Abstract
Background
Prior research on the relationship between sleep and attempted weight loss failed to recognize the multidimensional nature of sleep. We examined the relationship between a composite measure of sleep health and change in weight and body composition among adults in a weight loss intervention.
Methods
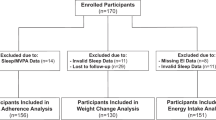
Adults (N = 125) with overweight or obesity (50.3 ± 10.6 years, 91% female, 81% white) participated in a 12-month behavioral weight loss intervention, with assessments of sleep, weight, fat mass, and fat-free mass at baseline, 6 months, and 12 months. Six sleep dimensions (regularity, satisfaction, alertness, timing, efficiency, and duration) were categorized as “good” or “poor” using questionnaires and actigraphy. A composite score was calculated by summing the number of “good” dimensions. Obstructive sleep apnea (OSA) was assessed in a subsample (n = 117), using the apnea–hypopnea index (AHI) to determine OSA severity. Linear mixed modeling was used to examine the relationships between sleep health and outcomes of percent weight, fat mass, or fat-free mass change during the subsequent 6-month interval, adjusting for age, sex, bed partner, and race; an additional model adjusted for AHI.
Results
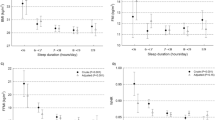
Mean baseline and 6-month sleep health was 4.5 ± 1.1 and 4.5 ± 1.2, respectively. Mean weight, fat mass, and fat-free mass changes from 0 to 6 months were −9.3 ± 6.1%, −16.9 ± 13.5%, and −3.4 ± 3.4%, respectively, and 0.4 ± 4.8%, −0.3 ± 10.3%, and 0.7 ± 4.1% from 6 to 12 months. Better sleep health was associated with greater subsequent weight loss (P = 0.016) and fat loss (P = 0.006), but not fat-free mass loss (P = 0.232). Following AHI adjustment, the association between sleep health and weight loss was attenuated (P = 0.102) but remained significant with fat loss (P = 0.040). Regularity, satisfaction, timing, and efficiency were each associated with weight and/or fat loss (P ≤ 0.041).
Conclusions
Better sleep health was associated with greater weight and fat loss, with associations attenuated after accounting for OSA severity. Future studies should explore whether improving sleep health, OSA, or the combination improves weight loss.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Ng M, Fleming T, Robinson M, Thomson B, Graetz N, Margono C, et al. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980-2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2014;384:766–81.
Hales CM, Carroll MD, Fryar CD, Ogden CL. Prevalence of obesity and severe obesity among adults: United States, 2017–2018. NCHS Data Brief, no 360. Hyattsville, MD: National Center for Health Statistics; 2020.
Abdelaal M, le Roux CW, Docherty NG. Morbidity and mortality associated with obesity. Ann Transl Med. 2017;5:161.
Afshin A, Forouzanfar MH, Reitsma MB, Sur P, Estep K, Lee A, et al. Health effects of overweight and obesity in 195 countries over 25 years. N Engl J Med. 2017;377:13–27.
Jensen MD, Ryan DH, Apovian CM, Ard JD, Comuzzie AG, Donato KA, et al. 2013 AHA/ACC/TOS guideline for the management of overweight and obesity in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and The Obesity Society. J Am Coll Cardiol. 2014;63:2985–3023.
Lv N, Azar KMJ, Rosas LG, Wulfovich S, Xiao L, Ma J. Behavioral lifestyle interventions for moderate and severe obesity: a systematic review. Prev Med. 2017;100:180–93.
MacLean PS, Wing RR, Davidson T, Epstein L, Goodpaster B, Hall KD, et al. NIH working group report: innovative research to improve maintenance of weight loss. Obesity. 2015;23:7–15.
Lytle LA, Nicastro HL, Roberts SB, Evans M, Jakicic JM, Laposky AD, et al. Accumulating Data to Optimally Predict Obesity Treatment (ADOPT) core measures: behavioral domain. Obesity. 2018;26:S16–24.
