Abstract
Cancer immunotherapy has revolutionized the approach to cancer treatment of malignant tumors by harnessing the body’s immune system to selectively target cancer cells. Despite remarkable advances, there are still challenges in achieving successful clinical responses. Recent evidence suggests that immune cell-derived exosomes modulate the immune system to generate effective antitumor immune responses, making them a cutting-edge therapeutic strategy. However, natural exosomes are limited in clinical application due to their low drug delivery efficiency and insufficient antitumor capacity. Technological advancements have allowed exosome modifications to magnify their intrinsic functions, load different therapeutic cargoes, and preferentially target tumor sites. These engineered exosomes exert potent antitumor effects and have great potential for cancer immunotherapy. In this review, we describe ingenious modification strategies to attain the desired performance. Moreover, we systematically summarize the tumor-controlling properties of engineered immune cell-derived exosomes in innate and adaptive immunity. Collectively, this review provides a comprehensive and intuitive guide for harnessing the potential of modified immune cell-derived exosome-based approaches, offering valuable strategies to enhance and optimize cancer immunotherapy.
Similar content being viewed by others
Introduction
Cancer immunotherapy has gained widespread attention for its ability to activate the immune system to target tumors, unlike conventional treatments that affect both cancerous and healthy cells1. The success of immunotherapy highlights the crucial role of the immune system in the elimination of malignant cells2. Tumor growth is precisely controlled by two major immune cell groups: innate and adaptive immune cells3. Innate immune cells destroy tumor cells to induce the release of tumor-specific antigens. They are captured by antigen-presenting cells (APCs), including dendritic cells (DCs), and presented to T cells to prime the adaptive immune response. Subsequently, antigen-specific T cells evoke a specific immune response against cancer cells4,5. Cancer immunotherapies that harness the power of this immune system can specifically kill cancer cells with minimal influence on normal cells and trigger long-term memory that prevents tumor recurrence5. Thus, the development of methods to direct or harness the immune response can enhance the success of cancer immunotherapy.
In recent decades, the proposal of various new immunotherapies has emerged, with treatment strategies being continuously refined to improve antitumor efficacy6,7. Monoclonal antibody-based immune checkpoint blockades (ICBs) have shown substantial antitumor activity in several cancers, such as melanoma, lung cancer, and kidney cancer7,8. However, the clinical effect of this approach is only beneficial in approximately 20–30% of patients, with the majority showing resistance7. Chimeric antigen receptor (CAR)-T cell therapy, a treatment that genetically engineers a patient’s T cells to express CARs targeting specific cancer cells, exhibits significant efficacy in the treatment of hematologic malignancies, including acute lymphocytic leukemia and non-Hodgkin lymphoma6,7,9. However, the use of this therapy in solid tumors has been impeded by tumor microenvironmental barriers and immunosuppressive environments, and CAR-T cells have elicited severe toxicities, such as cytokine release syndrome (CRS)9. Therefore, the field of immunotherapy is currently aspiring to discover novel, low-toxicity, and biostable immunomodulators.
Emerging evidence indicates that exosomes, ranging in size from 30 to 150 nm, can modulate the antitumor immune response, presenting them as a promising avenue for cancer immunotherapy10. As endogenous transporters, exosomes deliver lipids, proteins, and nucleic acids to nearby or distant cells11. Compared to conventional nanoparticles, such as viruses and synthetic nanocarriers, endogenously derived exosomes demonstrate superior biocompatibility, evade phagocytosis, and significantly reduce immunogenicity12. Specifically, exosomes can readily infiltrate the extracellular matrix of tumor tissue, unaffected by the tumor microenvironment (TME), thereby overcoming the challenges of cell therapy13. Owing to these properties of exosomes, immune cell-derived exosomes (IEXs) have emerged as key immune response modulators that can regulate the TME and even directly shape antitumor activity4,13,14. Given these unique and valuable biological and pharmacological properties, IEXs have attracted considerable scientific interest as a novel strategy for cancer immunotherapy.
Importantly, IEXs can be designed to acquire therapeutic potential and improve the efficacy of existing agents15. In recent years, various exosome modification strategies, including genetic engineering, chemical modification, and cargo transport, have been developed to boost their therapeutic potential16,17. Additionally, preconditioning of parental cells with cytokines that augment immune cell function can enhance the secretion or antitumor efficacy of their exosomes18. We propose that exosomes that trigger a higher level of immune response against cancer through various manipulations can pave the way for novel directions in cancer immunotherapy.
In this review, the different strategies employed to design exosomes are investigated, and the recent therapeutic applications of modified innate and adaptive IEXs are discussed. The potential of these modified exosomes to serve as an innovative tool in the fight against cancer inspires further research and development in cancer immunotherapy.
Modification strategies of IEXs for cancer immunotherapy
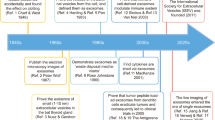
With the increase in the understanding of the biological properties of IEXs, there is a growing interest in research aimed at manipulating these exosomes to optimize their therapeutic potential16,17,18,19,20. A wide range of techniques have been employed for such modifications, from parental cell preconditioning to cargo packaging and surface engineering (Fig. 1). These modifications have revealed promise for cancer treatment by improving the target specificity, immunogenicity, biodistribution, and pharmacokinetics of exosomes.
IEXs can undergo modifications to either encapsulate therapeutic molecules or display them on the IEX surface. Pretreatment of immune cells with cytokines enhances IEX efficacy. Genetic engineering, using viral vectors or plasmids, packages therapeutics inside IEXs or expresses molecules such as antibodies on the IEX surface. Physical methods, such as electroporation, sonication, freeze‒thaw cycles, and extrusion, increase the permeability of the exosome membrane to facilitate the loading of drugs. Chemical modifications, both covalent and noncovalent, allow for the display of ligands or receptors on the IEX surface. Created with BioRender.com.
Parental cell preconditioning
Cytokines are important factors in the stimulation of the immune system to regulate immune cell activity21. Growing evidence suggests that cytokine pretreatment of parental cells can promote IEX activity to enhance therapeutic efficacy22,23,24,25,26. DC-derived exosomes (DEXs) preconditioned with interferon-γ (IFN-γ), which stimulates immature DC differentiation into mature DCs, augmented natural killer (NK) cell-mediated antitumor efficacy against non-small cell lung cancer (NSCLC) patients22. Similarly, IFN-γ-treated macrophages exhibited an M1 phenotype, and exosomes derived from these cells migrated to the lymph nodes, creating a proinflammatory microenvironment23. Interleukin (IL)-15 and IL-21-stimulated NK cell-derived exosomes possessed profound cytotoxic activity24. Furthermore, it was demonstrated that CD4+ T cell-derived exosomes pretreated with IL-2, a key regulator of T cells, increase the cytotoxicity of CD8+ T cells25. Li et al. elucidated that exosomes from CD8+ T cells cultured with IL-12 can promote the proliferation of bystander resting CD8+ T cells and the production of IFN-γ and granzyme B26. Thus, IEXs generated from cytokine-pretreated parental cells appear to be a step-up from natural exosomes. With the absence of specialized equipment requirements and cost efficiency, this approach holds considerable promise in clinical applications.
