Abstract
Background/objectives
The aim of the study was to examine the effects of exercise training through telerehabilitation applied during COVID-19 isolation period on overweight and obese individuals on physical fitness and quality of life.
Subjects/methods
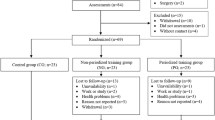
In our study, 41 participants between the ages of 18–65 years and whose BMI values were 25 kg/m2 and above were randomly divided into two groups as telerehabilitation group (n: 21) and control group (n: 20). Exercise training applied to the telerehabilitation group with remote live connection included warm-up exercises, trunk stabilization exercises and breathing exercises under the supervision of a physiotherapist for 6 weeks, 3 days in a week. The control group was only informed about the importance of exercise for one session and evaluated at baseline and after 6 weeks. The physical fitness levels of individuals was assessed by Senior Fitness Test protocol and quality of life by Short Form-36.
Results
As a result of the study, statistically significant improvements were obtained in all parameters of physical fitness, quality of life in the telerehabilitation group (p < 0.05). In the difference values of the two groups, all parameters of physical fitness and quality of life were observed that there were statistically significant differences in favor of telerehabilitation group (p < 0.05).
Conclusions
As a result, it was found that exercise training applied through telerehabilitation during the COVID-19 pandemic process was an effective, safe and viable approach in overweight and obese individuals. In the future, studies investigating the long-term effectiveness of telerehabilitation in this population are needed.
Similar content being viewed by others
Introduction
The World Health Organization (WHO) defines excess weight and obesity as abnormal or excess fat accumulation that poses a risk to health [1]. Excessive and wrong eating habits, inadequate physical activity, age, gender, educational level and socio-cultural characteristics, hormonal and metabolic factors, income status, genetic factors frequent intervals, very low-energy diets, smoking, alcohol use, birth process and drugs that have been used are the major risk factors in the formation of obesity [2].
Evidence exists that identifies habitual sedentary behavior (prolonged sitting) as a new risk factor for cardio metabolic disease and all-cause mortality, regardless of time spent in exercise [3]. Maintaining regular physical activity and exercising routinely in a safe home environment is an important strategy for healthy living during the COVID-19 outbreak [4]. Overweight and obese individuals who are considered high risk for COVID-19 infection are more likely to participate in exercise in their lives, staying more active in this process so that they can get through this process more smoothly.
In the most current version of a systematic review examining rehabilitation practices in COVID-19, it is stated that telerehabilitation should be the first treatment option for people at home [5]. In many other publications published during this period, the importance of telerehabilitation-based approaches is emphasized in the physiotherapy and rehabilitation practices of individuals with both COVID-19 positive and negative and another disease. Moreover, it is recommended to use telerehabilitation practices in the in-hospital period in appropriate patients in order to minimize the risk of transmission and to enable physiotherapists to work effectively and safely [6, 7].
Because of COVID-19 outbreak in our country and in the world, during the period of social isolation/quarantine that face-to-face interview is not possible so we thought exercise training in obese and overweight individuals who need the most physical activity supervised by a physical therapist, the patient with a live connection (sync) with a suitable option for the application might be a suitable idea. In our literature review, it is seen that the effects of telerehabilitation in overweight and/or obese individuals prior to the COVID-19 pandemic process and during this period have not yet been examined in any study.
In our study, our aim was to examine the effect of telerehabilitation on physical fitness and quality of life in overweight and obese individuals during the COVID-19 pandemic social isolation period.
Individuals and method
The study to examine the effect of telerehabilitation on physical fitness and quality of life in overweight and obese individuals during the COVID-19 pandemic social isolation period was carried out in Başkent University, Faculty of Health Sciences, Department of Physiotherapy and Rehabilitation.
Our study took place during a period of nationwide restrictions immediately after the onset of the COVID-19 pandemic in our country. Individuals aged 18–65 years with BMI values of 25 kg/m2 and above were included in the study. Individuals with cognitive, neuromuscular, musculoskeletal, chronic systemic diseases that may prevent exercising, who have undergone surgery in the last 6 months, who are suspected of pregnancy or who are pregnant, active COVID-19 positive and previously infected COVID-19 were not included in the study. Sociodemographic information was recorded after obtaining the necessary oral and written permissions from individuals who met the admission criteria. Informed consent was obtained from the individuals included in the study by giving verbal and written information prior to the evaluations.
