effects of the intervention on body weight.
Methods
Participants and procedure
This is a sub-study to the Finnish Diabetes Prevention Study (DPS)—a multicenter lifestyle intervention RCT with a parallel design aiming at assessing the efficacy of lifestyle management to prevent or delay the onset T2DM in people with IGT [28,29,30]. The DPS study was registered with ClinicalTrials.gov (NCT00518167). In the present study we used the eating behavior data collected only in the Kuopio DPS research center, with 38 men and 60 women comprising the study group. People were recruited by screening of high-risk individuals or were identified in earlier epidemiological surveys. The main inclusion criteria were age 40–64 years, body mass index (BMI) > 25 kg/m2 and IGT based on the mean of two 75 g oral glucose tolerance tests (OGTT) (WHO 1985 criteria). At baseline, the mean (SD) age was 53.6 (7.4) years and BMI was 31.3 (4.6) (kg/m2). The study protocol was approved by the ethics committees of the National Public Health Institute in Helsinki, Finland (intervention phase), and of the North Ostrobothnia Hospital District (post-intervention follow-up period). All participants gave written informed consent at baseline and again at the beginning of the post-intervention follow-up.
The RCT started in November 1993 and the recruitment period lasted until June 1997. Randomization to the intervention (n = 51 in the present study) or the control group (n = 47 in the present study) was stratified by center, sex, and baseline 2-h plasma glucose to ensure a balanced study design [30]. All participants had a baseline measurement and annual examinations that included standardized questionnaires and clinical and laboratory measurements. The current study includes data from measurements until November 2006 (i.e. 9 years from the initiation of the study). Participants diagnosed with T2DM during the intervention phase were excluded from the rest of the intervention phase examinations. The intervention phase of the study was discontinued prematurely as recommended by the independent end point committee based on interim endpoint analyses showing that the original research question of the DPS had been reached earlier than had been anticipated [30]. Thus, the median duration of the intervention varied among study participants (median 5 and range 3–6 years in Kuopio) because of the lengthy recruitment period. At the last intervention period visit all participants were given a summary of their laboratory test results during the intervention period, and they were told about the findings of the trial [31]. A post-intervention follow-up was offered to all participants, both those who had not developed T2DM as well as those who had developed T2DM. This article presents the results from the intervention and post-intervention follow-up phases corresponding altogether nine years from baseline. A total of 24 participants did not complete the 9-year study period. Based on Mann–Whitney U test or χ2 test, they did not differ in any of the baseline characteristics from those (n = 74) who completed the entire period (Supplementary Table 1). The fifth-year annual study visit was missing from one participant and the seventh-year study visit from 13 participants.
Lifestyle intervention group
The specific intervention goals were weight reduction (5% or more from baseline weight), dietary modification (energy proportion of total fat <30% and saturated fat <10% of total energy and dietary fiber intake at least 3.6 g/MJ (15 g/1000 kcal), and moderate intensity physical activity (30 min/day or more) [29]. Lifestyle intervention included seven face-to-face consultation sessions (from 30 min to 1 h) with the study nutritionist during the first year and every 3 months thereafter for 3–6 years depending on intervention duration. The sessions in the first year had preplanned topics (e.g., diabetes risk factors, saturated fat, fiber, physical activity, and problem solving), but the discussions were individualized, focusing on specific individual problems. Printed material was used to serve as a reminder at home.
The goal of the counselling was to equip the participants with necessary skills and knowledge and to achieve gradual, permanent behavioral changes to prevent the progression of IGT to T2DM [29]. The dietary advice was tailored to each participant based on 3-day food records, which were filled out four times yearly. Calculated nutrient intakes and a summary of the results were given to the participants with further explanations. The spouse was invited to join some of the sessions, especially if he or she was the one responsible for cooking or shopping in the family.
