Abstract
Human fetal metabolism is largely unexplored. Understanding how a healthy fetus achieves its fast growth rates could eventually play a pivotal role in improving future nutritional strategies for premature infants. To quantify specific fetal amino acid kinetics, eight healthy pregnant women received before elective cesarean section at term, continuous stable isotope infusions of the essential amino acids [1-13C,15N]leucine, [U-13C5]valine, and [1-13C]methionine. Umbilical blood was collected after birth and analyzed for enrichments and concentrations using mass spectrometry techniques. Fetuses showed considerable leucine, valine, and methionine uptake and high turnover rates. α-Ketoisocaproate, but not α-ketoisovalerate (the leucine and valine ketoacids, respectively), was transported at net rate from the fetus to the placenta. Especially, leucine and valine data suggested high oxidation rates, up to half of net uptake. This was supported by relatively low α-ketoisocaproate reamination rates to leucine. Our data suggest high protein breakdown and synthesis rates, comparable with, or even slightly higher than in premature infants. The relatively large uptakes of total leucine and valine carbon also suggest high fetal oxidation rates of these essential branched chain amino acids.
Similar content being viewed by others
Main
Historical wise, the fact that the design of current nutrition for premature neonates is merely step-by-step alterations of the original composition of breast milk (1) is not surprising. Years ago, gestational viability was closer to term than it is currently, and the analysis of normal neonatal nutrition was easier than the study of fetal nutrition. But with increased survival of less mature infants, metabolic demands of these young individuals probably deviate much more from those who receive breast milk or regular formula after term birth. Besides, we know from several decades of animal fetal research that intrauterine nutrient supply delivers more amino acids and less fat than is supplied during breast feeding (2). Today, however, the exact composition of human fetal nutrient supply still remains unknown.
With the availability of harmless tracer studies, human fetal metabolism can be unraveled (3–7). To add to the very scarce knowledge bank, our aim was to investigate several aspects of human fetal essential amino acid metabolism. In this study, we were interested in fetal kinetics of the branched chain amino acids (leucine and valine) and of another essential amino acid, methionine. Previously, fetal kinetics of phenylalanine and tyrosine were described. These two amino acids together with those studied here were chosen both scientifically as well as practically. First, they are often subject of debate when it comes to (parenteral) neonatal nutrition. Second, their stable isotopomers are affordable, and our laboratory has much experience analyzing them accurately. Metabolism was determined after the infusion of stable isotopically labeled amino acids into pregnant women undergoing elective cesarean section at term and by analyzing umbilical cord blood. These studies provide explorative and normative data against which amino acid metabolism in the premature fetus or neonate after, for example, fetal growth restriction or prematurity can be judged.
METHODS
Patients.
The study was performed at the Mother and Child Center of the Erasmus MC–Sophia Children's Hospital after approval by both the institutional medical ethical review board (Erasmus MC, Rotterdam, The Netherlands) and the Dutch central committee on research involving human subjects. Pregnant women undergoing elective cesarean section (repeat or breech presentation) at term were eligible. Exclusion criteria were obesity (preconceptional BMI >30), preeclampsia, diabetes, known fetal anomalies, or severe IUGR (<−2 SD). Participating women gave written consent after having been fully informed about all study details.
Experimental design.
To determine the umbilical blood flow, blood flow velocity and vessel diameters were measured in the umbilical vein using an ultrasound machine (iU22; Philips Medical Systems, Eindhoven, The Netherlands) as previously described (8). Ultrasound measurements were made in the late afternoon on the day preceding surgery; cesarean sections were scheduled at ∼0800 h after an overnight fast.