Leger D, Bayon V, de Sanctis A. The role of sleep in the regulation of body weight. Mol Cell Endocrinol. 2015;418:101–7.
Wu Y, Zhai L, Zhang D. Sleep duration and obesity among adults: a meta-analysis of prospective studies. Sleep Med. 2014;15:1456–62.
Capers PL, Fobian AD, Kaiser KA, Borah R, Allison DB. A systematic review and meta-analysis of randomized controlled trials of the impact of sleep duration on adiposity and components of energy balance. Obes Rev. 2015;16:771–82.
Sun W, Yuan J, Yu Y, Wang Z, Shankar N, Ali G, et al. Poor sleep quality associated with obesity in men. Sleep Breath. 2016;20:873–80.
Baron KG, Reid KJ, Kern AS, Zee PC. Role of sleep timing in caloric intake and BMI. Obesity. 2011;19:1374–81.
Wirth MD, Hebert JR, Hand GA, Youngstedt SD, Hurley TG, Shook RP, et al. Association between actigraphic sleep metrics and body composition. Ann Epidemiol. 2015;25:773–8.
Ogilvie RP, Redline S, Bertoni AG, Chen X, Ouyang P, Szklo M, et al. Actigraphy measured sleep indices and adiposity: the Multi-Ethnic Study of Atherosclerosis (MESA). Sleep. 2016;39:1701–8.
Sawamoto R, Nozaki T, Furukawa T, Tanahashi T, Morita C, Hata T, et al. Higher sleep fragmentation predicts a lower magnitude of weight loss in overweight and obese women participating in a weight-loss intervention. Nutr Diabetes. 2014;4:e144.
Elder CR, Gullion CM, Funk KL, Debar LL, Lindberg NM, Stevens VJ. Impact of sleep, screen time, depression and stress on weight change in the intensive weight loss phase of the LIFE study. Int J Obes. 2012;36:86–92.
Chaput JP, Tremblay A. Sleeping habits predict the magnitude of fat loss in adults exposed to moderate caloric restriction. Obes Facts. 2012;5:561–6.
Thomson CA, Morrow KL, Flatt SW, Wertheim BC, Perfect MM, Ravia JJ, et al. Relationship between sleep quality and quantity and weight loss in women participating in a weight-loss intervention trial. Obesity. 2012;20:1419–25.
Papandreou C, Bullo M, Diaz-Lopez A, Martinez-Gonzalez MA, Corella D, Castaner O, et al. High sleep variability predicts a blunted weight loss response and short sleep duration a reduced decrease in waist circumference in the PREDIMED-Plus Trial. Int J Obes. 2020;44:330–9.
O’Brien EM, Fava J, Subak LL, Stone K, Hart CN, Demos K, et al. Sleep duration and weight loss among overweight/obese women enrolled in a behavioral weight loss program. Nutr Diabetes. 2012;2:e43.
Tuomilehto H, Peltonen M, Partinen M, Lavigne G, Eriksson JG, Herder C, et al. Sleep duration, lifestyle intervention, and incidence of type 2 diabetes in impaired glucose tolerance: the Finnish Diabetes Prevention Study. Diabetes Care. 2009;32:1965–71.
Chang MW, Tan A, Schaffir J, Wegener DT. Sleep and weight loss in low-income overweight or obese postpartum women. BMC Obes. 2019;6:12.
Matthews KA, Patel SR, Pantesco EJ, Buysse DJ, Kamarck TW, Lee L, et al. Similarities and differences in estimates of sleep duration by polysomnography, actigraphy, diary, and self-reported habitual sleep in a community sample. Sleep Health. 2018;4:96–103.
Kline CE, Burke LE, Sereika SM, Imes CC, Rockette-Wagner B, Mendez DD, et al. Bidirectional relationships between weight change and sleep apnea in a behavioral weight loss intervention. Mayo Clin Proc. 2018;93:1290–8.
Buysse DJ. Sleep health: can we define it? Does it matter? Sleep. 2014;37:9–17.
Burke LE, Shiffman S, Music E, Styn MA, Kriska A, Smailagic A, et al. Ecological momentary assessment in behavioral research: addressing technological and human participant challenges. J Med Internet Res. 2017;19:e77.
