Abstract
Background
The biased immune reactions of the adenotonsillar tissues are not always reflected by the serum immunoglobulin E (IgE); thus, we hypothesize that the systemic atopic status may not be changed after the adenotonsillectomy (AT) in children.
Methods
Twenty-five children with AT and 23 age-matched healthy children were enrolled into this study, and followed up for ~4 years. Nasal Symptoms Scores (NSS), Quality of Life Scores (QOLS), specific IgE (sIgE), cytokines, and inflammatory cell were documented in all the subjects before and after study.
Results
Fourteen patients and three healthy controls had positive serum sIgE levels (>0.35 kU/l) at the study-start that was not changed by the study-end. Two patients and two sIgE-negative healthy controls showed the Dermatophagoidespteronyssinus sensitization at the study-end. NSS and QOLS showed significant improvement after the surgery in the sIgE-positive patients (P<0.05), whereas no significant changes were found in the sIgE-negative patients (P=1.00). In addition, the serum sIgE-negative patients showed significant increases in interleukin (IL)-4, IL-5, and IL-10 levels in the serum (P<0.001), although no significant differences were found post surgery (P=0.667, 0.408, and 0.714, respectively).
Conclusions
Our study showed that AT did not affect the pediatric atopic status. The systemic atopy may be independent of the tonsillar and adenoid tissues in children.
Similar content being viewed by others
Main
Nasopharynx-associated lymphoid tissue is an important site for the induction and regulation of mucosal immunity. Shin et al. detected local immunoglobulin E (IgE)-mediated hypersensitivity to Staphylococcus only in atopic patients, whereas local IgE-mediated hypersensitivity to Alternaria was detected in both atopic and non-atopic patients (1, 2). We previously reported that in childhood adenotonsillar hypertrophy, patients were sensitized to more than two allergens in both the tonsillar and adenoidal tissues, despite the fact that half of the patients were serum-specific IgE (sIgE)-negative (3). These data imply that there may be biased immune reactions in the adenotonsillar tissues that are not always reflected by the serum IgE.
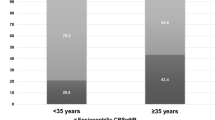
Published data indicate that adenotonsillectomy (AT) has no significant effect on the systemic immunity (4), and no detectable changes in serum IgE levels can be found after AT (5, 6). However, in a group of 274 adenoidectomized children followed up for 16 months, the incidence of atopy was 23.6% at study-start, which was even increased to 39.0% (ref. 7). Thus, we hypothesize that the systemic atopy may be independent of the tonsillar and adenoid tissues in children. In the present study, the serum sIgE levels were measured for ~4 years after AT. Eosinophils, mast cells, and cytokines were examined in both blood samples and adenotonsillar tissues. The differential inflammatory cells and germinal centers were counted in histology sections of the surgically removed tonsil and adenoid tissues. This study provides new evidence to investigate the relationship between systemic immunity and adenotonsillar atopy in children.
Methods
Study Subjects and Design
A total of 48 children were enrolled in this study. Twenty-five of them received AT surgery between February 2010 and May 2012 in our department. The inclusion criteria were the same as our previous report (3). The exclusion criteria were as follows: (i) signs of acute infections at the time of sample collection in children; (ii) steroid or other immunosuppressor consumption by patients during the study period. Twenty-three children who visited our hospital for routine health examinations without any history and symptoms of adenotonsillar hypertrophy, allergic rhinitis, and asthma were enrolled into this study as controls. All patients were re-examined on February to May 2016. Table 1 shows the demographic data. The Nasal Symptoms Scores (NSS) and the Quality of Life Scores (QOLS) were recorded pre-surgery and at the time of follow-up. This study was approved by the Ethics Committee at Guangzhou Medical University, and an informed written consent was obtained from the legal caregiver of each participant.
sIgE Analysis in Adenotonsillar Tissues and Serum
Adenotonsillar tissue samples were divided into three pieces: the first piece was processed for the detection of sIgE as previously described (3); the second piece was used to extract proteins for cytokine detection; and the third piece was fixed overnight in 4% formaldehyde (pH 7.4) and then embedded in paraffin wax for histological evaluation. The sera were obtained from whole-blood samples after centrifugation and stored at −80 °C until use. Serum sIgE against 31 common allergens was measured pre- and post surgery using the Pharmacia Immuno-CAP system according to the manufacturer’s instructions (Pharmacia Diagnostics, Clayton, NC). The analysis for the presence of a sIgE was defined as positive when the serum level of sIgE was ≥0.35 kU/l.
