Abstract
Importance
Screen viewing in adults has been associated with greater abdominal adiposity, with the magnitude of associations varying by sex and ethnicity, but the evidence is lacking at younger ages. We aimed to investigate sex- and ethnic-specific associations of screen-viewing time at ages 2 and 3 years with abdominal adiposity measured by magnetic resonance imaging at age 4.5 years.
Methods
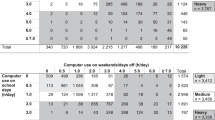
The Growing Up in Singapore Towards healthy Outcomes is an ongoing prospective mother–offspring cohort study. Parents/caregivers reported the time their child spent viewing television, handheld devices, and computer screens at ages 2 and 3 years. Superficial and deep subcutaneous and visceral abdominal adipose tissue volumes were quantified from magnetic resonance images acquired at age 4.5 years. Associations between screen-viewing time and abdominal adipose tissue volumes were examined by multivariable linear regression adjusting for confounding factors.
Results
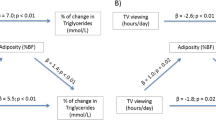
In the overall sample (n = 307), greater total screen-viewing time and handheld device times were associated with higher superficial and deep subcutaneous adipose tissue volumes, but not with visceral adipose tissue volumes. Interactions with child sex were found, with significant associations with superficial and deep subcutaneous and visceral adipose tissue volumes in boys, but not in girls. Among boys, the increases in mean (95% CI) superficial and deep subcutaneous and visceral adipose tissue volumes were 24.3 (9.9, 38.7), 17.6 (7.4, 27.8), and 7.8 (2.1, 13.6) mL per hour increase in daily total screen-viewing time, respectively. Ethnicity-specific analyses showed associations of total screen-viewing time with abdominal adiposity only in Malay children. Television viewing time was not associated with abdominal adiposity.
Conclusion
Greater total screen-viewing time (and in particular, handheld device viewing time) was associated with higher abdominal adiposity in boys and Malay children. Additional studies are necessary to confirm these associations and to examine screen-viewing interventions for preventing excessive abdominal adiposity and its adverse cardiometabolic consequences.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
Data availability
The dataset supporting the conclusions of this article can be made available upon request and after approval by the GUSTO Executive Committee.
References
World Health Organization. Childhood overweight and obesity. Global strategy on diet, physical activity and health. World Health Organization, 2016. https://www.who.int/dietphysicalactivity/childhood/en/.
von Schnurbein J, Klenk J, Galm C, Berg S, Gottmann P, Steinacker JM, et al. Reference values and early determinants of intra-abdominal fat mass in primary school children. Horm Res Paediatr. 2011;75:412–22.
Haffner SM. Abdominal adiposity and cardiometabolic risk: do we have all the answers? Am J Med. 2007;120:S10–S6.
Pischon T, Boeing H, Hoffmann K, Bergmann M, Schulze MB, Overvad K, et al. General and abdominal adiposity and risk of death in Europe. N Engl J Med. 2008;359:2105–20.
Shah RV, Murthy VL, Abbasi SA, Blankstein R, Kwong RY, Goldfine AB, et al. Visceral adiposity and the risk of metabolic syndrome across body mass index: the MESA Study. JACC Cardiovasc Imaging. 2014;7:1221–35.
Sadananthan SA, Tint MT, Michael N, Aris IM, Loy SL, Lee KJ, et al. Association between early life weight gain and abdominal fat partitioning at 4.5 years is sex, ethnicity, and age dependent. Obesity. 2019;27:470–8.
Tint MT, Fortier MV, Godfrey KM, Shuter B, Kapur J, Rajadurai VS, et al. Abdominal adipose tissue compartments vary with ethnicity in Asian neonates: Growing Up in Singapore Toward Healthy Outcomes birth cohort study. Am J Clin Nutr. 2016;103:1311–7.
