Abstract
The incidence of allergic diseases has increased, and a relation between allergy and dietary fatty acids has been proposed. Modulation of the maternal immune function during pregnancy may have an impact on future clinical outcomes in the child. The aim of this study was to determine the effects of omega (ω)-3 long-chain polyunsaturated fatty acids (LCPUFA) supplementation during pregnancy on the plasma fatty acid composition in relation to the maternal immune function. Pregnant women with allergic disease in their immediate family were supplemented daily with 2.7 g ω-3 LCPUFA (n = 70) or 2.8 g soybean oil as placebo (n = 75) from the 25th gestational week. The proportions of eicosapentaenoic acid and docosahexaenoic acid in plasma/serum phospholipids increased in the ω-3-supplemented group, whereas arachidonic acid decreased during intervention. Lipopolysaccharide-induced prostaglandin E2 secretion from whole blood culture supernatants (n = 59) decreased in a majority of the ω-3-supplemented mothers (18 of 28, p = 0.002). The decreased prostaglandin E2 production was more pronounced among nonatopic than atopic mothers. The lipopolysaccharide-induced cytokine and chemokine secretion was not affected. Our results indicate that ω-3 LCPUFA supplementation during the last trimester may dampen certain immune responses involved in allergic inflammation.
Similar content being viewed by others
Main
The human being is proposed to have evolved on a diet consisting of almost equal amounts of omega-(ω-)6 and ω-3 polyunsaturated fatty acids (PUFA) (1). The food habits concerning dietary fats have changed in the westernized world during recent decades and today the ω-6/ω-3 PUFA ratio has been estimated as high as 20–30:1 (1), in Sweden the corresponding ratio is approximately 5:1 (2). The predominant ω-6 PUFA in the western diet is linoleic acid (LA) and consequently cell membranes of inflammatory cells contain large amounts of its long-chain derivative, arachidonic acid (AA) (3). AA is a substrate for the production of proinflammatory eicosanoids, such as prostaglandin E2 (PGE2) and leukotriene B4 (LTB4), which are immune modulators involved in e.g. allergic inflammation (4).
Because of a common enzyme system and competition, an increased dietary intake of ω-3 long-chain PUFA (LCPUFA), i.e. eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA), may dampen the proinflammatory effects of AA at multiple levels (3). ω-3 LCPUFA supplementation may result in decreased production of AA-derived eicosanoids (3) and has been reported to decrease lipopolysaccharide (LPS)-induced interleukin (IL)-1β, IL-6, and tumor necrosis factor (TNF) production by mononuclear cells (5).
Epidemiologic studies suggest that the period from early fetal life to about 3 y of age is the most critical time period for the establishment of the immunity to allergens (6). During pregnancy, the maternal immunologic status influences the fetal immune system and may thereby have an impact on future clinical outcomes in the child (7). The debate about prenatal vs postnatal sensitization is intense (8,9). Still, it is reasonable to believe that the fetal immune system is primed during the prenatal period and studies exploring the effect of environmental factors on the development of allergic disease in childhood need to be performed in pregnant women. This was done by Dunstan et al. (10) in a previous study with focus on the prevention of clinical allergy in the offspring by ω-3 fatty acids supplementation of atopic mothers during pregnancy.
The aim of this study was to determine the effects of ω-3 LCPUFA supplementation during pregnancy on the plasma phospholipid fatty acid composition in relation to immune function, i.e. LPS-induced eicosanoid, cytokine, and chemokine release in both atopic and nonatopic women.
METHODS
Subjects.
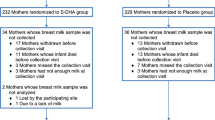
One hundred forty-five pregnant women were recruited to this investigator-initiated prospective allergy prevention study based on dietary ω-3 LCPUFA supplementation. The women were recruited at the antenatal departments or by advertisements in local newspapers in Linköping (n = 99) and Jönköping (n = 46) in the south east of Sweden during a 2-y period. Inclusion criteria were self-reported allergic symptoms, i.e. eczema, allergic rhinitis and/or conjunctivitis, asthma, urticaria, and food allergy, in the immediate family (i.e. the mother herself and/or the father and/or older siblings). Women were not included if they had fish or soy allergies, were treated with anticoagulantia, consumed supplements containing ω-3 fatty acids, or planned not to breastfeed the child.
