Abstract
We ascertained two unrelated consanguineous families with two affected children each having microcephaly, refractory seizures, intellectual disability, and spastic quadriparesis. Magnetic resonance imaging showed atrophy of cerebrum, cerebellum and spinal cord, prominent cisterna magna, symmetric T2 hypo-intensities in the bilateral basal ganglia and thinning of corpus callosum. Whole-exome sequencing of three affected individuals revealed c.105C>A [p.(Tyr35Ter)] variant in AIMP2. The variant lies in a common homozygous region of 940 kb on chromosome 7 and is likely to have been inherited from a common ancestor. The phenotype noted in our subjects’ shares marked similarity with that of hypomyelinating leukodystrophy-3 caused by mutations in closely related gene AIMP1. We hereby report the first human disease associated with deleterious mutations in AIMP2.
Similar content being viewed by others
Introduction
Aminoacyl-tRNA synthetases (ARSs) are housekeeping enzymes needed for translation of genetic information into functional proteins. Mammalian multi-tRNA synthetase complex (MSC) is a specialized macromolecular multienzyme complex of nine ARSs and three auxiliary proteins AIMP1/p43, AIMP2/p38, and AIMP3/p18 of apparent molecular masses of 43, 38, and 18 kD respectively [1]. MSC has been found to play role in various signaling pathways other than its role in protein synthesis [2]. Various ARS are now known to cause encephalopathies, peripheral neuropathies, and other sensorineural disorders. Among them, mutations in 10 cytosolic ARSs are associated with Charcot–Marie–Tooth and related neuropathies, and 14 mitochondrial ARSs are associated with severe leukoencephalopathies. In human and other mammalian cells, a unique large multi-tRNA synthetase complex organizes nine cytoplasmic ARSs consisting of bifunctional, as well as the monospecific tRNA synthetases and three non-enzyme factors, namely p43 (AIMP1), p38 (AIMP2), and p18 (AIMP3). The p38 protein is a key component of the multi-ARS complex and is crucial for the assembly of the complex. With the advent of exome sequencing, several neurological disorders have been recognized with defects in these enzymes and their associated proteins [3].
We herein describe four subjects from two unrelated consanguineous families of Indian origin with progressive neurological disorder characterized by lack of development, absent speech, microcephaly, spasticity, seizures, and contractures. Magnetic resonance imaging (MRI) of the brain showed atrophy of cerebral cortex, spinal cord, and cerebellum with basal ganglia hypo-intensities in all subjects. Whole-exome sequencing revealed a variant, c.105C>A [p.(Tyr35Ter)] in homozygous state in exon 1 (NM_006303.3) of AIMP2 in both the families.
Materials and Methods
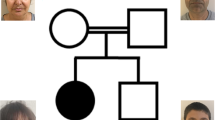
Family 1
The proband P1, born to consanguineous parents presented at 7 years of age with global developmental delay, microcephaly, seizures, and spasticity. She was born at term by normal vaginal delivery after an uncomplicated pregnancy and weighed 3.6 kg (normal) at birth. There were no perinatal complications. She was non-ambulatory and had not achieved any developmental milestones. She had repeated respiratory infections, multifocal seizures, and feeding difficulty from neonatal period. Seizures were controlled by multiple antiepileptic medications by about age 4 years. A similarly affected male sib succumbed at 6 months of age to intractable seizures and dehydration following an episode of acute gastroenteritis. The couple had a stillbirth, a spontaneous abortion, and three medically induced termination of pregnancies (Fig. 1A).
