Abstract
Anderson–Fabry disease (AFD) is an X-linked lysosomal storage disorder caused by abnormalities in the α-galactosidase (Gal) A gene (GLA; MIM:300644). The reduced activity of the lysosomal enzyme, α-galactosidase A (α-Gal A) leads to classic early manifestations and vascular disease of the heart, kidneys, and brain. As a high-risk screening for symptomatic AFD using an enzymatic assay on dried blood spot samples, we enrolled 2325 individuals (803 females and 1522 males; median age: 66 years) with cardiac, renal, or neurological manifestations that met at least one of the following criteria: (a) family history of early-onset cardiovascular diseases; (b) typical classic manifestations, such as acroparesthesias, clustered angiokeratoma, cornea verticillata, and hypo-anhidrosis; (c) proteinuria; (d) receiving dialysis; (e) left ventricular hypertrophy on electrocardiography or echocardiography; or (f) history of stroke. Ninety-two patients displayed low α-Gal A activity. Four males and two females had different pathogenic GLA mutations (0.26%) including a novel mutation c.908-928del21. Four males (0.17%) harbored the GLA c.196G>C (p.E66Q) variant. This simple screening protocol using dried blood spot samples is useful for early diagnosis of AFD in high-risk and underdiagnosed patients suffering from various cardiac, renal, or neurological manifestations.
Similar content being viewed by others
Introduction
Anderson–Fabry disease (AFD) is an X-linked lysosomal storage disorder caused by abnormalities in the α-galactosidase (Gal) A gene (GLA, MIM:300644). The reduced activity of the lysosomal enzyme, α-galactosidase A (α-Gal A) [1] leads to classic early manifestations that include acroparesthesias, clustered angiokeratoma, cornea verticillata, and hypo-anhidrosis, as well as vascular disease of the heart, kidneys, and brain [1].
The worldwide incidence of AFD is reportedly ranges from 1 in 40,000–117,000 [2]. This may be a significant underestimate given the under-recognition of symptoms and delayed or missed diagnosis [1].
Screening of high-risk populations displaying various cardiac, renal, or neurological manifestations could increase the diagnostic rate of AFD and facilitate therapeutic interventions that could prevent serious complications. Currently, screening for AFD involves measuring α-Gal A activity in peripheral blood leukocytes. However, the evaluation of dried blood spot (DBS) samples can permit easier and more efficient screening. We herein report our high-risk screening program of AFD and successful detection of six patients with AFD among 2325 patients with various cardiac, renal, or neurological manifestations.
Materials and methods
Experimental design
Forty-five hospitals in Hokkaido prefecture, Japan, participated in this prospective study. From July 2012 to December 2017, we analyzed DBS samples obtained from 2325 patients with various cardiac, renal, or neurological manifestations. Patients were included if they met at least one of the following criteria: (a) family history of early-onset cardiovascular diseases (to identify patients with early and asymptomatic, especially for asymptomatic heterozygote); (b) typical classic manifestations, such as acroparesthesias, clustered angiokeratoma, cornea verticillata, and hypo-anhidrosis; (c) proteinuria; (d) receiving dialysis; (e) left ventricular hypertrophy (LVH) on electrocardiography or echocardiography; or (f) a history of stroke. Patients who did not agree to undergo measurement of α-Gal A activity and genetic analysis were excluded. The standard nomenclature for representing pedigrees was used [3].
Preparation of DBS samples
All the DBS samples were prepared from peripheral blood as previously reported [4]. Blood droplets were spotted onto filter paper (Toyo Roshi Kaisha Ltd., Tokyo, Japan), allowed to dry for ~4 h at room temperature, and sent through the mail within 1 week of preparation to Kumamoto University for analysis. The DBS samples were stored at −20 °C until use.
