Abstract
Background
Frequent weight loss attempts are related to maladaptive eating behaviours and higher body mass index (BMI). We studied associations of several type 2 diabetes (T2D) risk factors with weight loss history, defined as the frequency of prior weight loss attempts, among Finnish adults at increased risk for T2D.
Methods
This study (n = 2684, 80% women) is a secondary analysis of the 1-year StopDia lifestyle intervention with digital intervention group, digital intervention + face-to-face counselling group, or control group. The frequency of prior weight loss attempts was categorized into five groups: no attempts/no attempts to lose weight, but trying to keep weight stable/1–2 attempts/3 or more attempts/ continuous attempts. Data on emotional eating and social/emotional nutrition self-efficacy were collected with a digital questionnaire. We assessed baseline differences between categories of weight loss history as well as the intervention effects.
Results
Altogether 84% of participants had attempted weight loss. Those with one or more weight loss attempts had higher BMI, larger waist circumference, and more emotional eating compared to ‘no attempts’ and ‘no attempts to lose weight, but trying to keep weight stable’ categories. The ‘no attempts’ category had the highest baseline fasting insulin, whereas it showed the largest decrease in this measure with the intervention. This change in fasting insulin in the ‘no attempts’ category was significantly different from all the other categories. Emotional nutrition self-efficacy slightly improved in the ‘no attempts’ category, which was significantly different from its concomitant decrease in the categories ‘1-2 attempts’ and ‘3 or more attempts’. The intervention group assignment did not affect the results.
Conclusions
Multiple attempts to lose weight may unfavourably affect T2D risk factors as well as lifestyle intervention outcomes. More research is needed on how weight loss frequency could affect T2D risk factors and how to design lifestyle interventions for individuals with frequent previous weight loss attempts.
Similar content being viewed by others
Introduction
Type 2 diabetes (T2D) is a continuously growing global health problem [1]. An increase in the prevalence of T2D in parallel with the increase in obesity prevalence mirrors their close relationship, as obesity is associated with more cardiovascular disease outcomes, including a significantly higher risk of T2D incidence [2]. Interventions focusing on the two major lifestyle factors, diet and physical activity, have proven successful in preventing T2D among those at high risk for the disease [3, 4].
Dieting and attempting to lose weight have become increasingly common among the general population while maintaining the lost weight remains the main challenge [5,6,7]. On the other hand, the greater number of attempts to lose weight and weight instability have been associated with higher body mass index (BMI) [8,9,10,11], higher prevalence of binge eating disorder in women with obesity [12] as well as in both sexes in a general population [13], greater eating disinhibition in women [13] and maladaptive eating behaviours [14], all of which could mediate the risk of developing T2D. One type of maladaptive eating behaviours associated with weight loss attempts and dieting is emotional eating, which is eating in response to negative emotions [15]. Emotional eating has also been associated with higher BMI [16], greater consumption of energy-dense, high-fat foods [17], poorer weight loss maintenance [18], as well as a higher likelihood of central obesity and T2D [19].
Repeated failed attempts to lose weight could lead to decreased self-efficacy [20], i.e. lower confidence in one’s ability to make changes according to desired goals [21]. Nutrition self-efficacy is one of the psychosocial determinants of adopting healthy dietary behaviours and weight loss [22,23,24]. Some studies have reported that better dietary self-efficacy is associated with more consumption of fruits and vegetables [25, 26], as well as with reduced fat intake and improved glycemic control in adults with T2D [27, 28], although this has not been confirmed in all studies [29].
Given the ever-growing burden of T2D along with ongoing efforts to lose weight, we studied the associations of anthropometric, metabolic, psychological and lifestyle factors with weight loss history, defined as number of prior attempts to lose weight, at baseline and at the end of a 1-year lifestyle intervention, among Finnish adults identified to be at increased risk for T2D.
Materials and methods
Study design and participants
The present study is a secondary analysis of Finnish adults with an increased risk for T2D who participated in the 1-year randomized controlled trial (RCT) of Stop Diabetes (StopDia) (ClinicalTrials.gov registration no. NCT03156478). General aim of the StopDia was to create and implement evidence-based and digitally supported strategies for the prevention of T2D at population level. Details of the StopDia study have been published elsewhere [30]. Briefly, 3265 participants were recruited to participate in the study using the StopDia digital screening tool, including questions from the Finnish Diabetes Risk Score (FINDRISC) questionnaire [31] as well as other questions on inclusion and exclusion criteria for RCT [30]. Participants to take part in the RCT were those who (i) had FINDRISC ≥ 12 points or previous gestational diabetes or history of impaired fasting glucose (IFG) or impaired glucose tolerance (IGT); (ii) were residing in one of the three Finnish provinces (Northern Savo, Southern Carelia, or Päijät-Häme); (iii) had possibility to use a computer, smartphone or tablet with an internet connection; (iv) had a personal cell phone number and (v) had adequate Finnish language skills. The exclusion criteria were (i) diagnosed type 1 or type 2 diabetes; (ii) pregnancy or breastfeeding and (iii) current cancer or less than 6 months since the last cancer treatment. Eligible participants visited a study nurse in their local health care center for baseline anthropometric measurements and reference for clinical measurements in the local laboratories. At this stage, participants signed a written informed consent form. Participants who subsequently gave blood samples for laboratory measurements and filled out the web-based StopDia digital questionnaire were randomly assigned into one of the three RCT groups: (i) digital lifestyle intervention group, in which participants received lifestyle intervention through the ‘BitHabit’ web application, (ii) digital lifestyle intervention and face-to-face counselling group, in which participants received lifestyle intervention through the ‘BitHabit’ web application and six face-to-face group counselling sessions and (iii) control group, in which participants merely received written information on healthy diet and physical activity. Diet and physical activity-related goals in the intervention groups (i) and (ii) as well as content of the written information provided to the control group were built upon established recommendations of Nordic Nutrition Recommendations [32], Finnish Nutrition Recommendations [33] and international physical activity guidelines [34,35,36].