Cargo packaging into exosomes
Exosomes have emerged as an attractive drug delivery system (DDS) due to their low toxicity, high biocompatibility, and stability5,17,19,20. Cargo can be packaged by endogenous and exogenous loading methods into exosomes27. Endogenous cargo loading is typically performed through parental cell modification using viral vectors and plasmids that are commonly employed for nucleotide or protein loading19,27. Kaban et al. utilized lentiviruses produced from HEK293T cells to load BCL-2 siRNA into NK cell-derived exosomes. This process allows specific siRNAs to be overexpressed in NK cell-derived exosomes, inducing breast cancer cell apoptosis28. However, despite the high loading efficiency, toxicity and stability issues persist, and there are concerns regarding the alterations in the biological activity of the exosomes due to modifications of gene expression in the producing cells20. Exogenous cargo loading employs techniques such as electroporation, sonication, freeze‒thaw cycles, extrusion, and saponin treatment to load small-molecule drugs5,19,20. For instance, electroporation creates small pores in the exosome membrane through an electric field, facilitating drug diffusion into the exosome19,20. The integrity of the exosome membrane is restored after drug loading17. Han et al. successfully loaded the antitumor drug paclitaxel (PTX) into exosomes isolated from NK cells using electroporation to increase apoptosis of MCF-7 cells29. However, the electroporation process can potentially compromise the stability of exosomes, resulting in a diminished loading capacity19. An alternative method, sonication, facilitates drug permeation by decreasing the microviscosity of the exosomal membrane19. Using sonication, PTX was loaded into exosomes derived from the M1 phenotype polarized via IFN-γ. These M1 exosomes transported PTX into the tumor tissue and accelerated its antitumor effects30. However, it is important to note that sonication can impose a certain degree of membrane damage5. Although the strategies to engineer exosomes still show limitations, drug delivery through the manipulation of these IEXs has successfully inhibited cancer cells while also reducing side effects and enhancing treatment outcomes.
Genetic engineering of the exosome surface
Exosomes exhibit stable circulation within the bloodstream, but they present challenges in targeting specific cells31. Several strategies have been proposed to improve tumor-specific targeting in exosome-based cancer immunotherapy17,20,31. Strategies for exosome surface engineering have been divided into genetic engineering and chemical modification, and these approaches allow tumor tissue-specific therapy17,20,31. Genetic engineering approaches are useful for displaying targeted ligands on the exosome membrane. Parental cells can express the desired membrane-bound protein via lentiviral packaging techniques or transfection with a plasmid encoding the gene of interest32,33,34. Overexpressed proteins in donor cells subsequently confer modifications to the membrane surface of exosomes secreted by these cells. An illustrative example is DCs, which were transfected with the plasmid vector pcDNA3.1(+) encoding the anti-programmed cell death protein-1 (PD-1) single-chain variable fragment gene, enabling the engineering of membrane-localized anti-PD-1 antibodies. Exosomes isolated from these modified cells then reinvigorate exhausted CD8+ T cells, thereby improving cytotoxic T lymphocyte (CTL) responses32.
Recently, membrane-tethering technology for proteins (MTFP) has been introduced as a promising strategy to display bioactive proteins, such as cytokines and antibodies, on the cell surface21. MTFP expresses cytokines and antibodies via a glycine-serine linker with the transmembrane domain of the platelet-derived growth factor receptor (PDGFR) on the exosome membrane. Additionally, the linker provides flexibility to allow an increase in accessibility to neighboring receptor molecules. Remarkably, cytokines expressed in cells with MTFP exert an autocrine effect, triggering continuous downstream signaling of receptors in a membrane-anchored form. Intriguingly, IL-2 surface tethering on T cells using MTFP facilitated the self-activation of T cells and caused a dramatic enrichment of antitumor miRNAs within exosomes derived from these T cells. IL-2 tethering by MTFP allowed both internal reprogramming of exosomes and external drug delivery, thus enhancing the antitumor efficacy of exosomes33. Moreover, CD8+ T cell-derived exosomes tethered with both anti-epidermal growth factor receptor (EGFR) antibodies and IL-2 via MTFP specifically induced EGFR-positive cancer cell death through immune activation34. These genetic modification strategies for IEXs represent a viable avenue for the creation of novel targeted therapeutics.
Chemical modification of the exosome surface
IEXs can undergo chemical alterations to display both natural and synthetic ligands on their surface. Chemical conjugation encompasses both covalent and noncovalent modifications17,31. The direct attachment of antigens or other molecules to exosomes using click chemistry has been used as an effective covalent surface engineering method. Click chemistry is a copper-catalyzed azide-alkyne cycloaddition reaction that facilitates a bioorthogonal bond between an azide and an alkyne group35. However, owing to the cytotoxic effects of copper, a strain-promoted azide-alkyne cycloaddition through a strained cyclooctyne has been developed as a copper-free reaction35. In this approach, azide-modified M1 macrophage-derived exosomes were simultaneously conjugated with dibenzocyclooctyne (DBCO)-modified anti-CD47 and anti-SIRPα antibodies via benzoic-imine linkages. These pH-sensitive benzoic-imine bonds were cleaved in the acidic TME. This leads to the release of anti-SIRPα and anti-CD47 antibodies, thereby increasing tumor cell phagocytosis36. Unlike covalent modifications, noncovalent coupling, such as electrostatic and hydrophobic interactions, is a strategy for the stable modification of biological membranes17,31. The lipid bilayer membrane of exosomes facilitates the spontaneous incorporation of amphiphilic substances via hydrophobic interactions. Kim et al. successfully conjugated aminoethyl anisamide (AA), a sigma ligand, into exosome membranes based on polyethylene glycol (PEG)-grafted 1,2-distearoyl-sn-glycero-3-phosphoethanolamine (DSPE-PEG). These engineered exosomes exhibited high targeting efficacy for sigma receptors, which are overexpressed in lung cancer, and accumulated efficiently in cancer cells upon systemic administration, leading to prolonged survival in a lung metastasis mouse model37. Furthermore, DSPE-PEG is an FDA-approved material for medical use that can be widely applied to exosome membrane modification to enhance its clinical potential17.
Overall, to address their limitations alongside technological advances, current strategies for exosome modifications have continuously evolved. These challenges can be sequentially addressed through multifaceted manipulations, and the integration of these diverse engineering strategies can potentiate robust antitumor efficacy, offering a novel and innovative approach to cancer immunotherapy.
Modification of innate IEXs
Exosomes from innate immune cells, including DCs, NK cells, macrophages, and neutrophils, are vital in immune surveillance and response18. These exosomes carry the immunological traits of their parent cells and can interact with other immune cells. To amplify their inherent antitumor properties, they can also be engineered, making them promising for cancer immunotherapy16. In the following section, we discuss the unique characteristics of each type of engineered innate IEX, as uncovered by recent research (Fig. 2 and Table 1).
Modified innate IEXs affect various immune cells and cancer cells within the TME. DEXs engineered with tumor-derived antigens, T cell-targeting antibodies, and cytokines activate CD8+ T cells. NK cell-derived exosomes exert cytotoxic effects through enhanced lytic proteins due to cytokine stimulation or mediate cell death via delivery of chemical drugs or antitumor miRNAs. M1 macrophage-derived exosomes amplify antitumor response by directly killing cancer cells via drug delivery or promoting M2-to-M1 macrophage polarization. Neutrophil-derived exosomes equipped with SPIONs and loaded with DOX target tumor and exhibit tumor suppressive activity. Created with BioRender.com.
DEXs
DCs are the most effective APCs, initiating antigen-specific immune responses and acting as a bridge between innate and adaptive immune responses. In the TME, DCs present tumor-specific antigens through major histocompatibility complex class-I (MHC-I) and -II (MHC-II) molecules to effector T cells in cooperation with accessory costimulatory molecules such as CD80 and CD8638,39. Since a study demonstrated the ability of DEX to express functional MHC-I and MHC-II molecules and induce tumor regression via CTL activation, DEXs have become a significant cancer immunotherapy strategy40,41. The presence of C-C motif chemokine receptor 7 molecules on the DEX membrane allows them to migrate to T cells in the spleen, and they can express intracellular adhesion molecule-1 (ICAM-1) to promote recruitment to T cells through binding to lymphocyte function-associated antigen-1, a surface mediator of T cells42,43. Additionally, DEXs directly activate NK cells in MHC-independent manners, including through IL-15Rα, tumor necrosis factor (TNF) superfamily ligand, and natural killer Group 2 member D (NKG2D) on their surface44,45.