Brindle RC, Cribbet MR, Samuelsson LB, Gao C, Frank E, Krafty RT, et al. The relationship between childhood trauma and poor sleep health in adulthood. Psychosom Med. 2018;80:200–7.
Brindle RC, Yu L, Buysse DJ, Hall MH. Empirical derivation of cut-off values for the sleep health metric and its relationship to cardiometabolic morbidity: results from the Midlife in the United States (MIDUS) study. Sleep. 2019;42:zsz116.
Wallace ML, Stone K, Smagula SF, Hall MH, Simsek B, Kado DM, et al. Which sleep health characteristics predict all-cause mortality in older men? An application of flexible multivariable approaches. Sleep. 2018;41:zsx189.
Irish LA, Kline CE, Gunn HE, Buysse DJ, Hall MH. The role of sleep hygiene in promoting public health: a review of empirical evidence. Sleep Med Rev. 2015;22:23–36.
Manber R, Bootzin RR, Acebo C, Carskadon MA. The effects of regularizing sleep-wake schedules on daytime sleepiness. Sleep. 1996;19:432–41.
Buysse DJ, Reynolds CF III, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28:193–213.
Johns MW. A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep. 1991;14:540–5.
Baron KG, Reid KJ. Circadian misalignment and health. Int Rev Psychiatry. 2014;26:139–54.
Chen X, Wang R, Zee P, Lutsey PL, Javaheri S, Alcantara C, et al. Racial/ethnic differences in sleep disturbances: the Multi-Ethnic Study of Atherosclerosis (MESA). Sleep. 2015;38:877–88.
Beattie L, Espie CA, Kyle SD, Biello SM. How are normal sleeping controls selected? A systematic review of cross-sectional insomnia studies and a standardized method to select healthy controls for sleep research. Sleep Med. 2015;16:669–77.
Hirshkowitz M, Whiton K, Albert SM, Alessi C, Bruni O, DonCarlos L, et al. National Sleep Foundation’s updated sleep duration recommendations: final report. Sleep Health. 2015;1:233–43.
Lauderdale DS, Knutson KL, Yan LL, Liu K, Rathouz PJ. Self-reported and measured sleep duration: how similar are they? Epidemiology. 2008;19:838–45.
Patel SR, Weng J, Rueschman M, Dudley KA, Loredo JS, Mossavar-Rahmani Y, et al. Reproducibility of a standardized actigraphy scoring algorithm for sleep in a US Hispanic/Latino population. Sleep. 2015;38:1497–503.
Kushida CA, Chang A, Gadkary C, Guilleminault C, Carrillo O, Dement WC. Comparison of actigraphic, polysomnographic, and subjective assessment of sleep parameters in sleep-disordered patients. Sleep Med. 2001;2:389–96.
Oktay B, Rice TB, Atwood CW Jr, Passero M Jr, Gupta N, Givelber R, et al. Evaluation of a single-channel portable monitor for the diagnosis of obstructive sleep apnea. J Clin Sleep Med. 2011;7:384–90.
Redline S, Kirchner HL, Quan SF, Gottlieb DJ, Kapur V, Newman A. The effects of age, sex, ethnicity, and sleep-disordered breathing on sleep architecture. Arch Intern Med. 2004;164:406–18.
Varkevisser RDM, van Stralen MM, Kroeze W, Ket JCF, Steenhuis IHM. Determinants of weight loss maintenance: a systematic review. Obes Rev. 2019;20:171–211.
Yu H, Lu J, Jia P, Liu C, Cheng J. Experimental sleep restriction effect on adult body weight: a meta-analysis. Sleep Breath. 2019;23:1341–50.
DeSantis AS, Dubowitz T, Ghosh-Dastidar B, Hunter GP, Buman M, Buysse DJ, et al. A preliminary study of a composite sleep health score: associations with psychological distress, body mass index, and physical functioning in a low-income African American community. Sleep Health. 2019;5:514–20.