Individuals were randomly divided into telerehabilitation (n:21) and control (n:20) group using the computer numbering system. The necessary information and explanations were made before the training to be applied to the individuals in the telerehabilitation group. The interviews took place synchronously (live) from a convenient computer program that allowed remote exercise training. Prior to the training, all individuals were supported to access these programs. At the first meeting, the basic principles of exercises to be applied to individuals were explained to telerehabilitation group. The exercise training was carried out for 6 weeks, 3 sessions per week, an average of 45 min. Assessment surveys used in the study were also transferred to an appropriate computer program, allowing individuals to answer. All exercise training sessions in the telerehabilitation group took place with live remote supervision of the individual participating in the study and a physiotherapist. Assessments of individuals in the control group before and after the 6-week study period were also carried out by providing a live connection. In addition, individuals in the control group were told about the importance of exercise and breathing exercises that they can practice on their own at home with only one session of remote meeting so that they can get through this period more comfortably.
This study was approved by Baskent University Medical and Health Science Research Board and Ethics Committee (Project no: KA20/156) and supported by Baskent University Research Fund.
Sociodemographic characteristics of the individuals involved in our study and height (cm) and body weight (kg) measured by remote control of the physiotherapist were recorded. Before and after the six-week study period of the individuals were evaluated with the following measurements.
Assessment of health-related physical fitness levels
Health- related physical fitness levels of individuals are evaluated by Senior Fitness Test Protocol [8].
-
1.
Chair stand test; is a test used to evaluate the muscle strength of the lower extremity. For the test, the individual is asked to get up from the chair in which he is located and sit again for 30 s, in a position with the arms crossed in the chest. The number of repetitions completed during this time is recorded.
-
2.
Arm curl test; is a test used to evaluate the muscle strength of the upper extremity. 3.5 kg for male individuals and 2.5 kg for female individuals, for 30 s, the elbow is supported on the torso, forearm flexion and extension are asked to do, and the test is repeated for both limbs. The total number of repetitions performed is recorded.
-
3.
2-Minute step test; is a test used to assess cardiovascular endurance. For the test, the distance to the midpoint of the iliac crystal with the patella of the knees is marked and the number of steps completed by maintaining that distance is recorded for 2 min.
-
4.
Chair sit and reach test; is a test used to assess lower limb flexibility. For the test, one knee flexion is requested in the sitting position on the chair, while the other knee is in extension and the ankle is in 90-degree flexion, the individual is asked to reach towards the tip of the toe with both hands. The distance between the fingertip of the hand and the tip of the toe is recorded in centimeters (cm) with the help of a tape measure. The test is repeated three times and the best distance is recorded, and the test is repeated for both limbs. For the measurement, the participant’s relatives were informed and received support.
-
5.
Back scratch test; is a test used to assess upper limb flexibility. The dorsal face of the lower hand, the palmar face of the upper hand is placed on the back, and the approach distance of the middle fingers is recorded in cm by measuring with a tape measure. The test is repeated three times and the best distance is recorded, and the test is repeated for both limbs. For the measurement, the participant’s relatives were informed and received support.
-
6.
8 Foot up and go test; is a test used to assess agility and dynamic balance. The individual is asked to get up from the chair where he is located and take eight steps and sit back in the chair. Time performed is recorded.
Assessment of health-related quality of life
Health related quality of life of individuals was evaluated by Short-form 36 (SF-36). SF-36, developed by Rand Corporation in 1992 [9]. Validity and reliability studies of the Turkish version of SF-36 were conducted by Koçyiğit and his colleagues [10]. The scale consists of 36 items and allows the measurement of 8 separate subheadings. These 8 subheadings are called physical functioning, social functioning, role limitation due to physical health, role limitation due to emotional problems, mental health, energy/vitality, pain and general health. For each subheading, individual points and overall total are obtained from 0 to 100. Zero reports poor health and 100 reports good health.