A Pedigree of family 1. B Sanger validation of the AIMP2 variant in family 1. The pathogenic variation c.105C>A of AIMP2 is found in homozygous state in proband and is heterozygous in her parents. C Proband (P1) at 7 years of age shows microcephaly, kyphoscoliosis, and contractures at wrist joints. D T2-weighted magnetic resonance imaging of brain on postnatal day 10 revealed significant cerebral atrophy, cerebellar atrophy, prominent cisterna magna, hypo-intensities in the bilateral basal ganglia (arrows in D(i)) on T2-weighted sequences, spinal cord atrophy, and thinning of corpus callosum (arrow in D(iii))
At the time of examination, her head circumference was 40 cm (−10 SD) and length was 103 cm (−10 SD), measurement limited by contractures). She had thick vermilion of lips, low hanging columella, and gum hypertrophy. Severe contractures of wrists and ankles and kyphoscoliosis were noted. Central nervous system examination revealed spastic quadriparesis with exaggerated deep tendon reflexes and extensor plantar responses (Fig. 1C). Rest of the systemic examination was unremarkable.
MRI of brain on postnatal day 10 revealed cerebral atrophy, cerebellar atrophy, prominent cisterna magna, hypo-intensities in the bilateral basal ganglia, spinal cord atrophy, and thinning of corpus callosum (Fig. 1D). Electroencephalogram (EEG) revealed multifocal spike wave epileptiform activity. Karyotype showed normal female constitution (46, XX).
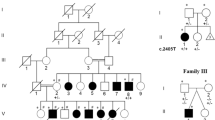
Family 2
The patient P2 was first born female child to a third-degree consanguineous couple (Fig. 2A) with a birth weight of 2.5 kg (−1 SD). She had delayed cry at birth and developed tonic spasms followed by multifocal seizures in the first week of life requiring multiple antiepileptic medications. Subsequently, there was global developmental delay, failure to thrive, microcephaly, and spasticity. She never gained any milestones and was non-ambulatory. She had a moderate gastroesophageal reflux disease and required anti-reflux medications. At the age of 7 years, she developed septicemia and lower respiratory infection and succumbed. Her hearing and fundus examination were normal. Metabolic work-up (tandem mass spectrometry of blood and gas chromatography mass spectrometry of urine) was unremarkable. Her initial EEG revealed hypsarrhythmia. MRI of brain at age 2 years showed generalized cerebral atrophy with paucity of white matter and bilateral symmetrical areas of altered signal intensities in periventricular white matter suggestive of demyelination. However, these images were not available for re-evaluation.
A Pedigree of family 2. B Sanger validation of the AIMP2 variant in family 2. The variation c.105C>A of AIMP2 is found in homozygous state in probands and is heterozygous in their parents. C P3 at age 6 years shows microcephaly, contractures at knees and ankles, and kyphoscoliosis. D T2-weighted magnetic resonance imaging of brain done at 4 years of age shows cerebral atrophy, cerebellar atrophy, hypo-intensities in the bilateral basal ganglia on T2-weighted sequences (arrows in D(i)), prominent cisterna magna, and thinning of corpus callosum (D(ii)) and spinal cord
P3 is the younger sib of P2. He was born by normal delivery and required bag and mask ventilation at birth. The APGAR score at 1, 5, and 10 min was 5, 7, and 9, respectively. He developed symptomatic hypoglycemia at 15 h of life and received appropriate management. On day 5 of life, he developed generalized tonic-clonic convulsions. Subsequently, the seizure pattern changed to myoclonic seizures. Global developmental delay was noted and no milestones were achieved. There were recurrent episodes of pneumonia and prolonged mechanical ventilation followed by tracheostomy at the age of 5 years. Currently, he is non-ambulatory and is on nasogastric feeds (Fig. 2C). Seizures are persistent with 1–2 episodes of myoclonic seizures daily despite multiple antiepileptic drugs.
At age 6 years and 7 months he weighed 12 kg (−4.1 SD), length was 97 cm (−4.3 SD), and head circumference of 38.5 cm (−10 SD). He had widely spaced teeth, anteverted nostrils, prognathism, hyper-convex nails, and generalized hirsutism. He has generalized spasticity, dynamic contractures at heels and knees, and kyphoscoliosis. His arterial pH, lactate, and blood ammonia were normal. EEG revealed hypsarrhythmia. He has normal hearing, but visual evoked responses showed extinguished response. Brain imaging at age 4 years showed significant cerebral and cerebellar atrophy, hypo-intensities in the bilateral basal ganglia, prominent cisterna magna, and thinning of corpus callosum and spinal cord (Fig. 2D). Clinical features of the affected individuals from both families are summarized in Table 1.
