Abstract
Background
Excessive adiposity provides an inflammatory environment. However, in people with severe obesity, how systemic and local adipose tissue (AT)-derived cytokines contribute to worsening glucose tolerance is not clear.
Methods
Ninty-two severely obese (SO) individuals undergoing bariatric surgery were enrolled and subjected to detailed clinical phenotyping. Following an oral glucose tolerance test, participants were included in three groups, based on the presence of normal glucose tolerance (NGT), impaired glucose tolerance (IGT), or type 2 diabetes (T2D). Serum and subcutaneous AT (SAT) biopsies were obtained and mesenchymal stem cells (MSCs) were isolated, characterized, and differentiated in adipocytes in vitro. TNFA and PPARG mRNA levels were determined by qRT-PCR. Circulating, adipocyte- and MSC-released cytokines, chemokines, and growth factors were assessed by multiplex ELISA.
Results
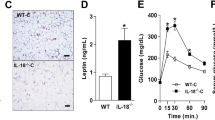
Serum levels of IL-9, IL-13, and MIP-1β were increased in SO individuals with T2D, as compared with those with either IGT or NGT. At variance, SAT samples obtained from SO individuals with IGT displayed levels of TNFA which were threefold higher compared to those with NGT, but not different from those with T2D. Elevated levels of TNFα were also found in differentiated adipocytes, isolated from the SAT specimens of individuals with IGT and T2D, compared to those with NGT. Consistent with the pro-inflammatory milieu, IL-1β and IP-10 secretion was significantly higher in adipocytes from individuals with IGT and T2D. Moreover, increased levels of TNFα, both mRNA and secreted protein were detected in MSCs obtained from IGT and T2D, compared to NGT SO individuals. Exposure of T2D and IGT-derived MSCs to the anti-inflammatory flavonoid quercetin reduced TNFα levels and was paralleled by a significant decrease of the secretion of inflammatory cytokines.
Conclusion
In severe obesity, enhanced SAT-derived inflammatory phenotype is an early step in the progression toward T2D and maybe, at least in part, attenuated by quercetin.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Saeedi P, Petersohn I, Salpea P, Malanda B, Karuranga S, Unwin N, et al. Global and regional diabetes prevalence estimates for 2019 and projections for 2030 and 2045: results from the international diabetes federation diabetes atlas, 9(th) edition. Diab Res Clin Pract. 2019;157:107843.
Chooi YC, Ding C, Magkos F. The epidemiology of obesity. Metabolism. 2019;92:6–10.
Schernthaner G, Morton JM. Bariatric surgery in patients with morbid obesity and type 2 diabetes. Diabetes Care. 2008;31:S297–302.
Silveira EA, de Souza Rosa LP, de Carvalho Santos A, de Souza Cardoso CK, Noll M. Type 2 diabetes mellitus in class II and III obesity: prevalence, associated factors, and correlation between glycemic parameters and body mass index. Int J Environ Res Public Health. 2020;17:11.
D’Esposito V, Ambrosio MR, Giuliano M, Cabaro S, Miele C, Beguinot F, et al. Mammary adipose tissue control of breast cancer progression: impact of obesity and diabetes. Front Oncol. 2020;10:1554.
Funcke JB, Scherer PE. Beyond adiponectin and leptin: adipose tissue-derived mediators of inter-organ communication. J Lipid Res. 2019;60:1648–84.
Poulos SP, Hausman DB, Hausman GJ. The development and endocrine functions of adipose tissue. Mol Cell Endocrinol. 2010;323:20–34.
Smith U, Kahn BB. Adipose tissue regulates insulin sensitivity: role of adipogenesis, de novo lipogenesis and novel lipids. J Intern Med. 2016;280:465–75.
Kusminski CM, Bickel PE, Scherer PE. Targeting adipose tissue in the treatment of obesity-associated diabetes. Nat Rev Drug Discov. 2016;15:639–60.
Hotamisligil GS, Spiegelman BM. Tumor necrosis factor alpha: a key component of the obesity-diabetes link. Diabetes. 1994;43:1271–8.
Li D, Zhang T, Lu J, Peng C, Lin L. Natural constituents from food sources as therapeutic agents for obesity and metabolic diseases targeting adipose tissue inflammation. Crit Rev Food Sci Nutr. 2020: 1–19.