Enzyme-Linked Immunosorbent Assay Measurements of Cytokines in the Serum and Adenotonsillar Tissue
The tonsils and/or adenoid tissues were minced into small pieces and homogenized with cold phosphate-buffered saline on ice. The lysates were further sonicated. After centrifuging for 15 min at 5,000g, the supernatant was collected. The protein concentration in the samples was determined using the BCA assay method (Thermo Scientific Pierce, Waltham, MA). The levels of interleukin (IL)-2, IL-4, IL-5, IL-10, IL-13, IL-17, interferon (IFN)-γ, and tumor necrosis factor (TNF)-β in the samples were determined using commercial enzyme-linked immunosorbent assay (ELISA) kits from Cayman Chemical (Ann Arbor, MI) according to the manufacturer’s instructions.
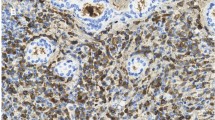
Differential Inflammatory Cell and Germinal Center Counts
Paraffin sections were prepared with the tonsil and adenoid tissues, and were stained with hematoxylin and eosin. Different inflammatory cells were counted using the following criteria: macrophage cells were based on evidence of red blood cell phagocytosis, the presence of phagocytosed pigment, non-distinct nucleoli, and on whether the cells possessed an irregular shape. Eosinophils were identified based on the presence of a band-shaped nucleus, two bean-shaped nuclei, or a nucleus with three lobes; additional criteria were the presence of a pinkish granular cytoplasm and an irregular multilobed nucleus. Neutrophils were identified based on the presence of neutrophil granules in the cytoplasm, filaments connecting nuclear lobes, and coarse chromatin. Lymphocyte cells were identified based on the presence of azurophilic granules in a light-blue cytoplasm. The germinal centers were identified based on the presence of distributed uniform and dense small lymphocytes, surrounded with flat reticular cells; the boundary is clear and the central part of the nodule is stained relatively light. At least 500 macrophages, eosinophils, neutrophils, and lymphocytes on one section were counted using microscopy.
Statistical Analysis
The statistical package of SPSS (Version 16; SPSS, Chicago) was used in data analysis. All the data are presented as mean±SEM. The results of NSS and QOLS were compared between pre- and post-study with Student's t-test. The differences of cytokines, inflammatory cell, and germinal center counts between serum sIgE-positive and -negative patients or controls were determined by Student's t-test. A P value <0.05 was considered statistically significant.
Results
Improvement of Clinical Symptoms after Surgery
In atopic (serum sIgE-positive) patients post surgery, the NSS and QOLS were reduced 71.4 % and 72.2%, respectively, (P<0.01) as compared with those in patients pre-surgery. In contrast, no significant differences in NSS and QOLS were found between post- and pre-surgery samples in non-atopic (serum sIgE-negative) patients (Figure 1). These findings suggest that the AR-related symptoms in serum sIgE-positive patients were relieved after surgery.
Improvement in clinical symptoms post surgery. The Nasal Symptoms Score (NSS; a) and the Quality of Life Scores (QOLS; b) were both significantly reduced in serum sIgE-positive patients post surgery vs. pre-surgery (decreases of 71.4% and 72.2%, respectively; both P<0.01), whereas no significant changes in NSS or QOLS were found in serum sIgE-negative patients post-surgery vs. pre-surgery or all healthy controls pre-study vs. post-study. The data presented are mean±SEM. ** denotes P<0.01.
Systemic Atopic State was not Changed after Surgery
All patients with ATH were sensitized to more than two allergens as revealed by the sIgE levels in the tonsil and/or the adenoid tissues, in which 14 (56%) of the patients and 3 (13%) of the controls also had positive results of serum sIgE (i.e., one or more anti-allergen serum sIgEs were detected). The atopic state was not changed post surgery in these patients. Two (18.2%) of the serum sIgE-negative patients and two (10%) of the serum sIgE-negative controls showed the Dermatophagoides pteronyssinus (house dust mite) sensitization in the period of follow-up.
Th2-Predominant Responses relate to Systemic Allergy
To further explore the difference between local and systemic immunity, we examined the expression of cytokines (IL-2, IL-4, IL-5, IL-10, IL-13, IL-17, IFN-γ, and TNF-β) in the serum and adenotonsillar tissues, respectively. The results showed that, in both pre-surgery patients and pre-study controls, the levels of IL-4, IL-5, and IL-10 in the serum of atopic children (serum sIgE-positive) were higher than those in pre-surgery patients (P<0.05, Figure 2). There were no differences in the serum levels of IL-2, IL-13, IL-17, IFN-γ, and TNF-β in both atopic group and non-atopic group in pre- and post surgery. We also compared the expression of IL-2, IL-4, IL-5, IL-10, IL-13, IL-17, IFN-γ, and TNF-β in surgically removed tissues between atopic and non-atopic groups; no significant difference was found in any of the cytokines tested (Figure 3). The results suggest that Th2 responses relate to the systemic immune response.