We collected blood samples from all affected siblings and both parents after informed consent. This study was approved by the Institutional Ethics Committees of respective institutes.
Whole-exome sequencing
Whole-exome sequencing was carried out on peripheral leukocyte DNA of the affected individuals from both families to ascertain coding sequence variants. Exome capture was performed on genomic DNA sample from the P1 and P3 using Nextera Rapid Capture Exome Kit V1.2 (Illumina, USA) following manufacturer’s protocol. For P2 Agilent SureSelectXT V5 Exome Capture Kit (Agilent, USA) was used. The libraries were sequenced to mean >100× coverage on Illumina NextSeq Platform (Illumina, San Diego, California, USA) (Supplementary Table S1). The raw data of the two affected siblings was analyzed on Red Hat Enterprise Linux 7 using an automated pipeline, SeqMule v1.2.5 [4]. The resulting variant call format (.vcf) file was annotated using ANNOVAR [5]. The variant filtering strategy is outlined in Supplementary Table S2. PCR was performed using specific primers F-5′-CCCTTTTGCTTTGGTTCTGC-3′ and R-5′-GTCTGAGTGAGTCCCTGGC-3′ and Sanger sequencing was done using ABI 3130 Genetic analyzer (Life Technologies, Carlsbad, CA, USA) following the manufacturer’s protocol in control, parents, and patient samples to validate the variant [6].
Homozygosity mapping
Homozygosity mapping was carried out from the VCF files of the proband from family 1 and siblings from family 2 using the AutEx algorithm in FILTUS (Oslo University Hospital and University of Oslo, Oslo, Norway) [7] with no segment size threshold [8].
RNA extraction and reverse transcription quantitative PCR
RNA extraction and reverse transcription quantitative PCR (RT-qPCR) experiments were performed as described earlier [9]. RT-qPCR was performed using complimentary DNA (cDNA) specific primers F-5′-CCCTTTTGCTTTGGTTCTGC-3′ and R-5′-AGAGCTTGCAGAGACAGGTT-3′ for AIMP2. Two group t-test was performed using GraphPad Prism version 7 to compare the RT-qPCR data.
Results
We ascertained two consanguineous families with four affected children with severe microcephaly, seizures, lack of development, spastic quadriparesis, and contractures. The symptoms began early in neonatal period. Exome sequencing in the patients followed by variant filtering (Supplementary Table S2) revealed a variant in AIMP2 (NM_006303.3:c.105C>A [p.(Tyr35Ter)]) as the only common likely pathogenic variant between the two families. The variant was not present in a homozygous state in 1000 Genomes project, the Exome Variant Server, ExAC browser, and in our in-house exome data of unrelated individuals from the local population. However, it was present in the heterozygous state in 1/15404 East Asian individuals (allele frequency 0.00006492) with overall frequency of in 1/227,386 (allele frequency 0.000004398) in gnomAD database. The CADD score for the variant is 34 [10]. Thus this nonsense variant, NM_006303.3:c.105C>A [p.(Tyr35Ter)] in exon 1 of AIMP2 gene was likely to be associated with the condition in the patients (ClinVar submission ID: SUB2744031). The variant was validated by Sanger sequencing in the probands and parents in both families (Figs. 1B, 2B). Parents were found to be heterozygous carriers of the variant confirming the autosomal recessive segregation in the family. The siblings (P2, P3) had 37 common regions of homozygosity (ROH) and P1 from family 1 was found to have 51 ROH on homozygosity mapping using FILTUS software. The variant in AIMP2 was located in a common shared ROH of 940 kb observed in chromosome 7 (Supplementary Table S3).The common variants shared by the three patients on whole-exome sequencing are provided in Supplementary Table S4. Thus the variant present in a shared homozygous region is likely to be due to a founder effect. On RT-qPCR, AIMP2 messenger RNA (mRNA) level was found to be reduced in the patients as compared to controls although the difference was not statistically significant (P-values for P1 and P3 were 0.1694 and 0.1240, respectively). This suggests low level of nonsense mediated decay of AIMP2 mRNA in peripheral leukocytes (Fig. 3).