Telerehabilitation program
Our telerehabilitation program, which was applied to overweight and obese individuals, continued for 3 sessions per week, an average of 45 min, for a total of 6 weeks. Our exercise training consisted of body stabilization-based mat exercises and breathing exercises. 5-minute warm-up and cooling exercises consisting of flexibility exercises for the lower and upper extremities and torso before and after our exercise training were included. Mat exercises, which included a total of 21 body stabilizers performed in five different positions (back, side down, knee up, sitting and face up) were initially performed 10 repetitions. All core stabilization exercises were performed to provide abdominal hallowing. The degree of difficulty was increased when individuals performed 10 repetitions (approximately every 2 weeks), maintaining spinal smoothness in each movement. For individuals who had difficulty maintaining spinal smoothness, the exercises were modified according to the person. In the last 10 min of our telerehabilitation program, 5 breathing exercises including diaphragmatic, chest breathing exercises and thoracic expansion exercises were included. All exercises were supervised with a program that was remotely connected by an experienced physiotherapist. For any situation that may occur during training, individuals were informed in advance, and the necessary person and contact information for emergencies were recorded.
Statistical method
All data in our study was analyzed using the SPSS 20.0 statistical package program. The distribution of demographic information of the participants was examined by frequency analysis. Descriptive statistics such as mean and standard deviation of age, weight, height and body mass index values were calculated. Pre-and post-training measurements obtained from the control and study group were examined by Wilcoxon sign Test and chi square analysis. Cross-Group comparison of measurements obtained before and after training was examined with the Mann–Whitney U test. According to the results of the power analysis, the number of samples required per group for 85% reliability was calculated as 19 [11].
Results
At the end of the 6-week study periods all participants were able to complete the study protocol. There was no individual who had to interrupt the exercise program or assessments.
There was no difference between telerehabilitation and control groups in terms of age, height, weight and BMI prior to the study (p > 0.05) (Table 1).
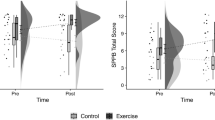
In the telerehabilitation group, pre-training and post-training measurement parameters of the Senior Fitness Test Protocol were compared. Accordingly, all Senior Fitness test protocol sub-measurements were significantly different between pre and post-training averages (p < 0.05) (Table 2).
In the control group, the measurement averages of the Senior Fitness Test protocol before and after training were compared. The 2-minute step test, sit down and stand up in a chair test, and forearm bending test (left) post-training measurements were significantly lower than pre-training measurements, while the 8 foot up and go test post-training average was significantly higher than the pre-training average (p < 0.05) (Table 2).
The results of the Mann–Whitney U test were given to determine whether the physical fitness measurement parameters of the Senior Fitness Test protocol after training and before training were different between groups. Accordingly, post-training and pre-training differences in the Senior Fitness Test Protocol differed significantly between the telerehabilitation and control groups, and the change in the telerehabilitation group was significantly higher than the change in the control group (p < 0.05) (Table 2).
Pre-training and post-training averages of SF-36 quality of life scale were compared in telerehabilitation group. Accordingly, the averages of physical functioning, role limitations due to physical health, energy, mental health, pain and overall health perception differed significantly before and after training (p < 0.05). No difference was found in other measurement parameters (p > 0.05). Post-training averages of physical functioning, role limitation due to physical health, energy, mental health, pain, and overall health perception were significantly higher than pre-training averages (Table 3).
In the control groups, the average pre-and post-training dimensions of the SF-36 quality of life scale were compared. According to that; physical functioning, role limitation due to physical health, role limitation due to emotional problems, energy, mental health, and social functioning subscales and pre- and post-training significant differences were found between their averages (p < 0.05). The average of physical functioning, role limitation due to physical health, role limitation due to emotional problems, energy, mental health and social functioning obtained after training was significantly lower than the average before training (Table 3).
After and before training, the results of the Mann–Whitney U test were examined to determine the differences between groups of sub-parameters of the SF-36 quality of Life Scale. According to that, post-training and pre-training differences in sub-parameters of the SF-36 Quality of Life Scale differed significantly between the training and control groups (p < 0.05). A significant increase in the sub-parameters of the SF-36 quality of Life Scale was observed in the telerehabilitation group, while a decrease was observed in the control group (Table 3).
