Abstract
Background and aims
Very low-calorie ketogenic diets (VLCKDs) have recently gained increasing interest for their anti-inflammatory effects. Phase angle (PhA), a bioelectrical impedance analysis (BIA)-derived measure used as a screening tool to assess inflammatory status in various clinical conditions has recently been suggested as a novel predictor of inflammatory status in correlation with high-sensitivity C-reactive protein (hs-CRP) levels. PhA’s usefulness in monitoring inflammatory status changes in patients with obesity during active phase VLCKD has not yet been explored. The aim of this pilot study was to examine the role of PhA as a biomarker detecting early inflammatory status changes in women with overweight and obesity 1 month into the active stage of a VLCKD.
Methods—Results
This uncontrolled, single-center, open-label pilot clinical study investigated 260 consecutively enrolled Caucasian women aged 18–69 years (BMI 25.0–50.9 kg/m2) after 31 days of an active stage VLCKD. Anthropometric measurements and PhA were assessed. hs-CRP levels were determined by nephelometric assay. Dietary compliance, physical activity recommendations, and ketosis status were tested weekly by telephone recall. At Day 31, BMI, WC, and hs-CRP levels were observed to have decreased (∆−7.3 ± 2.9%, ∆−6.3 ± 5.0%, and ∆−38.9 ± 45.6%; respectively), while PhA had increased (∆+8.6 ± 12.5%). Changes in ∆ hs-CRP were significantly correlated with changes in BMI, WC, and PhA (p < 0.001). After adjusting for confounding variables, the correlation between changes in ∆ PhA and ∆ hs-CRP remained statistically significant, albeit attenuated (p = 0.024).
Conclusion
This is the first study reporting how, along with the expected rapid effect on body weight, PhA changes during active stage VLKCD occurred very early on and independently of weight loss, and were negatively associated with hs-CRP levels. These findings further support the VLCKD as a first-line dietary intervention to obtain a rapid effect on the obesity-related inflammatory status. They also suggest the possible role of PhA as an easy diagnostic tool to detect inflammation, thereby avoiding blood sampling and expensive biochemical assays. It is also posited that changes in PhA could help nutritionists correctly plan the different stages of the VLCKD protocol.
Similar content being viewed by others
Introduction
Diet is a mainstay of any lifestyle intervention program to tackle the obesity epidemic [1]. Among various dietary interventions and nutritional strategies to manage obesity and its comorbidities, very low-calorie ketogenic diets (VLCKDs) have recently gained increasing interest [2,3,4,5]. The European Association for the Study of Obesity (EASO) guidelines defines a VLCKD as a diet that usually provides less than 800 calories (kcal) per day, no more than 20–50 g/day carbohydrates, and 0.8–1.5 g/kg protein of ideal body weight [6]. The advantages of VLCKDs are increased satiation and satiety, and rapid weight loss, both of which help improve patient compliance [7]. In addition, VLCKDs might also preserve muscle mass [8], whose critical role in glucose metabolism is well-established, although this effect is still debatable [6]. VLCKD treatment is a three-stage multistep protocol: active weight loss, dietary re-education, and maintenance [9]. The active stage is the most important VLCKD stage consisting of a very low-calorie (600–800 kcal/day), with low-carbohydrate intake (20–50 g/day from vegetables), and low-fat consumption (10 g/day of extra virgin olive oil). This active stage lasts between 30 to 45 days, depending on the individual’s weight loss rate, during which patients are expected to obtain about 80% of their target weight loss [9]; as also reported by EASO, the active phase can, however, last up to 12 weeks [6].
Interestingly, mainly on account of the production of ketone bodies, VLCKDs have been associated not only with significant body weight loss but also with anti-oxidant and anti-inflammatory effects [10, 11], which in turn help to reduce inflammation more significantly than other nutritional interventions [2, 10, 12], and ameliorate clinical manifestations of inflammatory diseases, such as psoriasis [13]. Although VLCKDs are effective for weight loss, their relationship with inflammation, particularly in the early phase of the active stage, remains still largely unexplored.
Very recently, Monda et al. [12] reported the short-term anti-inflammatory effects of a VLCKD in a small case study of patients with obesity of both genders on the basis of the significant changes observed in serological markers of inflammation [12]. More appropriate and practical methods of assessing the anti-inflammatory effects induced by VLCKDs in patients with obesity have not yet been investigated [6].