At least 4 h before planned surgery, the women received a primed continuous infusion of L-[1-13C,15N]leucine [8 μmol/(kg · h)] through a forearm vein. Two hours later, primed continuous infusions of L-[U-13C5]valine and L-[1-13C]methionine [5 and 2 μmol/(kg · h), respectively] were started along. All priming doses were half the hourly doses. Isotopes (all >98% enriched and tested for sterility and pyrogenicity) were obtained from Buchem BV, Apeldoorn, The Netherlands (local distributor of Cambridge Isotope Laboratories, Andover, MA). Our hospital pharmacy dissolved the isotopes in 0.9% saline, and the solutions were filtered (0.2 μm) and sterilized. Tests were performed to ensure the correct identity, concentration, and a sterile and pyrogen-free product. Tracers were given using Perfusor fm (B Braun Medical B.V., Oss, The Netherlands) infusion pumps. Maternal blood was sampled before the tracer infusions started (baseline), once immediately before anesthesia (spinal) and, if possible (n = 4), about 20 min later just before surgery started. Fetal blood was sampled after birth from both the vein and arteries of a doubly clamped segment of the umbilical cord. After collection in heparin tubes, blood was centrifuged and plasma was frozen at −80°C until analysis.
Analysis.
As calculations in a venoarterial balance model (as on the umbilical cord in the fetus, see later) largely depend on the small differences in concentration and enrichment between the vein and arteries, rather than on the absolute values, measurements must be extremely precise. To minimize the effects of potential analytical measurement errors, samples were prepared for analysis twice using two different derivatization methods [propylchloroformate (PCF) and N-methyl-N-(tert-butyldimethylsilyl)trifluoroacetamide (MTBSTFA), see later]. Each derivatized sample was analyzed in triplicate on two different gas chromatography mass spectrometers (GCMS, see later). Enrichments of valine and methionine were calculated from the mean of all 12 analyses; enrichments of leucine isotopomers [m + 0, m + 1: [1-13C]leucine (without 15N) and m + 2: [1-13C,15N]leucine] were calculated from the MTBSTFA samples only (due to the fragmentation pattern after PCF analysis); and amino acid concentrations were calculated from the mean of the six analyses using the MTBSTFA derivative.
PCF derivatization on samples was performed using commercial kits (EZ:Faast for hydrolysates; Phenomenex, Bester BV, Amstelveen, the Netherlands) according to the enclosed protocol. Samples to be derivatized with MTBSTFA were added with [D10]leucine, [D8]valine, and [U-13C5,15N] methionine as internal standards for concentration determinations. Concentration calibration curves were prepared using MTBSTFA as well. Two different enrichment calibration curves were derivatized with PCF and MTBSTFA for analysis. Samples and calibration curves were analyzed with a MSD 5975C Agilent GCMS (Agilent Technologies, Amstelveen, The Netherlands) on a VF-17 ms, 30 m × 0.25 mm ID capillary column (Varian Inc., Middelburg, The Netherlands) and a Thermo DSQ GCMS (Thermo Fisher, Breda, The Netherlands) on a VF-1701 ms, 30 m × 0.25 mm ID capillary column (Varian Inc.).
Samples intended to be analyzed for the enrichments and concentrations of the ketoacids α-ketoisocaproate (αKIC) and α-ketoisovalerate (αKIV) were added with [methyl-D3]αKIC and [dimethyl-13C2]αKIV as internal standards. Enrichment and concentration calibration curves were also prepared. Samples were derivatized with quinoxanol-silyl, phenylenediamine, and MTBSTFA and measured in triplicate on the same Thermo DSQ GCMS as described earlier.
Calculations.
Maternal leucine fluxes were calculated from the tracer dilution resulting from the rate of leucine appearance (9,10). In short, carbon leucine flux (QC) is made up of leucine appearing from proteolysis only, whereas nitrogen leucine flux (QN) is made up of both proteolysis and αKIC reamination. Thus, the difference between QN and QC yields the rate of αKIC reamination to leucine. Fluxes were calculated as I × [(Ei/Ep) − 1], where I is the [1-13C,15N]leucine infusion rate and Ei and Ep represent the enrichments in mole percent excess (MPE) of the infusate and of plasma [1-13C,15N]leucine, or [1-13C]αKIC yielding QN or QC, respectively. Because [1-13C,15N]leucine enrichment in plasma is no more than the site of infusion and not the site where the majority of metabolism will take place, the plasma enrichment will be slightly overestimated leading to an underestimated QN. The [1-13C]αKIC enrichment is the resultant from intracellular metabolism and thus gives a good reflection of intracellular metabolism because of rapid exchange. Maternal valine and methionine kinetics were studied regarding their carbon skeletons only; QC was calculated analogous to leucine using the [U-13C6]αKIV enrichment.
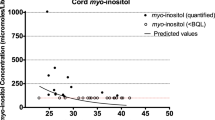
We quantified fetal whole body kinetics by using the concept of an umbilical venoarterial balance model (Fick principle). To do so, we rewrote the leucine arteriovenous balance model by Tessari et al. (11) to suit fetal studies. The model is outlined in Figure 1 and its determinants are calculated using the following equations:
Schematic model of fetal leucine metabolism. Numbers in brackets correspond to the equations in the methods section and the fluxes outlined in Table 4. Dashed lines indicate fluxes that could not be quantified. Fluxes 14 and 15 are the sums of protein synthesis and either deamination or oxidation, respectively.
Rate of leucine (leu) delivery from umbilical vein to the fetus:
Equation 1