Goal-setting was an integral part of the intervention. Participants were encouraged to establish personal intermediate lifestyle goals for themselves by proposing practical issues that they could try to improve [29]. The subjects were encouraged to self-monitor the actualization of the goals. The fulfillment of the goals was also discussed during the study visits. Weight was measured at every visit and the participants were encouraged to follow their weight regularly at home. The rate of weight loss not more than 0.5 to 1 kg per week was recommended. In addition, there were some voluntary group sessions, expert lectures and between-visit phone calls and letters. Three participants also received a very low-calorie diet (VLCD) for 2–5 weeks.
The participants were individually advised to increase their overall level of physical activity [29]. This was done and monitored by the nutritionist during the dietary counselling sessions and underlined by the study physicians at the annual visits. The participants were offered voluntary free of charge, supervised, individually tailored circuit-type moderate-intensity resistance training sessions in the gym to improve the functional capacity and strength of the large muscle groups of the body.
Control group
At baseline, the participants in the control group were given general verbal and written information about healthy lifestyle (diet and physical activity) and diabetes risk but no specific individually tailored advice was offered [29]. This was done either personally or in one group session (30 min to 1 h). The key messages were the same as for the intervention group participants: to reduce weight, increase physical activity and make qualitative changes in diet.
Post-intervention follow-up
During the post-intervention follow-up, all participants had a yearly visit with the study nurse [31]. These visits included the same measurement procedures as during the intervention period and were similar for all participants irrespective of their former group allocation. No detailed diet or exercise counselling was given.
Study measures
Information about eating behavior dimensions was obtained by using the Three Factor Eating Questionnaire [10] translated to Finnish. The questionnaire was given as a paper version at every yearly visit during intervention and post-intervention follow-up phase to be filled out at home and returned via mail. The questionnaire contained 51 items, which were summed up into three scales: cognitive restraint of eating (21 items; measures conscious attempts to monitor and regulate food intake), disinhibition (16 items; measures uncontrolled eating in response to cognitive or emotional cues), and susceptibility to hunger (14 items; measures the extent to which respondents experience feelings of hunger in their daily living). Higher scores represented more cognitive restraint of eating, disinhibition, and perceived hunger. In addition to total score of cognitive restraint of eating, two additional scores, flexible (7 items) and rigid (7 items) restraint were calculated according to Westenhoefer [11] (Supplementary Table 2). In this study, term “dietary restraint” is used to describe all three: total cognitive, flexible and rigid restraint of eating. The Cronbach’s alpha’s were for total cognitive restraint α = 0.86, flexible restraint α = 0.74, rigid restraint α = 0.66, disinhibition α = 0.75 and susceptibility to hunger α = 0.76, indicating reasonable internal consistency.
Body weight was measured in light indoor clothing to the nearest 100 g at the baseline and at each annual visit.
Statistical analysis
We present data for the measures of eating behavior dimensions and body weight changes up to nine years study period where data were available for 39 (76%) participants (for both eating behavior and body weight measures) in the intervention group, and 32 (70%) participants for eating behavior and 34 (72%) participants for body weight measures in the control group. Descriptive statistics, Pearson’s chi-squared and correlation tests, Mann–Whitney U-test and independent samples t-test were derived with IBM SPSS statistical software, version 27.0. Correlations were used to evaluate the associations between 1-year changes in eating behavior dimensions and 9-year changes in body weight (weight at year 9 – weight at baseline). All the tests were two-sided.
We analyzed Group × Time latent change scores using structural equation modeling (Mplus statistical software, version 8.4, Muthén and Muthén 1998–2020). We used full information maximum likelihood with robust standard errors and chi-square which accounts for missing values at random and includes all available data. The Group×Time latent change scores were tested to investigate the impact of the intervention on changes in the TFEQ scales and body weight (Wald test).