Phase angle (PhA) is a bioelectrical impedance analysis (BIA)-derived measure calculated from the arctangent of the reactance (Xc) and resistance (R) ratio [14]. An indicator of cellular health and integrity, PhA is therefore a valuable tool for determining the inflammatory state associated with many diseases [14]. Gender, age, body mass index (BMI), and nutritional status are the major determinants of PhA [15]. PhA has been used as a screening tool to identify inflammation in patients with cancer [16], obesity [17], type 2 diabetes [18], and hypovitaminosis D [19]. Interestingly, PhA was negatively associated in a group of older women with C-reactive protein (CRP), the acute-phase protein most studied as an inflammatory biomarker for a broad range of pathologic processes [20], and also found to be independent of common modifiable and non-modifiable risk factors, such as age and body composition [21], as well as Prader-Willi syndrome in adults, the most common genetic cause of obesity [22]. We too reported PhA to be inversely associated with CRP levels independently of covariates commonly affecting both PhA and CRP, such as gender, and adherence to the Mediterranean diet [23]. Our study supports the hypothesis that PhA might be an easy and reliable measure to detect inflammation, thereby avoiding expensive biochemical assays and blood sampling [23]. Very recently, PhA has been confirmed as a screening technique for inflammatory processes in chronic diseases, allowing monitoring of subjects at risk for disease onset or progression [24].
PhA has been previously investigated in patients with obesity after three sequential 10-day cycles of ketogenic enteral nutrition.
Results obtained at day 50, including 3 treatment cycles, evidenced that the greater the change in PhA, the greater the weight loss [25]. However, the usefulness of PhA to monitor changes in the inflammatory status in patients with obesity undergoing VLCKDs has not yet been explored, nor have studies been conducted on whether PhA and CRP modifications appear early on during the active VLCKD phase.
Given the above, the aim of this pilot study was to examine the role of PhA as a simple, non-invasive biomarker to detect early inflammatory status changes in a large sample of women with overweight and obesity 1 month into the active stage VLCKD.
Materials and methods
Design and setting
This was an uncontrolled, single-center, open-label pilot clinical study. Participants were enlisted from May 2020 to September 2021 at the Obesity Unit (C.I.B.O. and EASO center), Unit of Endocrinology, Clinical Medicine and Surgery Department, University “Federico II” of Naples. The study included a total of two visits: at baseline and during active stage VLCKD after 1 month (31 days) for anthropometric measures, PhA determinations, and blood sample collection. The research study was approved by the Federico II Ethical Committee (file no. 50/20) and was conducted following the Code of Ethics of the World Medical Association (Declaration of Helsinki) for human studies. All subjects were informed of the study design and purpose, subsequently giving their informed consent.
Population study
A total of 260 Caucasian women aged 18–69 years, with a BMI between 25.0 and 50.9 kg/m2, wishing to lose weight, with a history of failed dietary attempts, who had completed the active VLCKD stage, were consecutively enrolled in this study. Complete medical information was collected from all participants. Baseline physical activity levels, i.e., at least 30 min/day aerobic exercise (YES/NO), were assessed in all participants. To increase case study homogeneity, the exclusion criteria were: male gender; pregnancy or breastfeeding; type 1 and type 2 diabetes mellitus; administration of anti-inflammatory drugs in the month prior to entering the study; previous treatment with anti-obesity drugs or bariatric surgery; clinical conditions that might affect fluid balance or body composition, including endocrine diseases, in particular menstrual abnormalities, liver or kidney failure, cancer, immune and inflammatory diseases documented by a full medical examination and laboratory tests; failure to comply with the guidelines and non-attendance of follow-up visits. Since the PhA device may potentially be negatively affected by the field current induced by impedance measurements, we excluded patients with pacemakers or implanted defibrillators, and also subjects who had sustained a skin injury where the BIA electrodes were placed. In addition, participants of reproductive age were evaluated in early follicular phase, at both at baseline and follow up (end of the active stage).
Anthropometric measurements
Measurements and assessment were performed by the same staff member, between 8 a.m. and 10 a.m. after an overnight fast. All anthropometric measurements were performed with subjects wearing only light clothing and no shoes. Weight and height were measured for each subject to calculate BMI (kg/m2). Height was measured to the nearest 0.5 cm using a wall-mounted stadiometer (Seca 711; Seca, Hamburg, Germany). Body weight was determined to the nearest 0.1 kg using a calibrated beam scale (Seca 711; Seca, Hamburg, Germany). BMI was classified according to WHO criteria: Normal weight, 18.5–24.9 kg/m2; Overweight, 25.0–29.9 kg/m2; Obesity grade I, 30.0–34.9 kg/m2; Obesity grade II, 35.0–39.9 kg/m2; Obesity grade III 40.0 kg/m [2, 26]. Waist circumference (WC), according to the NCHS, was obtained using a non-stretchable measuring tape to the closest 0.1 cm at the narrowest point. In patients with grade III obesity, or in subjects where no narrowest point of the waist was visible, WC was taken using a non-stretchable measuring tape to the nearest 0.1 cm at umbilical level [27]. The measurement was taken with the subject standing upright with the feet together and the arms hanging loosely by her sides, breathing normally, as previously reported [28,29,30].