Lee MJ, Wu Y, Fried SK. Adipose tissue heterogeneity: implication of depot differences in adipose tissue for obesity complications. Mol Aspects Med. 2013;34:1–11.
Golan R, Shelef I, Rudich A, Gepner Y, Shemesh E, Chassidim Y, et al. Abdominal superficial subcutaneous fat: a putative distinct protective fat subdepot in type 2 diabetes. Diabetes Care. 2012;35:640–7.
Vogelezang S, Gishti O, Felix JF, van der Beek EM, Abrahamse-Berkeveld M, Hofman A, et al. Tracking of abdominal subcutaneous and preperitoneal fat mass during childhood. The Generation R Study. Int J Obes. 2016;40:595–600.
Kindblom JM, Lorentzon M, Hellqvist A, Lönn L, Brandberg J, Nilsson S, et al. BMI changes during childhood and adolescence as predictors of amount of adult subcutaneous and visceral adipose tissue in men: the GOOD Study. Diabetes. 2009;58:867–74.
Pandita A, Sharma D, Pandita D, Pawar S, Tariq M, Kaul A. Childhood obesity: prevention is better than cure. Diabetes Metab Syndr Obes. 2016;9:83–9.
Modi N, Thomas EL, Uthaya SN, Umranikar S, Bell JD, Yajnik C. Whole body magnetic resonance imaging of healthy newborn infants demonstrates increased central adiposity in Asian Indians. Pediatr Res. 2009;65:584–7.
Fletcher E, Leech R, McNaughton SA, Dunstan DW, Lacy KE, Salmon J. Is the relationship between sedentary behaviour and cardiometabolic health in adolescents independent of dietary intake? A systematic review. Obes Rev. 2015;16:795–805.
Whitaker KM, Pereira MA, Jacobs DR Jr., Sidney S, Odegaard AO. Sedentary behavior, physical activity, and abdominal adipose tissue deposition. Med Sci Sports Exerc. 2017;49:450–8.
Byun W, Dowda M, Pate RR. Associations between screen-based sedentary behavior and cardiovascular disease risk factors in Korean youth. J Korean Med Sci. 2012;27:388–94.
Bernard JY, Padmapriya N, Chen B, Cai S, Tan KH, Yap F, et al. Predictors of screen viewing time in young Singaporean children: the GUSTO cohort. Int J Behav Nutr Phys Act. 2017;14:112–21.
Robinson TN, Banda JA, Hale L, Lu AS, Fleming-Milici F, Calvert SL, et al. Screen media exposure and obesity in children and adolescents. Pediatrics. 2017;140:S97–101.
Cliff DP, McNeill J, Vella SA, Howard SJ, Santos R, Batterham M, et al. Adherence to 24-Hour Movement Guidelines for the Early Years and associations with social-cognitive development among Australian preschool children. BMC Public Health. 2017;17:857.
Tremblay MS, Chaput JP, Adamo KB, Aubert S, Barnes JD, Choquette L, et al. Canadian 24-Hour Movement Guidelines for the Early Years (0-4 years): an integration of physical activity, sedentary behaviour, and sleep. BMC Public Health. 2017;17:874.
Goh SN, Teh LH, Tay WR, Anantharaman S, van Dam RM, Tan CS, et al. Sociodemographic, home environment and parental influences on total and device-specific screen viewing in children aged 2 years and below: an observational study. BMJ Open. 2016;6:e009113.
Carson V, Janssen I. Associations between factors within the home setting and screen time among children aged 0-5 years: a cross-sectional study. BMC Public Health. 2012;12:539.
Collings PJ, Kelly B, West J, Wright J. Associations of TV viewing duration, meals and snacks eaten when watching TV, and a TV in the bedroom with child adiposity. Obesity. 2018;26:1619–28.
