Abstract
Objectives
Screen-viewing in late childhood has been associated with adiposity and blood pressure (BP), but evidence is lacking at younger ages. To investigate the prospective associations of total and device-specific screen-viewing at age 2–3 years with BMI, sum of skinfold thicknesses and BP among Singaporean children at age 3–5 years.
Methods
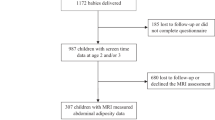
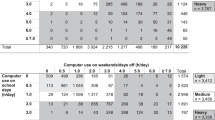
As part of the Growing Up in Singapore Towards healthy Outcomes (GUSTO) cohort, mothers/caregivers reported the time per day their 2 and 3-year-old children watched/used television, handheld devices and computers. Average screen-viewing time (total, television and handheld-devices) at ages 2 and 3 years was used in the analyses. Height; weight; triceps, biceps and subscapular skinfold thicknesses; and systolic and diastolic BP were measured at ages 3, 4 and 5. Associations of screen-viewing with BMI, sum of skinfold thicknesses and BP in 956 children were investigated using repeated-measures linear regression models. Analyses were further stratified by sex as we found significant interaction.
Results
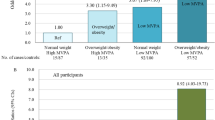
Among boys and girls combined, screen-viewing was positively associated with sum of skinfold thicknesses, but not with BMI or BP. Sex-specific analyses showed significant associations with both BMI and sum of skinfold thicknesses in boys, but not in girls. Screen-viewing was not associated with BP in boys or girls. The increases in mean (95% CI) BMI per hour increase in daily total, television and handheld-devices screen-viewing among boys were 0.12 (0.03, 0.21), 0.18 (0.06, 0.30) and 0.11 (−0.07, 0.29) kg/m2, respectively. The corresponding increases in mean sum of skinfold thicknesses were 0.68 (0.29, 1.07), 0.79 (0.26, 1.32) and 1.18 (0.38, 1.99) mm.
Conclusions
Greater screen-viewing at age 2–3 years was associated with later adiposity at 3–5 years in boys, but not in girls. In light of the increasing use of screen devices and cardiometabolic risk in young children, these findings may have important public health implications.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Ferreira HS, Lucio GM, Assuncao ML, Silva BC, Oliveira JS, Florencio TM, et al. High blood pressure among students in public and private schools in Maceio, Brazil. PLoS ONE 2015;10:e0142982.
World Health Organization. Global strategy on diet, physical activity and health. 2018. Accessed 23 August 2018. http://www.who.int/dietphysicalactivity/childhood_consequences/en/.
World Health Organization. Obesity and overweight. 2016. Accessed 23 August 2018. http://www.who.int/mediacentre/factsheets/fs311/en/.
Essouma M, Noubiap JJN, Bigna JJR, Nansseu JRN, Jingi AM, Aminde LN, et al. Hypertension prevalence, incidence and risk factors among children and adolescents in Africa: a systematic review and meta-analysis protocol. BMJ Open. 2015;5:1–5.
Rao G. Diagnosis, epidemiology, and management of hypertension in children. Pediatrics. 2016;138:1–13.
Fletcher E, Leech R, McNaughton SA, Dunstan DW, Lacy KE, Salmon J. Is the relationship between sedentary behaviour and cardiometabolic health in adolescents independent of dietary intake? A systematic review. Obes Rev. 2015;16:795–805.
Lee PH, Wong FKY. The association between time spent in sedentary behaviors and blood pressure: a systematic review and meta-analysis. Sports Med. 2015;45:867–80.
Ofcom’s media literacy research programme. Children’s and parents’ media use and attitudes (Research report). 2017. Accessed 23 August 2018. https://www.ofcom.org.uk/__data/assets/pdf_file/0020/108182/children-parents-media-use-attitudes-2017.pdf.
Goh SN, Teh LH, Tay WR, Anantharaman S, van Dam RM, Tan CS, et al. Sociodemographic, home environment and parental influences on total and device-specific screen viewing in children aged 2 years and below: an observational study. BMJ Open. 2016;6:e009113.
