Abstract
Background
Previous research has shown that sleep can play a role in obesity and weight loss. However, the association of sleep with weight loss in patients with severe obesity after bariatric surgery remains unexplored. We aimed to evaluate the role of sleep in weight loss evolution in a cohort of patients who underwent sleeve gastrectomy.
Methods
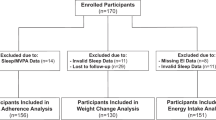
A cohort of 252 patients with severe obesity (75.7% women; age [mean ± SD] 47.7 ± 10.8 years; BMI 44.2 ± 5.9 kg/m2) was followed for 1 year after surgery. Anthropometric, biochemical, physical activity, sleep (bedtime, wakeup time, and sleep duration) and dietary intake variables were collected pre- and post-surgery (1 year). Linear and non-linear regression models were used to examine the associations between sleep variables and weight loss. Participants were grouped into ‘early’ and ‘late’ sleepers according to a bedtime threshold (before or after 24:00 h), and the differences in weight loss, physical activity, meal timing, and dietary intake between groups were studied.
Results
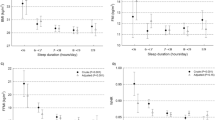
1-h increments in bedtime were linearly associated with less excess weight loss (EWL) [−2.23%; 95%CI: −3.37; −0.70; p = 0.005] 1 year after the sleeve gastrectomy. Late sleepers lost less weight (−5.64% of EWL [95%CI: −10.11; −1.17]; p = 0.014) when compared to early sleepers and showed a higher energy intake after 21:00 h (8.66% of total energy intake [95% CI: 4.87; 12.46]; p < 0.001).
Conclusions
Late bedtime is associated with less success of weight loss 1 year after the sleeve gastrectomy. Late sleepers consumed more of their calories closer to bedtime. Our results highlight the relevance of considering recommendations on bedtime and meal timing for patients after bariatric surgery.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Bentham J, Di Cesare M, Bilano V, Bixby H, Zhou B, Stevens GA, et al. Worldwide trends in body mass index, underweight, overweight, and obesity from 1975 to 2016: a pooled analysis of 2416 population-based measurement studies in 128·9 million children, adolescents, and adults. Lancet. 2017;390:2627–42.
Nguyen NT, Varela JE. Bariatric surgery for obesity and metabolic disorders: state of the art. Nat Rev Gastroenterol Hepatol. 2017;14:160–9.
Himpens J, Ramos A, Welbourn R, Dixon H, Kinsman R, Walton P. The 4th IFSO Global Registry Report 2018. Oxfordshire, United Kingdom; 2018.
Robinson A, Adler S, Stevens H, Darcy A, Morton J, Safer D. What variables are associated with successful weight loss outcomes for bariatric surgery after 1 year? Surg Obes Relat Dis. 2014;10:697–704.
Courcoulas A, Yanovski S, Bonds D, Eggerman T, Horlick M, Staten M. Long-term outcomes of bariatric surgery: a National Institutes of Health symposium. JAMA Surg. 2014;149:1323–9.
Holsen LM, Davidson P, Cerit H, Hye T, Moondra P, Haimovici F, et al. Neural predictors of 12-month weight loss outcomes following bariatric surgery. Int J Obes. 2018;42:785–93.
Wallwork A, Tremblay L, Chi M, Sockalingam S. Exploring partners’ experiences in living with patients who undergo bariatric surgery. Obes Surg. 2017;27:1973–81.
Ruíz-Lozano T, Vidal J, de Hollanda A, Scheer F, Garaulet M, Izquierdo-Pulido M. Timing of food intake is associated with weight loss evolution in severe obese patients after bariatric surgery. Clin Nutr. 2016;35:1308–14.
Ruíz-Lozano T, Vidal J, de Hollanda A, Canteras M, Garaulet M, Izquierdo-Pulido M. Evening chronotype associates with obesity in severely obese subjects: interaction with CLOCK 3111T/C. Int J Obes. 2016;40:1550–7.
Zuraikat FM, Thomas E, Roeshot D, Gallagher D, St-Onge MP. Can healthy sleep improve long-term bariatric surgery outcomes? Results of a pilot study and call for further research. Obesity. 2019;27:1769–71.
Martín E, Ruiz-Tovar J, Sánchez R. Vía Clínica de Cirugía Bariátrica 2017. Albacete, España; 2017.