where [leu] is the total (labeled + unlabeled) leucine concentration (μmol/L) and blood flow is expressed in L/(kg · h), where kg denotes fetal weight (= birth weight). Subscripts indicate whether blood was sampled from the umbilical vein or arteries (as below). All rates are expressed in μmol/(kg · h).
Rate of leucine release from fetus to umbilical artery:
Equation 2

Net fetal leucine uptake:
Equation 3

Rate of αKIC delivery from umbilical vein to the fetus:
Equation 4

where [KIC] is the total (labeled + unlabeled) αKIC concentration (μmol/L).
Rate of αKIC release from fetus to umbilical artery:
Equation 5

Net fetal α-ketoisocaproate uptake:
Equation 6

Net total leucine carbon (TLC) uptake:
Equation 7

Fraction of leucine that is metabolized intracellularly:
Equation 8

where [13C,15N · leu] is the labeled [1-13C,15N]leucine concentration (μmol/L).
Fraction of [1-13C]leucine that is metabolized intracellularly:
Equation 9

where [13C·leu] is the total labeled [1-13C]leucine concentration (μmol/L). The total [1-13C]leucine enrichment was calculated as the sum of the [1-13C]leucine (without 15N) enrichment and the [1-13C,15N]leucine enrichment.
Rate of leucine inflow from umbilical vein to intracellular compartment:
Equation 10

Rate of leucine outflow from intracellular compartment to umbilical artery:
Equation 11

Rate of leucine directly released from umbilical vein to artery without being metabolized:
Equation 12

Rate of intracellular α-ketoisocaproate reamination to leucine:
Equation 13

where 13C · KIC · E is the [1-13C]αKIC enrichment (MPE).
In our model, we could not discriminate between leucine being incorporated into protein and leucine being deaminated to αKIC. Thus, we calculated the sum of the latter two rates:
Equation 14

In our model, we could not discriminate between leucine being incorporated into protein and αKIC being oxidized to CO2. Thus, we calculated the sum of the latter two rates:
Equation 15

Rate of leucine release from proteolysis into the intracellular space:
Equation 16