Nutritional intervention
Subjects who fulfilled inclusion/exclusion criteria were administered the replacement meal VLCKD protocol consisting of three stages: active, re-education, and maintenance. A commercial weight-loss program was used for the VLCKD (New Penta, Cuneo, Italy). After nutritional status assessment, the active-stage diet was prepared by a qualified nutritionist and prescribed by the endocrinologist. The VLCKD provided a total daily energy intake of <800 kcal. The breakdown of macronutrients was as follows: 13% carbohydrates (<30 g/day); 43% protein (1.2–1.5 g/kg ideal body weight); 44% lipids (including 10 g/day extra virgin olive oil as the only seasoning fats). The VLCKD was based on protein from high biological value preparations derived from peas, eggs, soy and whey. In particular, all replacement meals used in this protocol contained between 15 g and 18 g high biological value protein. The average biological value of the replacement meals used in this protocol was about 110, therefore higher than the reference protein (chicken egg protein (albumin) whose glycemic index is 100). In compliance with international recommendations, patients were given multi-vitamin and saline supplements to maintain physiological acid/base balance (PentaCal, Penta, s.r.l., Cuneo, Italy) (B complex vitamins, C and E vitamins, minerals, including potassium, sodium, magnesium, calcium, and omega-3 fatty acids). During the ketosis phase, participants were asked to perform 30 min of moderate physical activity three times a week.
Bioelectrical impedance analysis
To avoid inter-device and inter-observer variability, bioelectrical impedance analysis was performed by the same certified clinical nutritionist using the same phase-sensitive BIA-device (an 800 A current, frequency 50 kHz BIA 101 RJL, Akern Bioresearch, Florence, Italy) [31]. In compliance with European Society of Parenteral and Enteral Nutrition (ESPEN) guidelines [32], all participants lay supine with limbs slightly apart from the body, did not eat, drink or exercise for 6 h or ingest alcohol for 24 h before assessment. Immediately before applying the electrodes, shoes and socks were removed and the contact surfaces cleaned with alcohol. Electrodes (BIATRODES Akern Srl; Florence, Italy) were placed proximal to the phalangeal-metacarpal joint on the dorsal surface of the right hand and distal to the transverse arch on the superior surface of the right foot. The sensing electrodes were placed midway between the distal projection of the radius and ulna of the right wrist and between the medial and lateral malleoli of the right ankle [33]. All measurements were performed under strictly standardized conditions and with the same device to avoid inter-observer and inter-device variability. In particular, as reported by Kyle et al. [32], all patients were asked to empty their bladder 30 min before the BIA evaluation. The device was routinely checked with resistors and capacitors of known values. Reliability for intraday and interday measurements by the same observer was <2% for R, < 2.5% for Xc, and <3.3% for R, < 2.8% for Xc, respectively. The coefficient of variation (CV) of repeated measurements of R and Xc at 50 kHz was determined in 10 females by the same observer: CVs were 1.4% for R and 1.3% for Xc. PhA was derived from the conditions at 50 kHz according to the following formula: PhA (°, degrees) = arc tangent Xc/R*(180/π).
Compliance adherence
Compliance to the VLCKD and the physical activity recommendation was assessed by weekly individual telephone counseling according to a structured support program developed by an endocrinologist and nutritionist. β-hydroxybutyrate was measured from capillary blood once a week by test strips (Optium Xceed Blood Glucose and Ketone Monitoring System; Abbott Laboratories, Chicago, IL, USA). In particular, at baseline and on Day 31, β-hydroxybutyrate levels were measured at the outpatient clinic, while ketosis status was verified directly once a week by patients on telephone recall.
Assay methods
Blood samples were collected between 8.00–10.00 a.m. after an overnight fast of at least 8 h, and subsequently stored at −80 °C until processed. High-sensitivity (hs)-CRP levels were determined by a high-sensitivity CardioPhase nephelometric assay of Siemens Healthcare Diagnostics (Marburg, Germany). The CV of intra- and interassay was <7%.
Statistical analysis
Only subjects who completed the study and had both baseline and final measurements were included in the analysis. Data were analyzed using the SPSS Software and MedCalc® package. Results were described as mean ± standard deviation (SD) or percentage (%). Data distribution was evaluated by a Kolmogorov–Smirnov test. Skewed variables were normalized by a logarithm and re-converted into tables and figures. The differences in variables at baseline and after the VLCKD were compared using the Student’s paired t-test. The chi square (χ2) test was used to determine the significance of differences in frequency distribution across BMI categories. Spearman’s correlation was used to assess the association between pre/post intervention percentage changes (delta ∆%). A partial correlation was performed to control for effects of BMI and age as confounding factors on the correlation between ∆ PhA and ∆ hs-CRP. Because this was a pilot study, no power calculations were performed. It follows that all findings need to be confirmed by larger clinical trials.
Results
Two hundred and sixty women with overweight/obesity, aged 37.6 ± 14.1 years were included in the analyses. All the participants were evaluated after 1 month during the VLCKD active stage. Compliance with diet and physical activity recommendations, and capillary testing for ketosis in the morning just before breakfast, were tested once a week on telephone recall. After 1 month (Day 31) of the active stage VLCKD, mean weight loss percentage was 41.9%.