Effect sizes were investigated to analyze the possible difference between and within groups. Effect sizes were reported using Cohen’s d and were calculated as follows, both for the initial 1-year study period and the entire 9-year study period. The between-group effect sizes were calculated by subtracting the mean difference between the intervention and control groups at baseline from the mean difference between the intervention and control groups at 1-year or 9-years and the result was then divided by the pooled standard deviation of baseline measurements. The within-group effect sizes for both 1-year and 9-year study periods were calculated as follows: the mean change from the baseline to the 1-year measurement was divided by the combined (pooled) baseline and 1-year measurements’ standard deviation, and the mean change from the baseline to the 9-year measurement was divided by the combined baseline and 9-year measurements’ standard deviation. Effect size (between-group, within-group) d ≥ 0.2 was considered small, d ≥ 0.5 moderate and d ≥ 0.8 large [32].
We analyzed mediation using structural equation modeling with full information maximum likelihood, which accounts for missing values at random and includes all available data. These simple mediation analyses (Fig. 1) were conducted to determine whether the effects of the intervention (independent variable) on 9-year change in body weight (dependent variable) were mediated by 1-year change in total cognitive restraint of eating or its rigid or flexible components (mediators). Disinhibition and hunger were not tested as mediators because their 1-year changes did not significantly differ between the intervention and control groups. Sex, age, baseline dietary restraint and baseline weight were controlled for in the analyses. The results were reported as the total, direct and indirect effects (i.e. regression coefficients and bias-corrected bootstrap 95% confidence intervals). The reported total effect (a × b + c’ in Fig. 1) illustrates the relationship between the intervention and weight change before adjustment for the change in dietary restraint. The indirect effect (a × b in Fig. 1) represents how much of the association between the intervention and weight change was explained by the dietary restraint change [33]. The indirect effect was considered statistically significant, if the 95% bias-corrected bootstrap confidence intervals (obtained using 5000 bootstrap resamples) did not include zero. The model fit was evaluated using the χ2 statistic, comparative fit index (CFI), and standard root mean square residual (SRMR). A non-significant χ2 (p > 0.05), CFI ≥ 0.95 and SRMR ≤ 0.08 were considered to indicate a good fit for the data [34].
Results
The descriptive characteristics of the participants in the intervention and control groups did not differ at baseline (Table 1).
Changes in body weight during the 9-year study period
At 9 years the intervention goal of weight reduction of 5% or more from the baseline was achieved by 43.6% of the participants in the intervention group as compared with 23.5% in the control group (p = 0.07). The mean percentage change in body weight at 9 years was −2.9% (SD 7.1) in the intervention and +0.8% (SD 5.8) in the control group (p = 0.05). Individual changes in body weight (in percentage) by group are shown in Supplementary Fig. 1.
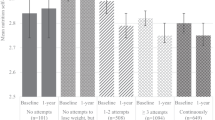
There was a significant interaction effect (time x group) from baseline to year 9 in body weight (p = 0.046) indicating that the changes in weight differed between the groups (Table 2). Weight loss in the intervention group (−5.2 kg) was significantly larger than in the control group (−1.2 kg) during the first year of the study (p < 0.001) (Fig. 2). Furthermore, at 9 years weight loss was still significantly larger in the intervention group (−3.0 kg) compared with the control group (+0.1 kg) (p = 0.046) (Fig. 2). The between-group effect sizes for weight changes at year 1 and 9 were both in favor of the intervention group (Table 2).
Changes in eating behavior dimensions during the 9-year study period
There was a significant interaction effect (time × group) from baseline to year 9 in total (p = 0.002) and in rigid (p = 0.004) restraint of eating indicating that the measures of these dimensions changed differently between the groups (Table 2). Total (p < 0.001) and rigid (p = 0.001) restraint increased significantly more in the intervention group compared with the control group during the first year of the study (Figs. 2, 3). The between-group effect sizes at year 1 and 9 were moderate (d > 0.5) for total and from moderate to small for rigid restraint in favor of the intervention group (Table 2). Within group effect sizes also showed larger changes in the intervention group compared with the control group from baseline to year 1 in total (intervention: d = 1.00, control: d = 0.38) and in rigid (intervention: d = 0.97, control: d = 0.30) restraint, where the change was large in the intervention group and small in the control group. Furthermore, from baseline to year 9 there was a moderate change in total cognitive restraint of eating in the intervention group but only negligible change in the control group (intervention: d = 0.58, control: d = 0.03) and a moderate change in rigid restraint in the intervention group but a small change in the control group (intervention: d = 0.56, control: d = 0.24).