Carson V, Janssen I. Associations between factors within the home setting and screen time among children aged 0-5 years: a cross-sectional study. BMC Public Health. 2012;12:539.
Roberts DF, Foehr UG, Rideout VJ, Brodie M. Kids and media at the new millennium: a Kaiser family foundation report. A comprehensive national analysis of children's media use. Accessed 23 August 2018. https://kaiserfamilyfoundation.files.wordpress.com/2013/01/kids-media-the-new-millennium-report.pdf; 1999.
Council on communication and media. Media and Young Minds. Pediatrics. 2016;138:e20162591.
Smith L, Gardner B, Hamer M. Childhood correlates of adult TV viewing time: a 32-year follow-up of the 1970 British cohort study. Journal of Epidemiology and Community Health. 2015;69:309–313.
Stamatakis E, Coombs N, Jago R, Gama A, Mourao I, Nogueira H, et al. Associations between indicators of screen time and adiposity indices in Portuguese children. Prev Med. 2013;56:299–303.
Ekelund U, Brage S, Froberg K, Harro M, Anderssen SA, Sardinha LB, et al. TV viewing and physical activity are independently associated with metabolic risk in children: the European Youth Heart Study. PLoS Med. 2006;3:2449–56.
Martinez-Gomez D, Tucker J, Heelan KA, Welk GJ, Eisenmann JC. Associations between sedentary behavior and blood pressure in young children. Arch Pediatr Adolesc Med. 2009;163:724–30.
Gopinath B, Baur LA, Hardy LL, Kifley A, Rose KA, Wong TY, et al. Relationship between a range of sedentary behaviours and blood pressure during early adolescence. J Hum Hypertens. 2012;26:350–6.
Stamatakis E, Coombs N, Jago R, Gama A, Mourao I, Nogueira H, et al. Type-specific screen time associations with cardiovascular risk markers in children. Am J Prev Med. 2013;44:481–8.
de Moraes AC, Carvalho HB, Siani A, Barba G, Veidebaum T, Tornaritis M, et al. Incidence of high blood pressure in children—effects of physical activity and sedentary behaviors: the IDEFICS study: High blood pressure, lifestyle and children. Int J Cardiol. 2015;180:165–70.
Nightingale CM, Rudnicka AR, Donin AS, Sattar N, Cook DG, Whincup PH, et al. Screen time is associated with adiposity and insulin resistance in children. Arch Dis Child. 2017;102:612–6.
Mendoza JA, Zimmerman FJ, Christakis DA. Television viewing, computer use, obesity, and adiposity in US preschool children. Int J Behav Nutr Phys Act. 2007;4:44.
Proctor MH, Moore LL, Gao D, Cupples LA, Bradlee ML, Hood MY, et al. Television viewing and change in body fat from preschool to early adolescence: the Framingham Children’s Study. Int J Obes. 2003;27:827–33.
Laurson KR, Eisenmann JC, Welk GJ, Wickel EE, Gentile DA, Walsh DA. Combined influence of physical activity and screen time recommendations on childhood overweight. J Pediatr. 2008;153:209–14.
Robinson TN. Television viewing and childhood obesity. Pediatr Clin North Am. 2001;48:1017–25.
Pardee PE, Norman GJ, Lustig RH, Preud’homme D, Schwimmer JB. Television viewing and hypertension in obese children. Am J Prev Med. 2007;33:439–43.
Canadian Paediatric Society DHTFOO. Screen time and young children: promoting health and development in a digital world. Paediatr Child Health. 2017;22:461–8.
Gopinath B, Hardy LL, Kifley A, Baur LA, Mitchell P. Activity behaviors in schoolchildren and subsequent 5-yr change in blood pressure. Med Sci Sports Exerc. 2014;46:724–9.
Robinson S, Daly RM, Ridgers ND, Salmon J. Screen-based behaviors of children and cardiovascular risk factors. J Pediatr. 2015;167:1239–45.
Bernard JY, Padmapriya N, Chen B, Cai S, Tan KH, Yap F, et al. Predictors of screen viewing time in young Singaporean children: the GUSTO cohort. Int J Behav Nutr Phys Act. 2017;14:017–0562.