For the present study, we selected those who had participated in the RCT based on having FINDRISC ≥ 12 points, previous gestational diabetes, or confirmed IFG/IGT by the StopDia laboratory measurements. In addition, those who had current eating disorders were excluded (n = 23). The final number of participants in the present study was 2684 (80% women).
Study data were collected and managed using REDCap electronic data capture tools hosted at the University of Eastern Finland [37, 38]. REDCap (Research Electronic Data Capture) is a secure, web-based software platform designed to support data capture for research studies, providing (1) an intuitive interface for validated data capture; (2) audit trails for tracking data manipulation and export procedures; (3) automated export procedures for seamless data downloads to common statistical packages and (4) procedures for data integration and interoperability with external sources.
Measures
FINDRISC questionnaire
The FINDRISC questionnaire is a practical tool to screen for the risk of developing T2D within the next 10 years of life [31]. It consists of eight questions about age, BMI, waist circumference, weekly physical activity, daily consumption of vegetables, fruit or berries, use of anti-hypertensive medication, history of having high blood glucose concentrations, and family history of diabetes. The total FINDRISC score is the sum of scores of its questions and it ranges from 0 to 26. The higher the FINDRISC score the higher the risk of developing T2D during the next 10 years.
Background characteristics
For background information, the StopDia digital questionnaire included questions about individuals’ sociodemographic characteristics (e.g. age, marital status, education level), history of diagnosed non-communicable diseases (e.g. coronary heart disease) and history of medication (e.g. use of anti-hypertensive medication).
Lifetime history of weight loss
Individuals’ weight loss history was assessed within the StopDia digital questionnaire by asking: Have you tried to lose weight during your lifetime? The question had five answer options: (i) No, (ii) No, but I have been trying to keep my weight stable, (iii) Yes, 1–2 times, (iv) Yes, ≥3 times, (v) Yes, continuously [39].
Anthropometric, clinical and biochemical measures
Trained nurses performed the measurements at the local health care centers and the local laboratories. Body weight was measured in light clothing by digital scales to accuracy of 0.1 kg. Height was measured in a Frankfurt position and without shoes to accuracy of 1 cm. Waist circumference was measured in standing position on bare skin at the end of normal exhalation and at the mid-distance between the bottom of the rib cage and the top of the iliac crest to accuracy of 1 cm. Following a 5-minute rest, resting blood pressure was measured twice, with a 2-min interval, from the right arm in a sitting position to accuracy of 1 mmHg, and mean of the two measurements was reported for systolic and diastolic blood pressures.
After a 12 hour overnight fasting, blood samples were taken to be analysed for glucose and insulin concentrations [fasting and 2 hours after the ingestion of 75 g glucose in an oral glucose tolerance test, glycated haemoglobin (HbA1c)] and fasting plasma total and lipoprotein lipid concentrations [total cholesterol, low-density lipoprotein (LDL) cholesterol, high-density lipoprotein (HDL) cholesterol and total triglycerides]. The disposition index, as a measure of early-phase insulin secretion, and the Matsuda index, as a measure of peripheral insulin sensitivity, were calculated using commonly used formulas [30, 40, 41].
Psychobehavioural measures
The StopDia digital questionnaire included measures of emotional eating and nutrition self-efficacy. Emotional eating was measured using the three items of the Three-Factor Eating Questionnaire (TFEQ-R18) [42] [When I feel anxious, I find myself eating; When I feel blue, I often overeat; When I feel lonely, I console myself by eating]. These items are scored on a 4-point scale with a higher score indicating a higher level of emotional eating. The final score is the sum of the raw scores of the three items transformed into a 0–100 scale [((raw score-lowest possible raw score)/possible raw score range)*100] [43]. Nutrition self-efficacy was assessed using a 10-item questionnaire [44, 45]. The general stem for all items was How certain are you that you could overcome the following barriers? [23], followed by five items measuring social nutrition self-efficacy (the belief in being able to deviate from the social norms), and five items measuring emotional nutrition self-efficacy (the belief in being able to stick to healthy eating in negative psychological states). The item scores range from 1 (very certain I cannot) to 4 (very certain I can) [46], and the final score is calculated as the mean of the related items. A higher score indicates a higher level of total/social/emotional nutrition self-efficacy.