Flexible restraint increased significantly more (p = 0.018) in the intervention group compared with the control group during the first year of the study (Fig. 3). Also, flexible restraint (p = 0.093) showed a trend in interaction effect from baseline to year 9 (Table 2). The between-group effect sizes at year 1 and 9 for flexible restraint were from small to moderate in favor of intervention group. Within group effect sizes also showed larger changes in the intervention group compared with the control group from baseline to year 1 in flexible restraint (intervention: d = 0.87, control: d = 0.51), where the change was large in the intervention group and moderate in the control group. From baseline to year 9 there was a moderate change in the intervention group but negligible change in the control group (intervention: d = 0.55, control: d = 0.03).
There was no significant interaction effect (time × group) from baseline to year 9 in disinhibition (p = 0.48) (Table 2). Susceptibility to hunger showed a trend in interaction effect from baseline to year 9 (p = 0.05). However, the change was not significantly different in the intervention group compared with the control group during the first year of the study. The between group effect sizes at year 1 and 9 for disinhibition and susceptibility to hunger were negligible.
Overall, in the intervention group the short-term changes in the measures of total cognitive, flexible and rigid restraint of eating were large and the long-term changes were moderate, whereas the changes were small or negligible in the control group, or in disinhibition or hunger in both groups.
Associations between changes in eating behavior dimensions and body weight
The 1-year changes in total (r = −0.34, p = 0.004), rigid (r = −0.32, p = 0.007) and flexible (r = −0.23, p = 0.058) restraint of eating had moderate inverse correlations with the 9-year body weight change indicating that the more the measures of dietary restraint increased during the first year of the study, the more body weight decreased during the 9-year study period. The scatter plots of the correlations are shown in Supplementary Fig. 2.
Dietary restraint scores mediating the effect of intervention on body weight change
Using three simple mediation models we investigated whether 1-year change in total cognitive restraint of eating or its rigid or flexible components mediated the effects of intervention on 9-year weight change (Table 3). The fit indices of all three mediation models indicated a good fit for the data (Table 3). The intervention was significantly related to a greater 1-year increase in total, flexible and rigid restraint (path a, Table 3), respectively. Increases in total and rigid restraint were related to a greater weight loss (path b, Table 3) and for flexible restraint this association showed a borderline trend for statistical significance (p = 0.057). Significant indirect effects (a × b, Table 3) on body weight change from baseline to year 9 were observed for 1-year change in total, flexible and rigid restraint, indicating that these changes statistically mediated the impact of the intervention on weight up to 9 years.
Discussion
This study offered a rare opportunity to study eating behavior dimensions and their associations with long-term weight changes in participants with IGT during the 9-year study period. We found that during the first year of the RCT, dietary restraint (i.e., total cognitive, flexible and rigid restraint of eating) increased and body weight decreased more in the intervention group receiving intensive and individually tailored lifestyle counselling compared with the control group receiving a standard health advice at baseline. These between-group differences remained up to nine years and the results from the mediation analyses suggested that early-phase increase in dietary restraint could have a role in long-term weight loss maintenance.
Our results on the effects of increase in dietary restraint on body weight are consistent with the few previous studies conducted in people with IGT [23, 25]. In the DPP, an increase in the restraint of eating during the initial six months of intervention as measured by DEBQ predicted the achievement of 7% weight loss target after 2.8-year intervention [25]. Also in the DELIGHT, a 1-year increase in flexible restraint as measured by extended version of TFEQ correlated with favorable changes in central obesity and fasting plasma glucose [23].