The above outlined model can also be used for calculations on valine kinetics by replacing leucine, TLC, and αKIC with valine, TVC (total valine carbon), and αKIV, respectively. Equations 8 and 10–14, however, cannot be solved due to the lack of a nitrogen label on our valine tracer. Methionine kinetics were solved by replacing leucine with methionine in eqs 1–3, 9, 15, and 16; other equations were not applicable. The denominator in eq 15 (αKIC enrichment) was also replaced by methionine enrichment, thereby possibly slightly underestimating proteolysis fluxes. The term oxidation in eq 15 should be read as transsulphuration.
Proteolysis rates of these three amino acids can be converted from molar rates into grams of protein under the assumption that 1 g of fetal protein contains on average 562 μmol leucine, 395 μmol valine, and 130 μmol methionine (12).
Statistics.
Calculations were made using Microsoft Office—Excel software (version 2007; Microsoft Corp, Redmond, WA). Statistical analysis was performed using GraphPad Prism software (version 4.0; San Diego, CA). Because the number of included subjects was small (n = 8), normality of data could not be assumed. All results were therefore expressed as median (25th–75th percentile). Where informative, nonparametric testing (Mann-Whitney) was used to detect significant differences (p < 0.05).
RESULTS
We included eight feto-maternal dyads. These patients are the same as those described in an earlier study by our group on fetal phenylalanine and tyrosine kinetics (4). Maternal age, preconceptional and actual BMI, and parity together with fetal characteristics in terms of gestational age, birth weight, birth weight z-score (13), sex, umbilical blood flow, umbilical pulsatility index, and Apgar score are shown in Table 1.
From four women, we obtained two blood samples before surgery had started with an interval of ∼20 min. Enrichments did not differ during this time interval, despite spinal anesthesia being applied in between. Therefore, steady state was assumed. The other four women had only one blood sample taken, which was before anesthetics were initiated. Achieving steady state is important in whole body modeling; however, calculating kinetics in a balance model like we did on the fetus does not depend on steady state (14). The maternal and umbilical leucine, αKIC, valine, αKIV, and methionine concentrations, enrichments, and feto-maternal ratios are shown in Table 2. The feto-maternal enrichment ratios provide qualitative information on transplacental amino acid transport in relation to proteolysis rates in the placenta or fetus (and endogenous synthesis with nonessential amino acids). For example, [1-13C,15N]leucine and total [1-13C]leucine feto-maternal enrichment ratios were significantly different from each other (p = 0.012), indicating considerable placental reamination rates.
Table 3 shows maternal leucine, valine, and methionine kinetics. As the women were fasting, amino acids released from protein breakdown equaled the total rate of appearance.
Table 4 displays fetal leucine, valine, and methionine kinetics. Because we presented our data as medians, flux rates in the table do not add up correctly as outlined in our model (Fig. 1). Nonetheless, the fluxes of each individual subject do. Leucine and valine data from one patient were excluded from Table 4 as the findings deviated greatly from the other seven subjects. Results from this particular patient are outlined in the discussion.
DISCUSSION
This report is the third in a series exploring fetal amino acid and protein metabolism by our group (4,5). In this study, several metabolic pathways of the essential amino acids leucine, valine, and methionine were quantified. Previously, we found that the median fetal net protein accretion rate in the same subjects as here was 1.70 g/(kg · d) (4). This can be converted to a net accretion rate of 40 μmol leucine/(kg · h), 28 μmol valine/(kg · h), and 9.2 μmol methionine/(kg · h) (12). However, the net TLC, TVC, and methionine uptakes (Table 4) are much higher than the net accretion rates. This would therefore seem to suggest that a large proportion of these amino acids is being oxidized