Li Y, Yao J, Han C, Yang J, Chaudhry MT, Wang S, et al. Quercetin, inflammation and immunity. Nutrients. 2016;8:167.
Chen S, Jiang H, Wu X, Fang J. Therapeutic effects of quercetin on inflammation, obesity, and type 2 diabetes. Med Inflamm. 2016;2016:9340637.
Nettore IC, Rocca C, Mancino G, Albano L, Amelio D, Grande F, et al. Quercetin and its derivative Q2 modulate chromatin dynamics in adipogenesis and Q2 prevents obesity and metabolic disorders in rats. J Nutr Biochem. 2019;69:151–62.
Xu M, Pirtskhalava T, Farr JN, Weigand BM, Palmer AK, Weivoda MM, et al. Senolytics improve physical function and increase lifespan in old age. Nat Med. 2018;24:1246–56.
Eckel RH, Kahn SE, Ferrannini E, Goldfine AB, Nathan DM, Schwartz MW, et al. Obesity and type 2 diabetes: what can be unified and what needs to be individualized? Diabetes Care. 2011;34:1424–30.
Zatterale F, Longo M, Naderi J, Raciti GA, Desiderio A, Miele C, et al. Chronic adipose tissue inflammation linking obesity to insulin resistance and type 2 diabetes. Front Physiol. 2019;10:1607.
American Diabetes A. Diagnosis and classification of diabetes mellitus. Diabetes Care. 2014;37:S81–90.
D’Esposito V, Lecce M, Marenzi G, Cabaro S, Ambrosio MR, Sammartino G, et al. Platelet-rich plasma counteracts detrimental effect of high-glucose concentrations on mesenchymal stem cells from Bichat fat pad. J Tissue Eng Regener Med. 2020;14:701–13.
de Girolamo L, Lucarelli E, Alessandri G, Avanzini MA, Bernardo ME, Biagi E, et al. Mesenchymal stem/stromal cells: a new “cells as drugs” paradigm. Efficacy and critical aspects in cell therapy. Curr Pharmaceut Des. 2013;19:2459–73.
Aprile M, Ambrosio MR, D’Esposito V, Beguinot F, Formisano P, Costa V, et al. PPARG in human adipogenesis: differential contribution of canonical transcripts and dominant negative isoforms. PPAR Res. 2014;2014:537865.
Caso F, Postiglione L, Covelli B, Ricciardone M, Di Spigna G, Formisano P, et al. Pro-inflammatory adipokine profile in psoriatic arthritis: results from a cross-sectional study comparing PsA subset with evident cutaneous involvement and subset “sine psoriasis”. Clin Rheumatol. 2019;38:2547–52.
Pisano S, Catone G, Coppola G, Carotenuto M, Iuliano R, Tiano C, et al. Different immune signature in youths experiencing antipsychotic-induced weight gain compared to untreated obese patients. J Child Adolesc Psychopharmacol. 2017;27:844–8.
Ambrosio MR, D’Esposito V, Costa V, Liguoro D, Collina F, Cantile M, et al. Glucose impairs tamoxifen responsiveness modulating connective tissue growth factor in breast cancer cells. Oncotarget. 2017;8:109000–17.
Vinciguerra F, Baratta R, Farina MG, Tita P, Padova G, Vigneri R, et al. Very severely obese patients have a high prevalence of type 2 diabetes mellitus and cardiovascular disease. Acta Diabetol. 2013;50:443–9.
Catoi AF, Busetto L. Metabolically healthy obesity and bariatric surgery. Obes Surg. 2019;29:2989–3000.
Dalmas E, Rouault C, Abdennour M, Rovere C, Rizkalla S, Bar-Hen A, et al. Variations in circulating inflammatory factors are related to changes in calorie and carbohydrate intakes early in the course of surgery-induced weight reduction. Am J Clin Nutr. 2011;94:450–8.
Schmidt FM, Weschenfelder J, Sander C, Minkwitz J, Thormann J, Chittka T, et al. Inflammatory cytokines in general and central obesity and modulating effects of physical activity. PLoS ONE. 2015;10:e0121971.
van der Zalm IJB, van der Valk ES, Wester VL, Nagtzaam NMA, van Rossum EFC, Leenen PJM, et al. Obesity-associated T-cell and macrophage activation improve partly after a lifestyle intervention. Int J Obes. 2020;44:1838–50.