The capacity of DEXs to enhance antitumor immune responses is amplified after maturation stimuli. For instance, exosomes from lipopolysaccharide-induced mature DCs showed 50–100-fold more potent antigen-specific T cell activation than exosomes from immature DCs46. These mature DEXs exhibited notably high expression of miR-15547. Moreover, DEXs obtained after incubation with ovalbumin (OVA), a representative tumor-specific antigen, demonstrated the ability to activate both CD4+ T cells and B cells, leading to enhanced CTL responses48. DEXs, stimulated using the Toll-like receptor 3 agonist poly (I:C) and loaded with the B16 antigen, proliferated effector CD8+ T cells and recruited NK and NK-T cells to tumors in melanoma-bearing animals49. DEXs can offer better stability and easier manipulation than DCs50, leading to various efforts to boost their therapeutic effect. Particularly, in an orthotopic hepatocellular carcinoma (HCC) mouse model, DEXs engineered to express the HCC antigen α-fetoprotein (AFP) revealed a strong antitumor response by reducing immunosuppressive cytokines, such as IL-10 and transforming growth factor (TGF)-β, and increasing IFN-γ-expressing CD8+ T cells51. These results underscore the potential of engineered DEXs as cell-free vaccines for HCC immunotherapy. Further investigations involving DEXs engineered with HCC-targeting peptides, AFP, and immune adjuvants (DEXP&A2&N) to promote the recruitment and activation of DCs demonstrated complete tumor eradication in orthotopic HCC mice by activating both innate and adaptive immunity52. Notably, in light of the limited potency of ICBs, a cornerstone of immunotherapy, several therapeutic modifications were applied to DEXs32,53,54,55. Fan et al. developed DC exosomes engineered with anti-CD3 and anti-EGFR antibodies. Precultured with OVA, modified DEXs activated T cells via MHC-antigen peptide complexes and CD86 costimulatory molecules and acted as a bridge between cancer cells and T cells by simultaneously targeting T cell surface CD3 and EGFR on cancer cells. Surprisingly, these exosomes effectively inhibited tumor recurrence and metastasis by upregulating programmed death-ligand 1 (PD-L1) expression in tumors, reducing the immune escape of tumor cells when combined with ICB53. Liu et al. proposed an alternative therapy for anti-PD-1 antibodies through the direct expression of anti-PD-1 antibodies on DEXs. These engineered exosome platforms integrating antigen self-presentation and immune suppression reversal (ASPIRE) can directly present neoantigens to CD8+ T cells and have shown the potential to overcome immune tolerance by enhancing the immune function of anti-PD-1 antibodies and CD28/B7 costimulation32. Additionally, Jung et al. produced DEXs carrying both anti-cytotoxic T lymphocyte associated protein (CTLA)-4 antibodies and tumor antigens to improve the response rate of anti-CTLA-4 antibodies and reduce toxicity. These exosomes prevented side effects by exclusively activating tumor-specific CTLs by blocking CLTA-4 while presenting tumor antigens54. To treat immunotherapy-resistant breast cancer, IL-2-tethered exosomes derived from personalized autologous DCs pulsed with patient tumor lysates sensitized tumor cells to ICBs through lymphocyte targeting and IL-2-mediated immune cell activation55. These multipurpose DEXs with more than one modification showed synergistic effects of activating immune responses and inhibiting immune escape. Such a strategy holds significant value as a combination immunotherapy platform capable of augmenting the efficacy of ICB therapy.
NK cell-derived exosomes
NK cells, as an integral component of the innate immune response, contribute to adoptive immunotherapy and exhibit functional activity against metastatic or hematological cancers56,57. In addition to direct utilization of NK cells, recent studies have revealed the remarkable antitumor efficacy of NK cell-derived exosomes58. Exosomes from these cells possess typical NK cell components, including perforin, granzymes, Fas ligand (FasL), and granulysin59. By utilizing the well-established direct killing pathway, these exosomes effectively eliminate cancer cells, such as melanoma and breast cancer cells59,60.
In addition to their cytotoxic effects, there is a growing body of literature elucidating various modifications aimed at enhancing their antitumor activity in cancer immunotherapy. Exosomes derived from IL-15- and IL-21-activated NK-92 cells revealed enhanced cytolytic activity against cervical or lung cancer24. Zhu et al. discovered that exosomes derived from IL-15-primed NK-92MI cells exhibited notably increased cytotoxicity against various human cancer cell types, such as glioblastoma, breast cancer, and thyroid cancer cells61. Moreover, exosomes released by IL-12-, IL-15-, and IL-18-stimulated NK cells, including primary NK cells and NK-92 cells, showed enhanced efficacy in targeting tumor spheroids by utilizing the interaction between NKG2D and its ligands MHC-I chain-related protein A and B62. Interestingly, based on the cytolytic effect of NK cell-derived exosomes, their use as a DDS in cancer immunological applications has been remarkably attractive. Han et al. demonstrated that NK cell-derived exosomes loaded with PTX showed a significantly enhanced antitumor effect on breast cancer compared to PTX treatment alone. This study suggests that these exosomes can serve as competitive tools for drug delivery29. Additionally, surface-engineered NK cell-derived exosomes can enhance their targeting capability and binding affinity toward other substances, consequently augmenting their duration of action and stability in vivo. In a study by Nie et al., NK cell-derived exosomes conjugated on the CTL surface were released at low pH in the TME, leveraging their tumor-targeting capability and promoting the cytotoxic action of CTLs against tumors63. In another study, a cocktail therapy strategy was employed, combining NK cell-derived exosomes with dendrimer cores loaded with therapeutic miRNAs, thus enabling targeted tumor therapy64. These innovative strategies underscore the potential of NK cell-derived exosomes in improving tumor-specific treatments. Altogether, these studies imply the high utility of NK cell-derived exosomes in advancing cancer immunotherapy, highlighting the efficacy of modified exosomes as valuable tools for cancer treatment.
Macrophage-derived exosomes
Macrophages can undergo polarization into two distinct phenotypes upon exposure to environmental signals, namely, pro-inflammatory M1 and anti-inflammatory M2 macrophages65,66. M2 macrophages, which secrete immunosuppressive cytokines, including IL-4, IL-10, IL-13, and TGF-β, contribute to the inhibition of T cell immunity in the TME and increase tumor growth67,68. Conversely, M1 macrophages show tumoricidal activity through the secretion of tumor-killing molecules, such as reactive oxygen species (ROS), inducible nitric oxide synthase, and immunostimulatory cytokines, including TNF-α, IFN-γ, and IL-1269,70,71. Considering their noteworthy features, exosomes derived from M1 macrophages have gained prominence as influential entities in cancer immunotherapy. It has been reported that M1 macrophage-derived exosomes, which have absorbed antigens, can subsequently deliver them to CD4+ or CD8+ T cells through receptor‒ligand interactions promoted by specific surface ligands and adhesion molecules such as tetraspanins, phosphatidylserine, and ICAM-172. Besides, these exosomes can serve as adjuvants for antitumor therapeutic agents, augmenting their efficacy in cancer treatment. M1 macrophage-derived exosomes demonstrated a distinctive ability to target lymph nodes, where they were selectively internalized by local macrophages and DCs. This led to the activation of Th1 inflammatory immune responses within the localized microenvironment73. Considering the transient and plastic nature of macrophages, Choo et al. devised M1 exosome mimetics to successfully reprogram M2 macrophages into the M1 phenotype, leading to a notable improvement in the therapeutic efficacy of anti-PD-L1 therapy73.