Measurement of α-Gal A activity and DNA analysis of GLA
We measured the α-Gal A activity of 2325 patients using a DBS test with a slight modification of a method described previously [5, 6]. α-Gal A activity <20 Agal U in females and <12 Agal U in males was identified as abnormally low. Patients with α-Gal A activity <20 Agal U in females or <12 Agal U in males had blood drawn again for the re-measurement of the α-Gal A activity on another day. Patients with low α-Gal A activity after re-measurement were assessed clinically, and they underwent a genetic analysis of GLA after genetic counseling by clinical geneticist certified by the Japanese board of medical genetics and genomics, clinical genetics. For DNA analysis, total genomic DNA was extracted from the leukocytes of the patients. All seven exons and the flanking intronic sequences of GLA were amplified by PCR, and the amplification products were analyzed by direct sequencing. All patients were screened for the GLA c.196G>C (p.E66Q) variant (rs104894833) as described previously [6].
Protocol approvals and patient consent
This study was approved by the Ethical Committee of Asahikawa Medical University (no. 735) and the ethics committees of each of the participating hospitals. Written informed consent was obtained from each patient prior to enrollment.
Results
Characteristics of patients
We enrolled 2325 individuals (803 females and 1522 males; median age, 66.0 years). Table 1 summarizes their demographic characteristics. The patient group included 1476 patients (63%) undergoing hemodialysis. Of the 2325 patients, 601 (26%) had LVH, 374 (16%) had proteinuria, 259 (11%) had prior stroke, 417 (18%) had any typical classic manifestations that included acroparesthesias, clustered angiokeratoma, cornea verticillata, or hypo-anhidrosis, and 304 (13%) had a family history of early-onset cardiovascular diseases.
α-Gal A assay of DBS samples and molecular analysis of GLA
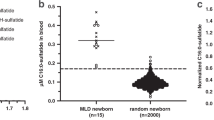
The mean (SD) blood α-Gal A activities of the females and males were 24.2 (12.4) and 24.5 (10.5) Agal U, respectively. α-Gal A activity values <20 Agal U in females and <12 Agal U in males were observed for 410 (333 females and 77 males) of the 2325 patients (Fig. 1). Thus, we repeated the α-Gal A assay using DBS samples obtained for a second time from these 410 patients. In the second determination, α-Gal A activity values <20 Agal U in females and <12 Agal U in males were observed for 92 (80 females and 12 males) of the 410 patients. Samples from these 92 patients were analyzed for mutations in GLA. Four men and two women displayed a different pathogenic mutation (0.26%; Fig. 2). The four male patients had the GLA c.196G>C (p.E66Q) variant (0.17%), which is not associated with the full clinical manifestations of AFD.
a Flow chart for screening patients with AFD. Two female and four male patients had a different pathogenic mutation. Further, four male patients had the GLA c.196G>C (p.E66Q) variant (0.17%), which is not associated with the full clinical manifestations of AFD. b, c Distribution of α-galactosidase A activity determined using DBS samples in female a and male b patients in the study. The mean (SD) α-Gal A activities of the female and male study populations were 24.2 (12.4) and 24.5 (10.5) Agal U, respectively. α-Gal A activity values <20 Agal U in females and <12 Agal U in males were observed for 410 (333 females and 77 males) out of 2325 patients
Family pedigrees and representative findings of the patients with AFD in this study. a, b, c, h, i, j Family pedigrees of patient 1 (a), patient 2 (b), patient 3 (c), patient 4 (h), patient 5 (i) and patient 6 (j). Males are denoted by squares, females by circles. Filled symbols indicate those with AFD. Open circles with vertical black lines indicate asymptomatic hemizygote patients with AFD. Open symbols indicate normal patients. Symbols with a question mark indicate family members who may carry the pathogenic mutation of AFD. The dashes indicate deceased patients. d–f Chest X-ray (d), electrocardiography (e) and cardiovascular magnetic resonance (f) of patient 2 showed LVH with complete right bundle branch block (e) and with late gadolinium enhancement in the basal posterolateral wall (f). g Pathologic findings from light microscopy of patient 3; all glomeruli show marked swelling of podocyte with expanded foamy or vacuolar cytoplasmic change (periodic acid-methenamine-silver stain, ×400). GT genetic testing
When a subset of patients undergoing hemodialysis was analyzed separately, α-Gal A activity values <20 Agal U in females and <12 Agal U in males were observed for 52 (46 females and six males) of 1476 (503 females and 973 males) patients. Finally, two male patients (patient 4 and 6 in Table 2) had a pathogenic mutation (0.14%) among the 1476 patients undergoing hemodialysis. As for the subset of patients with LVH and stroke, five (patient 1, 2, 4, 5, and 6 in Table 2) of 601 patients with LVH (0.8%) and two (patient 1 and 3 in Table 2) of 259 patients with prior stroke (0.8%) had a pathogenic mutation.