Increased levels of Th2 cytokines in serum from atopic children. The serum levels of IL-4 (b), IL-5 (c) and IL-10 (d) in all atopic children (both patients and healthy controls) were significantly enhanced compared to the levels of these same cytokines in all non-atopic children (P<0.05);there were no significant changes between pre- and post-surgery. The serum levels of interleukin (IL)-2 (a), IL-13 (e), IL-17 (f), interferon (IFN)-γ (g), and tumor necrosis factor (TNF)-β (h) were not significantly different between atopic and non-atopic children or between pre- and post-operation. The data presented are mean±SEM. * denotes P<0.05.
Local Inflammatory Cell and Germinal Center Counts Showed no Significant Differences between Atopic and Non-Atopic Children
Differential inflammatory cell counts (macrophages, eosinophils, and lymphocytes) and germinal center counts were conducted in adenotonsillar tissues from all the patients post surgery; no significant difference in any of the counts of the five cell types was observed between atopic and non-atopic children (Figure 4), which is consistent with the lack of difference in tissue cytokine levels between these children (Figure 3).
Discussion
Our results showed that AT did not change the atopic status of patients with adenoidectomy after a follow-up for an average of 4.1 years. Moreover, two (18.2%) new cases of atopy developed during the follow-up period. The data suggest that systemic atopy may be independent of the inflammation of tonsillar and adenoid gland in children.
Kjellman et al. reported that the incidence of atopic disease was inconsistent with the laboratory findings (7). It was noted that adenoidectomized children of any age did not have higher levels of sIgE. It seems that allergy is either overdiagnosed clinically or is insufficiently detected by serology among the adenoidectomized children (8). The conclusion that no change in serum IgE levels after AT is to be further tested. With the CAP method, which is the gold standard for identification of allergy, our result showed that atopy children after AT were still sensitized to more than one allergens in the serum. The data suggest that atopy still exist after AT.
Interestingly, a 6-year-old boy and a 15-year-old girl, who were serum sIgE-negative before AT, developed Dermatophagoides pteronyssinus sensitization after AT (64 months and 38 months, respectively). A similar observation was reported by Rondon et al. (9), which followed the natural evolution of 180 non-allergic rhinitis patients for 3–7 years and found that 24% of the patients became sensitive to aeroallergens. Sheehan et al. reported that cats, dogs, and dust mites were the predominant offending allergens in younger children, whereas trees and dust mites were the offending allergens in older children and adolescents. They also showed that in contrast to grass and ragweed, tree sensitization was more common than expected in very young children (10).
Increased local IgE production in polyp tissues might contribute to mucosal mast cell activation and eosinophilic inflammation independent of systemic atopy (11, 12). In the present study, the adenotonsillar tissue inflammatory cell (macrophages, eosinophils, neutrophils, and lymphocytes) counts as well as the adenotonsillar tissue germinal center counts revealed that there were no significant differences between atopic and non-atopic patients. Because of the inability to measure inflammatory cells in normal adenotonsillar tissue, we could not confirm that only eosinophils and mast cells were the two chief effector cells in the allergic response. Zhang et al. suggested that nasal IL-4(+) T follicular helper cells might be involved in local IgE production in eosinophilic nasal polyps (13). Our results showed enhanced levels of the cytokines of IL-4, IL-5, and IL-10 in the serum from atopic children compared with those from non-atopic children, and it was interesting that no significant differences were found in the same patients pre- and post surgery. The results suggest that the Th2 response is related to systemic allergy, but not to local allergy. The underlying mechanisms remain to be further investigated.
Regardless of the lack of effect of AT on cytokines, both the NSS and the QOLS were significantly improved after AT in subjects with atopy, suggesting that AT still has some benefit. Bhattacharjee et al. suggested that the adenotonsillar tissue removal may improve asthma (14). Another study showed that AT modulates chitinase activity, affects airway inflammation, and improves airway function (15). Kim and Han found that patients with worsened QOLS had higher total IgE levels and they complained of rhinitis symptoms more frequently; children with atopy were more likely to experience deterioration in QOLS than those without AT (16). It is worth noting that, from the evidence provided in the current study, AT does not change long-term pediatric atopic status and does not prevent the development of new atopy. Continued anti-allergic treatment is still necessary for atopic patients after AT.