Cox R, Skouteris H, Rutherford L, Fuller-Tyszkiewicz M, Dell’ Aquila D, Hardy LL. Television viewing, television content, food intake, physical activity and body mass index: a cross-sectional study of preschool children aged 2-6 years. Health Promot J Austr. 2012;23:58–62.
van Ekris E, Altenburg TM, Singh AS, Proper KI, Heymans MW, Chinapaw MJ. An evidence-update on the prospective relationship between childhood sedentary behaviour and biomedical health indicators: a systematic review and meta-analysis. Obes Rev. 2016;17:833–49.
Bosy-Westphal A, Booke C-A, Blöcker T, Kossel E, Goele K, Later W, et al. Measurement site for waist circumference affects its accuracy as an index of visceral and abdominal subcutaneous fat in a caucasian population. J Nutr. 2010;140:954–61.
Horan M, Gibney E, Molloy E, McAuliffe F. Methodologies to assess paediatric adiposity. Irish J Med Sci. 2015;184:53–68.
Sadananthan SA, Prakash B, Leow MKS, Khoo CM, Chou H, Venkataraman K, et al. Automated segmentation of visceral and subcutaneous (deep and superficial) adipose tissues in normal and overweight men. J Magn Reson Imaging. 2015;41:924–34.
Staiano AE, Harrington DM, Broyles ST, Gupta AK, Katzmarzyk PT. Television, adiposity, and cardiometabolic risk in children and adolescents. Am J Prev Med. 2013;44:40–7.
Stallmann-Jorgensen IS, Gutin B, Hatfield-Laube JL, Humphries MC, Johnson MH, Barbeau P. General and visceral adiposity in black and white adolescents and their relation with reported physical activity and diet. Int J Obes. 2007;31:622–9.
Padmapriya N, Aris IM, Tint MT, Loy SL, Cai S, Tan KH, et al. Sex-specific longitudinal associations of screen viewing time in children at 2-3 years with adiposity at 3-5 years. Int J Obes. 2019;43:1334–43.
Zilanawala A, Davis-Kean P, Nazroo J, Sacker A, Simonton S, Kelly Y. Race/ethnic disparities in early childhood BMI, obesity and overweight in the United Kingdom and United States. Int J Obes. 2015;39:520–9.
Kanter R, Caballero B. Global gender disparities in obesity: a review. Adv Nutr. 2012;3:491–8.
Soh SE, Chong YS, Kwek K, Saw SM, Meaney MJ, Gluckman PD, et al. Insights from the Growing Up in Singapore Towards Healthy Outcomes (GUSTO) cohort study. Ann Nutr Metab. 2014;64:218–25.
Soh SE, Tint MT, Gluckman PD, Godfrey KM, Rifkin-Graboi A, Chan YH, et al. Cohort profile: Growing Up in Singapore Towards healthy Outcomes (GUSTO) birth cohort study. Int J Epidemiol. 2014;43:1401–9.
Fogel A, Goh AT, Fries LR, Sadananthan SA, Velan SS, Michael N, et al. Faster eating rates are associated with higher energy intakes during an ad libitum meal, higher BMI and greater adiposity among 4·5-year-old children: results from the Growing Up in Singapore Towards Healthy Outcomes (GUSTO) cohort. Br J Nutr. 2017;117:1042–51.
Sadananthan SA, Prakash B, Leow MK, Khoo CM, Chou H, Venkataraman K, et al. Automated segmentation of visceral and subcutaneous (deep and superficial) adipose tissues in normal and overweight men. J Magn Reson Imaging. 2015;41:924–34.
Conway JM, Ingwersen LA, Vinyard BT, Moshfegh AJ. Effectiveness of the US Department of Agriculture 5-step multiple-pass method in assessing food intake in obese and nonobese women. Am J Clin Nutr. 2003;77:1171–8.
Health Promotion Board. Energy and nutrient composition of food. Singapore: Health Promotion Board, 2011. https://focos.hpb.gov.sg/eservices/ENCF/.