Dietary measures
Dietary intake was measured using an 18-item food intake questionnaire within the StopDia digital questionnaire. Healthy Diet Index (HDI), which has been developed and validated based on this 18-item questionnaire for assessing diet quality as compared to the Nordic Nutrition Recommendations was computed [32, 47]. HDI consists of seven weighted domains: meal pattern, grains, fruit and vegetables, fats, fish and meat, dairy, and snacks and treats. The total HDI score gives a comprehensive measure for diet quality based on the sum score of these domains. It ranges from 0 to 100, with a higher score indicating a better diet quality [47].
Data analysis
Statistical analyses were performed with the SPSS statistical software, version 27 (IBM SPSS Statistics for Windows, Armonk, NY). Differences and associations with P-values ≤ 0.05 were considered statistically significant. Continuous variables are reported as means (SDs) and categorical variables are reported as frequencies (percentages). For assessing baseline differences in the outcomes between the categories of weight loss history, we used analysis of covariance (ANCOVA) for continuous variables, and Chi-squared test for categorical variables. The ANCOVA analysis for BMI was adjusted for age and sex. The analyses for other outcome measures were adjusted for age, sex and BMI. The analyses for blood pressure measures were additionally adjusted for taking blood pressure medication and those of plasma lipid measures were adjusted for taking lipid-lowering medication.
In order to study how weight loss history contributed to changes in outcome measures during 1 year of intervention, we tested for the ‘lifetime history of weight loss × time’ interaction using the intention-to-treat principle, including all 2684 participants in the analyses. Linear mixed-effect model analysis was used, and for each of the outcome measures we tested several models with allowing/ignoring random intercept and random slope on subject and/or study province level [48]. The Bayesian information criterion (BIC) was used as a measure of model adequacy [49, 50]. We selected the model with the lowest BIC value as the best-fitting model for a given outcome variable. We also included in all the analyses the three-way interaction of ‘lifetime history of weight loss × time × intervention group’ to see if 1-year changes in outcome measures in categories of weight loss history were different between the intervention groups, and it was not significant for any of the outcome measures (p > 0.05). The longitudinal analyses were adjusted for age, sex, BMI and baseline values of the outcome measures. The category ‘no attempts’ was considered as the reference category in longitudinal analyses.
Results
Table 1 shows baseline associations of the studied outcomes and weight loss history. Altogether, 84% had attempted to lose weight during their lifetime, and most often reported doing so for three times or more (41%). Only few (4%) reported no conscious efforts to manage their weight, which is neither attempting to lose weight nor trying to keep their weight stable. Participants who reported trying to keep their weight stable were the oldest (Table 1). Those who had attempted to lose weight during their lifetime, especially more frequently, were more likely to be female, and to have higher education level, higher risk of developing T2D based on the FINDRISC score, greater BMI, larger waist circumference and more emotional eating than those who had either no previous weight loss attempts or had been trying to keep their weight stable. Fasting plasma insulin concentration was the highest in the category ‘no attempts’. The results separately for women and men are presented in the supplementary materials (Supplementary Tables 1 and 2).
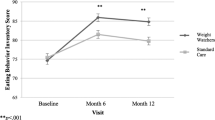
Among all the outcomes tested for (see section 2.2 and Table 1), weight loss history showed a significant contribution to 1-year changes in fasting plasma insulin (p = 0.003), total nutrition self-efficacy (p = 0.02) and emotional nutrition self-efficacy (p = 0.014), regardless of the intervention group assignment (Fig. 1). Mean fasting plasma insulin concentration (Fig. 1a) decreased in individuals with no previous weight loss attempts [−20 pmol/l (−17.6%)] and this change was significantly different from all the other categories of weight loss history, i.e. ‘no attempts to lose weight, but trying to keep weight stable’ [+0.5 pmol/l (+0.7%)], ‘1-2 attempts’ [+2.4 pmol/l (+2.9%)], ‘3 or more attempts’ (+4.3 pmol/l (+4.8%)] and ‘continuously' (−0.03 pmol/l (−0.03%)] (p = 0.002, p = 0.001, p < 0.001, p = 0.002, respectively). Slight increases in total nutrition self-efficacy and emotional nutrition self-efficacy were observed in individuals who had no previous weight loss attempts, whereas those with at least one previous weight loss attempt experienced a decrease in both measures. For total nutrition self-efficacy (Fig. 1b), the categories ‘no attempts’ and ‘1-2 attempts’ differed from each other [+0.02 (+0.7%) vs. −0.1 (−3.4%), p = 0.05]. Changes in emotional nutrition self-efficacy (Fig. 1c) were significantly different between ‘no attempts’ vs. ‘1-2 attempts’ [+0.09 (+3.3%) vs. −0.09 (−3.3%), p = 0.018], and between ‘no attempts’ vs. ‘3 or more attempts’ [+0.09 (+3.3%) vs. −0.05 (−1.9%), p = 0.046]. No other significant changes in outcome measures were observed in the categories of weight loss history. The intervention group assignment did not affect the results.
a Baseline and 1-year levels of fasting plasma insulin concentration in categories of weight loss history (p = 0.003, linear mixed-effect model), adjusted for age, sex, baseline body mass index, baseline fasting plasma insulin, and intervention group assignment. *p = 0.002, **p = 0.001, ***p < 0.001, ****p = 0.002. b Baseline and 1-year levels of total nutrition self-efficacy (possible score range 1–4) in categories of weight loss history (p = 0.02, linear mixed-effect model), adjusted for age, sex, baseline body mass index, baseline total nutrition self-efficacy, and intervention group assignment. *p = 0.05. c Baseline and 1-year levels of emotional nutrition self-efficacy (possible score range 1–4) in categories of weight loss history (p = 0.014, linear mixed-effect model), adjusted for age, sex, baseline body mass index, baseline emotional nutrition self-efficacy, and intervention group assignment. *p = 0.018, **p = 0.046.