Reverse transcription quantitative PCR (RT-qPCR) analysis showing the expression of AIMP2 mRNA (±SD) in the probands (P1 and P3) and two unrelated controls (C1 and C2). Comparative ∆∆Ct method was used to calculate gene expression, and HERC1 was used as reference gene. The graph was plotted using GraphPad Prism version 7 (Trial license, http://www.graphpad.com/)
Discussion
We report on three children sharing a common phenotype of an early onset severe neurodevelopmental disorder with microcephaly, seizures, and spasticity. All of them shared a common homozygous deleterious variant in AIMP2 possibly due to a founder effect.
ARSs are ubiquitous family of housekeeping enzymes, which carry out specific attachment of an amino acid to its cognate tRNA that ensures translation of the genetic information into functional proteins [11]. ARSs are present in both cytoplasm and mitochondria. Seventeen cytoplasmic ARS, 18 mitochondrial ARSs, and 2 dual localized enzymes are known till date [12]. The role of various ARSs and this translational machinery in the development and maintenance of neurons and the peripheral nervous system is being increasingly recognized. Various ARS are now known to cause encephalopathies, peripheral neuropathies, and other sensorineural disorders (Supplementary Fig. S1). Among them, mutations in 10 cytosolic ARSs are associated with Charcot–Marie–Tooth and related neuropathies, and 14 mitochondrial ARSs are associated with severe leukoencephalopathies [3]. Mitochondrial ARSs (AARS2, EARS2, FARS2, HARS2, MARS2, RARS2, SARS2, YARS2, DARS2) cause phenotypes similar to those observed due to mutations in the corresponding tRNA genes [12]. Pathogenic variants in DARS and its mitochondrial counterpart DARS2 cause hypomyelination with brainstem and spinal cord involvement and leg spasticity (MIM # 611105) [13]. Of the auxillary proteins, p43/AIMP1 has been associated with hypomyelinating leukodystrophy-3 characterized by progressive neurodegeneration, microcephaly, spasticity, coarse facies, progressive contractures, generalized brain atrophy, and early death (MIM #260600) [14].
In human and other mammalian cells, a unique large multi-tRNA synthetase complex (MSC) organizes nine cytoplasmic ARSs consisting of bifunctional ARSs, glutamyl-prolyl-tRNA synthetase, as well as the monospecific isoleucyl, leucyl, glutaminyl, methionyl, lysyl, arginyl, and aspartyl-tRNA synthetases [15] and three non-enzyme factors, namely p43, p38, and p18 (alternatively known as ARSs-interacting multifunctional proteins 1, 2, and 3, or AIMP1, AIMP2, and AIMP3, respectively) [16, 17]. Though the ARS complex has primary function of protein synthesis, there are several non-canonical biological functions of the various components of this complex, which includes their role in multiple signaling pathways.
AIMP2/p38 is a non-synthetase component of multi-ARS complex. The cDNA encodes 320 amino-acid protein that was first isolated by Quevillon et al. [15]. The p38 protein consists of a lysyl-tRNA synthetase binding domain, a putative leucine-zipper motif, and a C-terminal-like glutathione S-transferase domain and contains sequence patterns, which are the binding regions for protein–protein interactions (http://www.ebi.ac.uk/interpro/protein/Q13155). The protein is widely expressed in different human tissues including brain, colon, pancreas, breast (https://www.proteomicsdb.org). Five components of MSC (p43, p18, RRS, MRS, and IRS) depend on p38 for their stability. Thus, p38 serves as a template on which the other components are assembled [18].