The anthropometric characteristics and physical activity of the study population at baseline and during the active stage VLCKD after 1 month (Day 31) are shown in Table 1.
Along with the significant decrease in body weight, BMI, WC, and Xc, the distribution of participants across the BMI categories was significantly modified after the VLCKD, with the prevalence of normal weight and overweight individuals increasing and the prevalence of individuals with Grade III obesity dropping (p < 0.001).
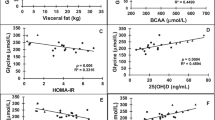
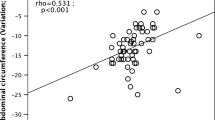
Figures 1 and 2 report PhA and hs-CRP changes. Post-VLCKD PhA measures were significantly increased, while hs-CRP levels were significantly reduced (p < 0.001).
At 1 month (Day 31) during the active stage VLCKD), BMI, WC, and hs-CRP levels had decreased (∆ −7.3 ± 2.9%, ∆ −6.3 ± 5.0%, and ∆ −38.9 ± 45.6%; respectively), while R, Xc, and PhA had risen (∆ +1.4 ± 8.9%, ∆ +9.8 ± 15.5%, and ∆ +8.6 ± 12.5%; respectively).
Correlation between the changes in ∆ hs-CRP and changes in anthropometric parameters and PhA (∆) are reported in Table 2. Changes in ∆ hs-CRP were significantly correlated with changes in BMI, WC, and PhA (p < 0.001).
Finally, as reported in Fig. 3, after adjusting for ∆ BMI, ∆ WC, age, and physical activity the correlation between changes in ∆ PhA and ∆ hs-CRP remained statistically significant, even if attenuated (r = 0.16, p = 0.024, confidence interval 3.14–7.22). Interestingly, the correlation between ∆ PhA and ∆ hs-CRP was also independent of the percentage weight loss (r = −0.25, p < 0.001).
Discussion
This pilot study aimed to evaluate the early effect of a VLCKD on PhA, employed as an inflammation status marker in a large sample of women with overweight and obesity during the active stage of a VLCKD program. All study participants complied with the first, month-long, active-stage of the VLCKD protocol, obtaining significant weight loss. Along with the expected rapid effect on body weight and WC, we also observed significant increases in PhA that were inversely correlated to hs-CRP levels even after the adjustment for common confounding variables, such as BMI, WC, age, and physical activity. As reported by EASO guidelines [6], patients were expected to reach about 80% of their target weight loss after 30 and 45 days of the VLCKD program, depending on their individual weight-loss rate. We observed a lower weight loss mean (41.9%) in our study population. Of note is the fact that the correlation between ∆ PhA and ∆ hs-CRP was also independent of weight-loss percentage.
A growing body of evidence demonstrates that increased adipose tissue deposits correlate directly with increased systemic inflammation [34]. Chronic, low-grade inflammation associated with excess, dysfunctional visceral adipose tissue is an underlying feature of obesity-related diseases [35]. It follows that diets geared to reducing inflammation are particularly useful in patients with obesity [36], clinical evidence indicating the ability of ketogenic diets to induce more significant reductions of inflammation than other nutritional interventions [10]. While the weight-loss and weight-control efficacy of VLCKDs have been evidenced, their relationship with inflammation, particularly in the early phase of the diets’ active stage, remains, however, still largely unexplored.
The ketone bodies produced during a VLCKD exert fast effective anti-inflammatory effects through different mechanisms, including the activation of the peroxisome proliferator-activated receptor gamma and the receptor hydroxy-carboxylic acid receptor 2, inhibition of NF-κB activation, inhibition of NLRP3 inflammasome [13], evidenced by lower levels of circulating markers of inflammation, such as hs-CRP [12]. Investigations have recently begun to explore the mechanisms, safety, and efficacy of ketogenic diets in inducing weight loss and reducing the risk for several chronic diseases, such as cancer, obesity, type 2 diabetes, and cardiovascular diseases [37]. It has been shown that by reducing carbohydrate intake, the ketogenic diet induces fatty acid mobilization from adipose tissue. Fatty acids are oxidized to produce ketone bodies, an important energy substrate, leading to reduced body weight and subsequently lowering chronic inflammation and the risk of obesity-related diseases [38]. In this context, we previously reviewed current evidence supporting the usefulness of VLCKD in psoriasis, a chronic skin immune-mediated disease, which, like obesity, is characterized by chronic underlying inflammation, reporting the clinical indications supporting the use of this dietary protocol as a potential first-line treatment in psoriatic patients with obesity [13].