Discussion
In the present study population, almost all participants had consciously tried to manage their weight during their lifetime. Those who had attempted to lose weight, in particular more frequently, were more likely to have unfavourable characteristics related to T2D, compared to those who had either no previous weight loss attempts or who had been trying to keep their weight stable. Interestingly, those reporting no previous weight loss attempts had the highest initial fasting plasma insulin concentration but also the greatest improvement in this measure. Furthermore, their total and emotional nutrition self-efficacy slightly improved, whereas these measures rather decreased in the other categories. These findings were independent of the intervention group assignment.
In assessing weight loss history, we aimed at distinguishing those who had previous conscious effort for weight management (trying to keep weight stable/trying to lose weight) from those who had no conscious efforts (no attempts for weight loss/maintenance). Almost all participants (96%) reported having consciously tried to manage their weight during their lifetime; either attempting to lose weight (84%) or trying to keep their weight stable (12%). In other words, only a very small proportion of participants (4%) had not made any conscious efforts for weight management. This is in line with previous findings showing that attempts to lose weight are very common among adults in general populations (42%) [5] and especially among individuals with T2D (71%) [51]. With these very high levels of ongoing individual efforts to lose weight, and weight loss being recommended for people at risk or diagnosed with T2D in order to improve glycemic control, it is of high importance to understand the consequences of frequent attempts to lose weight.
In the present study, attempts to lose weight were more common among women than among men. This could be partially attributed to higher health-consciousness and greater interest in healthy lifestyle among women [52]. However, this finding could be biased due to significantly more women participating in the RCT. In addition, having more previous weight loss attempts was most common among those having high education levels, which is also consistent with previous findings [5, 53, 54]. Individuals with higher education levels may attempt to lose weight more frequently, partially resulting from higher awareness of consequences of obesity and the social norm of lower body weight as well as better accessibility of services due to higher socioeconomic status [55, 56].
Participants with previous weight loss attempts showed higher baseline BMI, and larger waist circumference, particularly compared to those who had been trying to keep their weight stable. It may be suggested that attempting to lose weight, especially more frequently, may eventually result in increased total and central adiposity. Similar findings have been reported in some previous cross-sectional and prospective studies [11, 57]. More attempts to lose weight may lead to weight fluctuation, subsequent increase in abdominal obesity [11, 58, 59] and insulin resistance [60]. This pathway could be plausible also in our study population, although weight fluctuation in terms of weight loss magnitude was not studied. However, we could not draw any cause-effect relationship due to cross-sectional nature of the analysis, as individuals with more obesity/abdominal obesity may attempt to lose weight more frequently. In addition, higher FINDRISC score with more prior weight loss attempts in the present study could denote a need for healthier lifestyle adoption by these individuals, such as increasing fiber intake and being more physically active [31]. A few studies investigating the association between prior intentional attempts to lose weight and diabetes-related outcomes and risk factors have in fact yielded inconsistent findings [8, 11, 54, 61, 62], probably due to the use of different weight loss methods or different characteristics of study participants.
We found that mean fasting plasma insulin was significantly higher among those with no prior weight loss attempts than in the other weight loss attempt categories. However, after one year, mean fasting insulin concentration noticeably decreased in the ‘no attempts’ category, whereas only slight changes occurred in the other categories. This finding was independent of initial BMI, waist circumference and fasting insulin concentration, suggesting that individuals with no prior attempts to lose weight could benefit the most from incorporating modifications into their lifestyle. Although StopDia was not a weight loss intervention, those with no prior weight loss attempts being more motivated to implement a set of lifestyle changes and higher compliance with the program may partly justify this finding. On the other hand, as no beneficial changes were observed in those with any number of prior weight loss attempts, this finding gives additional evidence for probable negative metabolic consequences of repeated weight loss attempts. Previous studies have similarly reported a negative association between history of repeated weight loss attempts and adherence to lifestyle modification programs as well as poorer long-term weight loss outcomes [24, 63, 64].
Factors underlying frequent attempts to lose weight and its association with unfavourable metabolic changes are not clear; however, a physiological response to weight loss by means of restoring fat reserves and weight cycling have been suggested as potential contributors [54, 65, 66]. Repeated dieting and weight cycling have been reported to have negative health consequences, particularly in normal-weight individuals [11, 67]. Overall, it seems that unnecessary weight loss attempts should be avoided, and in any necessity to lose weight proper strategies to support maintenance of the reduced weight should be guaranteed.