RT-PCR in mice with mutation in p38 has shown undetectable levels of the p38 mRNA levels. However, the levels of MRS, RRS, p43, and p18 mRNA were same as that of controls but a variable decrease in the protein levels of the component enzymes of MSC as well as the cofactors, p43 and p18, suggesting decreased stability of these proteins in the absence of functional p38. Also, the complex-forming enzymes in the mutant cells showed reduced catalytic activities as compared with their corresponding enzymes in the wild type, whereas the activities of the two other free-form ARSs were only slightly affected in the mutant cells. Hence, p38 mutations perturb the stability and formation of the complex. On RT-qPCR, AIMP2 mRNA levels were found to be decreased in our patients similar to those reported with mutations in p38 in mice [18].
Further, homozygous mutant mice do not show embryonic lethality and are born with normal shape and size. However, they died within 2 days of birth, implying the physiological significance of p38 in the postnatal stage [18]. This correlates with the severe neurodegeneration and early death observed in the reported families. The second family in our study was ascertained through GeneMatcher [19]. Families with rare single gene disorders are unlikely to be ascertained at a single center and hence GeneMatcher has been a very helpful resource for ascertainment of additional family in our study.
The p38 protein is a key component of the multi-ARS complex. The phenotype of our patients shares marked similarity with that caused by mutations in closely related protein p43/AIMP1 [14]. Taken together, the data suggest that deleterious variants in AIMP2, which leads to decreased levels of mRNA are likely to be associated with a severe neurodevelopmental disorder in humans.
References
Robinson JC, Kerjan P, Mirande M. Macromolecular assemblage of aminoacyl-tRNA synthetases: quantitative analysis of protein-protein interactions and mechanism of complex assembly. J Mol Biol. 2000;304:983–94.
Kim JH, Han JM, Kim S. Protein-protein interactions and multi-component complexes of aminoacyl-tRNA synthetases. Top Curr Chem. 2014;344:119–44.
Ognjenovic J, Simonovic M. Human aminoacyl-tRNA synthetases in diseases of the nervous system. RNA Biol. 2017. https://doi.org/10.1080/15476286.2017.1330245.
Guo Y, Ding X, Shen Y, Lyon GJ, Wang K. SeqMule: automated pipeline for analysis of human exome/genome sequencing data. Sci Rep. 2015;5:14283. https://doi.org/10.1038/srep14283.
Wang K, Li M, Hakonarson H. ANNOVAR: functional annotation of genetic variants from high-throughput sequencing data. Nucleic Acids Res. 2010;38:e164. https://doi.org/10.1093/nar/gkq603.
Girisha KM, Shukla A, Trujillano D, Bhavani GS, Hebbar M, Kadavigere R, et al A homozygous nonsense variant in IFT52 is associated with a human skeletal ciliopathy. Clin Genet. 2016;90:536–9.
Vigeland MD, Gjotterud KS, Selmer KK. FILTUS: a desktop GUI for fast and efficient detection of disease-causing variants, including a novel autozygosity detector. Bioinformatics. 2016;32:1592–4.
Shukla A, Hebbar M, Srivastava A, Kadavigere R, Upadhyai P, Kanthi A, et al Homozygous p.(Glu87Lys) variant in ISCA1 is associated with a multiple mitochondrial dysfunctions syndrome. J Hum Genet. 2017. https://doi.org/10.1038/jhg.2017.35.
Aggarwal S, Das Bhowmik A, Ramprasad VL, Murugan S, Dalal A. A splice site mutation in HERC1 leads to syndromic intellectual disability with macrocephaly and facial dysmorphism: further delineation of the phenotypic spectrum. Am J Med Genet. 2016;170A:1868–73.
Kircher M, Witten DM, Jain P, O’Roak BJ, Cooper GM, Shendure J. A general framework for estimating the relative pathogenicity of human genetic variants. Nat Genet. 2014;46:310–5.
Schimmel PR, Soll D. Aminoacyl-tRNA synthetases: general features and recognition of transfer RNAs. Annu Rev Biochem. 1979;48:601–48.