Interestingly, obesity, obesity-related diseases, and nutrition have been observed to be strictly related to severity of the novel coronavirus disease, CoVID-19 [39,40,41]. Of note is the very recent focus on clinically prescribing VLCKD for patients with obesity and CoVID-19 infection [42]. The physiological increase of ketone bodies induced by a ketogenic diet with resultant anti-inflammatory and immunomodulating effects, may prove to be important tools in both the prevention and treatment of infection, as well as on potential adverse outcomes of CoVID-19 infection [42]. In this context, Cornejo-Pareja I et al. [43] showed PhA to be a prognostic factor for mortality at 90 days in patients with CoVID-19 infection. Indeed, independent of age, sex, BMI, and comorbidities, a low PhA (<3.95°) was a predictor of mortality risk in 127 patients diagnosed with CoVID-19 [43]. These findings suggest that the evaluation of PhA should be routinely included as a mortality risk predictor in the clinical assessment of COVID-19 patients on admission to hospital [43].
The present study is the first to report that PhA changes during active stage VLCKD occurred very early on during the treatment program and were independent of confounding variables influencing PhA values, especially weight loss. The study confirms and extends our previous clinical investigation into the long [2] and short-term [12] anti-inflammatory effects of VLCKDs, evidencing inflammatory biomarker modifications during the first month of active stage VLCKD, before the expected 80% weight loss had been achieved. The early anti-inflammatory effects observed in our study population support the proposed use of the VLCKD as a first-line dietary intervention to obtain a rapid effect on the obesity-related inflammatory status. This early effect is an interesting premise for employing this dietary intervention as part of the management of patients with overweight and obesity, in association with long-term lifestyle strategies to reduce the risk of weight regain. In addition, the inverse relationship between PhA and hs-CRP underpins the role PhA could have as an easy-to-use diagnostic tool to detect inflammation instead of blood sampling and expensive biochemical assays. Furthermore, since persistent inflammation has been recognized as one of the factors involved in the weight regain [44], monitoring PhA changes during early active-phase VLCKD could prove a simple predictor of persistent inflammatory and individual weight-loss rate during the ketogenic phases. This, in turn, would be instrumental to developing patient-specific VLCKD protocols.
Our study has a number of strengths but also limitations. First, this pilot study of a large adult population involved a single-center analysis that may have introduced some selection bias. Nevertheless, in light of the clear gender differences in both PhA values and CRP levels [45], population homogeneity was improved by included only women, of which women of reproductive age were examined at the same menstrual phase. Second, as a pilot study, we did not extend our observations to the end of the active stage and subsequent VLCKD stages. However, the very short observation period obviated patient drop out. Furthermore, as a purely diet-based weight loss strategy, VLCKD mirrored long-term weight loss, which is per se an effective non-pharmacologic strategy for lowering CRP levels [46]. Third, we did not include a control group to confirm that it is ketosis, rather than weight loss per se to exert the anti-inflammatory effect of VLCKD. However, the benefits of short and long-VLCKDs on inflammation in subjects with obesity have been largely demonstrated [9, 12], along with the superiority of VLCKDs compared to standard hypocaloric diets to induce weight loss [2]. Fourth, we did not analyze other inflammatory markers. However, CRP is the most studied inflammatory biomarker for a variety of pathologic processes [47]. In addition, as a direct BIA measurement, PhA is not influenced by altered tissue hydration in the algorithmic computations to assess other body composition compartments [48, 49]. Moreover, we did not evidence any causal effect of CRP levels on PhA, thus supporting the hypothesis that any negative correlation observed is likely without a direct causal link. Other strengths of this study were our adjustment of PhA and hs-CRP levels for commonly confounding factors, including age and BMI, and the performance and interpretation of BIA measurements by only one clinical nutritionist to minimize inter-operator variability.
Conclusion
This is the first report of a study of a large overweight/obese female population treated with a VLCKD to evidence after just 31 days of treatment a significant reduction in patient inflammatory status, as evaluated by hs-CRP levels, and an improvement in PhA, a non-invasive bioimpedance marker, following adjustment for common confounding variables, such as BMI, age, and physical activity. Changes in PhA could offer endocrinologists an easy clinical diagnostic tool to evaluate changes in the inflammation status of VLCKD-treated patients, avoiding blood sampling and expensive biochemical inflammation screening tests. For nutritionists, changes in PhA could be useful in the correct planning of the VLCKD protocol stages (Fig. 4). Further studies on different population samples of both genders undergoing a VLCKD are, however, warranted to highlight early changes in PhA and hs-CRP levels, while an extended follow-up at each VLCKD stage is required to monitor the long-term anti-inflammatory effects of VLCKDs during the weight-loss program.
Changes in PhA could offer to clinicians a possible diagnostic tool to evaluate changes in the inflammation status of VLCKD-treated patients, avoiding blood sampling and expensive biochemical inflammation screening tests. In addition, changes in PhA could be useful in the correct planning of the VLCKD protocol stages. VLCKD very low-calorie ketogenic diet, hs-CRP high sensitivity Creactive protein, PhA phase angle.
Data availability
The datasets generated during and analysed during the current study are available from the corresponding author on reasonable request.