To increase the therapeutic efficacy of these exosomes in cancer treatment, a multitude of approaches are currently being investigated to modify exosomes derived from M1 macrophages. In the context of cancer vaccines, exosomes derived from M1 macrophages stimulated with IFN-γ play a crucial role in increasing antitumor activity. These exosomes contributed to building a pro-inflammatory microenvironment within the lymph nodes, thereby enhancing the efficacy of cancer vaccines23. Furthermore, a study highlighted that exosomes derived from M1-polarized macrophages exhibited the capacity to encapsulate PTX. These PTX-loaded M1 exosomes have shown the ability to enhance antitumor efficacy by establishing a proinflammatory microenvironment. This enhanced inflammatory milieu led to the upregulation of the expression of caspase-3, which is a pivotal mediator of apoptotic cell death, in breast cancer cells30. To impart a targeting ability to PTX-loaded M1 macrophage-derived exosomes, Kim et al. conjugated PTX-loaded M1 macrophage exosomes with an AA-PEG vector moiety that specifically recognizes sigma receptors overexpressed on specific lung cancer cells. The modified exosomes demonstrated enhanced efficacy in cancer treatment and significantly improved survival outcomes in mice with lung metastases37. Gunasekaran et al. modified M1 macrophage-derived exosomes with NF-κB p50 siRNA and miR-511-3p to induce M1 polarization and decorated the exosome surface with an IL4R binding peptide (IL4RPep-1) to specifically target IL-4 receptors on M2 macrophages. These modified exosomes, referred to as IL4R-Exo (si/mi), were absorbed by M2 macrophages, which downregulated the target genes, reduced M2 marker expression and increased M1 marker expression74. In an interesting study conducted by Wang et al., a novel approach was employed for chimeric exosome generation. These exosomes were derived from macrophage-tumor hybrid cells (aMT-exos), where M1 macrophages phagocytosed tumor cell nuclei. The unique characteristic of aMT-exos involves their tropism toward both lymph nodes and tumors. These modified exosomes displayed the ability to facilitate T cell activation and proliferation through direct exosome stimulation and traditional APC-mediated stimulation. The cumulative effect of these dual pathways led to the augmentation of anti-PD-1 antibody treatment efficacy, illustrating the potential of aMT-exos as a valuable tool in enhancing immunotherapeutic interventions75. Overall, these findings strongly indicate that modified M1 macrophage-derived exosomes hold great promise for immunoregulation and cancer therapy.
Neutrophil-derived exosomes
Neutrophils, which are the predominant leukocytes in circulation, perform a variety of functions through the release of cytotoxic enzymes and effector molecules, ROS synthesis, phagocytosis and the generation of neutrophil extracellular traps76. Although the body of knowledge regarding exosomes released from other immune cells is continuously increasing, there remains a significant gap in understanding the specific contributions of neutrophil-derived exosomes. The limited exploration of these exosomes can be attributed to challenges associated with the short lifespan of neutrophils and the complexities involved in their isolation and manipulation77. Nonetheless, with the growing body of research on the pro-inflammatory role of IEXs, recent findings have shed light on the potential of neutrophil-derived exosomes as promising therapeutic agents in cancer therapy78,79.
On the basis of the spatiotemporal production mechanism, neutrophil-derived exosomes can be categorized into neutrophil-derived microvesicles (NDMVs) and neutrophil-derived trails (NDTRs)80. NDMVs are generated by neutrophils present at the site of inflammation, whereas NDTRs originate from neutrophils migrating from blood vessels to inflamed tissue81,82. While they share a common ability to effectively kill bacteria through ROS and granules, they often present significant distinctions83. NDMVs, characterized by the presence of protease-enriched granules, mostly exert anti-inflammatory effects by suppressing the expression of inflammatory genes in various cell types, including monocyte-derived DCs, macrophages and NK cells84,85,86. NDMVs have been observed to promote M0 macrophage polarization toward an anti-inflammatory phenotype, whereas NDTRs induce their polarization toward a pro-inflammatory phenotype80. Recently, emerging reports have highlighted the utility of neutrophil-derived exosome modification to propose a novel paradigm in cancer immunotherapy. In particular, neutrophil-derived exosomes loaded with drugs have emerged as a promising therapeutic approach for brain tumors by exploiting their distinctive abilities to be recruited to inflammatory sites and effectively penetrate the blood‒brain barrier (BBB)78,87. Wang et al. demonstrated that neutrophil-derived exosomes carrying doxorubicin (DOX) can rapidly cross the BBB and migrate into the brain. Moreover, intravenous injection of these exosomes in a glioma-bearing mouse model efficiently inhibited tumor growth and increased the survival rate78. Additionally, Zhang et al. successfully developed a targeted approach to cancer treatment by loading neutrophil-derived exosomes with DOX and incorporating superparamagnetic iron oxide nanoparticles (SPIONs). This innovative strategy ensured targeted drug delivery, resulting in the inhibition of tumor growth in mouse models bearing liver, colon, or gastric cancer79. These strategies underscore the potential of neutrophils as newly recognized promising candidates in the market of IEXs for cancer treatment.
Modification of adaptive IEXs
Adaptive immunity consists of B cell-mediated humoral immunity and T cell-mediated cellular immunity, conferring the ability for the human body to mount targeted defenses against harmful agents, encompassing bacteria, viruses, toxins, and even cancer88,89. Similar to innate immune cells, adaptive immune cells also contribute significantly to antitumor immune responses89,90. Recently, there has been increasing interest in exploring the functions of adaptive IEXs within the cancer-immune system18. These exosomes have emerged as promising candidates for inducing antitumor immune responses, prompting extensive research into engineering strategies to augment their antitumor effects. In the following section, we aim to comprehensively review the antitumor functions of adaptive IEXs, including those derived from B cells and T cells, and examine various strategies involving modified exosomes for cancer therapy (Fig. 3 and Table 2).
Engineered exosomes derived from adaptive immune cells serve to enhance antitumor function. Left panel: Engineered B cell-derived exosomes, which display tumor-targeting anti-CD20 antibodies on their surface and load ZnO NCs, induce tumor-specific cell death. Middle panel: CD4+ T cell-derived exosomes tethered with IL-2 via MTFP amplify the antitumor efficacy through an autocrine effect. These exosomes diminish PD-L1 expression on tumor cells while increasing the proliferation and activity of CD8+ T cells. Right panel: Exosomes derived from CD8+ T cells expressing tumor-targeting PD-1, anti-EGFR antibodies, or CARs bind to tumor and induce tumor cell death. Created with BioRender.com.
B cell-derived exosomes
Beyond their role in specific immunoglobulin generation, B cells possess the capacity to modulate immune cell activities via various mechanisms, including antigen presentation, cytokine secretion and supportive costimulatory signals90,91. Similar to innate immune cells, B cells release exosomes that mimic the functional attributes of B cells in the immune system. Exosomes released from B lymphomas after heat shock exposure display augmented expression of immunogenic molecules such as MHC I, MHC II, CD40, CD86, RANTES, and IL-1β, with increases in HSP60 and HSP9092. These exosomes showed an elevated immunogenicity and delivered MHC complexes to induce CD4+ and CD8+ T cell proliferation and cytokine secretion, ultimately enhancing CTL responses93. In an intriguing investigation by Dumontel et al., B cell-derived exosomes were subjected to engineering with zinc oxide nanocrystals (ZnO NCs), which responded to external stimuli such as acoustic shock waves. The resulting engineered exosomes displayed remarkable cytotoxicity against Burkitt’s lymphoma cells. Furthermore, an anti-CD20 monoclonal antibody was integrated onto these exosomes to enable precise lymphoma cell targeting, further enhancing their therapeutic potential94. While limited studies have specifically evaluated the feasibility of utilizing modified B cell-derived exosomes in cancer treatment, such studies provide valuable insights into the enhancement of therapeutic potential through the modification of B cell-derived exosomes.