Bowman MA, Brindle RC, Joffe H, Kline CE, Buysse DJ, Appelhans BM, et al. Multidimensional sleep health is not cross-sectionally or longitudinally associated with adiposity in the Study of Women’s Health Across the Nation. Sleep Health. 2020;6:790–6.
Dong L, Martinez AJ, Buysse DJ, Harvey AG. A composite measure of sleep health predicts concurrent mental and physical health outcomes in adolescents prone to eveningness. Sleep Health. 2019;5:166–74.
Nedeltcheva AV, Kilkus JM, Imperial J, Schoeller DA, Penev PD. Insufficient sleep undermines dietary efforts to reduce adiposity. Ann Intern Med. 2010;153:435–41.
Wang X, Sparks JR, Bowyer KP, Youngstedt SD. Influence of sleep restriction on weight loss outcomes associated with caloric restriction. Sleep. 2018;41:zsy027.
Stiegler P, Cunliffe A. The role of diet and exercise for the maintenance of fat-free mass and resting metabolic rate during weight loss. Sports Med. 2006;36:239–62.
Furihata R, Hall MH, Stone KL, Ancoli-Israel S, Smagula SF, Cauley JA, et al. An aggregate measure of sleep health is associated with prevalent and incident clinically significant depression symptoms among community-dwelling older women. Sleep. 2017;40:zsw075.
Dalmases M, Benitez I, Sapina-Beltran E, Garcia-Codina O, Medina-Bustos A, Escarrabill J, et al. Impact of sleep health on self-perceived health status. Sci Rep. 2019;9:7284.
Patel SR, Hayes AL, Blackwell T, Evans DS, Ancoli-Israel S, Wing YK, et al. The association between sleep patterns and obesity in older adults. Int J Obes. 2014;38:1159–64.
Sasaki N, Fujiwara S, Yamashita H, Ozono R, Monzen Y, Teramen K, et al. Association between obesity and self-reported sleep duration variability, sleep timing, and age in the Japanese population. Obes Res Clin Pract. 2018;12:187–94.
Kim M, Sasai H, Kojima N, Kim H. Objectively measured night-to-night sleep variations are associated with body composition in very elderly women. J Sleep Res. 2015;24:639–47.
Bailey BW, Allen MD, LeCheminant JD, Tucker LA, Errico WK, Christensen WF, et al. Objectively measured sleep patterns in young adult women and the relationship to adiposity. Am J Health Promot. 2014;29:46–54.
Logue EE, Scott ED, Palmieri PA, Dudley P. Sleep duration, quality, or stability and obesity in an urban family medicine center. J Clin Sleep Med. 2014;10:177–82.
Kobayashi D, Takahashi O, Shimbo T, Okubo T, Arioka H, Fukui T. High sleep duration variability is an independent risk factor for weight gain. Sleep Breath. 2013;17:167–72.
McHill AW, Wright KP Jr. Role of sleep and circadian disruption on energy expenditure and in metabolic predisposition to human obesity and metabolic disease. Obes Rev. 2017;18S:15–24.
Garaulet M, Corbalan MD, Madrid JA, Morales E, Baraza JC, Lee YC, et al. CLOCK gene is implicated in weight reduction in obese patients participating in a dietary programme based on the Mediterranean diet. Int J Obes. 2010;34:516–23.
Garaulet M, Esteban Tardido A, Lee YC, Smith CE, Parnell LD, Ordovas JM. SIRT1 and CLOCK 3111T>C combined genotype is associated with evening preference and weight loss resistance in a behavioral therapy treatment for obesity. Int J Obes. 2012;36:1436–41.
Seneviratne U, Puvanendran K. Excessive daytime sleepiness in obstructive sleep apnea: prevalence, severity, and predictors. Sleep Med. 2004;5:339–43.
Chin K, Oga T, Takahashi K, Takegami M, Nakayama-Ashida Y, Wakamura T, et al. Associations between obstructive sleep apnea, metabolic syndrome, and sleep duration, as measured with an actigraph, in an urban male working population in Japan. Sleep. 2010;33:89–95.