Saldanha-Gomes C, Heude B, Charles MA, de Lauzon-Guillain B, Botton J, Carles S, et al. Prospective associations between energy balance-related behaviors at 2 years of age and subsequent adiposity: the EDEN mother-child cohort. Int J Obes. 2017;41:38–45.
Falbe J, Rosner B, Willett WC, Sonneville KR, Hu FB, Field AE. Adiposity and different types of screen time. Pediatrics. 2013;132:e1497–e505.
Soh S-E, Tint MT, Gluckman PD, Godfrey KM, Rifkin-Graboi A, Chan YH, et al. Cohort profile: growing Up in Singapore towards healthy Outcomes (GUSTO) birth cohort study. Int J Epidemiol. 2014;43:1401–9.
Aris IM, Bernard JY, Chen LW, Tint MT, Pang WW, Soh SE, et al. Modifiable risk factors in the first 1000 days for subsequent risk of childhood overweight in an Asian cohort: significance of parental overweight status. Int J Obes. 2017;28:178.
Aris IM, Bernard JY, Chen L-W, Tint MT, Pang WW, Lim WY, et al. Infant body mass index peak and early childhood cardio-metabolic risk markers in a multi-ethnic Asian birth cohort. Int J Epidemiol. 2017;46:513–25.
Azur MJ, Stuart EA, Frangakis C, Leaf PJ. Multiple imputation by chained equations: what is it and how does it work? Int J Methods Psychiatr Res. 2011;20:40–9.
Moons KG, Donders RA, Stijnen T, Harrell FE Jr. Using the outcome for imputation of missing predictor values was preferred. J Clin Epidemiol. 2006;59:1092–101.
Koulouridis E, Georgalidis K, Kostimpa I, Kalantzi M, Ntouto P, Koulouridis I, et al. Factors influencing blood pressure control in children and adolescents. Int Urol Nephrol. 2008;40:741–8.
Agirbasli M, Agaoglu NB, Orak N, Caglioz H, Ocek T, Poci N, et al. Sex hormones and metabolic syndrome in children and adolescents. Metabolism. 2009;58:1256–62.
Rice M, Turner-Henson A, Hage FG, Azuero A, Joiner C, Affuso O, et al. Factors that influence blood pressure in 3- to 5-year-old children: a pilot study. Biol Res Nurs. 2017;20:25–31.
van Ekris E, Altenburg TM, Singh AS, Proper KI, Heymans MW, Chinapaw MJ. An evidence-update on the prospective relationship between childhood sedentary behaviour and biomedical health indicators: a systematic review and meta-analysis. Obes Rev. 2016;17:833–49.
Serrano-Sanchez JA, Martí-Trujillo S, Lera-Navarro A, Dorado-García C, González-Henríquez JJ, Sanchís-Moysi J. Associations between screen time and physical activity among Spanish adolescents. PLoS ONE 2011;6:e24453.
Yland J, Guan S, Emanuele E, Hale L. Interactive vs passive screen time and nighttime sleep duration among school-aged children. Sleep Health. 2015;1:191–6.
Miller AL, Lumeng JC, LeBourgeois MK. Sleep patterns and obesity in childhood. Curr Opin Endocrinol Diabetes Obes. 2015;22:41–7.
Heilmann A, Rouxel P, Fitzsimons E, Kelly Y, Watt RG. Longitudinal associations between television in the bedroom and body fatness in a UK cohort study. Int J Obes. 2017;41:1503.
Taverno Ross SE, Byun W, Dowda M, McIver KL, Saunders RP, Pate RR. Sedentary behaviors in fifth-grade boys and girls: where, with whom, and why? Child Obes. 2013;9:532–9.
