Abstract
Background
In animal studies early life antibiotic exposure causes metabolic abnormalities including obesity through microbiota disruption, but evidence from human studies is scarce. We examined involvement of gut microbiota in the associations between infant antibiotic exposure and childhood adiposity.
Methods
Infant antibiotic exposure in the first year of life was ascertained using parental reports during interviewer-administered questionnaires. Primary outcomes were childhood obesity [body mass index (BMI) z-score > 95th percentile] and adiposity [abdominal circumference (AC) and skinfold (triceps + subscapular (SST)) measurements] determined from ages 15–60 months. At age 24 months, when the gut microbiota are more stable, stool samples (n = 392) were collected for the gut microbiota profiling using co-abundancy networks. Associations of antibiotic exposure with obesity and adiposity (n = 1016) were assessed using multiple logistic and linear mixed effects regressions. Key bacteria associated with antibiotics exposure were identified by partial redundancy analysis and multivariate association with linear models.
Results
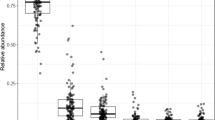
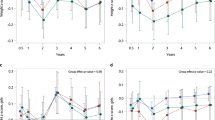
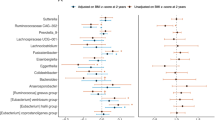
Antibiotic exposure was reported in 38% of study infants. In a fully adjusted model, a higher odds of obesity from 15–60 months of age was observed for any antibiotic exposure [OR(95% CI) = 1.45(1.001, 2.14)] and exposure to ≥3 courses of antibiotics [2.78(1.12, 6.87)]. For continuous adiposity indicators, any antibiotic exposure was associated with higher BMI z-score in boys [β = 0.15(0.01, 0.28)] but not girls [β = −0.04(−0.19, 0.11)] (P interaction = 0.026). Similarly, exposure to ≥3 courses of antibiotics was associated with higher AC in boys [1.15(0.05, 2.26) cm] but not girls [0.57(−1.32, 2.45) cm] (P interaction not significant). Repeated exposure to antibiotics was associated with a significant reduction (FDR-corrected P values < 0.05) in a microbial co-abundant group (CAG) represented by Eubacterium hallii, whose proportion was negatively correlated with childhood adiposity. Meanwhile, a CAG represented by Tyzzerella 4 was positively correlated with the repeated use of antibiotics and childhood adiposity.
Conclusions
Infant antibiotic exposure was associated with disruption of the gut microbiota and the higher risks of childhood obesity and increased adiposity.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
The Lancet. Managing the tide of childhood obesity. Lancet. 2015;385:2434.
Saari A, Virta LJ, Sankilampi U, Dunkel L, Saxen H. Antibiotic exposure in infancy and risk of being overweight in the first 24 months of life. Pediatrics. 2015;135:617–26.
Murphy R, Stewart AW, Braithwaite I, Beasley R, Hancox RJ, Mitchell EA. Antibiotic treatment during infancy and increased body mass index in boys: an international cross-sectional study. Int J Obes. 2014;38:1115–9.
Azad MB, Bridgman SL, Becker AB, Kozyrskyj AL. Infant antibiotic exposure and the development of childhood overweight and central adiposity. Int J Obes. 2014;38:1290–8.
Scott FI, Horton DB, Mamtani R, Haynes K, Goldberg DS, Lee DY, et al. Administration of antibiotics to children before age 2 years increases risk for childhood obesity. Gastroenterology. 2016;151:120–.e5.
Mbakwa CA, Scheres L, Penders J, Mommers M, Thijs C, Arts ICW. Early life antibiotic exposure and weight development in children. J Pediatr. 2016;176:105–.e2.
Ajslev TA, Andersen CS, Gamborg M, Sørensen TIA, Jess T. Childhood overweight after establishment of the gut microbiota: the role of delivery mode, pre-pregnancy weight and early administration of antibiotics. Int J Obes. 2011;35:522–9.
Trasande L, Blustein J, Liu M, Corwin E, Cox LM, Blaser MJ. Infant antibiotic exposures and early-life body mass. Int J Obes. 2013;37:16–23.