Lim HX, Toh JY, Tan KH, Chong Y-S, Yap F, Godfrey KM, et al. Validation of a semi-quantitative FFQ for 18-month-old toddlers: the Growing Up in Singapore Towards Healthy Outcomes (GUSTO) study. Public Health Nutr. 2019;22:1990–2000.
U.S. Department of Agriculture, Agricultural Research Service. FoodData Central. U.S. Department of Agriculture, Agricultural Research Service, 2019. https://fdc.nal.usda.gov/.
Aris IM, Bernard JY, Chen LW, Tint MT, Pang WW, Soh SE, et al. Modifiable risk factors in the first 1000 days for subsequent risk of childhood overweight in an Asian cohort: significance of parental overweight status. Int J Obes. 2017;28:178.
Aris IM, Bernard JY, Chen L-W, Tint MT, Pang WW, Lim WY, et al. Infant body mass index peak and early childhood cardio-metabolic risk markers in a multi-ethnic Asian birth cohort. Int J Epidemiol. 2017;46:513–25.
Azur MJ, Stuart EA, Frangakis C, Leaf PJ. Multiple imputation by chained equations: what is it and how does it work? Int J Methods Psychiatr Res. 2011;20:40–9.
Moons KG, Donders RA, Stijnen T, Harrell FE Jr. Using the outcome for imputation of missing predictor values was preferred. J Clin Epidemiol. 2006;59:1092–101.
Saldanha-Gomes C, Heude B, Charles MA, de Lauzon-Guillain B, Botton J, Carles S, et al. Prospective associations between energy balance-related behaviors at 2 years of age and subsequent adiposity: the EDEN mother-child cohort. Int J Obes. 2017;41:38–45.
Falbe J, Rosner B, Willett WC, Sonneville KR, Hu FB, Field AE. Adiposity and different types of screen time. Pediatrics. 2013;132:e1497–505.
Chaput J, Visby T, Nyby S, Klingenberg L, Gregersen NT, Tremblay A, et al. Video game playing increases food intake in adolescents: a randomized crossover study. Am J Clin Nutr. 2011;93:1196–203.
Michaud I, Chaput JP, O’Loughlin J, Tremblay A, Mathieu ME. Long duration of stressful homework as a potential obesogenic factor in children: a QUALITY study. Obesity. 2015;23:815–22.
Chaput JP, Drapeau V, Poirier P, Teasdale N, Tremblay A. Glycemic instability and spontaneous energy intake: association with knowledge-based work. Psychosom Med. 2008;70:797–804.
Chaput J-P, Tremblay A. Acute effects of knowledge-based work on feeding behavior and energy intake. Physiol Behav. 2007;90:66–72.
Henson J, Edwardson CL, Morgan B, Horsfield MA, Bodicoat DH, Biddle SJ, et al. Associations of sedentary time with fat distribution in a high-risk population. Med Sci Sports Exerc. 2015;47:1727–34.
Tchernof A, Despres JP. Pathophysiology of human visceral obesity: an update. Physiol Reviews. 2013;93:359–404.
Karastergiou K, Smith SR, Greenberg AS, Fried SK. Sex differences in human adipose tissues—the biology of pear shape. Biol Sex Differ. 2012;3:13.
Fitzgerald SJ, Janorkar AV, Barnes A, Maranon RO. A new approach to study the sex differences in adipose tissue. J Biomed Sci. 2018;25:89.
Taverno Ross SE, Byun W, Dowda M, McIver KL, Saunders RP, Pate RR. Sedentary behaviors in fifth-grade boys and girls: where, with whom, and why? Child Obes. 2013;9:532–9.
Liu A, Byrne NM, Kagawa M, Ma G, Kijboonchoo K, Nasreddine L, et al. Ethnic differences in body fat distribution among Asian pre-pubertal children: a cross-sectional multicenter study. BMC Public Health. 2011;11:500.
Tanaka S, Horimai C, Katsukawa F. Ethnic differences in abdominal visceral fat accumulation between Japanese, African-Americans, and Caucasians: a meta-analysis. Acta Diabetol. 2003;40:s302–4.