Acknowledgements
This research is supported by the Singapore National Research Foundation under its Translational and Clinical Research (TCR) Flagship Programme and administered by the Singapore Ministry of Health’s National Medical Research Council (NMRC), Singapore- NMRC/TCR/004-NUS/2008; NMRC/TCR/012-NUHS/2014. Additional funding is provided by the Singapore Institute for Clinical Sciences, Agency for Science Technology and Research (A*STAR), Singapore. KMG is supported by the National Institute for Health Research through the NIHR Southampton Biomedical Research Centre and by the European Union’s Erasmus + Capacity-Building ENeASEA Project and Seventh Framework Programme (FP7/2007-2013), projects EarlyNutrition and ODIN under grant agreement numbers 289346 and 613977. We would like to thank GUSTO study group, operational managers, research fellows, study coordinators and data management team. We greatly appreciate voluntary participation of all participants, and cooperation of KK Women’s and Children’s Hospital and National University Hospital. The GUSTO study group includes Allan Sheppard, Amutha Chinnadurai, Anne Eng Neo Goh, Anne Rifkin-Graboi, Anqi Qiu, Arijit Biswas, Bee Wah Lee, Birit F.P. Broekman, Boon Long Quah, Borys Shuter, Chai Kiat Chng, Cheryl Ngo, Choon Looi Bong, Christiani Jeyakumar Henry, Claudia Chi, Cornelia Yin Ing Chee, Yam Thiam Daniel Goh, Doris Fok, E Shyong Tai, Elaine Tham, Elaine Quah Phaik Ling, Evelyn Xiu Ling Loo, George Seow Heong Yeo, Helen Chen, Heng Hao Tan, Hugo P S van Bever, Iliana Magiati, Inez Bik Yun Wong, Ivy Yee-Man Lau, Izzuddin Bin Mohd Aris, Jeevesh Kapur, Jenny L. Richmond, Jerry Kok Yen Chan, Joanna D. Holbrook, Joanne Yoong, Joao N. Ferreira, Jonathan Tze Liang Choo, Joshua J. Gooley, Krishnamoorthy Niduvaje, Kuan Jin Lee, Leher Singh, Lieng Hsi Ling, Lin Lin Su, Ling-Wei Chen, Lourdes Mary Daniel, Marielle V. Fortier, Mark Hanson, Mary Foong-Fong Chong, Mary Rauff, Mei Chien Chua, Melvin Khee-Shing Leow, Michael Meaney, Mya Thway Tint, Neerja Karnani, Ngee Lek, Oon Hoe Teoh, P. C. Wong, Paulin Tay Straughan, Pratibha Agarwal, Queenie Ling Jun Li, Rob M. van Dam, Salome A. Rebello, S. Sendhil Velan, Seng Bin Ang, Shang Chee Chong, Sharon Ng, Shiao-Yng Chan, Shu-E Soh, Sok Bee Lim, Stella Tsotsi, Chin-Ying Stephen Hsu, Sue Anne Toh, Swee Chye Quek, Victor Samuel Rajadurai, Walter Stunkel, Wayne Cutfield, Wee Meng Han, Wei Wei Pang, Yin Bun Cheung, Yiong Huak Chan.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
KMG and YSC report receiving reimbursement for speaking at conferences sponsored by companies selling nutritional products. KMG and YSC report being part of an academic consortium that has received research funding from Abbott Nutrition, Nestle and Danone. The remaining authors declare that they have no conflict of interest.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Padmapriya, N., Aris, I.M., Tint, M.T. et al. Sex-specific longitudinal associations of screen viewing time in children at 2–3 years with adiposity at 3–5 years. Int J Obes 43, 1334–1343 (2019). https://doi.org/10.1038/s41366-019-0344-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41366-019-0344-x
This article is cited by
-
Sociodemographic and behavioural factors of adherence to the no-screen guideline for toddlers among parents from the French nationwide Elfe birth cohort
International Journal of Behavioral Nutrition and Physical Activity (2022)
-
The longitudinal association between early-life screen viewing and abdominal adiposity—findings from a multiethnic birth cohort study
International Journal of Obesity (2021)
-
The association between screen time and cardiometabolic risk in young children
International Journal of Behavioral Nutrition and Physical Activity (2020)
-
Socio-demographic and maternal predictors of adherence to 24-hour movement guidelines in Singaporean children
International Journal of Behavioral Nutrition and Physical Activity (2019)