Clinical characteristics of patients with pathogenic GLA mutation
The clinical characteristics of the six patients with a pathogenic GLA mutation (patients 1–6) and the four patients with a nonpathogenic c.196G>C (p.E66Q) variant (patients 7–10) are summarized in Table 2.
Patient 1 was a 42-year-old female with aseptic meningitis, ischemic stroke, LVH, and schizoaffective psychosis, as reported previously [7]. α-GAL activity determined using DBS samples was low (11.9 Agal U) and genetic analysis revealed the presence of a heterozygous mutation in intron 4 of GLA c.IVS4-1G>A, which has been reported previously [8]. Genetic analyses of the patient’s parents and daughter did not detect this mutation. Therefore, the patient was diagnosed with de novo AFD (Fig. 2a).
Patient 2 was a 36-year-old male with LVH detected by a health check-up (Fig. 2b, d and e). Cardiovascular magnetic resonance imaging revealed concentric LVH with late gadolinium enhancement in the basal posterolateral wall (Fig. 2f). He also suffered from coronary spastic angina, acroparesthesias, clustered angiokeratoma, hypo-anhidrosis, and gastrointestinal disorders. α-GAL activity was markedly low (2.8 Agal U) and genetic analysis revealed the presence of a hemizygous nonsense mutation in exon 5 of GLA c.707G>A (p.W236X), which has been reported previously [9]. His mother had a heterozygous mutation and LVH with coronary spastic angina (Fig. 2b).
Patient 3 was a 37-year-old female with nephrotic range proteinuria (4.0 g/gCr) and juvenile minor ischemic stroke. Her renal function and serum albumin were preserved with a serum creatinine of 0.70 mg/dL and serum albumin of 4.0 g/dL. She had a kidney biopsy, which demonstrated podocyte vacuolization on light microscopy sections with podocyte inclusions on semi-thin sections (Fig. 2g). α-GAL activity was low (9.0 Agal U) and genetic analysis revealed the presence of a hemizygous deletion mutation in exon 7 of GLA c.1072_1074del (p.358delE), which have been reported previously [10]. Genetic analyses of the patient’s parents did not detect this mutation. However, she had two boys with acroparesthesias and this hemizygous GLA mutation (Fig. 2c).
Patient 4 was a 64-year-old male who underwent hemodialysis for 20 years after being diagnosed with glomerulonephritis without kidney biopsy. He also had hypo-anhidrosis and LVH. α-GAL activity was markedly low (1.9 Agal U) and genetic analysis revealed the presence of a hemizygous missense mutation in exon 4 of GLA c.559A>G (p.M187V), which has been reported previously [11]. His mother died due to heart failure at 83 years of age and his maternal aunt underwent hemodialysis and died at 82 years of age, although they had undiagnosed AFD (Fig. 2h).
Patient 5 was a 56-year-old male with nephrotic range proteinuria (3.8 g/g Cr), renal dysfunction with a serum creatinine of 2.0 mg/dL and mild LVH. α-GAL activity was markedly low (2.8 Agal U) and genetic analysis revealed the presence of a hemizygous missense mutation in exon 7 of GLA c.1124G>A (p.G375E), which has been reported previously [12]. His mother had undiagnosed AFD, underwent hemodialysis, and died due to colon cancer at 76 years of age (Fig. 2i). He had two daughters who in theory must be heterozygous (Fig. 2i). Therefore, they will be analyzed for mutations in GLA.
Patient 6 was a 55-year-old male patient who underwent hemodialysis for 4 years after being diagnosed with glomerulonephritis without kidney biopsy. He had also acroparesthesias, hypo-anhidrosis, and LVH. α-GAL activity was markedly low (3.7 Agal U) and genetic analysis revealed the presence of a hemizygous deletion mutation in exon 7 of GLA c.908-928del21, which is a novel mutation not described before in the literature. His mother had undiagnosed AFD, but died due to heart failure at 82 years of age (Fig. 2j).