Acknowledgements
This research was supported by the Singapore National Research Foundation under its Translational and Clinical Research (TCR) Flagship Programme and administered by the Singapore Ministry of Health’s National Medical Research Council (NMRC), Singapore—NMRC/TCR/004-NUS/2008; NMRC/TCR/012-NUHS/2014. Additional funding was provided by the Singapore Institute for Clinical Sciences, Agency for Science Technology and Research (A*STAR), Singapore. KMG was supported by the National Institute for Health Research through the NIHR Southampton Biomedical Research Centre and by the European Union’s Erasmus+ Capacity-Building ENeASEA Project and Seventh Framework Programme (FP7/2007-2013), projects EarlyNutrition and ODIN under grant agreement numbers 289346 and 613977. The authors would like to thank GUSTO study group, operational managers, research fellows, study coordinators, and data management team. The authors greatly appreciate the voluntary participation of all participants and the cooperation of KK Women’s and Children’s Hospital and National University Hospital. The GUSTO study group includes Allan Sheppard, Amutha Chinnadurai, Anne Eng Neo Goh, Anne Rifkin-Graboi, Anqi Qiu, Arijit Biswas, Bee Wah Lee, Birit F.P. Broekman, Boon Long Quah, Borys Shuter, Chai Kiat Chng, Cheryl Ngo, Choon Looi Bong, Christiani Jeyakumar Henry, Claudia Chi, Cornelia Yin Ing Chee, Yam Thiam Daniel Goh, Doris Fok, E Shyong Tai, Elaine Tham, Elaine Quah Phaik Ling, Evelyn Xiu Ling Loo, George Seow Heong Yeo, Helen Chen, Heng Hao Tan, Hugo P S van Bever, Iliana Magiati, Inez Bik Yun Wong, Ivy Yee-Man Lau, Izzuddin Bin Mohd Aris, Jeevesh Kapur, Jenny L. Richmond, Jerry Kok Yen Chan, Joanna D. Holbrook, Joanne Yoong, Joao N. Ferreira, Jonathan Tze Liang Choo, Joshua J. Gooley, Krishnamoorthy Niduvaje, Kuan Jin Lee, Leher Singh, Lieng Hsi Ling, Lin Lin Su, Ling-Wei Chen, Lourdes Mary Daniel, Marielle V. Fortier, Mark Hanson, Mary Foong-Fong Chong, Mary Rauff, Mei Chien Chua, Melvin Khee-Shing Leow, Michael Meaney, Mya Thway Tint, Neerja Karnani, Ngee Lek, Oon Hoe Teoh, P. C. Wong, Paulin Tay Straughan, Pratibha Agarwal, Queenie Ling Jun Li, Rob M. van Dam, Salome A. Rebello, S. Sendhil Velan, Seng Bin Ang, Shang Chee Chong, Sharon Ng, Shiao-Yng Chan, Shu-E Soh, Sok Bee Lim, Stella Tsotsi, Chin-Ying Stephen Hsu, Sue Anne Toh, Swee Chye Quek, Victor Samuel Rajadurai, Walter Stunkel, Wayne Cutfield, Wee Meng Han, Wei Wei Pang, Yin Bun Cheung, and Yiong Huak Chan.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
KMG and YSC report receiving reimbursement for speaking at conferences sponsored by companies selling nutritional products and report being part of an academic consortium that has received research funding from Abbott Nutrition, Nestle, and Danone. No other disclosures were reported. The authors wish to confirm that there has been no significant financial support for this work that could have influenced its outcome.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Padmapriya, N., Tint, MT., Sadananthan, S.A. et al. The longitudinal association between early-life screen viewing and abdominal adiposity—findings from a multiethnic birth cohort study. Int J Obes 45, 1995–2005 (2021). https://doi.org/10.1038/s41366-021-00864-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41366-021-00864-9