Schwartz BS, Pollak J, Bailey-Davis L, Hirsch AG, Cosgrove SE, Nau C, et al. Antibiotic use and childhood body mass index trajectory. Int J Obes. 2016;40:615–21.
Gerber JS, Bryan M, Ross RK, Daymont C, Parks EP, Localio AR. et al. Antibiotic exposure during the first 6 months of life and weight gain during childhood. JAMA. 2016;315:1258–65. https://doi.org/10.1001/jama.2016.2395.
Li D-K, Chen H, Ferber J, Odouli R, Ha C, Lam Y, et al. Infection and antibiotic use in infancy and risk of childhood obesity: a longitudinal birth cohort study. Lancet Diabetes Endocrinol. 2016;0:16498–517.
Isolauri E, Salminen S, Rautava S. Early microbe contact and obesity risk: evidence of causality. J Pediatr Gastroenterol Nutr. 2016;63(Suppl 1):S3–5.
Cox LM, Blaser MJ. Pathways in microbe-induced obesity. Cell Metab. 2013;17:883–94.
Goulet O. Potential role of the intestinal microbiota in programming health and disease. Nutr Rev. 2015;73:32–40.
Cho I, Yamanishi S, Cox L, Methé BA, Zavadil J, Li K, et al. Antibiotics in early life alter the murine colonic microbiome and adiposity. Nature. 2012;488:621–6.
Cox LM, Yamanishi S, Sohn J, Alekseyenko AV, Leung JM, Cho I, et al. Altering the intestinal microbiota during a critical developmental window has lasting metabolic consequences. Cell. 2014;158:705–21.
Soh SE, Tint MT, Gluckman PD, Godfrey KM, Rifkin-Graboi A, Chan YH, et al. Cohort profile: Growing up in Singapore Towards Healthy Outcomes (GUSTO) birth cohort study. Int J Epidemiol. 2013. https://doi.org/10.1093/ije/dyt125.
Chen L-W, Aris I, Bernard J, Tint M-T, Chia A, Colega M, et al. Associations of maternal dietary patterns during pregnancy with offspring adiposity from birth until 54 months of age. Nutrients. 2016;9:2.
National Healthcare Group Polyclinics. Age and gender-specific national BMI cut-offs. Singapore: National Healthcare Group Polyclinics; 2010.
Hamilton CM, Strader LC, Pratt JG, Maiese D, Hendershot T, Kwok RK, et al. The PhenX Toolkit: get the most from your measures. Am J Epidemiol. 2011;174:253–60.
Alberti KG, Zimmet PZ. Definition, diagnosis and classification of diabetes mellitus and its complications. Part 1: diagnosis and classification of diabetes mellitus provisional report of a WHO consultation. Diabet Med. 1998;15:539–53.
Chong Y-S, Cai S, Lin H, Soh SE, Lee Y-S, Leow MK-S, et al. Ethnic differences translate to inadequacy of high-risk screening for gestational diabetes mellitus in an Asian population: a cohort study. BMC Pregnancy Childbirth. 2014;14:345.
Tamburini S, Shen N, Wu HC, Clemente JC. The microbiome in early life: implications for health outcomes. Nat Med. 2016;22:713–22.
Caporaso JG, Lauber CL, Walters WA, Berg-Lyons D, Huntley J, Fierer N, et al. Ultra-high-throughput microbial community analysis on the Illumina HiSeq and MiSeq platforms. ISME J. 2012;6:1621–4.
Tong X, Xu J, Lian F, Yu X, Zhao Y, Xu L, et al. Structural alteration of gut microbiota during the amelioration of human type 2 diabetes with hyperlipidemia by metformin and a traditional chinese herbal formula: a multicenter, randomized, open label clinical trial. MBio. 2018;9. https://doi.org/10.1128/mBio.02392-17.
WHO Multicentre Growth Reference Study Group. WHO Child Growth Standards based on length/height, weight and age. Acta Paediatr. 2006;450:76–85.
Finucane MM, Samet JH, Horton NJ. Translational methods in biostatistics: linear mixed effect regression models of alcohol consumption and HIV disease progression over time. Epidemiol Perspect Innov. 2007;4:8.