Interestingly, after the 1-year lifestyle intervention, those who had previously attempted to lose weight, even once, experienced a small decrease in nutrition self-efficacy in general and in emotional nutrition self-efficacy in particular. On the contrary, those who had no prior weight loss attempts experienced a slight increase in these measures. However, it should be noted that the changes in nutrition self-efficacy measures were small, and we cannot conclude their clinical significance. This is, however, an interesting finding and warrants further research on whether even few attempts to lose weight could disadvantageously affect self-efficacy. Furthermore, it probably suggests that the StopDia intervention was not adequately effective for improving nutrition self-efficacy among those with prior weight loss attempts. Therefore, a more targeted approach for improving nutrition self-efficacy, e.g. through identifying reasons behind the previous failures in losing weight should be considered in future lifestyle interventions involving similar target populations. From the perspective of habit theory, this group may benefit more from habit-breaking skills, which demands more effortful strategies than forming a new habit [68].
Those with greater number of weight loss attempts reported more initial emotional eating, although longitudinal changes in this measure were not significant. Similarly, previous studies have reported more emotional eating and more disinhibition of eating among individuals with previous weight loss attempts compared to those with no previous attempts [39, 69]. Thus, as participants in the present study were at high risk for T2D and emotional eating has been linked to unfavourable metabolic characteristics [19, 70, 71], we suggest that future T2D prevention and treatment programs should address emotional eating, particularly among individuals with a history of repeated attempts to lose weight.
As for diet quality, no baseline and longitudinal differences between the categories of weight loss attempt history were observed. This finding contradicts the findings of a recent study among the general Finnish population, which found that individuals with previous intentional weight loss attempts had a better diet quality than those with no previous attempts [54]. On the other hand, individuals with prior intentional weight loss attempts and the lowest diet quality had a greater 15-year T2D risk, compared to those with the lowest diet quality and no prior weight loss attempts [54]. Different measures for self-reported diet quality and different characteristics of the study populations could justify discrepancy of these findings. However, further research is needed to better understand plausible interactions of weight loss attempt history and diet quality regarding T2D risk.
Strengths and limitations
Our study has various strengths such as a large study sample as well as using a comprehensive set of anthropometric, clinical, metabolic, lifestyle, and behavioural factors related to T2D risk, which to our knowledge is the first of its kind. The FINDRISC was used to reach individuals at risk for T2D that is a simple validated non-invasive tool. The lifestyle intervention was integrated into the routines in health care centers, which could decrease burden of committing and participating in the intervention.
As a limitation, women comprised 80% of the participants in the present study, which could limit generalizability of the findings. However, ‘sex’ was adjusted for in all the statistical analyses. For the weight loss history, only number of previous attempts to lose weight was inquired, but not the net weight change (net increase/decrease) or the amount of weight change. Thus, we could not study whether weight fluctuation was modifying the effect of weight loss history on the outcomes. Another important limitation of the study was that the number of participants in the ‘no attempts’ category was less than in the other categories, which might affect the comparisons between the weight loss history categories. Furthermore, participants in the control group received brief recommendations for diet and physical activity, which could at least partially explain why the intervention group assignment had no effects on the results. Finally, it should be noted that as the present study was a secondary analysis of the StopDia intervention study, the analyses were not considered in the power calculation.
Conclusions
Great majority of individuals at risk for T2D, who participated in the Stop Diabetes T2D prevention intervention had attempted to lose weight during their lifetime. Particularly those with more frequent attempts to lose weight had less favourable profile for several T2D risk factors. Individuals with no previous weight loss attempts particularly benefited from participating in the StopDia study, showing slight improvements in fasting insulin as well as in nutrition self-efficacy. These findings suggest that multiple attempts to lose weight may unfavourably affect T2D risk factors as well as efficacy of lifestyle modification. Therefore, we suggest that frequency of prior weight loss attempts should be taken into account for designing T2D prevention strategies, although more research is needed on the effects of conscious weight loss efforts on T2D risk factors.
References
International Diabetes Federation. IDF Diabetes Atlas, 9th edn. Brussels, Belgium. 2019. http://www.idf.org/sites/default/files/Atlas-poster-2014_ES.pdf.
Riaz H, Khan MS, Siddiqi TJ, Usman MS, Shah N, Goyal A, et al. Association between obesity and cardiovascular outcomes: a systematic review and meta-analysis of Mendelian randomization studies. JAMA Netw Open. 2018;1:e183788.
Tuomilehto J, Lindström J, Eriksson JG, Valle TT, Hämäläinen H, Ilanne-Parikka P, et al. Prevention of type 2 diabetes mellitus by changes in lifestyle among subjects with impaired glucose tolerance. N Engl J Med. 2001;344:1343–50.
Knowler WC, Barrett-Connor E, Fowler SE, Hamman RF, Lachin JM, Walker EA, et al. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med. 2002;346:393–403.
Santos I, Sniehotta FF, Marques MM, Carraça EV, Teixeira PJ. Prevalence of personal weight control attempts in adults: a systematic review and meta-analysis. Obes Rev. 2017;18:32–50.
Sumithran P, Proietto J. The defence of body weight: a physiological basis: for weight regain after weight loss. Clin Sci. 2013;124:231–41.