The producer supplied a list for random allocation to active intervention, i.e. daily treatment with nine capsules containing a total of 2.7 g of ω-3 LCPUFA i.e. 1.6 g of EPA and 1.1 g of DHA, (Pharma Nord, Vejle, Denmark; n = 70) and 23 mg of α-tocopherol as an antioxidant, or placebo treatment, i.e. nine soybean oil capsules in total 2.8 g of soybean oil i.e. 2.5 of g LA and 0.3 g of α-linolenic acid (LNA) and 36 mg α-tocopherol (Pharma Nord; n = 75).
The supplementation started at the 25th (range 23.0–27.1) gestational week (gw) and continued during pregnancy and lactation for an average of 30.5 wk. All women participating in this study were supplemented during the entire period, i.e. from gw 25 to 1 wk postpartum. The total dropout rate from inclusion to partus was 17% (n = 25), 16 of 70 (23%) in the ω-3 treatment group and 9 of 75 (12%) in the placebo group (ns). The reasons for dropout were similar in the two groups and were inability to swallow capsules, nausea, abdominal pain, obstipation, urticaria, urinary tract infection, premature rupture of membranes, preeclampsia, and missed experimental supplements. Data from blood analyses performed in samples obtained at study inclusion and 1 wk after delivery are included in this study. In all, 120 mothers completed the intervention until 1 wk after delivery.
The allergic status of the mother was classified based on a standardized interview performed by an experienced allergy nurse. Serum/plasma IgE antibodies to a panel of inhalant allergens were analyzed with Phadiatop (Phadia, Uppsala, Sweden). Maternal atopy was defined as previous and/or current symptoms of allergic disease and a positive IgE Phadiatop screening test (Table 1), and consistent with these criteria 66 of 120 (55%) mothers were defined as atopic and 36 of 120 (30%) as nonatopic.
In connection with inclusion, 3-d food diaries were completed by the subjects. A certified dietician calculated the daily maternal intake of energy and fat according to a routine clinical device using the software “Dietist XP” (Kost-och näringsdata, Bromma, Sweden; www.kostdata.se). The calculated dietary intake of energy, total fat, and PUFA were similar in the ω-3 and the placebo groups (Table 1, for PUFA and energy intake).
Baseline medical data and characteristics were collected from medical records (Obstetrix, Siemens Medical Solutions, Solna, Sweden) and did not differ between the groups (Table 1). All laboratory analyses were performed in Linköping and blood samples for cell cultures were due to logistic reasons obtained only from participating women in Linköping. Serum (n = 35)/plasma (n = 77) samples for the measurement of phospholipids and detection of IgE were available from 112 women at both sampling occasions and whole blood cultures were accessible from 59 of these women. Baseline characteristics on the subgroup of mothers providing the whole blood cultures were similar with both the whole cohort and between intervention groups (data not shown).
Blood sample collection and whole blood cultures.
Blood samples with or without heparin as an additive were drawn at inclusion and within 1 wk after delivery. Serum/plasma samples were stored at −70°C until analyzed.
Whole blood cultures were established with equal parts of blood and RPMI 1640 (VWR, Stockholm, Sweden) supplemented with 2 mM l-glutamine (VWR) and 250 μg/mL gentamicin (Sigma Chemical Co., Sigma-Aldrich, Stockholm, Sweden). The cells were cultured at 37°C with 5% CO2 with 100 ng/mL LPS (Escherichia coli 026:B6, Sigma Chemical Co.) for 1 h for LTB4 secretion and for 24 h for PGE2, cytokine, and chemokine secretion. The LPS dose and incubation times for optimal PGE2 and LTB4 measurements were chosen based on earlier experiments at our laboratory. Cell cultures with medium alone served as controls, and eicosanoid, cytokine, and chemokines responses from these cultures were subtracted from the responses measured in cultures including LPS. The mean time from blood sampling to the establishment of whole blood cultures was 2 h. Supernatants were collected and stored in aliquots at −70°C until analysis.
Analysis of PGE2 and LTB4.