or, in the case of methionine, follows the transsulphuration pathway. This is especially true for valine, where 60% of the net TVC uptake would be oxidized. Leucine oxidation would contribute for ∼40% of total TLC uptake. This is close to Chien et al. (3) who estimated fetal leucine oxidation rate to be one third of TLC uptake. In the ovine fetus around term, valine has the highest net fetal uptake of all essential amino acids (15–18) but only a relatively small part is necessary for protein deposition (16). These findings, in combination with the fact that especially valine plasma concentrations are much higher during fetal life (19,20) than postnatally in healthy term breast-fed infants (21), could confirm that valine is largely oxidized during intrauterine life. However, one must note that calculations of molar ratios of amino acids in tissues can be fraught with large errors because plasma data reflect only relatively short-term half-life proteins.
We as well as Chien et al. (3) showed that human fetuses have a net output of αKIC toward the placenta. Ovine fetuses on the contrary demonstrated a net uptake of αKIC (22). However, the ketoacid of valine, i.e. αKIV, did not show any significant net uptake or output. To our knowledge, studies on ovine fetal metabolism have not described αKIV concentrations. As addressed in the results section, one fetus showed different results, especially reflected by a very high positive net uptake of αKIC [92 μmol/(kg · h)]. The uptake of αKIV was also higher [30 μmol/(kg · h)] than in the other seven fetuses. Given the surprising result in this infant, measurements on αKIC and αKIV concentrations were repeated but did not change. Interestingly enough, this fetus also had a very high reamination rate [307 μmol/(kg · h)], probably to dispose the high αKIC uptake into leucine. All other fetal leucine and valine kinetic parameters were comparable to the other fetuses. We do not have any explanation for this finding. The postnatal and later course of the infant was normal. The maternal reamination rate was comparable to the other women. As can be seen in eq 13 under methods, the quantification of the fetal reamination rate occurs mathematically independent of fetal αKIC uptake or concentrations. Besides, the fact that a high fetal αKIC uptake was counterbalanced by a mathematically independent high reamination rate gives us confidence in our methods, analyses, and thus overall results in all other subjects. As shown in Table 2, the enrichment of [1-13C]leucine (without 15N) was very similar to the enrichment of [1-13C]αKIC. This also confirms the model as a [1-13C]leucine molecule (without the 15N label) can only be formed through the reamination of a [1-13C]αKIC molecule.
Ovine premature fetuses showed reamination rates approximately twice the rate of leucine appearance from protein breakdown (23,24). This is in contrast with our results, where reamination rates are only one third of the proteolysis rates. Apart from species differences, a higher growth rate in premature fetal sheep could demand fast transamination rates to shuttle nitrogen between various tissues. Reamination rates in enterally fed growing premature neonates at 35 wk corrected GA were with ∼250 μmol/(kg · h) (25) much higher than the rates we observed in fetuses at term. In term-born healthy neonates on postnatal d 2, however, reamination rates amounting ∼140 μmol/(kg · h) were closer to our values, although still higher (26).
Taken together, it seems that our observed fetal reamination rates are lower than the postnatal values in human neonates. A reason, partially explaining the higher postnatal values, is that the placenta cannot take up substrates anymore. Thus, to avoid irreversible αKIC oxidation, neonates reaminate at high rates. Another reason for a lower reamination rate in human fetuses compared with fetal sheep could be that αKIC is being transported toward the placenta, whereas in ovine fetuses the opposite is true, which necessitates a higher reamination rate. The activity of BCAA aminotransferases (deamination) was reported to be very high in in vitro studies in human first trimester placentas (27) and ovine placentas at term (28,29). The fact that the feto-maternal enrichment ratio of [1-13C,15N]leucine was much lower than the total [1-13C]leucine enrichment ratio (p = 0.012) indicates that in this in vivo study, the placenta indeed reaminates at a high rate.