Discussion
Obese individuals are a high-risk and complex group of patients for COVID-19 infection and the need for hospitalization increases in these patients. Obesity patients also need intensive care to reduce the risk of death. Therefore, it is of great importance that these people avoid infections in order to reduce the spread of the virus. COVID-19 is reported to play a crucial role in the prognosis of obesity. Obesity patients who are subjected to strict measures to control the pandemic have close monitoring needs, including the use of telemedicine due to less physical activity, unhealthy food consumption [12].
Although recent statistics are definite, the level of physical activity during prolonged quarantine is known to be lower than normal [13]. Physical inactivity not only leads to increased predisposition to weight gain, but also lead to deficiencies in skeletal novelization and immune system. Thus, supportive, preventive as a component, moderate physical activity, especially in functional residual capacity and expiratory reserve volume are the additional loss with weight gain, which can lead to serious health consequences, including rapid should be recommended for patients with obesity [13, 14].
Based on these, in our planned study, we wanted to implement a program especially consisting of body stabilization and respiratory exercises, in order to support both musculoskeletal and respiratory systems in our exercise training for obese individuals during the COVID-19 pandemic. No adverse events were encountered in individuals during exercise training program.
Trunk (core) muscles, which include the transverse abdominis, multifidus, diaphragm and pelvic floor muscles contribute to the stability of the spine [15]. Diaphragm muscle, which is one of the body stabilizations muscles, is also the most important inspiration muscle [16]. Physical activity and exercise have positive effects on lung function. In addition, regular exercise training reduces the risk of respiratory infection and may partially prevent COVID-19 from binding to the angiotensin-converting enzyme-2 (ACE-2) receptor. ACE-2 is considered the receptor that allows COVID-19 to enter host cells. ACE-2 is found in the alveolar epithelial cell of types 1 and 2, in the endothelium, there are organs such as the heart, pancreas, and intestinal epithelium. These organs, especially the lungs, are in the risky group in terms of COVID-19 involvement [13].
Lack of exercise associated with inadequate self-management can lead to low levels of physical fitness in people with obesity [17]. According to our literature review, there are no studies investigating the effectiveness of exercise training with telerehabilitation in obese individuals on physical fitness.
When we look at the studies that examine the effects of physical fitness parameters of similar exercise trainings performed face-to-face and obese individuals; Tongvichean and colleagues, in obese individuals controlled self-management-based strategies for a variety of (group discussions, home visits and phone calls) as a result of the exercise program, lower physical fitness parameters, cardiorespiratory fitness, and they get 3-minute step test, chair sit and reach test flexibility in the training group were evaluated with the test parameters indicated that significant improvements in [17]. In the study, Rayes and colleagues compared the control group with Pilates exercises, aerobic exercise (walking), which included body stabilization, in overweight and obese adults, where it was applied for 8 weeks, it is noted that in both exercise groups, they achieved significant improvements in abdominal endurance after exercise training compared to the control group, it has been noted that both aerobic and pilates are effective in improving abdominal muscle endurance, but pilates is more effective in improving abdominal muscle endurance. It is stated that only in the pilates group, there are significant improvements in the flexibility parameters evaluated by the body extensor muscle endurance and chair sit and reach test [18].
Obesity negatively affects postural stability and balance; the incidence of falls and the risk of fractures are higher in these individuals. A study found that obese individuals have poor postural stability and motor control in standing upright posture, during walking and in daily life activities compared to normal weight individuals [19]. Hue and colleagues are noted that increasing body weight negatively affects balance and stability [20]. In another study examining the effects of body stabilization training, it is stated that the contraction of body stabilization muscles increases intra-abdominal pressure and provides body stability. In the same study, it is noted that in a situation where the support surface and posture change due to external forces, higher, stable intra-abdominal pressure is associated with both the postural reaction and stability of the spine [15].
In our study, we used the Senior Fitness Test protocol to determine the effect of exercise training on physical fitness. As a result of our training through telerehabilitation, we have achieved significant improvements in all sub-parameters of physical fitness in the training group, similar to other studies.