Eicosanoids in cell supernatants were analyzed with commercial ELISA kits from R&D Systems according to the manufacturer's instructions. Detection limits were 39 pg/mL for PGE2 and 12 pg/mL for LTB4. As a control for the quality of the method, an LPS-stimulated whole blood cell supernatant sample from a blood donor was included in every assay. The coefficient of variance for the PGE2 and LTB4 controls were 7 and 30%, respectively.
Analysis of cytokines and chemokines.
Cytokine and chemokine secretion in cell supernatants was analyzed on the XMap Luminex 100 System using Bio-Plex Cytokine Assay (Bio-Rad, Stockholm, Sweden) including reagents for the detection of monocyte-derived IL-1β, IL-6, CXCL8 (IL-8), IL-10, IL-12p70, TNF, CCL2 (MCP-1), and CCL3 (MIP-1α) and also T-cell-associated IL-5 and interferon (IFN)-γ according to the manufacturer's instructions. Detection limits were 1 pg/mL for IL-1β, IL-6, CXCL8, IL-10, IL-12p70, and CCL3; 2 pg/mL for TNF; 0.8 pg/mL for IL-5; and 10 pg/mL for IFN-γ and CCL2. Data were analyzed with the software StarStation 2.0 (Applied Cytometry Systems, Sheffield, UK). As a control for the quality of the method, an LPS-stimulated whole blood cell supernatant sample from a blood donor was included in every assay. The coefficient of variance was <12%.
Analysis of phospholipids.
Total lipids from 200 μL freeze-dried plasma or serum were extracted three times according to Folch et al. (11) using 0.01% butylated hydroxytoluene (VWR) as an antioxidant. The lipids were evaporated with N2 and reconstituted in 0.4 mL chloroform. Lipid fractions were separated on an SEP-PAK aminopropyl cartridge (Waters Sverige AB, Sollentuna, Sweden). Total lipids were applied to cartridges preconditioned twice with 1 mL n-hexane. Neutral lipids and free fatty acids were eluted with chloroform:isopropanol 2:1 (vol/vol) and diethyl ether:acetic acid 98:2 (vol/vol), respectively, and discharged. The phospholipids were eluted with methanol and subsequently dried in N2 and transmethylated in methanolic-HCl 3 N (VWR) at 80°C for 4 h. The fatty acid methyl esters were extracted with n-hexane (VWR), washed with water and dried with water-free MgSO4 (VWR). Finally, the extractions were dried with N2 and reconstituted in 1.4 mL n-hexane Uvasol (VWR). The fatty acids methyl esters were separated by Agilent Technologies 6890N Network GC System gas chromatograph (Agilent Technologies, Stockholm, Sweden) equipped with a fused silica capillary column (45 m × 0.25 mm × 0.2 μm film thickness) (Supelco SP-2380, Sigma Chemical Co.-Aldrich). Helium was used as a carrier gas and the injection was splitless; injector and detector temperature was 250°C. Column oven temperature was increased 8°C/min from 60°C to 155°C, 1.5°C/min to 180°C, and 6°C/min to 230°C. The data were analyzed with Agilent Technologies Chemstation Software (Agilent Technologies). C21:0 methyl ester (Larodan, Malmö, Sweden) was used as an internal standard and the fatty acids methyl esters were identified by comparing with a known standard (Mixture Me 100, Larodan). The proportions were expressed as mol%. A serum sample from a blood donor was analyzed in every run as a quality control. The inter assay coefficient of variance was 3.5% for LA (C18:2 ω-6) and 7% for EPA (C20:5 ω-3).
Analysis of IgE antibodies.
The presence of maternal IgE to a panel of inhalant allergens was assessed with the ImmunoCAP 100 Phadiatop (Phadia, Uppsala, Sweden) according to the manufacturer's instructions.
Ethical aspects.
The study was approved by the Regional Ethics Board at the Faculty of Health Sciences, Linköping University, Linköping, Sweden and all families gave written informed consent.
Statistics.
Differences in fatty acid composition and baseline characteristics of the women in the ω-3 LCPUFA-treated group and the placebo group were analyzed by unpaired t test. PGE2, LTB4, cytokine, and chemokine data were not normally distributed, not even after logarithmic transformation, and were therefore analyzed with nonparametric tests. Mann Whitney U test was used for unpaired analyses and Wilcoxon signed rank test for paired analyses. Categorical variables were compared with the χ2-test and Spearman rank correlation was used to examine correlations between different parameters.