It is clear that there are many physicochemical differences between pre- and postnatal life, such as differences in energy requirements or redox state. This for sure influences whole body metabolism and implies that one cannot directly translate fetal rates into postnatal rates. Nor would fetal rates that were theoretically mimicked postnatally result in comparable in utero accretion rates. Nevertheless, for example, high fetal synthesis rates of protein would provide good insight in the ontogenetic capabilities of the metabolic system also during postnatal life.
All our concentration and enrichment measurements were done in the plasma compartment, rather than in whole blood because of analytical precision. Many studies, however, reported rapid equilibrium between erythrocyte and plasma concentrations of various amino acids, including those studied here (30–32). The role of erythrocytes in organ amino acid delivery is thus as important as the role of the plasma compartment. Compared with normal organ balance studies, the circulation time of blood in fetal balance studies is relatively long because blood from the umbilical vein can flow multiple times through the whole fetus before returning to the umbilical arteries. By then, complete mixing can be expected. Even in single organ balance studies, many groups chose to use plasma sampling in combination with whole blood flows rather than plasma flows (33–36). The latter would reduce all kinetic rates by ±40% (hematocrit) and yield improbably low kinetic rates.
Whether maternal anesthesia and surgery would have any consequences on fetal metabolism remains speculative. Spinal anesthesia might result in maternal hypotension and blood flow redistribution, but these effects can be prevented by using a lateral wedge. Furthermore, blood pressure monitoring allows for prompt correction if necessary. Besides, the pulsatility index of the umbilical artery does not seem to be influenced by spinal anesthesia (37). Konje et al. (38) measured flow using a transonic time flowmetry technique on a exteriorized loop of the umbilical cord during cesarean surgery. Their flow values halfway during surgery correspond well to our flow measurements. Besides, umbilical blood flow after vaginal delivery has been reported to be stable for the first 100 postnatal seconds (39). We thus assume that umbilical blood flow is fairly constant during surgery. The fetal metabolic response to maternal surgery remains speculative. A maternal noradrenaline surge after an invasive procedure did not seem to reach the human fetus (40). In mice, however, noradrenaline was suggested to have reached the placenta (41).
To conclude, we have described an explorative study on several metabolic pathways of three essential amino acids in human fetuses at term. Our data suggest high protein breakdown and synthesis rates, comparable with or even slightly higher than in premature infants. The relatively large uptakes of total leucine and valine carbon also suggest high fetal oxidation rates of these branched chain amino acids. Although the transamination rates seem to be large in the placenta, rates are much lower in the term fetus when compared with preterm neonates.
Abbreviations
- αKIC:
-
α-ketoisocaproate
- αKIV:
-
α-ketoisovalerate
- GCMS:
-
gas chromatography mass spectrometer
- MPE:
-
mole percent excess
- MTBSTFA:
-
N-methyl-N-(tert-butyldimethylsilyl)trifluoroacetamide
- PCF:
-
propylchloroformate
- Q C :
-
carbon leucine flux
- Q N :
-
nitrogen leucine flux
- TLC:
-
total leucine carbon
- TVC:
-
total valine carbon.
References
Greer FR 2001 Feeding the premature infant in the 20th century. J Nutr 131: 426S–430S
Battaglia FC, Meschia G 1978 Principal substrates of fetal metabolism. Physiol Rev 58: 499–527
Chien PF, Smith K, Watt PW, Scrimgeour CM, Taylor DJ, Rennie MJ 1993 Protein turnover in the human fetus studied at term using stable isotope tracer amino acids. Am J Physiol 265: E31–E35