Physical activity has a crucial role in improving health and is a key variable for enhancing multidimensional aspects of quality of life. On the other hand, a better quality of life is a motivator for strengthening the practice of physical activity. Physical activity can improve psychological variables such as cognitive function, social relationships, and mood that form a positive health cycle [21]. A study by Dalle and colleagues’ states that obese patients who underperformed on the 6-minute walking test had a lower quality of life than those who walked farther than predicted, also, physical function and quality of life are related in both their physical and mental fields [22]. A study conducted by Vancini and colleagues to improve the physical adaptation levels of overweight and obese individuals’ states that walking and pilates programs significantly benefit health status and quality of life in overweight and/ or obese individuals [23]. As a result of an 8-week study that evaluated group exercises combined with breathing on the SF-36 quality of life scale in obese women, it was noted that the quality of life improved [24]. In another study conducted in obese older individuals, it is reported that aerobic or resistant exercises along with diet reduce BMI and increase quality of life [25].
In our study, in relation to the exercise training we applied to overweight and obese individuals, significant improvements were obtained in the parameters of physical functioning, limitations due to physical healt, energy, mental health, pain and general health perception on the SF-36 quality of life scale. These data are compatible with the literature. On the other hand, it has been observed that a statistically insignificant improvement can be obtained in emotional and social functions. We believe that the reason for the inability to achieve statistically significant development in these two parameters may be due to mandatory social constraints caused by the COVID-19 pandemic and our relatively shorter working time.
There are some limitations in our study which have been conducted during COVID-19 pandemic isolation period. Our study, which was carried out in April 2020 when the pandemic first started in our country and especially when physical activity was decreasing, was carried out in 6 weeks, covering the period when the first mandatory restrictions began and was completed. Therefore, our results covered this period. Another limitation of our study is that the result measurements evaluated before and after the study period were not performed face-to-face and were performed with less objective evaluation methods due to the fact that the study was conducted during COVID-19 pandemic.
During the isolation period of the COVID-19 pandemic, exercise training with telerehabilitation was one of the most ideal methods to be applied to obese individuals in this process in order to minimize the risk of transmission. As a result of our study, we found that exercise training with telerehabilitation had positive effects on physical fitness and quality of life in obese individuals by breaking the chains of inactivity during quarantine. According to our literature review, we believe that our study is important because it is the first study conducted in obese individuals using the telerehabilitation method and the study is able to show effective results. Further studies on how exercise training will affect obese individuals are also needed later in the pandemic.
References
World Health Organization[Internet]. Obesity[Updated 2020; cited 2020 Apr 18]. Available from: https://www.who.int/health-topics/obesity#tab=tab_1.
TC Sağlık Bakanlığı Halk Sağlığı Genel Müdürlüğü Sağlıklı Beslenme ve Hareketli Hayat Dairesi Başkanlığı. Obezitenin Nedenleri 2017 (Accessed: 20 April 2020) Available from: https://hsgm.saglik.gov.tr/tr/obezite/obezitenin-nedenleri.html.
Owen N, Sparling PB, Healy GN, Dunstan DW, Matthews CE. Sedentary behavior: emerging evidence for a new health risk. Mayo Clin Proc. 2010;85:1138–41.
Chen P, Mao L, Nassis GP, Harmer P, Ainsworth BE, Li F. Coronavirus disease (COVID-19): the need to maintain regular physical activity while taking precautions. J Sport Health Sci. 2020;9:103–4.
Kahraman T. Koronavirüs Hastalığı (COVID-19) Pandemisi ve Telerehabilitasyon. İzmir Katip Çelebi Üniversitesi Sağlık Bilimleri Fakültesi Dergisi. 2020;5:87–92.
The Physiotherapy Association of British Council (PABC) Physiotherapy Virtual Care Toolkit. https://bcphysio.org/telerehabilitation/pabc-physiotherapy-virtual-care-toolkit. Access: 01.12.2020.
College of Physical Therapists of British Columbia. Advice to Consider, COVID 19 and telerehabilitation. https://cptbc.org/physical-therapists/practice-resources/advice-to-consider/covid-19-and-tele-rehabilitation/ Access: 22.11.2020.
Jones CJ, Rikli RE. Measuring functional fitness in older adults. J Act Aging. 2002;25–30.
Ware JE Jr, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992;30:473–83.