References
Salam RA, Padhani ZA, Das JK, Shaikh AY, Hoodbhoy Z, Jeelani SM, et al. Effects of lifestyle modification interventions to prevent and manage child and adolescent obesity: A systematic review and meta-analysis. Nutrients. 2020. https://doi.org/10.3390/nu12082208.
Moreno B, Bellido D, Sajoux I, Goday A, Saavedra D, Crujeiras AB, et al. Comparison of a very low-calorie-ketogenic diet with a standard low-calorie diet in the treatment of obesity. Endocrine. 2014. https://doi.org/10.1007/s12020-014-0192-3.
Caprio M, Infante M, Moriconi E, Armani A, Fabbri A, Mantovani G, et al. Very-low-calorie ketogenic diet (VLCKD) in the management of metabolic diseases: systematic review and consensus statement from the Italian Society of Endocrinology (SIE). J Endocrinol Investig. 2019. https://doi.org/10.1007/s40618-019-01061-2.
Casanueva FF, Castellana M, Bellido D, Trimboli P, Castro AI, Sajoux I, et al. Ketogenic diets as treatment of obesity and type 2 diabetes mellitus. Rev Endocr Metab Disord. 2020. https://doi.org/10.1007/s11154-020-09580-7.
Castellana M, Conte E, Cignarelli A, Perrini S, Giustina A, Giovanella L, et al. Efficacy and safety of very low calorie ketogenic diet (VLCKD) in patients with overweight and obesity: A systematic review and meta-analysis. Rev Endocr Metab Disord. 2020. https://doi.org/10.1007/s11154-019-09514-y.
Muscogiuri G, El Ghoch M, Colao A, Hassapidou M, Yumuk V, Busetto L. European Guidelines for Obesity Management in Adults with a Very Low-Calorie Ketogenic Diet: A Systematic Review and Meta-Analysis. Obes Fact. 2021. https://doi.org/10.1159/000515381.
Gibson AA, Seimon R V., Lee CMY, Ayre J, Franklin J, Markovic TP, et al. Do ketogenic diets really suppress appetite? A systematic review and meta-analysis. Obes Rev. 2015. https://doi.org/10.1111/obr.12230.
Colica C, Merra G, Gasbarrini A, De Lorenzo A, Cioccoloni G, Gualtieri P, et al. Efficacy and safety of very-low-calorie ketogenic diet: A double blind randomized crossover study. Eur Rev Med Pharmacol Sci. 2017;21:2274–89.
Muscogiuri G, Barrea L, Laudisio D, Pugliese G, Salzano C, Savastano S, et al. The management of very low-calorie ketogenic diet in obesity outpatient clinic: A practical guide. J Transl Med. 2019;17. https://doi.org/10.1186/s12967-019-2104-z.
Forsythe CE, Phinney SD, Fernandez ML, Quann EE, Wood RJ, Bibus DM, et al. Comparison of low fat and low carbohydrate diets on circulating fatty acid composition and markers of inflammation. Lipids. 2008. https://doi.org/10.1007/s11745-007-3132-7.
Merra G, Miranda R, Barrucco S, Gualtieri P, Mazza M, Moriconi E, et al. Very-low-calorie ketogenic diet with aminoacid supplement versus very low restricted-calorie diet for preserving muscle mass during weight loss: a pilot double-blind study. Eur Rev Med Pharmacol Sci. 2016;20:2613–21.
Monda V, Polito R, Lovino A, Finaldi A, Valenzano A, Nigro E, et al. Short-term physiological effects of a very low-calorie ketogenic diet: Effects on adiponectin levels and inflammatory states. Int J Mol Sci. 2020. https://doi.org/10.3390/ijms21093228.
Barrea L, Megna M, Cacciapuoti S, Frias-Toral E, Fabbrocini G, Savastano S, et al. Very low-calorie ketogenic diet (VLCKD) in patients with psoriasis and obesity: an update for dermatologists and nutritionists. Crit Rev Food Sci Nutr. 2020. https://doi.org/10.1080/10408398.2020.1818053.
Norman K, Stobäus N, Pirlich M, Bosy-Westphal A. Bioelectrical phase angle and impedance vector analysis—Clinical relevance and applicability of impedance parameters. Clin Nutr. 2012. https://doi.org/10.1016/j.clnu.2012.05.008.
Stobäus N, Pirlich M, Valentini L, Schulzke JD, Norman K. Determinants of bioelectrical phase angle in disease. Br J Nutr. 2012. https://doi.org/10.1017/S0007114511004028.
Zuo T, Zhang F, Lui GCY, Yeoh YK, Li AYL, Zhan H, et al. Alterations in Gut Microbiota of Patients With COVID-19 During Time of Hospitalization. Gastroenterology. 2020. https://doi.org/10.1053/j.gastro.2020.05.048.
Curvello-Silva K, Ramos L, Sousa C, Daltro C. Phase angle and metabolic parameters in severely obese patients [Ángulo defase y parámetros metabólicos en pacientes con obesidad severa]. Nutricion Hospitalaria. 2020;37:1130–4.