van den Akker CH, Schierbeek H, Dorst KY, Schoonderwaldt EM, Vermes A, Duvekot JJ, Steegers EA, van Goudoever JB 2009 Human fetal amino acid metabolism at term gestation. Am J Clin Nutr 89: 153–160
van den Akker CH, Schierbeek H, Rietveld T, Vermes A, Duvekot JJ, Steegers EA, van Goudoever JB 2008 Human fetal albumin synthesis rates during different periods of gestation. Am J Clin Nutr 88: 997–1003
Galan HL, Marconi AM, Paolini CL, Cheung A, Battaglia FC 2009 The transplacental transport of essential amino acids in uncomplicated human pregnancies. Am J Obstet Gynecol 200: 91.e1–91.e7
Marconi AM, Paolini CL, Stramare L, Cetin I, Fennessey PV, Pardi G, Battaglia FC 1999 Steady state maternal-fetal leucine enrichments in normal and intrauterine growth-restricted pregnancies. Pediatr Res 46: 114–119
Boito S, Struijk PC, Ursem NT, Stijnen T, Wladimiroff JW 2002 Umbilical venous volume flow in the normally developing and growth-restricted human fetus. Ultrasound Obstet Gynecol 19: 344–349
Matthews DE, Bier DM, Rennie MJ, Edwards RH, Halliday D, Millward DJ, Clugston GA 1981 Regulation of leucine metabolism in man: a stable isotope study. Science 214: 1129–1131
Kalhan SC, Rossi KQ, Gruca LL, Super DM, Savin SM 1998 Relation between transamination of branched-chain amino acids and urea synthesis: evidence from human pregnancy. Am J Physiol 275: E423–E431
Tessari P, Inchiostro S, Zanetti M, Barazzoni R 1995 A model of skeletal muscle leucine kinetics measured across the human forearm. Am J Physiol 269: E127–E136
Widdowson EM 1980 Chemical composition and nutritional needs of the fetus at different stages of gestation. In: Aebi H, Whitehead R (eds) Maternal Nutrition During Pregnancy and Lactation: A Nestlé Foundation Workshop, Lutry/Lausanne, April 26th and 27th 1979. Hans Huber, Bern, 39–48.
Usher R, McLean F 1969 Intrauterine growth of live-born Caucasian infants at sea level: standards obtained from measurements in 7 dimensions of infants born between 25 and 44 weeks of gestation. J Pediatr 74: 901–910
Wolfe RR, Chinkes DL 2005 Isotope Tracers in Metabolic Research: Principles and Practice of Kinetic Analysis. Wiley-Liss, Hoboken
Marconi AM, Battaglia FC, Meschia G, Sparks JW 1989 A comparison of amino acid arteriovenous differences across the liver and placenta of the fetal lamb. Am J Physiol 257: E909–E915
Lemons JA, Adcock EW 3rd, Jones MD Jr, Naughton MA, Meschia G, Battaglia FC 1976 Umbilical uptake of amino acids in the unstressed fetal lamb. J Clin Invest 58: 1428–1434
Józwik M, Teng C, Battaglia FC, Meschia G 1999 Fetal supply of amino acids and amino nitrogen after maternal infusion of amino acids in pregnant sheep. Am J Obstet Gynecol 180: 447–453
JóŸwik M, Teng C, Wilkening RB, Meschia G, Battaglia FC 2004 Reciprocal inhibition of umbilical uptake within groups of amino acids. Am J Physiol Endocrinol Metab 286: E376–E383
Cetin I, Corbetta C, Sereni LP, Marconi AM, Bozzetti P, Pardi G, Battaglia FC 1990 Umbilical amino acid concentrations in normal and growth-retarded fetuses sampled in utero by cordocentesis. Am J Obstet Gynecol 162: 253–261
Marconi AM, Mariotti V, Teng C, Ronzoni S, D'Amato B, Morabito A, Battaglia FC 2010 Effect of antenatal betamethasone on maternal and fetal amino acid concentration. Am J Obstet Gynecol 202: 166.e1–166.e6
Scott PH, Sandham S, Balmer SE, Wharton BA 1990 Diet-related reference values for plasma amino acids in newborns measured by reversed-phase HPLC. Clin Chem 36: 1922–1927
Loy GL, Quick AN Jr, Battaglia FC, Meschia G, Fennessey PV 1991 Measurement of leucine and alpha-ketoisocaproic acid fluxes in the fetal/placental unit. J Chromatogr 562: 169–174
Liechty EA, Denne SC, Lemons JA, Kien CL 1991 Effects of glucose infusion on leucine transamination and oxidation in the ovine fetus. Pediatr Res 30: 423–429
Liechty EA, Boyle DW, Moorehead H, Liu YM, Denne SC 1993 Increased fetal glucose concentration decreases ovine fetal leucine oxidation independent of insulin. Am J Physiol 265: E617–E623
Parimi PS, Devapatla S, Gruca LL, Amini SB, Hanson RW, Kalhan SC 2004 Effect of enteral glutamine or glycine on whole-body nitrogen kinetics in very-low-birth-weight infants. Am J Clin Nutr 79: 402–409