CD4+ T cell-derived exosomes
T cells, which are pivotal immune cells in the body, play important roles in orchestrating and augmenting the immune response against pathogens, self-antigens, allergens, and cancers95. T cells can be categorized into various subsets, mainly cytotoxic CD8+ T cells and CD4+ T helper cells95. Among these subsets, CD4+ T cells play a vital role in immune modulation by engaging in interactions with other immune cells96,97. They primarily contribute to the antitumor immune response of CD8+ T cells and promote antibody production by B cells either through direct cell-to-cell interactions or IL-2 release96,97. With a recent interest in the field, CD4+ T cell-derived exosomes are considered promising agents that can mediate antitumor effects in cancer immunotherapy. In a study by Lu et al., it was revealed that CD4+ T cell-derived exosomes exerted a stimulating effect on humoral immune responses by enhancing the proliferation, activation, and antibody production of B cells98. This effect is mediated by exosome uptake facilitated by CD40L expressed on their surface.
As the understanding of the inherent antitumor roles of CD4+ T cells is increased, there have been emerging reports of studies focused on enhancing antitumor effects through the modification of CD4+ T cell-derived exosomes. Shin et al. reported that CD4+ T cell-derived exosomes enhanced the antitumor response of CD8+ T cells through miR-25-3p, miR-155-5p, miR-215-5p, and miR-375 without affecting regulatory T cells, resulting in the suppression of melanoma growth. Moreover, they found that IL-2 reinforced the antitumor efficacy of CD4+ T cell-derived exosomes25. In a study by Jung et al., IL-2-tethered exosomes were generated from engineered Jurkat T cells expressing IL-2 at the plasma membrane using a flexible linker to induce an autocrine effect. The surface engineering of IL-2 led to significant alterations in the miRNA profiles within these exosomes, resulting in the activation of CD8+ T cells and downregulation of PD-L1 expression in melanoma through differentially expressed miRNAs33. We suggest that these modified CD4+ T cell-derived exosomes can serve as novel activators of CD8+ T cells, offering a new approach to amplify antitumor efficacy in cancer immunotherapy.
CD8+ T cell-derived exosomes
CD8+ T cells are a distinct population of white blood cells that exhibit their cytotoxic effects through the release of various cytokines. These cells play a pivotal role in specifically eliminating tumor cells, serving as a crucial defense mechanism in antitumor immunity99. According to multiple studies, CD8+ T cell-derived exosomes in cancer treatment undoubtedly show antitumor effects26,100,101,102. For instance, CD8+ T cell-derived exosomes possessed various cytotoxic molecules and either activated bystander T cells or suppressed lesional mesenchymal cells, establishing their multifaceted functional role26,101. Additionally, fully activated CTL-derived exosomes can promote the activation of CTLs with low affinity for antigens, thereby facilitating a comprehensive immune response102.
Most importantly, the modification of CD8+ T cell-derived exosomes has emerged as a thriving field of research within exosome-based cancer immunotherapy. In a recent study by Cho et al., it was revealed that engineered exosomes derived from primary CD8+ T cells expressing IL-2 and anti-EGFR antibodies not only demonstrated potent antitumor effects on A549 human lung cancer cells but also exhibited an augmented capacity for cancer targetability34. In light of the immunosuppressive role of PD-L1 expressed on cells or exosomes, Li et al. elucidated that exosomes derived from PD-1-expressing cytotoxic T cells had the capability to neutralize PD-L1, thereby increasing the activity and proliferation of CD8+ effector T cells and directly killing tumor cells through FasL and granzyme B103. Furthermore, IL-12-activated CTL-derived exosomes showed a unique capability to directly activate naive bystander CD8+ T cells, stimulating them to produce IFN-γ and granzyme B in the absence of antigens26. Moreover, CAR-T cells are highly esteemed in clinical studies as an emerging and effective modality for tumor treatment. Despite the remarkable potential of CAR-T cells as a systemic cell-based therapy, they have been associated with certain adverse effects, such as CRS104. Considering these factors, exosomes derived from CAR-T cells have emerged as a promising alternative to cell-based therapeutics for antitumor treatment. Yang et al. conducted a study in which they explored the potential of exosomes derived from mesothelin-targeted CAR-T cells for cancer immunotherapy. Interestingly, these exosomes revealed a striking resemblance to their parental cells, retaining crucial surface membrane molecules such as CARs, CD3, CD8 and T cell receptors (TCRs)105. Moreover, their therapeutic capacity was found to be comparable to that of the parental CAR-T cells, showing effective antitumor activity against triple-negative breast cancer cells without significant side effects. Additionally, the CAR-T cell-derived exosomes have been demonstrated to reduce CRS, thereby establishing them as a comparatively safer alternative to CAR-T cells106.
Clinical application of the modified IEXs and challenges
Although IEXs offer numerous advantages, including their natural antitumor functions and ability to efficiently deliver therapeutic cargo, only a limited number of clinical trials have used these exosomes in cancer treatment. Among various IEXs, DEXs from cancer patients were found to be feasible and safe for immunotherapy in clinical trials. In a phase 1 clinical trial, melanoma-associated antigen gene-loaded DEXs showed modest responses and were well tolerated by patients with NSCLC or melanoma107,108. Subsequently, exosomes derived from mature DCs preconditioned by IFN-γ were used in a phase 2 clinical trial to enhance the limited T cell responses induced by DEXs22. In that trial, despite no notable changes in the levels or phenotype of circulating CD4+ and CD8+ T cells in peripheral blood, the administration of IFN-γ-matured DEXs increased NK cell activity in NSCLC patients after chemotherapy cessation. Although the clinical trial did not achieve the primary endpoint, defined as 50% of patients with progression-free survival after 4 months of chemotherapy cessation, the modified DEXs revealed remarkable antitumor responses and excellent tolerability, demonstrating greater potential for clinical application.
Despite the extensive interest on DEXs, IEX-based therapies still experience unresolved limitations that have hindered their widespread clinical application in cancer treatment109. Several hurdles need to be overcome for the clinical application of IEXs. First, it is necessary to address the issue of large-scale production of exosomes110. Although it has been reported that therapeutic DEXs can be prepared on a large scale through rapid purification, further testing is still required in different cell types111. Additionally, the establishment of cell culture and standardized exosome purification methods that can allow large-scale production of exosomes is crucial112. Second, the challenges in exosome storage, such as aggregation and cargo degradation during the freeze–thaw process, further limit their clinical use113. Even using the most comprehensive method of −80 °C cryopreservation, exosomes can undergo morphological changes, and biological activity may decline with long-term storage114. Therefore, there is an urgent need to study the long-term storage technology of exosomes to protect their biological activity and render them suitable for clinical applications. Third, exosomes derived from various types of cells are highly different in size, function, and composition, and this heterogeneity can be a major hurdle. Although several exosome isolation and characterization techniques have been developed to understand and resolve the heterogeneity in the biophysical properties and composition of exosomes, additional studies are needed to surmount their heterogeneity114,115. Employing IEXs for cancer therapeutics is attractive and promising. Additionally, modified IEXs have the potential to be an innovative therapeutic strategy; thus, more systematic studies to address the above challenges contribute to bringing these modified IEXs one step closer to their expanded clinical application.
Conclusions and prospects
In this review, we introduce exosome modification strategies and provide a comprehensive overview of the therapeutic application of these modified IEXs in cancer treatment. Currently, extensive investigations into the structure, biogenesis, secretion, and function of exosomes have not only elucidated their significant role as mediators of cell-to-cell communication but also bolstered their potential as promising therapeutic agents11. In particular, IEXs possess several advantages, including excellent biocompatibility, low immunogenicity, high stability, and inherent antitumor activity, gathering significant interest in cancer therapeutics4,11,13,15,18. Simultaneously, efforts to enhance the efficacy of IEXs are underway through various strategies, including drug or antigen loading, surface engineering with targeting molecules and boosting exosomes with cytokine stimulation5,17,22,31. However, these methods still pose multiple challenges and need further optimization. Electroporation and sonication can cause exosome aggregation and membrane damage19. Genetic modification is confined to molecules suitable for genetic encoding, thus encompassing only a restricted range of molecules17. While chemical engineering can conjugate a broader range of molecules to exosomes, the surface complexity of exosomes may lead to decreased reaction efficiency and a lack of precise control of site specificity17. Thus, it is important to select the appropriate modification approach based on the drug to minimize the limitations. Collectively, owing to the ongoing developments in exosome engineering strategies, modified IEXs with enhanced antitumor effects and tumor-specific targeting show significant promise in advancing next-generation exosome-based cancer immunotherapy.