Furthermore, our study showed that the increase in total, rigid and flexible restraint during the first year statistically mediated the impact of DPS intervention on 9-year weight loss maintenance suggesting that all these restraint strategies could be associated with long-term weight loss maintenance when combined with intensive, individually tailored and professional lifestyle counselling. Also in the previous 3-year weight gain prevention study an increase in all three measures of dietary restraint was associated with decrease in weight at year three [18]. Instead, another intervention study investigating eating behavior dimensions as mediators of weight loss maintenance found that increase in flexible, but not rigid restraint, mediated a greater 24-month weight loss [27]. However, the participants of that study were all female and younger and study period substantially shorter than in the present study which might at least partly explain the different outcomes. Furthermore, Konttinen et al. found among participants with obesity who were treated at regular primary health care and were thus comparable to the control group of the DPS, that an increase in total cognitive restraint of eating measured with TFEQ predicted a greater 2-year weight loss, but not a 6- or 10-year weight loss [17].
Nevertheless, the concept of restrained eating is a controversial issue [19, 35]. This could be due to fact that different measures used to assess restraint of eating seem to capture different types of eaters [36, 37]. TFEQ has been shown to identify people who are motivated by health, successful to consistently control their food consumption, less likely to become disinhibited and more likely to lose or maintain weight over time as compared with restrained eaters identified by the Restraint Scale, another frequently used measure to assess dietary restraint [35, 38, 39]. Therefore, we emphasize that not any kind of dietary restraint would be beneficial. However, we suggest that in a professional lifestyle guidance it is possible to increase restraint of eating in a way that could be associated with successful long-term weight management.
Although we cannot define what were the exact intervention elements in the DPS that contributed to the current results, we can speculate they could have been related to self-regulation, a concept close to restraint of eating [19]. In the systematic review investigating psychological mediators of successful outcomes in obesity-related lifestyle change, self-regulation skills as well as autonomous motivation and self-efficacy emerged as the best predictors of beneficial weight and physical activity outcomes [21]. Emphasis should thus be put to interventions that combine lifestyle management with training of psychological skills, including self-regulation. Goal setting, self-monitoring and evaluation, problem solving, affect regulation and coping strategies in high-risk situations have been used as techniques to enhance self-regulation [19]. These techniques, especially goal setting, problem solving and self-monitoring and evaluation were integral part of the DPS intervention, too. These elements may have contributed to the strengthening of self-regulation skills, that was reflected as a better ability to cognitive restraint of eating which could have contributed to more successful weight loss maintenance. Consequently, training of self-regulation skills could be an important aspect to be emphasized in future lifestyle interventions. Although the data were collected 17−30 years ago the potentially effective intervention elements of the DPS are likely to be effective regardless of the time. Modern technology could offer means to conduct interventions utilizing these same elements even on a larger scale [40]. However, it should be ensured that such interventions are achievable and acceptable also in the vulnerable groups to not unintentionally widen health disparities. A recent review investigating explanations for the effectiveness of nutrition information interventions among adults with a low socioeconomic status (SES) emphasized tailored interventions including teaching of self-regulation skills as well as considering economic and social resources [41]. Furthermore, iterative design, use of visual and multimedia elements and social support have been identified as facilitators of eHealth interventions in groups with low SES [40].
The nine years study duration along with the initial RCT setting are the greatest strengths of the present study. The relatively low attrition, in turn, is a marker of high commitment to the intervention. Furthermore, the use of mediation analyses allowed us to gain more detailed knowledge on the potential role of eating behavior dimensions in the long-lasting body weight decrease among the DPS participants. Moreover, the difference in the long-term weight change between the groups was present after nine years and was comparable or even somewhat greater than the long-term weight reduction reported earlier in the entire DPS study population [42]. This earlier long-term report on the DPS showed that the risk of developing T2DM was still 37% smaller in the intervention group than in the control group even after 13 years. Besides better glucose values the intervention group had also healthier diet and other health benefits, e.g., lower blood pressure and triglycerides compared with the control group [42].