Among these patients with AFD, patients 2, 3, and 4 had resting angina and were diagnosed with coronary spastic angina by acetylcholine-loaded coronary spasm provocation tests as reported most recently [13]. All six patients with AFD had been regularly treated using enzyme replacement therapy (ERT), whereas the four patients with the GLA c.196G>C (p.E66Q) variant had not begun ERT.
Discussion
In this study, we confirmed the diagnosis of AFD in four men and two women who had different pathogenic GLA mutations (0.26%) including a novel mutation c.908-928del21, and four men who had the GLA c.196G>C (p.E66Q) variant (0.17%) among 2325 patients who suffered from various cardiac, renal, or neurological manifestations. This simple screening protocol using DBS samples is useful for the early diagnosis of AFD in high-risk and underdiagnosed patients suffering from these manifestations.
The prevalence in selected patient cohorts was previously reported to be between 0.25% and 3.5% in male patients undergoing hemodialysis [14,15,16,17], 0.9–3.9% in male patients with hypertrophic cardiomyopathy [17,18,19,20], and 0.13–5% in patients with cryptogenic stroke [17, 21]. In the present study, the prevalence of AFD was 0.26% for the 2325 patients who suffered from various cardiac, renal, or neurological manifestations; 0.14% for the 1476 hemodialysis patients; and 0.8% for the 601 patients with LVH and 259 patients with prior stroke. These rates were similar to previously reported prevalence rates even though our screening included females. In general, many females who are heterozygous for pathogenic GLA mutations have normal plasma α-Gal A activity. Thus, screening studies for AFD have predominantly focused on male patients. We presently confirmed the diagnosis of AFD in two women with stroke and LVH or proteinuria, suggesting that the inclusion of female patients with multiple cardiac, renal, or neurological manifestations might be taken into consideration in screening studies for AFD.
In the present study, roughly 40% of the enrolled female patients required re-measurement of α-GAL A activity because of measured values <20 Agal U. The rate of low α-GAL A activity was reduced to 10% upon repeat testing. This discrepancy in the measured enzyme activity might have been caused by inappropriate preparation and storage of DBS. Exposure of DBS to elevated heat and humidity can rapidly degrade enzyme functions [22]. Therefore, proper and consistent DBS preparation and storage are very important when screening for deficiencies of lysosomal enzymes.
Cardiac symptoms including LVH, arrhythmia, angina, and dyspnea have been reported in ~40–60% of patients with AFD [23, 24]. Furthermore, most recently, we reported that a high prevalence of coronary spastic angina was complicated with AFD in eight of the nine patients with AFD including three cases in the present study [13]. Coronary spasms and multivessel coronary spasms have been reported to be more prevalent in Japanese people than in Westerners [25], suggesting that AFD might be an underlying cause of coronary spastic angina in Japanese patients.
Two classes of GLA mutations are recognized according to their pathogenicity [26]. Class 1 mutations, also termed pathogenic mutations, have a high probability of causing disease. Class 2 mutations are nonpathogenic polymorphisms and include five missense changes (p.E66Q, p.S102L, p.S126G, p.D313Y, p.F396Y) [27]. In the nonpathogenic polymorphisms, the c.196G>C (p.E66Q) variant has been frequently observed in previous screening studies of Japanese hemodialysis [14, 16, 28, 29] and stroke patietnt [6, 30]. Therefore, the four patients (two patients with prior stroke, one with LVH, and one undergoing hemodialysis) (Table 2) in this study with the GLA c.196G>C (p.E66Q) variant had not begun ERT. However, recent reports demonstrated that the GLA c.196G>C (p.E66Q) variant is a genetic risk factor for cerebral small-vessel occlusion in elderly Japanese males [30] and non-cardioembolism in Japanese males, but not in females [6]. Thus, further epidemiological studies and biochemical and pathological examinations are necessary to elucidate the precise pathological mechanism by which the GLA c.196G>C (p.E66Q) variant increases the risk of stroke.
