Abstract
Background/objectives
The ability to adapt the level of daily fuel utilization to substrate availability is given by the respiratory quotient (RQ), which its variance is an indicator of metabolic flexibility. Metabolic inflexibility is associated with many pathologies including obesity, but evidence relies on bed-rest studies and exercise-based interventions. Our goal was to examine the associations for RQ variance in response to daily living activities with obesity, in healthy adults.
Subjects/methods
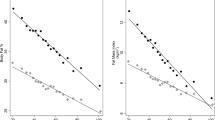
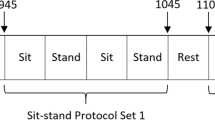
Participants (N = 50; 25 women), 20–64 years were lying for 60 min and randomly performed three conditions for 10 min each (sitting, standing, 1 sit/stand/sit transition min−1). RQ was measured by indirect calorimetry and fat mass (FM), trunk FM (TFM), and fat-free mass (FFM) by DXA.
Results
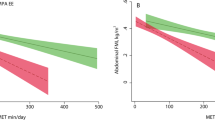
RQ variance among the three conditions was inversely associated with BMI (ß = 0.005; p < 0.001), FM (ß = 0.007; p = 0.024), and TFM (ß = 0.008; p = 0.026). A positive association was found between RQ variance and FFM (ß = −0.007; p = 0.024). No interactions for sex were found (p ≥ 0.05).
Conclusions
These findings suggest that a higher RQ variance in response to daily living metabolic challenges such as transitioning between sitting and standing is associated with lower overall and central obesity, as well as with a higher FFM, in healthy adults. Thus, RQ variance may work as an indication of metabolic flexibility, but these findings were obtained in a young and non-obese adult population without considering their fitness levels. Thus, further research in this field is warranted.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Kelley DE, Mandarino LJ. Fuel selection in human skeletal muscle in insulin resistance: a reexamination. Diabetes. 2000;49:677–83.
Muoio DM. Metabolic inflexibility: when mitochondrial indecision leads to metabolic gridlock. Cell. 2014;159:1253–62.
Bergouignan A, Antoun E, Momken I, Schoeller DA, Gauquelin-Koch G, Simon C, et al. Effect of contrasted levels of habitual physical activity on metabolic flexibility. J. Appl. Physiol. 2013;114:371–9.
Heilbronn LK, Gregersen S, Shirkhedkar D, Hu D, Campbell LV. Impaired fat oxidation after a single high-fat meal in insulin-sensitive nondiabetic individuals with a family history of type 2 diabetes. Diabetes. 2007;56:2046–53.
Rynders CA, Blanc S, DeJong N, Bessesen DH, Bergouignan A. Sedentary behaviour is a key determinant of metabolic inflexibility. J. Physiol. 2018;596:1319–30.
Mujika I, Padilla S. Detraining: loss of training-induced physiological and performance adaptations. Part I: short term insufficient training stimulus. Sports Med. 2000;30:79–87.
Mujika I, Padilla S. Cardiorespiratory and metabolic characteristics of detraining in humans. Med Sci Sports Exerc. 2001;33:413–21.
Blanc S, Normand S, Pachiaudi C, Fortrat JO, Laville M, Gharib C. Fuel homeostasis during physical inactivity induced by bed rest. J Clin Endocrinol Metab. 2000;85:2223–33.
Bergouignan A, Rudwill F, Simon C, Blanc S. Physical inactivity as the culprit of metabolic inflexibility: evidence from bed-rest studies. J Appl Physiol (1985). 2011;111:1201–10.
Craft LL, Zderic TW, Gapstur SM, Vaniterson EH, Thomas DM, Siddique J, et al. Evidence that women meeting physical activity guidelines do not sit less: an observational inclinometry study. Int J Behav Nutr Phys Act. 2012;9:122.
Reiff C, Marlatt K, Dengel DR. Difference in caloric expenditure in sitting versus standing desks. J Phys Act Health. 2012;9:1009–11.
Smith L, Hamer M, Ucci M, Marmot A, Gardner B, Sawyer A. et al. Weekday and weekend patterns of objectively measured sitting, standing, and stepping in a sample of office-based workers: the active buildings study. BMC Public Health. 2015;15:9.https://doi.org/10.1186/s12889-014-1338-1.
Judice PB, Hamilton MT, Sardinha LB, Zderic TW, Silva AM. What is the metabolic and energy cost of sitting, standing and sit/stand transitions? Eur J Appl Physiol. 2016;116:263–73.
Galgani JE, Moro C, Ravussin E. Metabolic flexibility and insulin resistance. Am J Physiol Endocrinol Metab. 2008;295:E1009–17.
Goodpaster BH, Sparks LM. Metabolic flexibility in health and disease. Cell metabolism. 2017;25:1027–36.
Freese J, Klement RJ, Ruiz-Núñez B, Schwarz S, Lötzerich H. The sedentary (r)evolution: have we lost our metabolic flexibility? F1000Research. 2017;6:1787.https://doi.org/10.12688/f1000research.12724.2.
Corpeleijn E, Saris WH, Blaak EE. Metabolic flexibility in the development of insulin resistance and type 2 diabetes: effects of lifestyle. Obes Rev. 2009;10:178–93.
Baig S, Parvaresh Rizi E, Shabeer M, Chhay V, Mok SF, Loh TP, et al. Metabolic gene expression profile in circulating mononuclear cells reflects obesity-associated metabolic inflexibility. Nutr Metab. 2016;13:74.
Tareen SHK, Kutmon M, Adriaens ME, Mariman ECM, de Kok TM, Arts ICW, et al. Exploring the cellular network of metabolic flexibility in the adipose tissue. Genes Nutr. 2018;13:17.