Samples with a concentration below the limit of detection were assigned a value corresponding to half the cutoff value. A difference together with a p value <0.05 was considered to be statistically significant, except for the analysis of cytokines and chemokines where differences were considered significant at a p value <0.01 as a consequence of multiple comparisons. Statistic analyses were performed using Stat View for Windows Version 5.9 (SAS Institute Inc., Cary, NC).
RESULTS
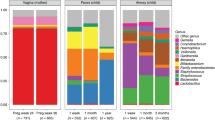
In women who received ω-3 LCPUFA, the relative proportion of EPA and DHA in serum/plasma phospholipids increased from gw 25 to 1 wk after partus. In contrast, the LA and AA proportions decreased and consequently the AA/EPA ratio decreased during the same period. Despite the presence of the ω-6 PUFA LA in the placebo capsules, the proportion of LA in the placebo group was not altered during supplementation, in contrast to the proportions of AA that increased (Table 2). The results were similar in both atopic and nonatopic mothers. The subgroup of 59 mothers, from whom whole blood cell cultures were established, displayed similar phospholipid fatty acid changes as those seen in the whole study group (data not shown).
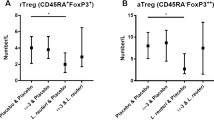
The mothers allocated to ω-3 fatty acids supplementation responded with higher LPS-induced PGE2 secretion from whole blood cell culture supernatants at inclusion compared with the mothers who were later treated with placebo (p = 0.01; Table 3). To overcome the influence of this random difference already present at inclusion, we chose to analyze the change in PGE2 secretion during supplementation, rather than the absolute levels. LPS-induced PGE2 secretion decreased during the supplementation period in a majority of the ω-3 LCPUFA-supplemented women but increased in the placebo-supplemented women (p = 0.002; Fig. 1A). The decrease in LPS-induced PGE2 secretion in the ω-3 LCPUFA-treated mothers was more pronounced among nonatopic mothers (Fig. 1B).
Changes in the LPS-induced PGE2 in whole blood cultures from gw 25 to 1 wk after partus in women treated with 2.7 g/d ω-3 fatty acids or 2.8 g/d placebo (soybean oil) from gw 25. The 10th, 25th, 50th, 75th, and 90th percentiles are indicated in the box plot. A, Nonparametric Wilcoxon signed rank test showed no differences in the ω-3 supplemented group but a significant increase in the placebo group, p < 0.001. PGE2 decreased in 18 of 28 (64%) of the ω-3 supplemented women and increased in 24 of 31 (77%) of the placebo-supplemented women; this difference was statistically significant with χ2, p = 0.002. B, The observed decrease in LPS-induced PGE2 secretion in the ω-3-supplemented group was more pronounced among nonatopic (4 of 5, 80%) than among atopic (11 of 16, 69%) mothers (ns).
The changes in LPS-induced PGE2 production during intervention correlated positively with changes in plasma phospholipid AA proportions (Fig. 2A) and negatively with changes in EPA, which was even stronger among the nonatopic (Fig. 2B). A positive correlation was also observed between changes in LPS-induced PGE2 secretion and changes in AA/EPA ratios (Fig. 2C).
Correlations between changes in serum/plasma PUFA phospholipids and changes in LPS-induced PGE2. Changes in serum/plasma phospholipid PUFA in pregnant women treated with 2.7 g/d ω-3 fatty acids (filled dots) or 2.8 g/d placebo (soybean oil) (open dots) from gw 25 to 1 after partus in correlation with changes in LPS-induced PGE2 from whole blood cultures. A, Changes in AA in relation to changes in PGE2, r* = 0.54 p < 0.001; B, Changes in EPA in relation to changes in PGE2, r* = −0.34 p = 0.011; C, Changes in AA/EPA ratio in relation to changes in PGE2, r* = 0.40, p = 0.002, *Spearman correlation.
Spontaneous secretion of PGE2, LTB4, and LPS-induced LTB4 secretion from whole blood culture supernatants were similar in the two groups both at inclusion and after intervention, and no change over time was observed in either group (data not shown). LTB4 secretion was enhanced by LPS stimulation (data not shown) but no difference was observed between the two groups (Table 3). Neither the dietary intervention (Table 3) nor the atopic status of the mother (data not shown) affected the cytokine and chemokine secretion from whole blood cultures with or without LPS. IL-5 was not detectable in cultures either with or without LPS.