Chakraborty S, Kubatzky KF, Mitra DK. An update on interleukin-9: from its cellular source and signal transduction to its role in immunopathogenesis. Int J Mol Sci. 2019;20:9.
Stechova K, Halbhuber Z, Hubackova M, Kayserova J, Petruzelkova L, Vcelakova J, et al. Case report: type 1 diabetes in monozygotic quadruplets. Eur J Hum Genet. 2012;20:457–62.
Chang TT, Chen JW. Emerging role of chemokine CC motif ligand 4 related mechanisms in diabetes mellitus and cardiovascular disease: friends or foes? Cardiovasc Diabetol. 2016;15:117.
Jiang LQ, Franck N, Egan B, Sjogren RJ, Katayama M, Duque-Guimaraes D, et al. Autocrine role of interleukin-13 on skeletal muscle glucose metabolism in type 2 diabetic patients involves microRNA let-7. Am J Physiol Endocrinol Metab. 2013;305:E1359–66.
Parisi V, Cabaro S, D’Esposito V, Petraglia L, Conte M, Campana P, et al. Epicardial adipose tissue and IL-13 response to myocardial injury drives left ventricular remodeling after ST elevation myocardial infarction. Front Physiol. 2020;11:575181.
Chen H, Wen F, Zhang X, Su SB. Expression of T-helper-associated cytokines in patients with type 2 diabetes mellitus with retinopathy. Mol Vis. 2012;18:219–26.
Crewe C, An YA, Scherer PE. The ominous triad of adipose tissue dysfunction: inflammation, fibrosis, and impaired angiogenesis. J Clin Investig. 2017;127:74–82.
Bullo M, Garcia-Lorda P, Peinado-Onsurbe J, Hernandez M, Del Castillo D, Argiles JM, et al. TNFalpha expression of subcutaneous adipose tissue in obese and morbid obese females: relationship to adipocyte LPL activity and leptin synthesis. Int J Obesity Relat Metab Disord. 2002;26:652–8.
Hoffstedt J, Arner E, Wahrenberg H, Andersson DP, Qvisth V, Lofgren P, et al. Regional impact of adipose tissue morphology on the metabolic profile in morbid obesity. Diabetologia. 2010;53:2496–503.
Katsuki A, Sumida Y, Murashima S, Murata K, Takarada Y, Ito K, et al. Serum levels of tumor necrosis factor-alpha are increased in obese patients with noninsulin-dependent diabetes mellitus. J Clin Endocrinol Metab. 1998;83:859–62.
Febbraio MA. Role of interleukins in obesity: implications for metabolic disease. Trends Endocrinol Metab. 2014;25:312–9.
Narumi S, Yoneyama H, Inadera H, Nishioji K, Itoh Y, Okanoue T, et al. TNF-alpha is a potent inducer for IFN-inducible protein-10 in hepatocytes and unaffected by GM-CSF in vivo, in contrast to IL-1beta and IFN-gamma. Cytokine. 2000;12:1007–16.
Parisi V, Petraglia L, Cabaro S, D’Esposito V, Bruzzese D, Ferraro G, et al. Imbalance between interleukin-1beta and interleukin-1 receptor antagonist in epicardial adipose tissue is associated with non ST-segment elevation acute coronary syndrome. Front Physiol. 2020;11:42.
Hueso L, Ortega R, Selles F, Wu-Xiong NY, Ortega J, Civera M, et al. Upregulation of angiostatic chemokines IP-10/CXCL10 and I-TAC/CXCL11 in human obesity and their implication for adipose tissue angiogenesis. Int J Obes. 2018;42:1406–17.
Ejarque M, Ceperuelo-Mallafre V, Serena C, Maymo-Masip E, Duran X, Diaz-Ramos A, et al. Adipose tissue mitochondrial dysfunction in human obesity is linked to a specific DNA methylation signature in adipose-derived stem cells. Int J Obes. 2019;43:1256–68.
Longo M, Zatterale F, Naderi J, Parrillo L, Formisano P, Raciti GA, et al. Adipose tissue dysfunction as determinant of obesity-associated metabolic complications. Int J Mol Sci. 2019;20:9.