Jun MH, Kim S, Ku B, Cho J, Kim K, Yoo HR, et al. Glucose-independent segmental phase angles from multi-frequency bioimpedance analysis to discriminate diabetes mellitus. Sci Rep. 2018. https://doi.org/10.1038/s41598-017-18913-7.
Barrea L, Muscogiuri G, Laudisio D, Di Somma C, Salzano C, Pugliese G, et al. Phase angle: A possible biomarker to quantify inflammation in subjects with obesity and 25(OH)D deficiency. Nutrients. 2019. https://doi.org/10.3390/nu11081747.
Sproston NR, Ashworth JJ. Role of C-reactive protein at sites of inflammation and infection. Frontiers in Immunology. 2018. https://doi.org/10.3389/fimmu.2018.00754
Tomeleri CM, Cavaglieri CR, de Souza MF, Cavalcante EF, Antunes M, Nabbuco HCG, et al. Phase angle is related with inflammatory and oxidative stress biomarkers in older women. Exp Gerontol. 2018. https://doi.org/10.1016/j.exger.2017.11.019.
Barrea L, Pugliese G, de Alteriis G, Colao A, Savastano S, Muscogiuri G. Phase angle: Could be an easy tool to detect low-grade systemic inflammation in adults affected by prader–willi syndrome? Nutrients. 2020. https://doi.org/10.3390/nu12072065.
Barrea L, Muscogiuri G, Pugliese G, Laudisio D, de Alteriis G, Graziadio C, et al. Phase Angle as an Easy Diagnostic Tool of Meta-Inflammation for the Nutritionist. Nutrients. 2021;13. https://doi.org/10.3390/nu13051446.
da Silva BR, Gonzalez MC, Cereda E, Prado CM. Exploring the potential role of phase angle as a marker of oxidative stress: A narrative review. Nutrition. 2022. https://doi.org/10.1016/j.nut.2021.111493.
Papadia C, Bassett P, Cappello G, Forbes A, Lazarescu V, Shidrawi R. Therapeutic action of ketogenic enteral nutrition in obese and overweight patients: a retrospective interventional study. Int Emerg Med. 2020. https://doi.org/10.1007/s11739-019-02092-6.
WHO | World Health Organization. Body mass index—BMI. https://www.euro.who.int/en/health-topics/disease-prevention/nutrition/a-healthy-lifestyle/body-mass-index-bmi. Accessed 15 Mar 2021.
National Center for Health Statistics. Available online: https://www.cdc.gov/nchs/data/nhanes/nhanes_11_12/Anthropometry_Procedures_Manual.pdf. Accessed 21 Jan 2022.
Barrea L, Muscogiuri G, Di Somma C, Annunziata G, Megna M, Falco A, et al. Coffee consumption, metabolic syndrome and clinical severity of psoriasis: Good or bad stuff? Arch Toxicol. 2018. https://doi.org/10.1007/s00204-018-2193-0.
Barrea L, Di Somma C, Macchia PE, Falco A, Savanelli MC, Orio F, et al. Influence of nutrition on somatotropic axis: Milk consumption in adult individuals with moderate-severe obesity. Clin Nutr. 2017;36:293–301.
Barrea L, Tarantino G, Di Somma C, Muscogiuri G, Macchia PE, Falco A, et al. Adherence to the Mediterranean Diet and Circulating Levels of Sirtuin 4 in Obese Patients: A Novel Association. Oxidative medicine and cellular longevity. 2017;2017:6101254.
Bioelectrical impedance analysis in body composition measurement: National Institutes of Health Technology Assessment Conference statement. Am J Clin Nutr. 1996 https://doi.org/10.1093/ajcn/64.3.524s.
Kyle UG, Bosaeus I, De Lorenzo AD, Deurenberg P, Elia M, Gómez JM, et al. Bioelectrical impedance analysis - Part II: Utilization in clinical practice. Clin Nutr. 2004. https://doi.org/10.1016/j.clnu.2004.09.012.
Bera TK. Bioelectrical impedance methods for noninvasive health monitoring: A review. J Med Eng. 2014. https://doi.org/10.1155/2014/381251.
Kawai T, Autieri M V., Scalia R. Adipose tissue inflammation and metabolic dysfunction in obesity. Am J Physiol Cell Physiol. 2021. https://doi.org/10.1152/ajpcell.00379.2020.
Saltiel AR, Olefsky JM. Inflammatory mechanisms linking obesity and metabolic disease. J Clin Investig. 2017. https://doi.org/10.1172/JCI92035.
Sung J, Ho CT, Wang Y. Preventive mechanism of bioactive dietary foods on obesity-related inflammation and diseases. Food Function 2018. https://doi.org/10.1039/c8fo01561a.
Weber DD, Aminazdeh-Gohari S, Kofler B. Ketogenic diet in cancer therapy. Aging. 2018. https://doi.org/10.18632/aging.101382.