Borel AL, Leblanc X, Almeras N, Tremblay A, Bergeron J, Poirier P, et al. Sleep apnoea attenuates the effects of a lifestyle intervention programme in men with visceral obesity. Thorax. 2012;67:735–41.
St-Onge MP, Shechter A. Sleep disturbances, body fat distribution, food intake and/or energy expenditure: pathophysiological aspects. Horm Mol Biol Clin Investig. 2014;17:29–37.
Spaeth AM, Dinges DF, Goel N. Effects of experimental sleep restriction on weight gain, caloric intake, and meal timing in healthy adults. Sleep. 2013;36:981–90.
Shechter A, St-Onge MP. Delayed sleep timing is associated with low levels of free-living physical activity in normal sleeping adults. Sleep Med. 2014;15:1586–9.
Coughlin JW, Smith MT. Sleep, obesity, and weight loss in adults: is there a rationale for providing sleep interventions in the treatment of obesity? Int Rev Psychiatry. 2014;26:177–88.
Logue EE, Bourguet CC, Palmieri PA, Scott ED, Matthews BA, Dudley P, et al. The better weight-better sleep study: a pilot intervention in primary care. Am J Health Behav. 2012;36:319–34.
Tasali E, Chapotot F, Wroblewski K, Schoeller D. The effects of extended bedtimes on sleep duration and food desire in overweight young adults: a home-based intervention. Appetite. 2014;80:220–4.
Al Khatib HK, Hall WL, Creedon A, Ooi E, Masri T, McGowan L, et al. Sleep extension is a feasible lifestyle intervention in free-living adults who are habitually short sleepers: a potential strategy for decreasing intake of free sugars? A randomized controlled pilot study. Am J Clin Nutr. 2018;107:43–53.
Jackson CL. Determinants of racial/ethnic disparities in disordered sleep and obesity. Sleep Health. 2017;3:401–15.
Matricciani L, Bin YS, Lallukka T, Kronholm E, Wake M, Paquet C, et al. Rethinking the sleep-health link. Sleep Health. 2018;4:339–48.
Funding
Funding for this study was provided by National Institutes of Health (NIH) grant R01HL107370 (PI: LEB). Additional investigator support for CEK, DDM, and ERC was provided by NIH grants K23HL118318 (PI: CEK), R01HL107370-S1 (PI: DDM), and K24NR016685 (PI: ERC). The ApneaLink Plus devices used in this study were donated by ResMed, Inc. ResMed had no role in the study design, data collection and analysis, decision to publish, or preparation of the paper.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
In the past 3 years, DJB has served as a paid consultant to Bayer, BeHealth Solutions, Emmi Solutions, Weight Watchers International, and Pear Therapeutics. He has served as a paid consultant for professional educational programs developed by the American Academy of Physician Assistants, CME Institute, and Emmi Solutions, and received payment for a professional education program sponsored by Eisai. DJB is an author of the PSQI, Pittsburgh Sleep Quality Index Addendum for PTSD (PSQI-A), Brief Pittsburgh Sleep Quality Index (B-PSQI), Daytime Insomnia Symptoms Scale, Pittsburgh Sleep Diary, Insomnia Symptom Questionnaire, and RU_SATED (copyright held by University of Pittsburgh). These instruments have been licensed to commercial entities for fees. He is also co-author of the Consensus Sleep Diary (copyright held by Ryerson University), which is licensed to commercial entities for a fee. No other authors report any conflicts of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Kline, C.E., Chasens, E.R., Bizhanova, Z. et al. The association between sleep health and weight change during a 12-month behavioral weight loss intervention. Int J Obes 45, 639–649 (2021). https://doi.org/10.1038/s41366-020-00728-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41366-020-00728-8
This article is cited by
-
Effect of sleep on weight loss and adherence to diet and physical activity recommendations during an 18-month behavioral weight loss intervention
International Journal of Obesity (2022)
-
Sleep characteristics modify the associations of physical activity during pregnancy and gestational weight gain
Archives of Gynecology and Obstetrics (2022)
-
Predictors of weight loss in obese patients with obstructive sleep apnea
Sleep and Breathing (2022)