DISCUSSION
In this study, we show that maternal serum/plasma phospholipid fatty acid proportions were altered by a ω-3 LCPUFA supplementation during pregnancy. Moreover, LPS-induced PGE2 secretion was decreased in a majority of the ω-3-supplemented women, in contrast to what was observed in the placebo group. This was most evident among nonatopic women. The secretions of LTB4, chemokines, and cytokines were not altered by the dietary intervention.
The maternal immune function can influence the immature immune system of the fetus, both transplacentally and later via the breast milk (as reviewed in Ref. 7). Normal pregnancy is associated with several signs of controlled inflammation and a predisposition toward Th2 immunity (12). The default Th2-skewed immunity of the fetus is probably caused by the high levels of the Th2 cytokine IL-4 and anti-inflammatory IL-10 in the fetomaternal interface (13). IL-4 promotes Th2 and counteracts Th1 differentiation, but the Th2 deviation is also possibly affected by the elevated levels of PGE2 associated with pregnancy (14). The surrounding cytokine and eicosanoid environment is crucial for the differentiation of naïve T cells.
Our study differs from some previous studies regarding ω-3 supplementation and immune responses as they were performed in men with cell cultures established on peripheral blood mononuclear cells (5,15,16). Previous studies in pregnant women supplemented with ω-3 LCPUFA were mainly focused on consequences for the child (17,18). However, there is one recently published report on the immunologic outcome for the mother after ω-3 LCPUFA supplementation from gw 22 (19) and yet another study on nonpregnant women was performed by Meydani et al. (5).
The effects of PGE2 in allergic inflammation are complex, both facilitating and hampering inflammatory reactions (reviewed in Refs. 20 and 21). On the one hand, PGE2 seems to facilitate sensitization as it inhibits the production of Th1 cytokines, primes immature T cells to produce IL-4 and IL-5, promotes a Th2 phenotype and facilitates B-lymphocyte immunoglobulin isotype switching to IgE (22). On the other hand, PGE2 has several anti-inflammatory properties including down-regulation of major histocompatibility complex class II molecules, protection from bronchoconstriction, reduction of tissue infiltration of eosinophils, and also inhibition of 5-lipoxygenase activity causing down-regulation of leukotriene production e.g. LTB4.
Despite small groups, we see a more pronounced although not significant reduction in PGE2 production among nonatopic than atopic women (Fig 1B). With our methods and in this study, we were not able to detect any differences in phospholipid fatty acids between atopic and nonatopic women to explain this discrepancy. A posterior power calculation based on maternal data of several serum/plasma fatty acids revealed that such a difference could not be expected within a study with this sample size. However, disturbed relationships within the individual fatty acids in human milk, related to atopic disease, have earlier been reported from our group (23). Xie and Innis (24) have recently shown that common genetic variations in the FADS1 FADS2 genes encoding for the Δ6 and Δ5 desaturases were associated with differences in ω-6 and ω-3 fatty acids in plasma and erythrocyte membrane lipids in gestation and in breast milk during lactation. Furthermore, a consequence of the genetic variability of several PUFAs could be an altered production of eicosanoids possibly having an impact on atopic disease risk as suggested by Schaeffer et al. (25).
Recognizing the difficulty in extrapolating findings from maternal peripheral circulation to fetal tissue, we still consider the maternal blood sample a mirror of the maternal immune milieu surrounding the fetus. We suggest that the lower maternal level of PGE2 after ω-3 LCPUFA supplementation gives a less Th2-like immune environment during fetal development and immune programming. This may contribute to a fetal immune system less prone to react in a way promoting the development of inflammatory diseases i.e. allergy.