Currently, ERT is available for the treatment that is necessary to prevent the irreversible organ damage that occurs in AFD, as well as in other lysosomal storage disorders, which include Gaucher disease, Pompe disease, and mucopolysaccharidosis. Furthermore, most recently an oral pharmacological chaperone migalastat for the treatment of AFD has become available for specific mutant (amenable) forms of GLA [31]. Therefore, it is important to identify patients with AFD and to perform pedigree analysis as soon as possible so that ERT or pharmacological chaperone therapy can be initiated in patients with AFD before irreversible organ damage and complications occur.
This study has several limitations. First, female patients with AFD might have been missed, as female patients could have normal α-Gal A activity. Therefore, plasma globotriaosylsphingosine (lyso-Gb3) [16] in addition to α-Gal A activity should be analyzed when screening female patients for AFD in future studies. Second, some mutation such as intronic mutation and large deletion might have been missed by sequencing only exon and exon/intron boundaries of GLA gene. Therefore, we are now carefully following patients with low enzyme activity, without mutation in exon and exon/intron boundaries. Third, there was a relatively small sample size. Further large-scale epidemiological studies are necessary to elucidate the prevalence of AFD among patients with various cardiac, renal, or neurological manifestations.
In conclusion, the high-risk screening system for AFD using DBS samples appears to be an effective method for identifying the specific disorder in individuals with cardiac, renal, or neurological manifestations caused by unidentified reasons. This simple diagnostic test is useful for specialists and general physicians to screen patients with various cardiac, renal, or neurological symptoms to identify patients with AFD.
References
Zarate YA, Hopkin RJ. Fabry’s disease. Lancet. 2008;372:1427–35.
Mehta A, Ricci R, Widmer U, Dehout F, Garcia de Lorenzo A, Kampmann C, et al. Fabry disease defined: baseline clinical manifestations of 366 patients in the Fabry Outcome Survey. Eur J Clin Invest. 2004;34:236–42.
Bennett RL, French KS, Resta RG, Doyle DL. Standardized human pedigree nomenclature: update and assessment of the recommendations of the National Society of Genetic Counselors. J Genet Couns. 2008;17:424–33.
Momosaki K, Kido J, Matsumoto S, Yoshida S, Takei A, Miyabayashi T, et al. High-risk screening for Gaucher disease in patients with neurological symptoms. J Hum Genet. 2018;63:717–21.
Inoue T, Hattori K, Ihara K, Ishii A, Nakamura K, Hirose S. Newborn screening for Fabry disease in Japan: prevalence and genotypes of Fabry disease in a pilot study. J Hum Genet. 2013;58:548–52.
Nagamatsu K, Sekijima Y, Nakamura K, Hattori K, Ota M, Shimizu Y, et al. Prevalence of Fabry disease and GLA c.196G>C variant in Japanese stroke patients. J Hum Genet. 2017;62:665–70.
Sawada J, Katayama T, Kano K, Asanome A, Takahashi K, Saito T, et al. A sporadic case of Fabry disease involving repeated fever, psychiatric symptoms, headache, and ischemic stroke in an adult Japanese woman. Intern Med. 2015;54:3069–74.
Shabbeer J, Yasuda M, Benson SD, Desnick RJ. Fabry disease: identification of 50 novel alpha-galactosidase A mutations causing the classic phenotype and three-dimensional structural analysis of 29 missense mutations. Hum Genom. 2006;2:297–309.
Germain DP, Shabbeer J, Cotigny S, Desnick RJ. Fabry disease: twenty novel alpha-galactosidase A mutations and genotype-phenotype correlations in classical and variant phenotypes. Mol Med. 2002;8:306–12.
Shabbeer J, Yasuda M, Luca E, Desnick RJ. Fabry disease: 45 novel mutations in the alpha-galactosidase A gene causing the classical phenotype. Mol Genet Metab. 2002;76:23–30.
Ashton-Prolla P, Tong B, Shabbeer J, Astrin KH, Eng CM, Desnick RJ. Fabry disease: twenty-two novel mutations in the alpha-galactosidase A gene and genotype/phenotype correlations in severely and mildly affected hemizygotes and heterozygotes. J Investig Med. 2000;48:227–35.