Paoli A. Ketogenic diet for obesity: Friend or foe? Int J Environ Res Public Health. 2014. https://doi.org/10.3390/ijerph110202092.
Belanger MJ, Hill MA, Angelidi AM, Dalamaga M, Sowers JR, Mantzoros CS. Covid-19 and Disparities in Nutrition and Obesity. N. Engl J Med. 2020. https://doi.org/10.1056/nejmp2021264.
Soares MJ, Müller MJ. Editorial: Nutrition and COVID-19. Eur J Clin Nutr. 2020. https://doi.org/10.1038/s41430-020-0647-y.
Pranata R, Lim MA, Yonas E, Vania R, Lukito AA, Siswanto BB, et al. Body mass index and outcome in patients with COVID-19: A dose–response meta-analysis. Diabet Metab. 2021. https://doi.org/10.1016/j.diabet.2020.07.005.
Paoli A, Gorini S, Caprio M. The dark side of the spoon—glucose, ketones and COVID-19: a possible role for ketogenic diet? J Transl Med. 2020. https://doi.org/10.1186/s12967-020-02600-9.
Cornejo-Pareja I, Vegas-Aguilar IM, García-Almeida JM, Bellido-Guerrero D, Talluri A, Lukaski H, et al. Phase angle and standardized phase angle from bioelectrical impedance measurements as a prognostic factor for mortality at 90 days in patients with COVID-19: A longitudinal cohort study. Clin Nutr. 2021. https://doi.org/10.1016/j.clnu.2021.02.017.
Schmitz J, Evers N, Awazawa M, Nicholls HT, Brönneke HS, Dietrich A, et al. Obesogenic memory can confer long-term increases in adipose tissue but not liver inflammation and insulin resistance after weight loss. Mol Metab. 2016. https://doi.org/10.1016/j.molmet.2015.12.001.
Khera A, McGuire DK, Murphy SA, Stanek HG, Das SR, Vongpatanasin W, et al. Race and gender differences in C-reactive protein levels. J Am Coll Cardiol. 2005. https://doi.org/10.1016/j.jacc.2005.04.051.
Selvin E, Paynter NP, Erlinger TP. The effect of weight loss on C-reactive protein: A systematic review. Archives of Internal Medicine. 2007. https://doi.org/10.1001/archinte.167.1.31.
Nimptsch K, Konigorski S, Pischon T. Diagnosis of obesity and use of obesity biomarkers in science and clinical medicine. Metabolism. 2019. https://doi.org/10.1016/j.metabol.2018.12.006.
Sardinha LB. Physiology of exercise and phase angle: another look at BIA. Eur J Clin Nutr. 2018;72:1323–7.
Saitoh M, Ogawa M, Kondo H, Suga K, Takahashi T, Itoh H, et al. Bioelectrical impedance analysis-derived phase angle as a determinant of protein-energy wasting and frailty in maintenance hemodialysis patients: retrospective cohort study. BMC Nephrol. 2020. https://doi.org/10.1186/s12882-020-02102-2.
Acknowledgements
The expert linguistic revision by Stephanie Johnson made available by New Penta s.r.l. (Cuneo, Italy) is gratefully acknowledged.
Author information
Authors and Affiliations
Contributions
The authors’ responsibilities were as follows: LB, GM, and SS were responsible for the concept and design of the study, data interpretation and drafting of the report; LB, GM and SS: conducted the statistical analyses; SA, CV, GdA, LV, LV, and AC: provided a critical review of the manuscript. All authors contributed to and agreed on the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Barrea, L., Muscogiuri, G., Aprano, S. et al. Phase angle as an easy diagnostic tool for the nutritionist in the evaluation of inflammatory changes during the active stage of a very low-calorie ketogenic diet. Int J Obes 46, 1591–1597 (2022). https://doi.org/10.1038/s41366-022-01152-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41366-022-01152-w
This article is cited by
-
Very low-calorie ketogenic diet (VLCKD) in the management of hidradenitis suppurativa (Acne Inversa): an effective and safe tool for improvement of the clinical severity of disease. Results of a pilot study
Journal of Translational Medicine (2024)
-
Very low-calorie ketogenic diet (VLCKD): a therapeutic nutritional tool for acne?
Journal of Translational Medicine (2024)
-
Ketogenic nutritional therapy (KeNuT)—a multi-step dietary model with meal replacements for the management of obesity and its related metabolic disorders: a consensus statement from the working group of the Club of the Italian Society of Endocrinology (SIE)—diet therapies in endocrinology and metabolism
Journal of Endocrinological Investigation (2024)
-
Very low-calorie ketogenic diet (VLCKD): an antihypertensive nutritional approach
Journal of Translational Medicine (2023)
-
Supplementation with medium-chain fatty acids increases body weight loss during very low-calorie ketogenic diet: a retrospective analysis in a real-life setting
Journal of Translational Medicine (2023)