References
Yang, Z., Ma, Y., Zhao, H., Yuan, Y. & Kim, B. Y. S. Nanotechnology platforms for cancer immunotherapy. Wiley Interdiscip. Rev. Nanomed. Nanobiotechnol. 12, e1590 (2020).
Yang, Y. P. Cancer immunotherapy: harnessing the immune system to battle cancer. J. Clin. Investig. 125, 3335–3337 (2015).
Dunkelberger, J. R. & Song, W. C. Complement and its role in innate and adaptive immune responses. Cell Res. 20, 34–50 (2010).
Yan, W. & Jiang, S. Immune Cell-Derived Exosomes in the Cancer-Immunity Cycle. Trends Cancer 6, 506–517 (2020).
Zhang, H. et al. Exosomes as smart drug delivery vehicles for cancer immunotherapy. Front. Immunol. 13, 1093607 (2023).
Dobosz, P. & Dzieciatkowski, T. The Intriguing History of Cancer Immunotherapy. Front. Immunol. 10, 2965 (2019).
Wang, D. R., Wu, X. L. & Sun, Y. L. Therapeutic targets and biomarkers of tumor immunotherapy: response versus non-response. Signal Transduct. Target Ther. 7, 331 (2022).
Kim, H. D. & Park, S. H. Immunological and clinical implications of immune checkpoint blockade in human cancer. Arch. Pharm. Res. 42, 567–581 (2019).
Zhao, Z., Chen, Y., Francisco, N. M., Zhang, Y. & Wu, M. The application of CAR-T cell therapy in hematological malignancies: advantages and challenges. Acta Pharm. Sin. B 8, 539–551 (2018).
Xu, Z., Zeng, S., Gong, Z. & Yan, Y. Exosome-based immunotherapy: a promising approach for cancer treatment. Mol. Cancer 19, 160 (2020).
S, E. L. A., Mager, I., Breakefield, X. O. & Wood, M. J. Extracellular vesicles: biology and emerging therapeutic opportunities. Nat. Rev. Drug Discov. 12, 347–357 (2013).
Samanta, S. et al. Exosomes: new molecular targets of diseases. Acta Pharm. Sin. 39, 501–513 (2018).
Choi, S. J., Cho, H., Yea, K. & Baek, M. C. Immune cell-derived small extracellular vesicles in cancer treatment. BMB Rep. 55, 48–56 (2022).
Veerman, R. E., Gucluler Akpinar, G., Eldh, M. & Gabrielsson, S. Immune Cell-Derived Extracellular Vesicles - Functions and Therapeutic Applications. Trends Mol. Med. 25, 382–394 (2019).
Zhao, Y., Liu, T. & Zhou, M. Immune-Cell-Derived Exosomes for Cancer Therapy. Mol. Pharm. 19, 3042–3056 (2022).
Markov, O., Oshchepkova, A. & Mironova, N. Immunotherapy Based on Dendritic Cell-Targeted/-Derived Extracellular Vesicles-A Novel Strategy for Enhancement of the Anti-tumor Immune Response. Front. Pharm. 10, 1152 (2019).
Liang, Y., Duan, L., Lu, J. & Xia, J. Engineering exosomes for targeted drug delivery. Theranostics 11, 3183–3195 (2021).
Yang, P. X. et al. Immune Cell-Derived Extracellular Vesicles - New Strategies in Cancer Immunotherapy. Front. Immunol. 12, 771551 (2021).
Luan, X. et al. Engineering exosomes as refined biological nanoplatforms for drug delivery. Acta Pharmacol. Sin. 38, 754–763 (2017).
Sen, S., Xavier, J., Kumar, N., Ahmad, M. Z. & Ranjan, O. P. Exosomes as natural nanocarrier-based drug delivery system: recent insights and future perspectives. 3 Biotech 13, 101 (2023).
Noh, S. et al. Exploring Membrane-tethering Technology for Proteins as a Versatile Tool for Uncovering Novel Disease Targets and Advancing Biotherapeutic Development. Isr. J. Chem. e202300046 (2023).
Besse, B. et al. Dendritic cell-derived exosomes as maintenance immunotherapy after first line chemotherapy in NSCLC. Oncoimmunology. 5, e1071008 (2016).
Cheng, L. F., Wang, Y. H. & Huang, L. Exosomes from M1-Polarized Macrophages Potentiate the Cancer Vaccine by Creating a Pro-inflammatory Microenvironment in the Lymph Node. Mol. Ther. 25, 1665–1675 (2017).
Enomoto, Y. et al. Cytokine-enhanced cytolytic activity of exosomes from NK Cells. Cancer Gene Ther. 29, 734–749 (2022).
Shin, S. et al. Novel antitumor therapeutic strategy using CD4(+) T cell-derived extracellular vesicles. Biomaterials 289, 121765 (2022).
Li, L., Jay, S. M., Wang, Y., Wu, S. W. & Xiao, Z. G. IL-12 stimulates CTLs to secrete exosomes capable of activating bystander CD8(+) T cells. Sci. Rep. 7, 13365 (2017).
Lu, Y., Mai, Z. Z., Cui, L. & Zhao, X. Y. Engineering exosomes and biomaterial-assisted exosomes as therapeutic carriers for bone regeneration. Stem Cell Res. Ther. 14, 55 (2023).
Kaban, K. et al. Therapeutic Silencing of BCL-2 Using NK Cell-Derived Exosomes as a Novel Therapeutic Approach in Breast Cancer. Cancers. 13, 2397 (2021).
Han, D., Wang, K., Zhang, T., Gao, G. C. & Xu, H. Natural killer cell-derived exosome-entrapped paclitaxel can enhance its anti-tumor effect. Eur. Rev. Med. Pharmacol. Sci. 24, 5703–5713 (2020).
Wang, P. P. et al. Exosomes from M1-Polarized Macrophages Enhance Paclitaxel Antitumor Activity by Activating Macrophages-Mediated Inflammation. Theranostics 9, 1714–1727 (2019).
Johnson, V., Vasu, S., Kumar, U. S. & Kumar, M. Surface-Engineered Extracellular Vesicles in Cancer Immunotherapy. Cancers. 15, 2838 (2023).
Liu, C. et al. A nanovaccine for antigen self-presentation and immunosuppression reversal as a personalized cancer immunotherapy strategy. Nat. Nanotechnol. 17, 531–540 (2022).
Jung, D. et al. Reprogramming of T cell-derived small extracellular vesicles using IL2 surface engineering induces potent anti-cancer effects through miRNA delivery. J. Extracell. Vesicles 11, e12287 (2022).
Cho, H., Jung, I., Ju, H., Baek, M. C. & Yea, K. Engineered CD8(+) T cell-derived extracellular vesicles induce enhanced anti-cancer efficacy and targeting to lung cancer cells. Cytokine 169, 156249 (2023).
Algar, W. R. et al. The controlled display of biomolecules on nanoparticles: a challenge suited to bioorthogonal chemistry. Bioconjug Chem. 22, 825–858 (2011).
Nie, W. et al. Responsive Exosome Nano-bioconjugates for Synergistic Cancer Therapy. Angew. Chem. Int Ed. Engl. 59, 2018–2022 (2020).
Kim, M. S. et al. Engineering macrophage-derived exosomes for targeted paclitaxel delivery to pulmonary metastases: in vitro and in vivo evaluations. Nanomedicine 14, 195–204 (2018).
Radford, K. J., Tullett, K. M. & Lahoud, M. H. Dendritic cells and cancer immunotherapy. Curr. Opin. Immunol. 27, 26–32 (2014).