Lukas J, Scalia S, Eichler S, Pockrandt AM, Dehn N, Cozma C, et al. Functional and clinical consequences of novel alpha-galactosidase A mutations in Fabry disease. Hum Mutat. 2016;37:43–51.
Kitani Y, Nakagawa N, Sakamoto N, Takeuchi T, Takahashi F, Momosaki K, et al. Unexpectedly high prevalence of coronary spastic angina in patients with Anderson–Fabry disease. Circ J. 2019;83:481–4.
Nakao S, Kodama C, Takenaka T, Tanaka A, Yasumoto Y, Yoshida A, et al. Fabry disease: detection of undiagnosed hemodialysis patients and identification of a “renal variant” phenotype. Kidney Int. 2003;64:801–7.
Kotanko P, Kramar R, Devrnja D, Paschke E, Voigtlander T, Auinger M, et al. Results of a nationwide screening for Anderson–Fabry disease among dialysis patients. J Am Soc Nephrol. 2004;15:1323–9.
Maruyama H, Takata T, Tsubata Y, Tazawa R, Goto K, Tohyama J, et al. Screening of male dialysis patients for fabry disease by plasma globotriaosylsphingosine. Clin J Am Soc Nephrol. 2013;8:629–36.
Doheny D, Srinivasan R, Pagant S, Chen B, Yasuda M, Desnick RJ. Fabry disease: prevalence of affected males and heterozygotes with pathogenic GLA mutations identified by screening renal, cardiac and stroke clinics, 1995–2017. J Med Genet. 2018;55:261–8.
Nakao S, Takenaka T, Maeda M, Kodama C, Tanaka A, Tahara M, et al. An atypical variant of Fabry’s disease in men with left ventricular hypertrophy. N Engl J Med. 1995;333:288–93.
Linhart A, Elliott PM. The heart in Anderson–Fabry disease and other lysosomal storage disorders. Heart. 2007;93:528–35.
Elliott P, Baker R, Pasquale F, Quarta G, Ebrahim H, Mehta AB, et al. Prevalence of Anderson–Fabry disease in patients with hypertrophic cardiomyopathy: the European Anderson–Fabry Disease survey. Heart. 2011;97:1957–60.
Shi Q, Chen J, Pongmoragot J, Lanthier S, Saposnik G. Prevalence of Fabry disease in stroke patients—a systematic review and meta-analysis. J Stroke Cereb Dis. 2014;23:985–92.
Elbin CS, Olivova P, Marashio CA, Cooper SK, Cullen E, Keutzer JM, et al. The effect of preparation, storage and shipping of dried blood spots on the activity of five lysosomal enzymes. Clin Chim Acta. 2011;412:1207–12.
Nakagawa N, Maruyama H, Ishihara T, Seino U, Kawabe J, Takahashi F, et al. Clinical and genetic investigation of a Japanese family with cardiac fabry disease. Identification of a novel alpha-galactosidase A missense mutation (G195V). Int Heart J. 2011;52:308–11.
Kampmann C, Baehner F, Whybra C, Martin C, Wiethoff CM, Ries M, et al. Cardiac manifestations of Anderson–Fabry disease in heterozygous females. J Am Coll Cardiol. 2002;40:1668–74.
Shimokawa H, Nagasawa K, Irie T, Egashira S, Egashira K, Sagara T, et al. Clinical characteristics and long-term prognosis of patients with variant angina. A comparative study between western and Japanese populations. Int J Cardiol. 1988;18:331–49.
Gal A, Hughes DA, Winchester B. Toward a consensus in the laboratory diagnostics of Fabry disease—recommendations of a European expert group. J Inherit Metab Dis. 2011;34:509–14.
Ortiz A, Germain DP, Desnick RJ, Politei J, Mauer M, Burlina A, et al. Fabry disease revisited: management and treatment recommendations for adult patients. Mol Genet Metab. 2018;123:416–27.
Fujii H, Kono K, Goto S, Onishi T, Kawai H, Hirata K, et al. Prevalence and cardiovascular features of Japanese hemodialysis patients with Fabry disease. Am J Nephrol. 2009;30:527–35.