Yao P, Fox PL. Aminoacyl-tRNA synthetases in medicine and disease. EMBO Mol Med. 2013;5:332–43.
van der Knaap MS, van der Voorn P, Barkhof F, Van, Coster R, Krägeloh-Mann I, Feigenbaum A, et al A new leukoencephalopathy with brainstem and spinal cord involvement and high lactate. Ann Neurol. 2003;53:252–8.
Feinstein M, Markus B, Noyman I, Shalev H, Flusser H, Shelef I, et al Pelizaeus-Merzbacher-like disease caused by AIMP1/p43 homozygous mutation. Am J Hum Genet. 2010;87:820–8.
Quevillon S, Robinson JC, Berthonneau E, Siatecka M, Mirande M. Macromolecular assemblage of aminoacyl-tRNA synthetases: identification of protein-protein interactions and characterization of a core protein. J Mol Biol. 1999;285:183–95.
Park SG, Choi EC, Kim S. Aminoacyl-tRNA synthetase-interacting multifunctional proteins (AIMPs): a triad for cellular homeostasis. IUBMB Life. 2010;62:296–302.
Cestari I, Kalidas S, Monnerat S, Anupama A, Phillips MA, Stuart K. A multiple aminoacyl-tRNA synthetase complex that enhances tRNA-aminoacylation in African trypanosomes. Mol Cell Biol. 2013;33:4872–88.
Kim JY, Kang YS, Lee JW, Kim HJ, Ahn YH, Park H, et al. p38 is essential for the assembly and stability of macromolecular tRNA synthetase complex: implications for its physiological significance. Proc Natl Acad Sci USA. 2002;99:7912–6.
Sobreira N, Schiettecatte F, Valle D, Hamosh A. GeneMatcher: a matching tool for connecting investigators with an interest in the same gene. Hum Mutat. 2015;36:928–30.
Acknowledgements
We thank the families who cooperated with the evaluation of the subjects and consented for participation in this study. We are also thankful to Dr. Vineeth VS & Dr. Usha R Dutta from Diagnostics Division, Centre for DNA Fingerprinting and Diagnostics, Hyderabad for assisting in RT-qPCR experiment. Our sincere thanks to Ms. Priyanka Bhakt and Dr. Rupinder Kaur from the Laboratory of Fungal Pathogenesis, Centre for DNA Fingerprinting and Diagnostics, Hyderabad for assisting in statistical analysis of RT-qPCR using GraphPad Prism software.
Funding
This work was supported by the Department of Health Research, which funded the project titled “Clinical and molecular characterization of leukodystrophies in Indian children” (V.25011/379/2015-GIA/HR) and Science and Engineering Research Board (SERB), Government of India (SERB file no. YSS/2015/001681) and Department of Biotechnology, Government of India, Grant Number: BT/PR3193/MED/12/521/2011.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Electronic supplementary material
Rights and permissions
About this article
Cite this article
Shukla, A., Das Bhowmik, A., Hebbar, M. et al. Homozygosity for a nonsense variant in AIMP2 is associated with a progressive neurodevelopmental disorder with microcephaly, seizures, and spastic quadriparesis. J Hum Genet 63, 19–25 (2018). https://doi.org/10.1038/s10038-017-0363-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s10038-017-0363-1
This article is cited by
-
Knockdown of Golgi Stress-Responsive Caspase-2 Ameliorates HLD17-Associated AIMP2 Mutant-Mediated Inhibition of Oligodendroglial Cell Morphological Differentiation
Neurochemical Research (2022)
-
Roles of aminoacyl-tRNA synthetase-interacting multi-functional proteins in physiology and cancer
Cell Death & Disease (2020)
-
Clinical Features of Patients With 7p22.1 Microdeletion
Indian Pediatrics (2020)
-
Aminoacyl-tRNA synthetases as therapeutic targets
Nature Reviews Drug Discovery (2019)