The limitations of the study were a relatively small number of participants as well as varied duration of the intervention period. The DPS study participants were volunteers willing to take part in a long-term trial, which can indicate that they were more health-conscious and motivated compared with the general population. The participants were mostly middle-aged, and the results may be different among younger or older population. In the mediator model, it was assumed that the change in dietary restraint affects the change in body weight. Because of the temporal process of weight loss maintenance (first weight loss, then weight maintenance), the changes in eating behavior dimensions and body weight partially overlapped in the model. However, the overlapping period was only one year as compared to nine years in body weight change. Nevertheless, we cannot rule out that part of the association between the change in dietary restraint and the change in body weight might have happened also the other way round, i.e., the change in body weight might have affected the change in dietary restraint.
To conclude, lifestyle intervention with intensive and individually tailored, professional counselling had long-lasting effects on cognitive restraint of eating and body weight in middle-aged participants with overweight and IGT. The results of the mediation models suggest that early phase increase in cognitive restraint of eating could have a role in long-term weight loss maintenance which may confer various health benefits, including reduced risk of T2DM.
Data availability
The data are subject to national data protection laws. Therefore, data cannot be made freely available in a public repository. However, data can be requested through an individual project agreement. To obtain permission reasonable requests should be addressed to the corresponding author.
References
Paulweber B, Valens P, Lindström J, Lalic NM, Greaves CJ, McKee M, et al. A European evidence-based guideline for the prevention of type 2 diabetes. Horm Metab Res. 2010;42:S3–36.
Uusitupa M, Khan TA, Viguiliouk E, Kahleova H, Rivellese AA, Hermansen K, et al. Prevention of type 2 diabetes by lifestyle changes: a systematic review and meta-analysis. Nutrients. 2019;11:2611–33.
Curioni C, Lourenco P. Long-term weight loss after diet and exercise: a systematic review. Int J Obes Relat Metab Disord. 2005;29:1168–74.
Turk MW, Yang K, Hravnak M, Sereika SM, Ewing LJ, Burke LE. Randomized clinical trials of weight loss maintenance: a review. J Cardiovasc Nurs. 2009;24:58–80.
Berthoud HR. Metabolic and hedonic drives in the neural control of appetite: who is the boss? Curr Opin Neurobiol. 2011;21:888–96.
Bryant EJ, Rehman J, Pepper LB, Walters ER. Obesity and eating disturbance: the role of TFEQ restraint and disinhibition. Curr Obes Rep. 2019;8:363–72.
Bellisle F. How and why should we study ingestive behaviors in humans? Food Qual Prefer. 2009;20:539–44.
Blundell JE, Cooling J. Routes to obesity: phenotypes, food choices and activity. Br J Nutr. 2000;83:S33–8.
Blundell JE, Stubbs RJ, Golding C, Croden F, Alam R, Whybrow S, et al. Resistance and susceptibility to weight gain: individual variability in response to a high-fat diet. Physiol Behav. 2005;86:614–22.
Stunkard AJ, Messick S. The three-factor eating questionnaire to measure dietary restraint, disinhibition and hunger. J Psychosom Res. 1985;29:71–83.
Westenhoefer J. Dietary restraint and disinhibition: is restraint a homogeneous construct? Appetite. 1991;16:45–55.
Cheng HL, Griffin H, Claes BE, Petocz P, Steinbeck K, Rooney K, et al. Influence of dietary macronutrient composition on eating behaviour and self-perception in young women undergoing weight management. Eat Weight Disord. 2014;19:241–7.
Dalle Grave R, Calugi S, Corica F, Di Domizio S, Marchesini G. Psychological variables associated with weight loss in obese patients seeking treatment at medical centers. J Am Diet Assoc. 2009;109:2010–6.
Foster G, Wadden T, Swain R, Stunkard A, Platte P, Vogt R. The Eating Inventory in obese women: clinical correlates and relationship to weight loss. Int J Obes Relat Metab Disord. 1998;22:778–85.
Vogels N, Westerterp-Plantenga M. Successful long-term weight maintenance: a 2-year follow-up. Obesity. 2007;15:1258–66.