Limitations
There were several limitations to this study. First, this was a single-center study with a relatively small sample size. Second, we evaluated changes in sIgE for all subjects at a single time point and not over a period of time; thus, we could have missed changes in any of the parameters measured. Third, cytokine levels were assessed using commercial ELISA kits; the measurements of number and identity of inflammatory cells could be significantly improved if flow cytometry were used.
Conclusions
To the best of our knowledge, this is the first report that AT did not change pediatric atopic status and new atopy development. The data suggest that systemic atopy may be independent of tonsillar and adenoid tissues in children. Therefore, continuous anti-allergy treatment after AT is still necessary for patients with atopy.
References
Shin SY, Choi GS, Lee KH, Kim SW, Cho JS, Park HS . IgE response to staphylococcal enterotoxins in adenoid tissues from atopic children. Laryngoscope 2009;119:171–5.
Shin SY, Ye YM, Eun YG, Kim SW, Cho JS, Park HS . Local IgE-mediated hypersensitivity to Alternaria in pediatric adenoid tissue. Int J Pediatr Otorhinolaryngol 2012;76:1423–8.
Zhang X, Sun B, Li S, Jin H, Zhong N, Zeng G . Local atopy is more relevant than serum sIgE in reflecting allergy in childhood adenotonsillar hypertrophy. Pediatr Allergy Immunol 2013;24:422–6.
Bitar MA, Dowli A, Mourad M . The effect of tonsillectomy on the immune system: a systematic review and meta-analysis. Int J Pediatr Otorhinolaryngol 2015;79:1184–91.
van den Akker EH, Sanders EA, van Staaij BK, et al. Long-term effects of pediatric adenotonsillectomy on serum immunoglobulin levels: results of a randomized controlled trial. Ann Allergy Asthma Immunol 2006;97:251–6.
Sainz M, Gutierrez F, Moreno PM, Munoz C, Ciges M . Changes in immunologic response in tonsillectomized children. I. Immunosuppression in recurrent tonsillitis. Clin Otolaryngol Allied Sci 1992;17:376–9.
Kjellman NI, Harder H, Hansson LO, Lindwall L . Allergy, otitis media and serum immunoglobulins after adenoidectomy. Acta Paediatr Scand 1978;67:717–23.
Suvilehto J, Seppanen M, Notkola IL, et al. Association of allergy, asthma and IgE sensitisation to adenoidectomy and infections in children. Rhinology 2007;45:286–91.
Rondon C, Dona I, Torres MJ, Campo P, Blanca M . Evolution of patients with nonallergic rhinitis supports conversion to allergic rhinitis. J Allergy Clin Immunol 2009;123:1098–102.
Sheehan WJ, Rangsithienchai PA, Baxi SN, et al. Age-specific prevalence of outdoor and indoor aeroallergen sensitization in Boston. Clin Pediatr 2010;49:579–85.
Cao PP, Zhang YN, Liao B, et al. Increased local IgE production induced by common aeroallergens and phenotypic alteration of mast cells in Chinese eosinophilic, but not non-eosinophilic, chronic rhinosinusitis with nasal polyps. Clin Exp Allergy 2014;44:690–700.
Bachert C, Gevaert P, Holtappels G, Johansson SG, van Cauwenberge P . Total and specific IgE in nasal polyps is related to local eosinophilic inflammation. J Allergy Clin Immunol 2001;107:607–14.
Zhang YN, Song J, Wang H, et al. Nasal IL-4(+)CXCR5(+)CD4(+) T follicular helper cell counts correlate with local IgE production in eosinophilic nasal polyps. J Allergy Clin Immunol 2016;137:462–73.
Bhattacharjee R, Choi BH, Gozal D, Mokhlesi B . Association of adenotonsillectomy with asthma outcomes in children: a longitudinal database analysis. PLoS Med 2014;11:e1001753.
Levin JC, Gagnon L, He X, Baum ED, Karas DE, Chupp GL . Improvement in asthma control and inflammation in children undergoing adenotonsillectomy. Pediatr Res 2014;75:403–8.
Kim DK, Han DH . Impact of allergic rhinitis on quality of life after adenotonsillectomy for pediatric sleep-disordered breathing. Int Forum Allergy Rhinol 2015;5:741–46.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
The first five authors contributed equally to this work.
Statement of Financial Support
This work was jointly supported by China National Natural Science Foundation (81271066), the Research and Innovation Foundation of Guangzhou (No.1561000231), and the Sciences and Technology Program of Guangdong province (2014A020212420).
Rights and permissions
About this article
Cite this article
Song, L., Guo, J., Liao, W. et al. Long-term effects of adenotonsillectomy on serum-specific immunoglobulin E. Pediatr Res 82, 801–805 (2017). https://doi.org/10.1038/pr.2017.165
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/pr.2017.165