Wing RR, Phelan S. Long-term weight loss maintenance. Am J Clin Nutr. 2005. https://doi.org/10.1093/ajcn/82.1.222s.
Pietiläinen KH, Saarni SE, Kaprio J, Rissanen A. Does dieting make you fat? A twin study. Int J Obes. 2012;36:456–64.
Sainsbury K, Evans EH, Pedersen S, Marques MM, Teixeira PJ, Lähteenmäki L, et al. Attribution of weight regain to emotional reasons amongst European adults with overweight and obesity who regained weight following a weight loss attempt. Eat Weight Disord. 2019;24:351–61.
Siahpush M, Tibbits M, Shaikh RA, Singh GK, Sikora Kessler A, Huang TTK. Dieting increases the likelihood of subsequent obesity and BMI gain: results from a prospective study of an Australian National Sample. Int J Behav Med. 2015;22:662–71.
Sares-Jäske L, Knekt P, Männistö S, Lindfors O, Heliövaara M. Self-report dieting and long-term changes in body mass index and waist circumference. Obes Sci Pract. 2019;5:291–303.
Giusti V, Héraïef E, Gaillard RC, Burckhardt P. Predictive factors of binge eating disorder in women searching to lose weight. Eat Weight Disord. 2004;9:44–49.
Serdar K, Mazzeo S, Mitchell K, Aggen S, Kendler K, Bulik C. Correlates of weight instability across the lifespan in a population-based sample. Int J Eat Disord. 2011;44:506–14.
Kaluski D, Natamba B, Goldsmith R, Shimony T, Berry E. Determinants of disordered eating behaviors among Israeli adolescent girls. Eat Disord. 2008;16:146–59.
van Strien T. Causes of emotional eating and matched treatment of obesity. Curr Diab Rep. 2018. https://doi.org/10.1007/s11892-018-1000-x.
Brytek-Matera A, Rogoza R, Czepczor-Bernat K. The Three-Factor Eating Questionnaire-R18 Polish version: factor structure analysis among normal weight and obese adult women. Arch Psychiatry Psychother. 2017;19:81–90.
Camilleri GM, Méjean C, Kesse-Guyot E, Andreeva VA, Bellisle F, Hercberg S, et al. The associations between emotional eating and consumption of energy-dense snack foods are modified by sex and depressive symptomatology. J Nutr. 2014;144:1264–73.
Elfhag K, Rössner S. Who succeeds in maintaining weight loss? A conceptual review of factors associated with weight loss maintenance and weight regain. Obes Rev. 2005;6:67–85.
Lopez-Cepero A, Frisard CF, Lemon SC, Rosal MC. Association of dysfunctional eating patterns and metabolic risk factors for cardiovascular disease among Latinos. J Acad Nutr Diet. 2018;118:849–56.
Kerrigan SG, Clark M, Convertino A, Forman EM, Butryn ML. The association between previous success with weight loss through dietary change and success in a lifestyle modification program. J Behav Med. 2018;41:152–9.
Bandura A. Health promotion by social cognitive means. Heal Educ Behav. 2004;31:143–64.
Laatikainen T, Philpot B, Hankonen N, Sippola R, Dunbar JA, Absetz P, et al. Predicting changes in lifestyle and clinical outcomes in preventing diabetes: The Greater Green Triangle Diabetes Prevention Project. Prev Med (Baltim). 2012;54:157–61.
Hankonen N, Absetz P, Kinnunen M, Haukkala A, Jallinoja P. Toward identifying a broader range of social cognitive determinants of dietary intentions and behaviors. Appl Psychol Heal Well Being. 2013;5:118–35.
Teixeira PJ, Going SB, Houtkooper LB, Cussler EC, Metcalfe LL, Blew RM, et al. Pretreatment predictors of attrition and successful weight management in women. Int J Obes. 2004;28:1124–33.
Luszczynska A, Tryburcy M, Schwarzer R. Improving fruit and vegetable consumption: a self-efficacy intervention compared with a combined self-efficacy and planning intervention. Health Educ Res. 2007;22:630–8.
Kreausukon P, Gellert P, Lippke S, Schwarzer R. Planning and self-efficacy can increase fruit and vegetable consumption: a randomized controlled trial. J Behav Med. 2012;35:443–51.
Al-Khawaldeh OA, Al-Hassan MA, Froelicher ES. Self-efficacy, self-management, and glycemic control in adults with type 2 diabetes mellitus. J Diabetes Complications. 2012;26:10–16.
Strychar I, Elisha B, Schmitz N. Type 2 diabetes self-management: role of diet self-efficacy. Can J Diabetes. 2012;36:337–44.
Teixeira PJ, Going SB, Houtkooper LB, Cussler EC, Martin CJ, Metcalfe LL, et al. Weight loss readiness in middle-aged women: psychosocial predictors of success for behavioral weight reduction. J Behav Med. 2002;25:499–523.
Pihlajamäki J, Männikkö R, Tilles-Tirkkonen T, Karhunen L, Kolehmainen M, Schwab U, et al. Digitally supported program for type 2 diabetes risk identification and risk reduction in real-world setting: protocol for the StopDia model and randomized controlled trial. BMC Public Health. 2019. https://doi.org/10.1186/s12889-019-6574-y.