Wing RR, Papandonatos G, Fava JL, Gorin AA, Phelan S, McCaffery J, et al. Maintaining large weight losses: the role of behavioral and psychological factors. J Consult Clin Psychol. 2008;76:1015–21.
Konttinen H, Peltonen M, Sjostrom L, Carlsson L, Karlsson J. Psychological aspects of eating behavior as predictors of 10-y weight changes after surgical and conventional treatment of severe obesity: results from the Swedish Obese Subjects intervention study. Am J Clin Nutr. 2015;101:16–24.
McGuire MT, Jeffery RW, French SA, Hannan PJ. The relationship between restraint and weight and weight-related behaviors among individuals in a community weight gain prevention trial. Int J Obes Relat Metab Disord. 2001;25:574–80.
Johnson F, Pratt M, Wardle J. Dietary restraint and self-regulation in eating behavior. Int J Obes Relat Metab Disord. 2012;36:665–74.
Karhunen L, Lyly M, Lapveteläinen A, Kolehmainen M, Laaksonen DE, Lähteenmäki L, et al. Psychobehavioural factors are more strongly associated with successful weight management than predetermined satiety effect or other characteristics of diet. J Obes. 2012;2012:274068.
Teixeira PJ, Carraca EV, Marques MM, Rutter H, Oppert JM, De Bourdeaudhuij I, et al. Successful behavior change in obesity interventions in adults: A systematic review of self-regulation mediators. BMC Med. 2015;13:84–100.
Batra P, Das SK, Salinardi T, Robinson L, Saltzman E, Scott T, et al. Eating behaviors as predictors of weight loss in a 6 month weight loss intervention. Obesity. 2013;21:2256–63.
Zyriax BC, Wolf C, Schlüter A, Khattak AH, Westenhoefer J, Windler E. Association of cognitive dietary restraint and disinhibition with prediabetes – cross-sectional and longitudinal data of a feasibility study in German employees. Public Health Nutr. 2012;15:860–7.
Van Strien T, Frijters JE, Bergers GP, Defares PB. The Dutch Eating Behavior Questionnaire (DEBQ) for assessment of restrained, emotional, and external eating behavior. Int J Eat Disord. 1986;5:295–315.
Delahanty LM, Peyrot M, Shrader PJ, Williamson DA, Meigs JB, Nathan DM, et al. Pretreatment, psychological, and behavioral predictors of weight outcomes among lifestyle intervention participants in the Diabetes Prevention Program (DPP). Diabetes Care. 2013;36:34–40.
Knowler WC, Barrett-Connor E, Fowler SE, Hamman RF, Lachin JM, Walker EA, et al. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med. 2002;346:393–403.
Teixeira PJ, Silva MN, Coutinho SR, Palmeira AL, Mata J, Vieira PN, et al. Mediators of weight loss and weight loss maintenance in middle-aged women. Obesity. 2010;18:725–35.
Eriksson J, Lindström J, Valle T, Aunola S, Hämäläinen H, Ilanne-Parikka P, et al. Prevention of Type II diabetes in subjects with impaired glucose tolerance: The Diabetes Prevention Study (DPS) in Finland. Study design and 1-year interim report on the feasibility of the lifestyle intervention programme. Diabetologia. 1999;42:793–801.
Lindström J, Louheranta A, Mannelin M, Rastas M, Salminen V, Eriksson J, et al. The Finnish Diabetes Prevention Study (DPS): lifestyle intervention and 3-year results on diet and physical activity. Diabetes Care. 2003;26:3230–6.
Tuomilehto J, Lindström J, Eriksson JG, Valle TT, Hämäläinen H, Ilanne-Parikka P, et al. Prevention of type 2 diabetes mellitus by changes in lifestyle among subjects with impaired glucose tolerance. N Engl J Med. 2001;344:1343–50.