Mechanick JI, Youdim A, Jones DB, Timothy Garvey W, Hurley DL, Molly McMahon M, et al. Clinical practice guidelines for the perioperative nutritional, metabolic, and nonsurgical support of the bariatric surgery patient-2013 update: Cosponsored by American Association of Clinical Endocrinologists, the Obesity Society, and American Society for. Endocr Pract. 2013;19:337–72.
Figura A, Ahnis A, Stengel A, Hofmann T, Elbelt U, Ordemann J. et al. Determinants of weight loss following laparoscopic sleeve gastrectomy: the role of psychological burden, coping style, and motivation to undergo surgery. J Obes. 2015;2015:626010
Cantós D, Farran-Codina A & Palma-Linares I. Programa de Càlcul Nutricional PCN Pro versió 1 [software]. University of Barcelona; 2013.
Farran-Codina A, Zamora RCP Tablas de Composición de Alimentos del CESNID [CESNID food-composition tables]. McGraw-Hil. Barcelona, Spain; 2004.
Mota MC, Silva C, Cristina L, Balieiro T, Gonçalves B, Fahmy W, et al. Association between social jetlag food consumption and meal times in patients with obesity-related chronic diseases. PLoS One. 2019;14:1–14.
Xiao Q, Garaulet M, Scheer FAJL. Meal timing and obesity: interactions with macronutrient intake and chronotype. Int J Obes. 2019;43:1701–11.
Roman-Viñas B, Serra-Majem L, Hagströmer M, Ribas-Barba L, Sjöström M, Segura-Cardona R. International Physical Activity Questionnaire: reliability and validity in a Spanish population. Eur J Sport Sci. 2010;10:297–304.
Horne JA, Ostberg O. A self-assessment questionnaire to determine morningness-eveningness in human circadian rhythms. Int J Chronobiol. 1976;4:97–110.
Bates D, Mächler M, Bolker B, Walker S. Fitting linear mixed-effects models using lme4. J Stat Softw. 2015;67:1–48.
R Core Team. R: A language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing; 2019. https://www.r-project.org/.
Kenny DA. Mediation [Internet]. 2018. http://davidakenny.net/cm/mediate.htm#RR. Accessed 8 Apr 2020.
Mascha EJ, Dalton JE, Kurz A, Saager L. Understanding the mechanism: mediation analysis in randomized and nonrandomized studies. Anesth Analg. 2013;117:980–94.
Hayes AJ. PROCESS Macro [Internet]. New York; 2018. http://www.processmacro.org.
Baron KG, Reid KJ, Kern AS, Zee PC. Role of sleep timing in caloric intake and BMI. Obesity. 2011;19:1374–81.
Lucassen EA, Zhao X, Rother KI, Mattingly MS, Courville AB, Jonge LDE, et al. Evening chronotype is associated with changes in eating behavior, more sleep apnea, and increased stress hormones in short sleeping obese individuals. PLoS One. 2013;8:e56519.
Baron KG, Reid KJ, Kim T, Van Horn L, Attarian H, Wolfe L, et al. Circadian timing and alignment in healthy adults: associations with BMI, body fat, caloric intake and physical activity. Int J Obes. 2017;41:203–9.
Roenneberg T, Allebrandt KV, Merrow M. Social Jetlag and obesity. Curr Biol. 2012;23:737.
Roenneberg T, Pilz LK, Zerbini G, Winnebeck ECChronotype. and Social Jetlag—a (self-) critical review. Biology. 2019;8:54.
Parsons MJ, Moffitt TE, Gregory AM, Goldman-Mellor S, Nolan PM, Poulton R, et al. Social jetlag, obesity and metabolic disorder: Investigation in a cohort study. Int J Obes. 2015;39:842–8.
Wong PM, Hasler BP, Kamarck TW, Muldoon MF, Manuck SB. Social Jetlag, chronotype, and cardiometabolic. Risk. 2015;100:4612–20.
Mota MC, Silva CM, Balieiro LCT, Fahmy WM, Crispim CA. Social jetlag and metabolic control in non-communicable chronic diseases: a study addressing different obesity statuses. Sci Rep. 2017;7:6358.
Jakubowicz D, Barnea M, Wainstein J, Froy O. High caloric intake at breakfast vs. dinner differentially influences weight loss of overweight and obese women. Obesity. 2013;21:2504–12.
Lombardo M, Bellia A, Padua E, Annino G, Gublielmi V, D’Adamo M, et al. Morning meal more efficient for fat loss in a 3-month lifestyle intervention. J Am Coll Nutr. 2014;33:198–205.