Sabado, R. L. & Bhardwaj, N. Cancer immunotherapy: dendritic-cell vaccines on the move. Nature 519, 300–301 (2015).
Andre, F. et al. Exosomes as potent cell-free peptide-based vaccine. I. Dendritic cell-derived exosomes transfer functional MHC class I/peptide complexes to dendritic cells. J. Immunol. 172, 2126–2136 (2004).
Zitvogel, L. et al. Eradication of established murine tumors using a novel cell-free vaccine: dendritic cell-derived exosomes. Nat. Med. 4, 594–600 (1998).
Gao, W. et al. Dendritic cells derived exosomes migration to spleen and induction of inflammation are regulated by CCR7. Sci. Rep. 7, 1–9 (2017).
Lindenbergh, M. F. S. & Stoorvogel, W. Antigen Presentation by Extracellular Vesicles from Professional Antigen-Presenting Cells. Annu. Rev. Immunol. 36, 435–459 (2018).
Munich, S., Sobo-Vujanovic, A., Buchser, W. J., Beer-Stolz, D. & Vujanovic, N. L. Dendritic cell exosomes directly kill tumor cells and activate natural killer cells via TNF superfamily ligands. Oncoimmunology 1, 1074–1083 (2012).
Viaud, S. et al. Dendritic Cell-Derived Exosomes Promote Natural Killer Cell Activation and Proliferation: A Role for NKG2D Ligands and IL-15R alpha. Plos One. 4, e4942 (2009).
Segura, E. et al. ICAM-1 on exosomes from mature dendritic cells is critical for efficient naive T-cell priming. Blood 106, 216–223 (2005).
Montecalvo, A. et al. Mechanism of transfer of functional microRNAs between mouse dendritic cells via exosomes. Blood 119, 756–766 (2012).
Naslund, T., Gehrmann, U., Qazi, K., Karlsson, M. & Gabrielsson, S. Dendritic cell derived exosomes need to activate both T and B cells to induce antitumor immunity. J. Immunol. 190, 2712–2719 (2013).
Damo, M., Wilson, D. S., Simeoni, E. & Hubbell, J. A. TLR-3 stimulation improves anti-tumor immunity elicited by dendritic cell exosome-based vaccines in a murine model of melanoma. Sci. Rep. 5, 17622 (2015).
Pitt, J. M. et al. Dendritic cell-derived exosomes for cancer therapy. J. Clin. Investig. 126, 1224–1232 (2016).
Lu, Z. et al. Dendritic cell-derived exosomes elicit tumor regression in autochthonous hepatocellular carcinoma mouse models. J. Hepatol. 67, 739–748 (2017).
Zuo, B. F. et al. Universal immunotherapeutic strategy for hepatocellular carcinoma with exosome vaccines that engage adaptive and innate immune responses. J. Hematol. Oncol. 15, 46 (2022).
Fan, M. et al. A CAR T-inspiring platform based on antibody-engineered exosomes from antigen-feeding dendritic cells for precise solid tumor therapy. Biomaterials. 282, 121424 (2022).
Jung, M. et al. Nanovesicle-Mediated Targeted Delivery of Immune Checkpoint Blockades to Potentiate Therapeutic Efficacy and Prevent Side Effects. Adv. Mater. 34, 2106516 (2022).
Wu, K. R. et al. Engineering an active immunotherapy for personalized cancer treatment and prevention of recurrence. Sci. Adv. 9, eade062 (2023).
Myers, J. A. & Miller, J. S. Exploring the NK cell platform for cancer immunotherapy. Nat. Rev. Clin. Oncol. 18, 85–100 (2021).
Shimasaki, N., Jain, A. & Campana, D. NK cells for cancer immunotherapy. Nat. Rev. Drug Discov. 19, 200–218 (2020).
Kang, Y. T. et al. On-Chip Biogenesis of Circulating NK Cell-Derived Exosomes in Non-Small Cell Lung Cancer Exhibits Antitumoral Activity. Adv. Sci. 8, 2003747 (2021).
Jong, A. Y. et al. Large-scale isolation and cytotoxicity of extracellular vesicles derived from activated human natural killer cells. J. Extracell. Vesicles 6, 1294368 (2017).
Zhu, L. et al. Exosomes Derived From Natural Killer Cells Exert Therapeutic Effect in Melanoma. Theranostics 7, 2732–2745 (2017).
Zhu, L. et al. Enhancement of antitumor potency of extracellular vesicles derived from natural killer cells by IL-15 priming. Biomaterials 190-191, 38–50 (2019).
Aarsund, M., Segers, F. M., Wu, Y. & Inngjerdingen, M. Comparison of characteristics and tumor targeting properties of extracellular vesicles derived from primary NK cells or NK-cell lines stimulated with IL-15 or IL-12/15/18. Cancer Immunol. Immunother. 71, 2227–2238 (2022).
Nie, W. D. et al. Natural killer cell-derived extracellular vesicle significantly enhanced adoptive T cell therapy against solid tumors via versatilely immunomodulatory coordination. Sci. China-Chem. 64, 1999–2009 (2021).
Wang, G. S. et al. Cocktail Strategy Based on NK Cell-Derived Exosomes and Their Biomimetic Nanoparticles for Dual Tumor Therapy. Cancers. 11, 1560 (2019).
Tomita, R., Sasabe, E., Tomomura, A. & Yamamoto, T. Macrophage-derived exosomes attenuate the susceptibility of oral squamous cell carcinoma cells to chemotherapeutic drugs through the AKT/GSK-3 beta pathway. Oncol. Rep. 44, 1905–1916 (2020).
Yuan, Y. et al. Macrophage-Derived Exosomal miR-31-5p Promotes Oral Squamous Cell Carcinoma Tumourigenesis Through the Large Tumor Suppressor 2-Mediated Hippo Signalling Pathway. J. Biomed. Nanotechnol. 17, 822–837 (2021).
Wei, K. et al. M2 macrophage-derived exosomes promote lung adenocarcinoma progression by delivering miR-942. Cancer Lett. 526, 205–216 (2022).
Ngambenjawong, C., Gustafson, H. H. & Pun, S. H. Progress in tumor-associated macrophage (TAM)-targeted therapeutics. Adv. Drug Deliv. Rev. 114, 206–221 (2017).
Bernsmeier, C., van der Merwe, S. & Perianin, A. Innate immune cells in cirrhosis. J. Hepatol. 73, 186–201 (2020).
Zhao, Y. et al. M1 Macrophage-Derived Exosomes Loaded with Gemcitabine and Deferasirox against Chemoresistant Pancreatic Cancer. Pharmaceutics. 13, 1493 (2021).
Qian, B. et al. M1 macrophage-derived exosomes impair beta cell insulin secretion via miR-212-5p by targeting SIRT2 and inhibiting Akt/GSK-3beta/beta-catenin pathway in mice. Diabetologia 64, 2037–2051 (2021).
Meng, W., Hao, Y., He, C., Li, L. & Zhu, G. Exosome-orchestrated hypoxic tumor microenvironment. Mol. Cancer 18, 57 (2019).
Choo, Y. W. et al. M1 Macrophage-Derived Nanovesicles Potentiate the Anticancer Efficacy of Immune Checkpoint Inhibitors. ACS Nano 12, 8977–8993 (2018).
Gunassekaran, G. R., Poongkavithai Vadevoo, S. M., Baek, M. C. & Lee, B. M1 macrophage exosomes engineered to foster M1 polarization and target the IL-4 receptor inhibit tumor growth by reprogramming tumor-associated macrophages into M1-like macrophages. Biomaterials 278, 121137 (2021).
Wang, S. et al. Macrophage-tumor chimeric exosomes accumulate in lymph node and tumor to activate the immune response and the tumor microenvironment. Sci. Transl. Med. 13, eabb6981 (2021).