Eicosanoids, cytokines, and chemokines are closely related in orchestrating immune responses (20). In the study by Meydani et al. six young, nonpregnant women aged between 23 and 33 y were supplemented with 2.4 g EPA and DHA daily for 3 mo. They found a 40%, reduction in PGE2 production from LPS-stimulated peripheral blood mononuclear cells, but this reduction was not statistically significant. They also reported a statistically significant reduction in mitogen-induced IL-1, IL-6, and TNF in peripheral blood mononuclear cell cultures (5). Krauss-Etschmann et al. (19) showed reduced mRNA levels of IL-1 and IFN-γ in unstimulated cells at delivery from women after ω-3 LCPUFA supplementation with 0.15 g EPA and 0.5 g DHA daily from gw 22. They did not report any data on eicosanoid secretion. Other studies, performed in men, report decreased production of various proinflammatory cytokines (15,16) and some state no effect (26) after ω-3 LCPUFA supplementation. The study by Blok et al. is similar to ours with respect to daily ω-3 LCPUFA dose and use of endotoxin-stimulated whole blood culture, but it was, however, performed in elderly monks.
ω-3 Fatty acid supplementation during pregnancy might theoretically be associated with complications, e.g. extended gestational length and excessive bleeding at delivery, to some extent due to alteration of eicosanoids production. The supplemented dose used in our study was based on an earlier study performed in pregnant women during late pregnancy (18) in which the fish oil supplementation seemed to prolong pregnancy but without detrimental effects on the course of labor or on the growth of the fetus. Likewise, we could not observe any adverse effects in the mothers participating in our study (Table 1).
The additional amount of EPA and DHA given in this study was 2.7 g/d. This is approximately 10 times the average daily dietary intake reported by the participating women at inclusion in the study, and also 10 times the average intake in Sweden (2). This caused a significant increase in both EPA and DHA proportions in serum/plasma phospholipids, a subsequent decrease in LA and AA proportions and consequently a reduction in the AA/EPA ratio. The supplement by soy bean oil in the placebo capsules corresponded to approximately one third of the daily LA intake (2). This did not alter the proportions of phospholipid LA in serum/plasma. However, the proportion of AA was significantly elevated in the placebo group 1 wk after partus compared with baseline. This is probably not due to the contribution of LA, because a previous study reporting supplementation with 10.9 g LA/d during pregnancy showed no impact on the AA proportions (27). Furthermore, the decreasing AA proportions during gestation have previously been reported to increase shortly after delivery also in women with no LCPUFA supplementation (28).
The LNA content of the placebo capsules is less than one fourth of the daily intake (2) but even this small amount may contribute to higher proportions of EPA and DHA. The conversion of LNA to EPA and DHA is estimated to vary from 0.2 to 6% in men; however, women of fertile age can have a substantially greater ability for conversion due to the effects of estrogen (29). We found equal proportions of LNA between the two groups after 15 wk of supplementation (Table 2). Therefore, we consider the LNA contribution in the placebo capsules to have negligible influence on the fatty acid composition.
There was no effect of the ω-3 LCPUFA intervention on the LPS-induced LTB4 production and no correlation between changes in AA and changes in LTB4 during treatment. Possibly, this can be explained by methodological limitations, because the interassay coefficient of variation was as high as 30%, thus potentially concealing any differences.
In conclusion, ω-3 LCPUFA supplementation during the last trimester dramatically decreases the AA/EPA ratio and a low ratio is associated with reduced secretion of proinflammatory and Th2-promoting PGE2, which in turn may contribute to an allergy-preventing effect.