Lindström J, Tuomilehto J. The diabetes risk score: a practical tool to predict type 2 diabetes risk. Diabetes Care. 2003;26:725–31.
Nordic Council of Ministers. Nordic Nutrition Recommendations 2012: Integrating nutrition and physical activity. 2012. https://doi.org/10.6027/Nord2014-002.
The National Nutrition Council of Finland. Terveyttä ruoasta—Suomalaiset ravitsemussuositukset 2014. 2014. https://www.ruokavirasto.fi/globalassets/teemat/terveytta-edistava-ruokavalio/kuluttaja-jaammattilaismateriaali/julkaisut/ravitsemussuositukset_2014_fi_web_versio_5.pdf.
Haskell WL, Lee IM, Pate RR, Powell KE, Blair SN, Franklin BA, et al. Physical activity and public health: updated recommendation for adults from the American College of Sports Medicine and the American Heart Association. Circulation. 2007;116:1081–93.
Colberg SR, Sigal RJ, Fernhall B, Regensteiner JG, Blissmer BJ, Rubin RR, et al. Exercise and type 2 diabetes: The American College of Sports Medicine and the American Diabetes Association: Joint position statement. Diabetes Care. 2010. https://doi.org/10.2337/dc10-9990.
Garber CE, Blissmer B, Deschenes MR, Franklin BA, Lamonte MJ, Lee IM, et al. Quantity and quality of exercise for developing and maintaining cardiorespiratory, musculoskeletal, and neuromotor fitness in apparently healthy adults: Guidance for prescribing exercise. Med Sci Sports Exerc. 2011;43:1334–59.
Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)-A metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42:377–81.
Harris PA, Taylor R, Minor BL, Elliott V, Fernandez M, O’Neal L, et al. The REDCap consortium: building an international community of software platform partners. J Biomed Inform. 2019. https://doi.org/10.1016/j.jbi.2019.103208.
Halali F, Lapveteläinen A, Karhunen L, Kantanen T. Eating behavior tendencies among Finnish adults in relation to previous weight loss attempts. Appetite. 2020. https://doi.org/10.1016/j.appet.2020.104650.
Matsuda M, Defronzo RA. Insulin sensitivity indices obtained from comparison with the euglycemic insulin clamp. Diabetes Care. 1999;22:1462–70.
Stǎácaková A, Javorský M, Kuulasmaa T, Haffner SM, Kuusisto J, Laakso M. Changes in insulin sensitivity and insulin release in relation to glycemia and glucose tolerance in 6,414 finnish men. Diabetes. 2009;58:1212–21.
Karlsson J, Persson LO, Sjöström L, Sullivan M. Psychometric properties and factor structure of the Three-Factor Eating Questionnaire (TFEQ) in obese men and women. Results from the Swedish Obese Subjects (SOS) study. Int J Obes. 2000;24:1715–25.
de Lauzon B, Romon M, Deschamps V, Lafay L, Borys J-M, Karlsson J, et al. The Three-Factor Eating Questionnaire-R18 is able to distinguish among different eating patterns in a general population. J Nutr. 2004;134:2372–80.
Schwarzer R, Renner B. Health-specific self-efficacy scales. Statistics (Ber). 2009.
Schwarzer R, Renner B. Social-cognitive predictors of health behavior: action self-efficacy and coping self-efficacy. Heal Psychol. 2000;19:487–95.
Hankonen N, Absetz P, Haukkala A, Uutela A. Socioeconomic status and psychosocial mechanisms of lifestyle change in a type 2 diabetes prevention trial. Ann Behav Med. 2009;38:160–5.
Lindström J, Aittola K, Pölönen A, Hemiö K, Ahonen K, Karhunen L, et al. Formation and validation of the healthy diet index (Hdi) for evaluation of diet quality in healthcare. Int J Environ Res Public Health. 2021;18:1–22.
Eloranta AM, Sallinen T, Viitasalo A, Lintu N, Väistö J, Jalkanen H, et al. The effects of a 2-year physical activity and dietary intervention on plasma lipid concentrations in children: the PANIC Study. Eur J Nutr. 2020. https://doi.org/10.1007/s00394-020-02260-x.
Raftery AE. Bayesian model selection in social research. Sociol Methodol. 1995;25:111.
Schwarz G. Estimating the dimension of a model. Ann Stat. 1978;6:461–4.
Green AJ, Fox KM, Grandy S. Impact of regular exercise and attempted weight loss on quality of life among adults with and without type 2 diabetes mellitus. J Obes. 2011. https://doi.org/10.1155/2011/172073.
Ek S. Gender differences in health information behaviour: a Finnish population-based survey. Health Promot Int. 2015;30:736–45.
Wardle J, Griffith J. Socioeconomic status and weight control practices in British adults. J Epidemiol Community Health. 2001;55:185–90.
Sares-Jäske L, Knekt P, Eranti A, Männistö S, Lindfors O, Heliövaara M. Intentional weight loss as a predictor of type 2 diabetes occurrence in a general population. Proc Nutr Soc. 2020. https://doi.org/10.1017/s0029665120001536.
Blane D. The life course, the social gradient, and health. In: Social Determinants of Health. Oxford University Press; 2009.