Saito O, Kusano E, Akimoto T, Asano Y, Kitagawa T, Suzuki K, et al. Prevalence of Fabry disease in dialysis patients: Japan Fabry disease screening study (J-FAST). Clin Exp Nephrol. 2016;20:284–93.
Nakamura K, Sekijima Y, Hattori K, Nagamatsu K, Shimizu Y, Yazaki M, et al. Mutation in the GLA gene is associated with a high risk of cerebral small-vessel occlusion in elderly Japanese males. Eur J Neurol. 2014;21:E66Q.
Germain DP, Hughes DA, Nicholls K, Bichet DG, Giugliani R, Wilcox WR, et al. Treatment of Fabry’s disease with the pharmacologic chaperone migalastat. N Engl J Med. 2016;375:545–55.
Acknowledgements
We thank Professor Yoshio Makita of Asahikawa Medical University for the genetic counseling and Kaori Kanno of Asahikawa Medical University, Fumiko Nozaki, Naomi Yano, and Matsumi Harada of Kumamoto University for their excellent technical assistance. In addition to the authors, the following investigators and institutions participated in this study: H.N. Medic Sapporo-Higashi (Masataka Tsunoda); H.N. Medic Sapporo (Nobuo Hashimoto); H.N. Medic Kitahiroshima (Ryota Ikee); Kitasaito Hospital (Atsushi Wada, Tomoya Hirayama); Nagayama Kidney and Urology Clinic (Mitsuhiro Mizunaga); Jinyukai Hospital (Kazuyuki Maeno); Tomakomai Nissho Hospital (Kazuya Sakamoto); Hokkaido Kitami Hospital (Kazumi Uekita); Hokkaido Haboro Hospital (Tomoya Koizumi, Wataru Sasao); Abashiri Kosei Hospital (Toshihiro Hirai, Hideki Nakamura); Teine Keijinkai Hospital (Takuto Maeda, Hideki Takizawa); Teine Inazumi Hospital (Susumu Saito); Engaru Kosei Hospital (Kanako Matsuda, Motoi Kijima); Uno Clinic (Motohiro Uno); Kushiro City General Hospital (Ken Morita); Kushiro Red Cross Hospital (Junya Yamamoto); NTT East Sapporo Hospital (Tomochika Maoka); KKR Sapporo Medical Center (Hirofumi Kon); Ebetsu City Hospital (Masahiko Abe); Municipal Ashibetsu Hospital (Yasuhiro Nakamura); Hokkaido Cardiovascular Hospital (Yusuke Kashiwagi); Sawamura Dialysis Clinic (Naruhiko Tanaka); National Hospital Organization Hokkaido Medical Center (Takashi Takenaka); National Hospital Organization Obihiro Hospital (Mayumi Aoki, Hiromi Obata); Hakodate Watanabe Hospital (Hisanobu Ota); Asahikawa Kosei Hospital (Atsushi Yamauchi); National Hospital Organization Asahikawa Medical Center (Yoko Aburakawa); Nayoro City General Hospital (Sarasa Toyoshima); Sapporo Rouaikai Hospital (Hidenori Furui); Nissei Hospital (Hiromitsu Yoshie); Hokusei Hospital (Eriko Yamagishi); Iwamizawa Municipal General Hospital (Yoshiaki Aizawa); Megumino Hospital (Yasutaka Hirayama); Ohkawara Neurosurgical Hospital (Noriaki Shojima); Iburi Urological Clinic (Masashi Bandou, Yutaka Takeuchi); Hakodate Goryoukaku Hospital (Fumio Obara); Hakodate Municipal Hospital (Misuzu Osaka); Kitamihara clinic (Sugako Akihama); Chitose City Hospital (Tomoko Sakai); and Ido Medical Clinic (Akira Ido).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Nakagawa, N., Sawada, J., Sakamoto, N. et al. High-risk screening for Anderson–Fabry disease in patients with cardiac, renal, or neurological manifestations. J Hum Genet 64, 891–898 (2019). https://doi.org/10.1038/s10038-019-0633-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s10038-019-0633-1