Abbreviations
- AA:
-
arachidonic acid
- DHA:
-
docosahexaenoic acid
- EPA:
-
eicosapentaenoic acid
- gw:
-
gestational week
- LA:
-
linoleic acid
- LCPUFA:
-
long-chain polyunsaturated fatty acids
- LNA:
-
α-linolenic acid
- LPS:
-
lipopolysaccharide
- LTB4:
-
leukotriene B4
- PGE2:
-
prostaglandin E2
- PUFA:
-
polyunsaturated fatty acids
References
Simopoulos AP 1999 Essential fatty acids in health and chronic disease. Am J Clin Nutr 70: 560S–569S
Becker W 1999 Riksmaten 1997–98. Results from the questionnaire. We are eating healthier—but getting heavier. Vår föda 51: 3–7
Calder PC 2007 Immunomodulation by omega-3 fatty acids. Prostaglandins Leukot Essent Fatty Acids 77: 327–335
Calder PC 2006 n-3 Polyunsaturated fatty acids, inflammation, and inflammatory diseases. Am J Clin Nutr 83: 1505S–1519S
Meydani SN, Endres S, Woods MM, Goldin BR, Soo C, Morrill-Labrode A, Dinarello CA, Gorbach S 1991 Oral (n-3) fatty acid supplementation suppresses cytokine production and lymphocyte proliferation: comparison between young and older women. J Nutr 121: 547–555
Wong GW, Leung TF, Ma Y, Liu EK, Yung E, Lai CK 2007 Symptoms of asthma and atopic disorders in preschool children: prevalence and risk factors. Clin Exp Allergy 37: 174–179
Hanson LA, Korotkova M, Lundin S, Haversen L, Silfverdal SA, Mattsby-Baltzer I, Strandvik B, Telemo E 2003 The transfer of immunity from mother to child. Ann N Y Acad Sci 987: 199–206
Bonnelykke K, Pipper CB, Bisgaard H 2008 Sensitization does not develop in utero. J Allergy Clin Immunol 121: 646–651
Rowe J, Kusel M, Holt BJ, Suriyaarachchi D, Serralha M, Hollams E, Yerkovich ST, Subrata LS, Ladyman C, Sadowska A, Gillett J, Fisher E, Loh R, Soderstrom L, Ahlstedt S, Sly PD, Holt PG 2007 Prenatal versus postnatal sensitization to environmental allergens in a high-risk birth cohort. J Allergy Clin Immunol 119: 1164–1173
Dunstan JA, Mori TA, Barden A, Beilin LJ, Taylor AL, Holt PG, Prescott SL 2003 Maternal fish oil supplementation in pregnancy reduces interleukin-13 levels in cord blood of infants at high risk of atopy. Clin Exp Allergy 33: 442–448
Folch J, Lees M, Sloane Stanley GH 1957 A simple method for the isolation and purification of total lipids from animal tissues. J Biol Chem 226: 497–509
Sargent IL, Borzychowski AM, Redman CW 2006 NK cells and human pregnancy—an inflammatory view. Trends Immunol 27: 399–404
Wegmann TG, Lin H, Guilbert L, Mosmann TR 1993 Bidirectional cytokine interactions in the maternal-fetal relationship: is successful pregnancy a TH2 phenomenon?. Immunol Today 14: 353–356
Allen KG, Harris MA 2001 The role of n-3 fatty acids in gestation and parturition. Exp Biol Med (Maywood) 226: 498–506
Trebble T, Arden NK, Stroud MA, Wootton SA, Burdge GC, Miles EA, Ballinger AB, Thompson RL, Calder PC 2003 Inhibition of tumour necrosis factor-alpha and interleukin 6 production by mononuclear cells following dietary fish-oil supplementation in healthy men and response to antioxidant co-supplementation. Br J Nutr 90: 405–412
Trebble TM, Wootton SA, Miles EA, Mullee M, Arden NK, Ballinger AB, Stroud MA, Burdge GC, Calder PC 2003 Prostaglandin E2 production and T cell function after fish-oil supplementation: response to antioxidant cosupplementation. Am J Clin Nutr 78: 376–382
Dunstan JA, Mori TA, Barden A, Beilin LJ, Taylor AL, Holt PG, Prescott SL 2003 Fish oil supplementation in pregnancy modifies neonatal allergen-specific immune responses and clinical outcomes in infants at high risk of atopy: a randomized, controlled trial. J Allergy Clin Immunol 112: 1178–1184
Olsen SF, Sörensen JD, Secher NJ, Hedegaard M, Henriksen TB, Hansen HS, Grant A 1992 Randomised controlled trial of effect of fish-oil supplementation on pregnancy duration. Lancet 339: 1003–1007
Krauss-Etschmann S, Hartl D, Rzehak P, Heinrich J, Shadid R, Del Carmen Ramirez-Tortosa M, Campoy C, Pardillo S, Schendel DJ, Decsi T, Demmelmair H, Koletzko BV 2008 Decreased cord blood IL-4, IL-13, and CCR4 and increased TGF-beta levels after fish oil supplementation of pregnant women. J Allergy Clin Immunol 121: 464–470