Friedman J, Alm EJ. Inferring correlation networks from genomic survey data. PLoS Comput Biol. 2012;8:e1002687.
Morgan XC, Tickle TL, Sokol H, Gevers D, Devaney KL, Ward DV, et al. Dysfunction of the intestinal microbiome in inflammatory bowel disease and treatment. Genome Biol. 2012;13:R79.
Miles RD, Butcher GD, Henry PR, Littell RC. Effect of antibiotic growth promoters on broiler performance, intestinal growth parameters, and quantitative morphology. Poult Sci. 2006;85:476–85.
Ong SF, Chan W-CS, Shorey S, Chong YS, Klainin-Yobas P, He H-G. Postnatal experiences and support needs of first-time mothers in Singapore: A descriptive qualitative study. Midwifery. 2014;30:772–8.
Zhang C, Yin A, Li H, Wang R, Wu G, Shen J, et al. Dietary modulation of gut microbiota contributes to alleviation of both genetic and simple obesity in children. EBioMedicine. 2015;2:968–84.
Ridaura VK, Faith JJ, Rey FE, Cheng J, Duncan AE, Kau AL, et al. Gut microbiota from twins discordant for obesity modulate metabolism in mice. Science. 2013;341:1241214.
Xu J, Lian F, Zhao L, Zhao Y, Chen X, Zhang X, et al. Structural modulation of gut microbiota during alleviation of type 2 diabetes with a Chinese herbal formula. ISME J. 2015;9:552–62.
Duncan SH, Louis P, Flint HJ. Lactate-utilizing bacteria, isolated from human feces, that produce butyrate as a major fermentation product. Appl Environ Microbiol. 2004;70:5810–7.
Shetty SA, Ritari J, Paulin L, Smidt H, De Vos WM. Complete Genome Sequence of Eubacterium hallii Strain L2-7. Genome Announc. 2017;5. https://doi.org/10.1128/genomeA.01167-17.
Vrieze A, Van Nood E, Holleman F, Salojärvi J, Kootte RS, Bartelsman JFWM, et al. Transfer of intestinal microbiota from lean donors increases insulin sensitivity in individuals with metabolic syndrome. Gastroenterology. 2012;143:913–.e7.
Backhed F, Ley RE, Sonnenburg JL, Peterson DA, Gordon JI. Host-bacterial mutualism in the human intestine. Science. 2005;307:1915–20.
Kang Y, Li Y, Du Y, Guo L, Chen M, Huang X, et al. Konjaku flour reduces obesity in mice by modulating the composition of the gut microbiota. Int J Obes. 2018. https://doi.org/10.1038/s41366-018-0187-x.
Zhang M, Differding MK, Benjamin-Neelon SE, Østbye T, Hoyo C, Mueller NT. Association of prenatal antibiotics with measures of infant adiposity and the gut microbiome. Ann Clin Microbiol Antimicrob. 2019;18:18.
VanderWeele TJ, Ding P. Sensitivity analysis in observational research: introducing the E-Value. Ann Intern Med. 2017;167:268–74.