Smith RL, Soeters MR, Wust RCI, Houtkooper RH. Metabolic flexibility as an adaptation to energy resources and requirements in health and disease. Endocr Rev. 2018;39.
van Uffelen JG, Wong J, Chau JY, van der Ploeg HP, Riphagen I, Gilson ND, et al. Occupational sitting and health risks: a systematic review. Am J Prevent Med. 2010;39:379–88.
World Medical Association. Declaration of Helsinki—ethical principles for medical research involving human subjects. WMJ. 2008;54:122–25.
Chobot A, G¢rowska-Kowolik K. Obesity and diabetes-Not only a simple link between two epidemics. Diabetes Metab. Res. Rev. 2018;34:e3042.
World Health Organization. Global status report on noncommunicable diseases 2014. Geneva: World Health Organization; 2014. p. xvii–280.
Church TS, Thomas DM, Tudor-Locke C, Katzmarzyk PT, Earnest CP, Rodarte RQ. et al. Trends over 5 decades in U.S. occupation-related physical activity and their associations with obesity. PLoS ONE. 2011;6:e19657
Buckley JP, Hedge A, Yates T, Copeland RJ, Loosemore M, Hamer M. The sedentary office: an expert statement on the growing case for change towards better health and productivity. 2015.
Dempsey PC, Owen N, Yates TE, Kingwell BA, Dunstan DW. Sitting Less and Moving More: Improved Glycaemic Control for Type 2 Diabetes Prevention and Management. Current diabetes reports. 2016;16:114.
Dunstan DW, Kingwell BA, Larsen R, Healy GN, Cerin E, Hamilton MT, et al. Breaking up prolonged sitting reduces postprandial glucose and insulin responses. Diabetes Care. 2012;35:976–83.
Duvivier BM, Schaper NC, Hesselink MK, van Kan L, Stienen N, Winkens B, et al. Breaking sitting with light activities vs structured exercise: a randomised crossover study demonstrating benefits for glycaemic control and insulin sensitivity in type 2 diabetes. Diabetologia. 2017;60:490–8.
Miles-Chan JL, Sarafian D, Montani JP, Schutz Y, Dulloo A. Heterogeneity in the energy cost of posture maintenance during standing relative to sitting: phenotyping according to magnitude and time-course. PLoS ONE. 2013;8:e65827.
Sparti A, DeLany JP, de la Bretonne JA, Sander GE, Bray GA. Relationship between resting metabolic rate and the composition of the fat-free mass. Metab Clin Exp. 1997;46:1225–30.
Gallagher D, Belmonte D, Deurenberg P, Wang Z, Krasnow N, Pi-Sunyer FX, et al. Organ-tissue mass measurement allows modeling of REE and metabolically active tissue mass. Am J Physiol. 1998;275(2 Pt 1):E249–58.
Illner K, Brinkmann G, Heller M, Bosy-Westphal A, Muller MJ. Metabolically active components of fat free mass and resting energy expenditure in nonobese adults. Am J Physiol Endocrinol Metab. 2000;278:E308–15.
Stephens BR, Granados K, Zderic TW, Hamilton MT, Braun B. Effects of 1 day of inactivity on insulin action in healthy men and women: interaction with energy intake. Metab Clin Exp. 2011;60:941–9.
Thorp AA, Kingwell BA, Sethi P, Hammond L, Owen N, Dunstan DW. Alternating bouts of sitting and standing attenuate postprandial glucose responses. Med Sci Sports Exerc. 2014;46:2053–61.
Duvivier BM, Schaper NC, Bremers MA, van Crombrugge G, Menheere PP, Kars M, et al. Minimal intensity physical activity (standing and walking) of longer duration improves insulin action and plasma lipids more than shorter periods of moderate to vigorous exercise (cycling) in sedentary subjects when energy expenditure is comparable. PLoS ONE. 2013;8:e55542.
McMurray RG, Soares J, Caspersen CJ, McCurdy T. Examining variations of resting metabolic rate of adults: a public health perspective. Med Sci Sports Exerc. 2014;46:1352–8.
Cooper JA, Watras AC, O’Brien MJ, Luke A, Dobratz JR, Earthman CP, et al. Assessing validity and reliability of resting metabolic rate in six gas analysis systems. J Am Diet Assoc. 2009;109:128–32.
Morris C, Grada CO, Ryan M, Roche HM, De Vito G, Gibney MJ, et al. The relationship between aerobic fitness level and metabolic profiles in healthy adults. Mol Nutr Food Res. 2013;57:1246–54.
Kriketos AD, Sharp TA, Seagle HM, Peters JC, Hill JO. Effects of aerobic fitness on fat oxidation and body fatness. Med Sci Sports Exerc. 2000;32:805–11.
Compher C, Frankenfield D, Keim N, Roth-Yousey L. Best practice methods to apply to measurement of resting metabolic rate in adults: a systematic review. J Am Diet Assoc. 2006;106:881–903.
Acknowledgements
We would like to express our gratitude to the participants for their time and effort. This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors. This investigation was conducted at Interdisciplinary Center of the Study of Human Performance (CIPER), I&D 472 (UID/DTP/00447/2020). PBJ is supported by the Portuguese Foundation for Science and Technology (SFRH/BPD/115977/2016).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
The study was approved by the Faculty Ethics Council (approval number: 14/2013) and conducted in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards [22].
Informed consent
Written informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Júdice, P.B., Sardinha, L.B. & Silva, A.M. Variance in respiratory quotient among daily activities and its association with obesity status. Int J Obes 45, 217–224 (2021). https://doi.org/10.1038/s41366-020-0591-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41366-020-0591-x