Harizi H, Corcuff JB, Gualde N 2008 Arachidonic-acid-derived eicosanoids: roles in biology and immunopathology. Trends Mol Med 14: 461–469
Sala-Vila A, Miles EA, Calder PC 2008 Fatty acid composition abnormalities in atopic disease: evidence explored and role in the disease process examined. Clin Exp Allergy 38: 1432–1450
Roper RL, Brown DM, Phipps RP 1995 Prostaglandin E2 promotes B lymphocyte Ig isotype switching to IgE. J Immunol 154: 162–170
Duchen K, Yu G, Bjorksten B 1998 Atopic sensitization during the first year of life in relation to long chain polyunsaturated fatty acid levels in human milk. Pediatr Res 44: 478–484
Xie L, Innis SM 2008 Genetic variants of the FADS1 FADS2 gene cluster are associated with altered (n-6) and (n-3) essential fatty acids in plasma and erythrocyte phospholipids in women during pregnancy and in breast milk during lactation. J Nutr 138: 2222–2228
Schaeffer L, Gohlke H, Muller M, Heid IM, Palmer LJ, Kompauer I, Demmelmair H, Illig T, Koletzko B, Heinrich J 2006 Common genetic variants of the FADS1 FADS2 gene cluster and their reconstructed haplotypes are associated with the fatty acid composition in phospholipids. Hum Mol Genet 15: 1745–1756
Blok WL, Deslypere JP, Demacker PN, van der Ven-Jongekrijg J, Hectors MP, van der Meer JW, Katan MB 1997 Pro- and anti-inflammatory cytokines in healthy volunteers fed various doses of fish oil for 1 year. Eur J Clin Invest 27: 1003–1008
de Groot RH, Hornstra G, van Houwelingen AC, Roumen F 2004 Effect of alpha-linolenic acid supplementation during pregnancy on maternal and neonatal polyunsaturated fatty acid status and pregnancy outcome. Am J Clin Nutr 79: 251–260
Otto SJ, van Houwelingen AC, Badart-Smook A, Hornstra G 2001 Comparison of the peripartum and postpartum phospholipid polyunsaturated fatty acid profiles of lactating and nonlactating women. Am J Clin Nutr 73: 1074–1079
Burdge GC 2006 Metabolism of alpha-linolenic acid in humans. Prostaglandins Leukot Essent Fatty Acids 75: 161–168
Acknowledgements
We thank Lena Lindell, Kicki Helander, Nina Timelin, Linnea Andersson, Ammi Fornander, Katarina Dahlgren, Kalle Wahlin, and Ben Kersley for excellent care of the mothers, technical assistance, statistical, and language advice, respectively. We also thank Prof. Birgitta Strandvik and Mrs. Berit Holmberg, Department of Pediatrics, Institute of the Health of Women and Children, The Sahlgrenska Academy, University of Gothenburg, Gothenburg, for kindly providing the phospholipid fatty acids analysis technique. We also thank Pharma Nord, Denmark for supplying the capsules at a reduced cost.
Author information
Authors and Affiliations
Corresponding author
Additional information
Supported by grants from The Ekhaga Foundation, The Swedish Research Council FORMAS, The Research Council for the South-East of Sweden, Östergötland County Council, and The Swedish Asthma and Allergy Research Foundation.
Rights and permissions
About this article
Cite this article
Warstedt, K., Furuhjelm, C., Duchén, K. et al. The Effects of Omega-3 Fatty Acid Supplementation in Pregnancy on Maternal Eicosanoid, Cytokine, and Chemokine Secretion. Pediatr Res 66, 212–217 (2009). https://doi.org/10.1203/PDR.0b013e3181aabd1c
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/PDR.0b013e3181aabd1c
This article is cited by
-
Prenatal omega-3 LCPUFA and symptoms of allergic disease and sensitization throughout early childhood – a longitudinal analysis of long-term follow-up of a randomized controlled trial
World Allergy Organization Journal (2018)
-
Fish oil diet in pregnancy and lactation reduces pup weight and modifies newborn hepatic metabolic adaptations in rats
European Journal of Nutrition (2017)
-
Fishmeal supplementation during ovine pregnancy and lactation protects against maternal stress-induced programming of the offspring immune system
BMC Veterinary Research (2015)
-
Maternal fish consumption during pregnancy and risks of wheezing and eczema in childhood: The Generation R Study
European Journal of Clinical Nutrition (2013)
-
Increased linoleic acid/α-linolenic acid ratio in Swedish cord blood samples collected between 1985 and 2005
European Journal of Nutrition (2013)