Parimi PS, Devapatla S, Gruca L, O'Brien AM, Hanson RW, Kalhan SC 2002 Glutamine and leucine nitrogen kinetics and their relation to urea nitrogen in newborn infants. Am J Physiol Endocrinol Metab 282: E618–E625
Jaroszewicz L, JóŸwik M, Jaroszewicz K 1971 The activity of aminotransferases in human placenta in early pregnancy. Biochem Med 5: 436–439
Liechty EA, Barone S, Nutt M 1987 Effect of maternal fasting on ovine fetal and maternal branched-chain amino acid transaminase activities. Biol Neonate 52: 166–173
Goodwin GW, Gibboney W, Paxton R, Harris RA, Lemons JA 1987 Activities of branched-chain amino acid aminotransferase and branched-chain 2-oxo acid dehydrogenase complex in tissues of maternal and fetal sheep. Biochem J 242: 305–308
Agli AN, Schaefer A, Geny B, Piquard F, Haberey P 1998 Erythrocytes participate significantly in blood transport of amino acids during the post absorptive state in normal humans. Eur J Appl Physiol Occup Physiol 78: 502–508
Darmaun D, Froguel P, Rongier M, Robert JJ 1989 Amino acid exchange between plasma and erythrocytes in vivo in humans. J Appl Physiol 67: 2383–2388
Schaefer A, Piquard F, Haberey P 1990 The effects of changes in plasma amino acid concentrations on erythrocyte amino acid content. Clin Biochem 23: 237–240
Moller N, Jensen MD, Rizza RA, Andrews JC, Nair KS 2006 Renal amino acid, fat and glucose metabolism in type 1 diabetic and non-diabetic humans: effects of acute insulin withdrawal. Diabetologia 49: 1901–1908
Chow LS, Albright RC, Bigelow ML, Toffolo G, Cobelli C, Nair KS 2006 Mechanism of insulin's anabolic effect on muscle: measurements of muscle protein synthesis and breakdown using aminoacyl-tRNA and other surrogate measures. Am J Physiol Endocrinol Metab 291: E729–E736
Volpi E, Kobayashi H, Sheffield-Moore M, Mittendorfer B, Wolfe RR 2003 Essential amino acids are primarily responsible for the amino acid stimulation of muscle protein anabolism in healthy elderly adults. Am J Clin Nutr 78: 250–258
Volpi E, Sheffield-Moore M, Rasmussen BB, Wolfe RR 2001 Basal muscle amino acid kinetics and protein synthesis in healthy young and older men. JAMA 286: 1206–1212
Valli J, Pirhonen J, Aantaa R, Erkkola R, Kanto J 1994 The effects of regional anaesthesia for caesarean section on maternal and fetal blood flow velocities measured by Doppler ultrasound. Acta Anaesthesiol Scand 38: 165–169
Konje JC, Taylor DJ, Rennie MJ 1996 Application of ultrasonic transit time flowmetry to the measurement of umbilical vein blood flow at caesarean section. Br J Obstet Gynaecol 103: 1004–1008
Stembera ZK, Hodr J, Janda J 1965 Umbilical blood flow in healthy newborn infants during the first minutes after birth. Am J Obstet Gynecol 91: 568–574
Giannakoulopoulos X, Teixeira J, Fisk N, Glover V 1999 Human fetal and maternal noradrenaline responses to invasive procedures. Pediatr Res 45: 494–499
Thomas SA, Matsumoto AM, Palmiter RD 1995 Noradrenaline is essential for mouse fetal development. Nature 374: 643–646
Acknowledgements
We thank all the participating women. We also thank Willemijn Corpeleijn, Frans te Braake, and all the personnel from the Obstetrics and Anesthesiological departments who were very helpful in the collection of material and provision of facilities.
Author information
Authors and Affiliations
Corresponding author
Additional information
Supported by the Sophia Children's Hospital Fund (SSWO, institutional grant no. 459) and the Nutricia Research Foundation (independent charity, grant no. 2006-10).
The authors report no conflicts of interest.
Rights and permissions
About this article
Cite this article
van den Akker, C., Schierbeek, H., Minderman, G. et al. Amino Acid Metabolism in the Human Fetus at Term: Leucine, Valine, and Methionine Kinetics. Pediatr Res 70, 566–571 (2011). https://doi.org/10.1203/PDR.0b013e31823214d1
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/PDR.0b013e31823214d1
This article is cited by
-
Impact of reduced uterine perfusion pressure model of preeclampsia on metabolism of placenta, maternal and fetal hearts
Scientific Reports (2022)
-
Fetoplacental oxygen homeostasis in pregnancies with maternal diabetes mellitus and obesity
Nature Reviews Endocrinology (2022)