Hoffmann K, De Gelder R, Hu Y, Bopp M, Vitrai J, Lahelma E, et al. Trends in educational inequalities in obesity in 15 European countries between 1990 and 2010. Int J Behav Nutr Phys Act. 2017. https://doi.org/10.1186/s12966-017-0517-8.
Strychar I, Lavoie M, Messier L, Karelis A, Doucet É, Prud’homme D, et al. Anthropometric, metabolic, psychosocial, and dietary characteristics of overweight/obese postmenopausal women with a history of weight cycling: a MONET (Montreal Ottawa New Emerging Team) Study. YJADA. 2009;109:718–24.
Mackie GM, Samocha-Bonet D, Tam CS. Does weight cycling promote obesity and metabolic risk factors. Obes Res Clin Pract. 2017;11:131–9.
Holbrook TL, Barrett-Connor E, Wingard DL. The association of lifetime weight and weight control patterns with diabetes among men and women in an adult community. Int J Obes. 1989;13:723–9.
Oh TJ, Moon JH, Choi SH, Lim S, Park KS, Cho NH, et al. Body-weight fluctuation and incident diabetes mellitus, cardiovascular disease, and mortality: a 16-year prospective cohort study. J Clin Endocrinol Metab. 2018;104:639–46.
Williamson DF, Pamuk E, Thun M, Flanders D, Byers T, Heath C. Prospective study of intentional weight loss and mortality in never-smoking overweight US white women aged 40-64 years. Am J Epidemiol. 1995;141:1128–41.
Will JC, Williamson DF, Ford ES, Calle EE, Thun MJ. Intentional weight loss and 13-year diabetes incidence in overweight adults. Am J Public Health. 2002;92:1245–8.
Leung AWY, Chan RSM, Sea MMM, Woo J. An overview of factors associated with adherence to lifestyle modification programs for weight management in adults. Int J Environ Res Public Health. 2017. https://doi.org/10.3390/ijerph14080922.
Pasman WJ. Predictors of weight maintenance. Obes Res. 1999;7:43–50.
Teixeira PJ, Going SB, Sardinha LB, Lohman TG. A review of psychosocial pre-treatment predictors of weight control. Obes Rev. 2005;6:43–65.
Maclean PS, Higgins JA, Giles ED, Sherk VD, Jackman MR. The role for adipose tissue in weight regain after weight loss. Obes Rev. 2015;16:45–54.
Montani JP, Schutz Y, Dulloo AG. Dieting and weight cycling as risk factors for cardiometabolic diseases: who is really at risk? Obes Rev. 2015;16:7–18.
Lally P, Gardner B. Promoting habit formation. Health Psychol Rev. 2013. https://doi.org/10.1080/17437199.2011.603640.
Marchesini G, Cuzzolaro M, Mannucci E, Dalle Grave R, Gennaro M, Tomasi F, et al. Weight cycling in treatment-seeking obese persons: data from the QUOVADIS study. Int J Obes. 2004;28:1456–62.
Delahanty LM, Meigs JB, Hayden D, Williamson DA, Nathan DM. Psychological and behavioral correlates of baseline BMI in the Diabetes Prevention Program (DPP). Diabetes Care. 2002;25:1992–8.
Tsenkova V, Boylan JM, Ryff C. Stress eating and health. Findings from MIDUS, a national study of US adults. Appetite. 2013;69:151–5.
Acknowledgements
We would like to thank the health and social care workers as well as the participants for their dedication and contribution to the study.
Funding
The StopDia study was funded by the Strategic Research Council at the Academy of Finland (http://www.aka.fi/en/about-us/SRC/) in 2016–2019 (303537, 303644) and the Novo Nordisk Foundation. The first author has received funding from the North-Savo Finnish Cultural Foundation, the University of Eastern Finland, the Kuopio University Foundation and the Finnish Food Research Foundation. The foundations had no role in writing and publishing the paper. Open access funding provided by University of Eastern Finland (UEF) including Kuopio University Hospital.
Author information
Authors and Affiliations
Contributions
PA, JL, TAL, JP, and LK conceptualized the StopDia project, and T.T-T, TAL, and JP were the project’s administrators. JL, TAL, JP, and LK acquired funding for the StopDia project, RM, T.T-T, PA, MK, US, JL, TAL, JP, and LK designed and developed methodology of the project, and KA, RM, T.T-T, E.J-R, TAL, and JP cured the collected data. JP is the PI of the StopDia project. For the present paper, FH designed the research questions, analyzed the data, and prepared original draft of the paper. AL, KA, RM, T.T-T, E.J-R, PA, MK, US, JL, TAL, JP, and LK critically assessed and reviewed the paper. AL and LK supervised the design, analyses and writing the paper. All authors have read and approved the final version of the paper.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Halali, F., Lapveteläinen, A., Aittola, K. et al. Associations between weight loss history and factors related to type 2 diabetes risk in the Stop Diabetes study. Int J Obes 46, 935–942 (2022). https://doi.org/10.1038/s41366-021-01061-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41366-021-01061-4
This article is cited by
-
The Physiological Effects of Weight-Cycling: A Review of Current Evidence
Current Obesity Reports (2024)