Aprile M, Cataldi S, Ambrosio MR, D’Esposito V, Lim K, Dietrich A, et al. PPARγΔ5, a naturally occurring dominant-negative splice isoform, impairs PPARγ function and adipocyte differentiation. Cell Rep. 2018;25:1577–92 e6.
Aprile M, Cataldi S, Perfetto C, Ambrosio MR, Italiani P, Tate R. et al. In-vitro-generated hypertrophic-like adipocytes displaying PPARG isoforms unbalance recapitulate adipocyte dysfunctions in vivo. Cells. 2020;9:5
D’Esposito V, Passaretti F, Hammarstedt A, Liguoro D, Terracciano D, Molea G, et al. Adipocyte-released insulin-like growth factor-1 is regulated by glucose and fatty acids and controls breast cancer cell growth in vitro. Diabetologia. 2012;55:2811–22.
Ronningen T, Shah A, Reiner AH, Collas P, Moskaug JO. Epigenetic priming of inflammatory response genes by high glucose in adipose progenitor cells. Biochem Biophys Res Commun. 2015;467:979–86.
Raciti GA, Spinelli R, Desiderio A, Longo M, Parrillo L, Nigro C, et al. Specific CpG hyper-methylation leads to Ankrd26 gene down-regulation in white adipose tissue of a mouse model of diet-induced obesity. Sci Rep. 2017;7:43526.
Gowers IR, Walters K, Kiss-Toth E, Read RC, Duff GW, Wilson AG. Age-related loss of CpG methylation in the tumour necrosis factor promoter. Cytokine. 2011;56:792–7.
Rancourt RC, Ott R, Ziska T, Schellong K, Melchior K, Henrich W, et al. Visceral adipose tissue inflammatory factors (TNF-Alpha, SOCS3) in gestational diabetes (GDM): epigenetics as a clue in GDM pathophysiology. Int J Mol Sci. 2020;21:2.
Palmer AK, Xu M, Zhu Y, Pirtskhalava T, Weivoda MM, Hachfeld CM, et al. Targeting senescent cells alleviates obesity-induced metabolic dysfunction. Aging Cell. 2019;18:e12950.
Lee Y, Song YS, Fang CH, So BI, Park JY, Joo HW, et al. Anti-obesity effects of granulocyte-colony stimulating factor in Otsuka-Long-Evans-Tokushima fatty rats. PLoS ONE. 2014;9:e105603.
Spoto B, Di Betta E, Mattace-Raso F, Sijbrands E, Vilardi A, Parlongo RM, et al. Pro- and anti-inflammatory cytokine gene expression in subcutaneous and visceral fat in severe obesity. Nutr Metab Cardiovasc Dis. 2014;24:1137–43.
Acknowledgements
The authors wish to thank Dr. Virginia Tagliamonte, Dr. Vincenzo Cosimato, and Dr. Aniello Rainone involved in patient enrollment and clinical phenotyping and in the management of the clinical records.
Funding
This work was supported by the Regione Campania POR FESR 2014–2020–Objective 1.2.—Realization of Technology Platform to fight oncologic diseases (RARE PLAT NET, SATIN, and COEPICA Projects) and by the Italian Association for the Cancer Research—AIRC (grant IG19001).
Author information
Authors and Affiliations
Contributions
VE: conceptualization, investigation, data curation, formal analysis, writing—original draft, writing—review & editing. MRA: conceptualization, investigation, data curation. DL: investigation, methodology. GP: investigation. ML: investigation, formal analysis. SC: investigation, writing—review & editing. MA: investigation. AM: data curation. VP: investigation. PF: conceptualization, supervision. CM: funding acquisition, supervision. DB: data curation, formal analysis. DT: project administration, supervision. FB: funding acquisition, resources. PF: conceptualization; funding acquisition; project administration; resources; supervision, writing—original draft; writing—review & editing.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
D’Esposito, V., Ambrosio, M.R., Liguoro, D. et al. In severe obesity, subcutaneous adipose tissue cell-derived cytokines are early markers of impaired glucose tolerance and are modulated by quercetin. Int J Obes 45, 1811–1820 (2021). https://doi.org/10.1038/s41366-021-00850-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41366-021-00850-1