Lindström J, Ilanne-Parikka P, Peltonen M, Aunola S, Eriksson JG, Hemiö K, et al. Sustained reduction in the incidence of type 2 diabetes by lifestyle intervention: follow-up of the Finnish Diabetes Prevention Study. Lancet. 2006;368:1673–9.
Cohen J (ed.). Statistical Power Analysis for the Behavioral Sciences. Mahwah, NJ, Erlbaum, 1988.
Mackinnon DP (ed.). Introduction to statistical mediation analysis. Mahwah, Erlbaum, 2008.
Hu L, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Struct Eq Modeling. 1999;6:1–55.
Polivy J, Herman CP, Mills JS. What is restrained eating and how do we identify it? Appetite. 2020;155:104820.
Williamson DA, Martin CK, York-Crowe E, Anton SD, Redman LM, Han H, et al. Measurement of dietary restraint: validity tests of four questionnaires. Appetite. 2007;48:183–92.
Mills JS, Weinheimer L, Polivy J, Herman CP. Are there different types of dieters? A review of personality and dietary restraint. Appetite. 2018;125:380–400.
Herman CP, Mack D. Restrained and unrestrained eating. J Pers. 1975;43:647–60.
Herman CP, Polivy J. Experimental and clinical aspects of restrained eating. In: Stunkard A (ed.). Obesity: Basic mechanisms and treatment. Philadelphia, W.B. Saunders, 1980. pp 208–25.
Al-Dhahir I, Reijnders T, Faber JS, van den Berg-Emons RJ, Janssen VR, Kraaijenhagen RA, et al. The barriers and facilitators of ehealth-based lifestyle intervention programs for people with a low socioeconomic status: scoping review. J Med Internet Res. 2022;24:e34229.
van Meurs T, Oude Groeniger J, de Koster W, van der Waal J. Suggested explanations for the (in)effectiveness of nutrition information interventions among adults with a low socioeconomic status: a scoping review. J Nutr Sci. 2022;11:e50.
Lindström J, Peltonen M, Eriksson JG, Ilanne-Parikka P, Aunola S, Keinänen-Kiukaanniemi S, et al. Improved lifestyle and decreased diabetes risk over 13 years: long-term follow-up of the randomised Finnish Diabetes Prevention Study (DPS). Diabetologia. 2013;56:284–93.
Acknowledgements
We thank Mrs Kaija Kettunen for her valuable assistance in collecting the data of the current study. The study was financially supported by the Academy of Finland (grant 309157 to HK, 332466 to JL) and the SalWe Research Program for Mind and Body (Tekes - the Finnish Funding Agency for Technology and Innovation grant 1104/10). DPS study has been financially supported by the Academy of Finland (128315, 129330), Ministry of Education, Novo Nordisk Foundation, Yrjö Jahnsson Foundation, Juho Vainio Foundation, Finnish Diabetes Research Foundation, Finnish Foundation for Cardiovascular Research, Unilever, and Competitive Research Funding from Tampere, Kuopio and Oulu University Hospitals. The study sponsors have had no role in the design and conduct of the study; the collection, analysis and interpretation of the data; or the preparation, review or approval of the manuscript.
Funding
Open access funding provided by University of Eastern Finland (UEF) including Kuopio University Hospital.
Author information
Authors and Affiliations
Contributions
JL, JT, MU, and LK designed the research protocol. AA worked as a nutritionist and was responsible to the intervention delivery and the acquisition of the data. JS and JM performed the statistical analyses. JS, HK, RL, and LK were responsible for the interpretation of the data and drafting of the manuscript. MU and JT were the principal investigators of the DPS study. All authors reviewed the manuscript critically and approved the final version.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Salmela, J., Konttinen, H., Lappalainen, R. et al. Eating behavior dimensions and 9-year weight loss maintenance: a sub-study of the Finnish Diabetes prevention study. Int J Obes 47, 564–573 (2023). https://doi.org/10.1038/s41366-023-01300-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41366-023-01300-w
This article is cited by
-
Integrating Pharmacotherapy and Psychotherapy for Weight Loss
Journal of Health Service Psychology (2023)