Koçyiğit H, Aydemir Ö, Ölmez N, Memiş A. Kısa form-36 (KF36)’nın Türkçe versiyonunun güvenirliliği ve geçerliliği. İlaç ve Tedavi Dergisi. 1996;12:102–6.
Perme MP, Manevski D. Confidence intervals for the Mann–Whitney test. Stat Methods Med Res. 2019;28:3755–68.
Muscogiuri G, Pugliese G, Barrea L, Savastano S, Colao A. Commentary: obesity: The “Achilles heel” for COVID-19?. Metabolism. 2020;108:154–251.
Rychter AM, Zawada A, Ratajczak AE, Dobrowolska A, Krela-Kaźmierczak I. Should patients with obesity be more afraid of COVID-19? Obes Rev. 2020;21:e13083.
Rahmati-Ahmadabad S, Hosseini F. Exercise against SARS-CoV-2 (COVID-19): does workout intensity matter? (A mini review of some indirect evidence related to obesity). Obes Med. 2020;19:100245.
Hsu SL, Oda H, Shirahata S, Watanabe M, Sasaki M. Effects of core strength training on core stability. J Phys Ther Sci. 2018;30:1014–8.
Ulubay G. Solunum kas fizyolojisi ve kas gücü ölçümü. Toraks cerrahi bülteni. 2017;10:37–46.
Tongvichean T, Aungsuroch Y, Preechawong S. The effect of self-management exercise program on physical fitness among people with prehypertension and obesity: A Quasi Experiment Study. PRIJNR. 2018;23:6–17. https://he02.tci-thaijo.org/index.php/PRIJNR/article/view/108336.
Rayes ABR, de Lira CAB, Viana RB, Benedito-Silva AA, Vancini RL, Mascarin N. et al. The effects of Pilates vs. aerobic training on cardiorespiratory fitness, isokinetic muscular strength, body composition, and functional tasks outcomes for individuals who are overweight/obese: a clinical trial. PeerJ. 2019;7:e6022.
Yosmaoğlu HB, YAkut Y, Baltacı G. Fazla kilolu ve normal kilolu bireylerde alt ekstremite nöromusküler koordinasyon farklılıkları. Fizyoterapi Rehabilitasyon. 2011;22:249–54.
Hue O, Simoneau M, Marcotte J, Berrigan F, Doré J, Marceau P. et al. Body weight is a strong predictor of postural stability. Gait Posture. 2007;26:32–8. https://doi.org/10.1016/j.gaitpost.2006.07.005.
Pedersen BK, Saltin B. Exercise as medicine - evidence for prescribing exercise as therapy in 26 different chronic diseases. Scand J Med Sci Sports. 2015;3:1–72.
Dalle Grave R, Soave F, Ruocco A, Dametti L, Calugi S. Quality of life and physical performance in patients with obesity: a network analysis. Nutrients. 2020;12:602.
Vancini RL, Rayes ABR, Lira CAB, Sarro KJ, Andrade MS. Pilates and aerobic training improve levels of depression, anxiety and quality of life in overweight and obese individuals. Arq Neuropsiquiatr.2017;75:850–7.
Bilgin A, Kutlutürk S. Obez Kadınlarda Solunumla Kombine Yapılandırılmış Grup Egzersizlerinin Fiziksel Aktivite Düzeyi Üzerine Etkisi. Haliç Üniversitesi Sağlık Bilimleri Dergisi. 2021;4:99–106.
Villareal DT, Aguirre L, Gurney AB, Waters DL, Sinacore DR, Colombo E. et al. Aerobic or resistance exercise, or both, in dieting obese older adults. N Engl J Med. 2017;376:1943–55. https://doi.org/10.1056/NEJMoa1616338.
Author information
Authors and Affiliations
Contributions
OB: follow-up of the patients, performing exercise training, article writing. DN: consulting the study, follow-up of the patients, statistical analysis, article writing. All authors have read and approved the paper.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ozturk, B., Duruturk, N. Effect of telerehabilitation applied during COVID-19 isolation period on physical fitness and quality of life in overweight and obese individuals. Int J Obes 46, 95–99 (2022). https://doi.org/10.1038/s41366-021-00965-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41366-021-00965-5