Selders, G. S., Fetz, A. E., Radic, M. Z. & Bowlin, G. L. An overview of the role of neutrophils in innate immunity, inflammation and host-biomaterial integration. Regen. Biomater. 4, 55–68 (2017).
Summers, C. et al. Neutrophil kinetics in health and disease. Trends Immunol. 31, 318–324 (2010).
Wang, J. et al. Inflammatory tumor microenvironment responsive neutrophil exosome-based drug delivery system for targeted glioma therapy. Biomaterials 273, 102784 (2021).
Zhang, J. et al. Engineered neutrophil-derived exosome-like vesicles for targeted cancer therapy. Sci. Adv. 8, eabj8207 (2022).
Hong, C. W. Extracellular Vesicles of Neutrophils. Immune Netw. 18, e43 (2018).
Hyun, Y. M. et al. Uropod elongation is a common final step in leukocyte extravasation through inflamed vessels. J. Exp. Med. 209, 1349–1362 (2012).
Youn, Y. J. et al. Neutrophil-derived trail is a proinflammatory subtype of neutrophil-derived extracellular vesicles. Theranostics 11, 2770–2787 (2021).
Dalli, J. et al. Heterogeneity in neutrophil microparticles reveals distinct proteome and functional properties. Mol. Cell Proteom. 12, 2205–2219 (2013).
Eken, C. et al. Polymorphonuclear neutrophil-derived ectosomes interfere with the maturation of monocyte-derived dendritic cells. J. Immunol. 180, 817–824 (2008).
Eken, C. et al. Ectosomes released by polymorphonuclear neutrophils induce a MerTK-dependent anti-inflammatory pathway in macrophages. J. Biol. Chem. 285, 39914–39921 (2010).
Pliyev, B. K., Kalintseva, M. V., Abdulaeva, S. V., Yarygin, K. N. & Savchenko, V. G. Neutrophil microparticles modulate cytokine production by natural killer cells. Cytokine 65, 126–129 (2014).
Wu, M. et al. MR imaging tracking of inflammation-activatable engineered neutrophils for targeted therapy of surgically treated glioma. Nat. Commun. 9, 4777 (2018).
Palucka, A. K. & Coussens, L. M. The Basis of Oncoimmunology. Cell 164, 1233–1247 (2016).
Thommen, D. S. & Schumacher, T. N. T Cell Dysfunction in Cancer. Cancer Cell 33, 547–562 (2018).
Helmink, B. A. et al. B cells and tertiary lymphoid structures promote immunotherapy response. Nature 577, 549–555 (2020).
Satitsuksanoa, P., van de Veen, W. & Akdis, M. B-cell responses in allergen immunotherapy. Curr. Opin. Allergy Clin. Immunol. 19, 632–639 (2019).
Chen, W. et al. Efficient induction of antitumor T cell immunity by exosomes derived from heat-shocked lymphoma cells. Eur. J. Immunol. 36, 1598–1607 (2006).
Klinker, M. W., Lizzio, V., Reed, T. J., Fox, D. A. & Lundy, S. K. Human B Cell-Derived Lymphoblastoid Cell Lines Constitutively Produce Fas Ligand and Secrete MHCII(+)FasL(+) Killer Exosomes. Front. Immunol. 5, 144 (2014).
Dumontel, B. et al. Nanotechnological engineering of extracellular vesicles for the development of actively targeted hybrid nanodevices. Cell Biosci. 12, 61 (2022).
Hickey, J. W. et al. Adaptive Nanoparticle Platforms for High Throughput Expansion and Detection of Antigen-Specific T cells. Nano Lett. 20, 6289–6298 (2020).
Borst, J., Ahrends, T., Babala, N., Melief, C. J. M. & Kastenmuller, W. CD4(+) T cell help in cancer immunology and immunotherapy. Nat. Rev. Immunol. 18, 635–647 (2018).
Crotty, S. A brief history of T cell help to B cells. Nat. Rev. Immunol. 15, 185–189 (2015).
Lu, J. et al. CD4(+) T Cell-Released Extracellular Vesicles Potentiate the Efficacy of the HBsAg Vaccine by Enhancing B Cell Responses. Adv. Sci. 6, 1802219 (2019).
Notarbartolo, S. & Abrignani, S. Human T lymphocytes at tumor sites. Semin. Immunopathol. 44, 883–901 (2022).
Peters, P. J. et al. Cytotoxic T lymphocyte granules are secretory lysosomes, containing both perforin and granzymes. J. Exp. Med. 173, 1099–1109 (1991).
Seo, N. et al. Activated CD8(+) T cell extracellular vesicles prevent tumour progression by targeting of lesional mesenchymal cells. Nat. Commun. 9, 435 (2018).
Wu, S. W., Li, L., Wang, Y. & Xiao, Z. CTL-Derived Exosomes Enhance the Activation of CTLs Stimulated by Low-Affinity Peptides. Front. Immunol. 10, 1274 (2019).
Li, B. Q. et al. Engineered T cell extracellular vesicles displaying PD-1 boost anti-tumor immunity. Nano Today. 46, 101606 (2022).
Messmer, A. S. et al. CAR T-cell therapy and critical care : A survival guide for medical emergency teams. Wien. Klin. Wochenschr. 133, 1318–1325 (2021).
Yang, P. et al. The exosomes derived from CAR-T cell efficiently target mesothelin and reduce triple-negative breast cancer growth. Cell Immunol. 360, 104262 (2021).
Fu, W. Y. et al. CAR exosomes derived from effector CAR-T cells have potent antitumour effects and low toxicity. Nat. Commun. 10, 4355 (2019).
Escudier, B. et al. Vaccination of metastatic melanoma patients with autologous dendritic cell (DC) derived-exosomes: results of thefirst phase I clinical trial. J. Transl. Med. 3, 10 (2005).
Morse, M. A. et al. A phase I study of dexosome immunotherapy in patients with advanced non-small cell lung cancer. J. Transl. Med. 3, 9 (2005).
Yamashita, T., Takahashi, Y. & Takakura, Y. Possibility of Exosome-Based Therapeutics and Challenges in Production of Exosomes Eligible for Therapeutic Application. Biol. Pharm. Bull. 41, 835–842 (2018).
Syromiatnikova, V., Prokopeva, A. & Gomzikova, M. Methods of the Large-Scale Production of Extracellular Vesicles. Int. J. Mol. Sci. 23, 10522 (2022).
Lamparski, H. G. et al. Production and characterization of clinical grade exosomes derived from dendritic cells. J. Immunol. Methods 270, 211–226 (2002).
Colao, I. L., Corteling, R., Bracewell, D. & Wall, I. Manufacturing Exosomes: A Promising Therapeutic Platform. Trends Mol. Med. 24, 242–256 (2018).
Jeyaram, A. & Jay, S. M. Preservation and Storage Stability of Extracellular Vesicles for Therapeutic Applications. AAPS J. 20, 1 (2017).
Komuro, H., Aminova, S., Lauro, K. & Harada, M. Advances of engineered extracellular vesicles-based therapeutics strategy. Sci. Technol. Adv. Mater. 23, 655–681 (2022).
Jafari, D. et al. Designer Exosomes: A New Platform for Biotechnology Therapeutics. BioDrugs 34, 567–586 (2020).
Acknowledgements
This study was supported by the Bio & Medical Technology Development Program of the National Research Foundation (NRF) of Korea funded by the Korean government (MSIT) (2020M3A9I4039539), the National Research Foundation of Korea (NRF) grant funded by the Korean government (MSIT) (2021R1A5A2021614), and the DGIST Program of the Ministry of Science and ICT (21‐DGRIP‐01).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Jung, I., Shin, S., Baek, MC. et al. Modification of immune cell-derived exosomes for enhanced cancer immunotherapy: current advances and therapeutic applications. Exp Mol Med 56, 19–31 (2024). https://doi.org/10.1038/s12276-023-01132-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s12276-023-01132-8