Acknowledgements
The authors thank the GUSTO study group, which includes Allan Sheppard, Amutha Chinnadurai, Anne Eng Neo Goh, Anne Rifkin-Graboi, Anqi Qiu, Arijit Biswas, Bee Wah Lee, Birit F.P. Broekman, Boon Long Quah, Borys Shuter, Carolina Un Lam, Chai Kiat Chng, Cheryl Ngo, Choon Looi Bong, Christiani Jeyakumar Henry, Claudia Chi, Cornelia Yin Ing Chee, Yam Thiam Daniel Goh, Doris Fok, E Shyong Tai, Elaine Tham, Elaine Quah Phaik Ling, Evelyn Xiu Ling Loo, FY, Falk Mueller-Riemenschneider, George Seow Heong Yeo, Helen Chen, Heng Hao Tan, Hugo P. S. van Bever, Iliana Magiati, Inez Bik Yun Wong, Ivy Yee-Man Lau, IBMA, Jeevesh Kapur, Jenny L. Richmond, Jerry Kok Yen Chan, Joanna D. Holbrook, Joanne Yoong, Joao N. Ferreira., Jonathan Tze Liang Choo, Jonathan Y. Bernard, Joshua J. Gooley, KMG, Kenneth Kwek, KHT, Krishnamoorthy Niduvaje, Kuan Jin Lee, Leher Singh, Lieng Hsi Ling, Lin Lin Su, LWC, Lourdes Mary Daniel, LP-CS, Marielle V. Fortier, Mark Hanson, Mary Foong-Fong Chong, Mary Rauff, Mei Chien Chua, Melvin Khee-Shing Leow, Michael Meaney, MTT, NK, Ngee Lek, Oon Hoe Teoh, P. C. Wong, Paulin Tay Straughan, PDG, Pratibha Agarwal, Queenie Ling Jun Li, Rob M. van Dam, Salome A. Rebello, Seang-Mei Saw, See Ling Loy, S. Sendhil Velan, Seng Bin Ang, Shang Chee Chong, Sharon Ng, Shiao-Yng Chan, Shirong Cai, Shu-ES, Sok Bee Lim, Stella Tsotsi, Chin-Ying Stephen Hsu, Sue Anne Toh, Swee Chye Quek, Victor Samuel Rajadurai, Walter Stunkel, Wayne Cutfield, Wee Meng Han, Wei Wei Pang, Y-SC, Yin Bun Cheung, Yiong Huak Chan, YSL, and Zhongwei Huang.
Funding
This research is supported by the Singapore National Research Foundation under its Translational and Clinical Research (TCR) Flagship Programme and administered by the Singapore Ministry of Health’s National Medical Research Council (NMRC), Singapore—NMRC/TCR/004-NUS/2008; NMRC/TCR/012-NUHS/2014. Additional funding is provided by the Singapore Institute for Clinical Sciences, Agency for Science, Technology and Research (A*STAR), Singapore. Study sponsors were not involved in the design of the study, statistical analysis and results interpretation. KMG is supported by the UK Medical Research Council (MC_UU_12011/4), National Institute for Health Research (NIHR Senior Investigator (NF-SI-0515–10042), NIHR Southampton 1000DaysPlus Global Nutrition Research Group and NIHR Southampton Biomedical Research Centre) and by the European Union (Erasmus+ Programme Early Nutrition eAcademy Southeast Asia-573651-EPP-1-2016-1-DE-EPPKA2-CBHE-JP).
Author information
Authors and Affiliations
Contributions
L-WC conducted statistical analysis, interpreted the data, and wrote the first draft of the paper. JX conducted the microbiota analysis, interpreted the data, and co-wrote the first draft of the paper. SES acquired antibiotic exposure data. NK and JAG generated the microbiota data and contributed to the microbiota analysis. L-WC, JX, SES, IMA, and MT-T contributed to data collection, cleaning, and analysis. PDG, KHT, LP-CS, Y-SC, FY, KMG, and YSL designed the GUSTO study. All authors critically revised and approved the final manuscript. YSL had primary responsibility for the final content.
Corresponding author
Ethics declarations
Conflict of interest
KMG, Y-SC, and YSL have received reimbursement for speaking at conferences sponsored by companies selling nutritional products. NK, KMG, and Y-SC are part of an academic consortium that has received research funding from Abbott Nutrition, Nestec and Danone. The other authors have no financial or personal conflict of interest to declare.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Chen, LW., Xu, J., Soh, S.E. et al. Implication of gut microbiota in the association between infant antibiotic exposure and childhood obesity and adiposity accumulation. Int J Obes 44, 1508–1520 (2020). https://doi.org/10.1038/s41366-020-0572-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41366-020-0572-0
This article is cited by
-
Oral and middle ear delivery of otitis media standard of care antibiotics, but not biofilm-targeted antibodies, alter chinchilla nasopharyngeal and fecal microbiomes
npj Biofilms and Microbiomes (2024)
-
Gut Microbiome and Its Impact on Obesity and Obesity-Related Disorders
Current Gastroenterology Reports (2023)