Keim NL, Van Loan MD, Horn WF, Barbieri TF, Mayclin PL. Weight loss is greater with consumption of large morning meals and fat-free mass is preserved with large evening meals in women on a controlled weight reduction regimen. J Nutr. 1997;127:75–82.
Madjd A, Taylor MA, Delavari A, Malekzadeh R, Macdonald IA, Farshchi HR. Beneficial effect of high energy intake at lunch rather than dinner on weight loss in healthy obese women in a weight-loss program: a randomized clinical trial. Am J Clin Nutr. 2016;104:982–9.
Wang JB, Patterson RE, Ang A, Emond JA, Shetty N, Arab L. Timing of energy intake during the day is associated with the risk of obesity in adults. J Hum Nutr Diet. 2014;27:255–62.
Baron KG, Reid KJ, Van Horn L, Zee PC. Contribution of evening macronutrient intake to total caloric intake and body mass index. Appetite. 2013;60:246–51.
Kutsuma A, Nakajima K, Suwa K. Potential association between breakfast skipping and concomitant late-night-dinner eating with metabolic syndrome and proteinuria in the Japanese population. Sci. 2014;2014:253581.
Fong M, Caterson ID, Madigan CD. Are large dinners associated with excess weight, and does eating a smaller dinner achieve greater weight loss? A systematic review and meta-analysis. Br J Nutr. 2017;118:616–28.
Beccuti G, Monagheddu C, Evangelista A, Ciccone G, Broglio F, Soldati L, et al. Timing of food intake: sounding the alarm about metabolic impairments? A systematic review. Pharmacol Res. 2017;125:132–41.
McCrory MA, Shaw AC, Lee JA. Energy and nutrient timing for weight control. Does timing of ingestion matter? Endocrinol Metab Clin. 2016;45:689–718.
St-Onge MP, Ard J, Baskin ML, Chiuve SE, Johnson HM, Kris-Etherton P, et al. Meal timing and frequency: implications for cardiovascular disease prevention: a scientific statement from the American Heart Association. Circulation. 2017;135:e96–121.
Mchill AW, Phillips AJK, Czeisler CA, Keating L, Yee K, Barger LK, et al. Later circadian timing of food intake is associated with increased body fat. Am J Clin Nutr. 2017;106:1213–9.
Morris CJ, Garcia JI, Myers S, Yang JN, Trienekens N, Scheer FA. The human circadian system has a dominating role in causing the morning/evening difference in diet-induced thermogenesis. Obesity. 2015;23:2053–8.
Lopez-Minguez J, Saxena R, Bandín C, Scheer FA, Garaulet M. Late dinner impairs glucose tolerance in MTNR1B risk allele carriers: a randomized, cross-over study. Clin Nutr. 2018;37:1133–40.
Chaix A, Manoogian ENC, Melkani GC, Panda S. Time-restricted eating to prevent and manage chronic metabolic diseases. Annu Rev Nutr. 2019;39:1–25.
Gill S, Panda S. A smartphone app reveals erratic diurnal eating patterns in humans that can be modulated for health benefits. Cell Metab. 2015;22:789–98.
Ross KM, Thomas JG, Wing RR. Successful weight loss maintenance associated with morning chronotype and better sleep quality. J Behav Med. 2016;39:465–71.
Giacchetti-Vega M, Baquerizo-VonBerswordts P, Carbone-Moane C, Bernabé-Ortiz A. Abandono de la terapia nutricional y pérdida de peso en pacientes bariátricos: cohorte retrospectiva en Lima. Perú. Rev Esp Nutr Humana Diet. 2017;21:18–28.
Michelini I, Falchi AG, Muggia C, Grecchi I, Montagna E, De Silvestri A, et al. Early dropout predictive factors in obesity treatment. Nutr Res Pract. 2014;8:94–102.
Acknowledgements
MFZR was supported by a scholarship from the ‘Consejo Nacional de Ciencia y Tecnologia’ CONACYT from Mexico. AH was supported by a Sara Borrell post-doctoral contract (CD17/00122) granted by the Instituto de Salud Carlos III (Spain).
Author information
Authors and Affiliations
Contributions
CB and MIP designed the study; CB and JFC acquired the data; CB, MFZR, AH and MIP analysed the data; CB, MFZR and MIP wrote the first draft; MFZR, AH, TC and MIP revised the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Barnadas-Solé, C., Zerón-Rugerio, M.F., Hernáez, Á. et al. Late bedtime is associated with lower weight loss in patients with severe obesity after sleeve gastrectomy. Int J Obes 45, 1967–1975 (2021). https://doi.org/10.1038/s41366-021-00859-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41366-021-00859-6