Abstract
Obesity is associated with elevated blood pressure (BP), insulin resistance, and altered plasma adiponectin levels; the relationship between the biochemical features of obesity and 24-h ambulatory blood pressure (24-h ABP) parameters in adolescents remains unknown. Anthropometric measurements and 24-h ABP monitoring were obtained on 41 obese adolescents with and without type 2 diabetes mellitus (T2DM). Serum adiponectin, high sensitivity C-reactive protein (hs-CRP), lipid profile, insulin, fasting glucose, liver enzymes, Hb A1c (HbA1c), and two random urine samples were obtained for creatinine and microalbumin measurements. The determinants of 24-h systolic (SBP) and diastolic (DBP) BP were examined using multivariate linear regression models with BP parameters as outcome variables. Forty-one obese adolescents were studied. Adiponectin levels were reduced and hs-CRP levels were elevated, and were inversely and significantly correlated (rho = −0.3, p = 0.05). ABP showed blunted nocturnal SBP dipping. Twenty-four hour SBP and DBP indexes were significantly (p < 0.05) and inversely correlated with adiponectin (rho = −0.4 and −0.42), respectively. In multivariate models, lower adiponectin level was independently associated with 24-h SBP and DBP. Adiponectin inversely correlate with ABP parameters in obese adolescents. Larger studies are needed to examine the relationship between adiponectin and mechanisms of BP regulation.
Similar content being viewed by others
Main
Obesity in children continues to be a significant public health burden, with a >100% increase in the number of children diagnosed as being overweight in the past 30 y (1). The increasing prevalence of obesity has been accompanied by an increase in complications of obesity such as type 2 diabetes mellitus (T2DM). At our own institution, for example, we have observed a 10-fold increase in the number of pediatric patients with T2DM over the 10-y period from 1990 to 2000 (2). Blood pressure (BP) levels and the prevalence of hypertension in the young are also increasing, with the obesity epidemic responsible for much of the increase (3).
Obesity is accompanied by generalized inflammation, characterized by increased plasma C-reactive protein levels as well as by dysregulation of cytokine production by monocytes, lymphocytes, and other immune cells (4). Simultaneously, the presence of obesity has long been associated with the presence of endothelial and vascular dysfunction (5–7). Adipose tissue itself secretes several hormones, particularly leptin and adiponectin, and a variety of other proteins that are collectively known as adipokines. Unlike most adipokines, adiponectin expression and serum concentration are reduced in obesity, insulin resistance, and T2DM. Adiponectin levels are also modulated by the renin-angiotensin system (RAS). Its concentration is inversely correlated with other traditional cardiovascular (CV) risk factors, such as BP, low-density lipoprotein (LDL), and triglyceride (TG) levels (8,9). Furthermore, there is evidence that adiponectin may protect the endothelium via its insulin sensitizing, anti-inflammatory, antiatherogenic, antioxidant signals, and by impeding arterial wall thickening (10).
Adiponectin, a 30 kDa complement C1Q-related protein, also known as Acrp30, is the most abundant gene product secreted by fat cells of white adipose tissue. This 247 amino acid protein monomer forms trimers, which further polymerize into larger polymeric complexes varying in size between 180 kDa (hexameres; LMW) or 400-600 kDa (16-meres; HMW) (11). Adiponectin modulates several physiologic processes, such as metabolism of glucose and fatty acids, and immune responses. Decreased plasma adiponectin levels are associated with insulin resistance, T2DM, obesity, and atherosclerosis. Adiponectin has been associated with several other factors known to contribute to hypertension in obese individuals, including increased sympathetic nervous system and RAS activity, insulin resistance, elevated FFA and atherosclerosis and impaired vasoreactivity (12).
Our objective in this study was to determine whether plasma adiponectin and other inflammatory markers associated with obesity and insulin resistance are also associated with abnormal 24-h ambulatory blood pressure (ABP) patterns in obese adolescents.
MATERIALS AND METHODS
Setting and study design.
Patients who fulfilled the following criteria were recruited from the Pediatric Diabetes and Pediatric Nephrology Clinics at the Children's Hospital at Montefiore in the Bronx, NY: age 10-21 y, obesity defined as BMI >95% for age and gender (13), a diagnosis within the past 3 y of T2DM according to the standard American Diabetes Association criteria (14), and serum test results negative for antibodies to glutamic acid decarboxylase-65 or insulin autoantibodies. Obese nondiabetic subjects, defined as BMI >95% for age and gender, and normal glucose tolerance, were recruited from primary care, nephrology, and pediatric endocrinology clinics.
Patients with T2DM were ineligible when they were metabolically unstable, as defined by the history of an episode of diabetic ketoacidosis or of hospitalization for uncontrolled diabetes within the previous 2 mo. Patients with comorbid inflammatory disease, secondary hypertension, other endocrine disorders, or any genetic syndrome that would independently predispose them to either diabetes mellitus or to kidney disease were also excluded. Additionally, patients on treatment with insulin-sensitizing agents known to affect adiponectin levels (15), statins, and treatment with any antihypertensive medication including angiotensin-converting enzyme (ACE) inhibitors, angiotensin receptor blockers (ARB) were excluded.
Written informed consent was obtained from the parent or guardian of each subject. Subjects who were 13-21 y old also provided written informed consent. Written informed assent was obtained from children aged 10-13 y. The protocol was approved by the Montefiore Medical Center Institutional Review Board.
Study procedures and definitions.
Subjects had a study visit that included a history and a physical examination. Family health history, smoking status, and medication and vitamin usage were assessed. Families self-identified the race/ethnicity of the subject.
Anthropometric and body composition measurements were performed in the morning, before breakfast, with the subject wearing light clothing, without footwear. Body weight and standing height were measured by the same observer using a digital scale and a wall-mounted stadiometer to the nearest 0.1 kg and 0.5 cm, respectively. Waist and hip circumference was measured in a standard fashion (16) and the waist to hip ratio (WHR), was calculated as the ratio of waist and hip circumferences. BMI was calculated by dividing the weight in kilograms by the square of the height in meters, and was further used to calculate the BMI z score.
Three resting BP measurements were obtained from the right upper arm using an aneroid sphygmomanometer and appropriate size cuff (17). The first measurement was discarded and the average of the other two measurements was recorded as the study visit BP. Subjects were classified as having casual hypertension if this mean value was ≥95th percentile for age, gender, and height (17).
The subjects underwent a 24-h ABP recording using the Spacelabs 90217 ambulatory monitor (Spacelabs Medical, Issaquah, WA), fitted and programmed as previously described (18). Awake, or daytime, and sleep, or nocturnal, periods were determined by means of a diary provided by the subjects. Ambulatory hypertension was diagnosed when the average ambulatory BP for the period was ≥95th percentile BP on the basis of the subject's sex and height according to normative values for ABP (19). BP load was defined as the percentage of readings for a given period that exceeded the 95th percentile for that individual. A BP load >40% was considered to be elevated (20). Percent dipping was calculated for both average systolic (SBP) and diastolic BP (DBP) with the following formula: [(daytime BP−nocturnal BP)/daytime BP] × 100. Each subject was categorized as a “dipper” (decrease in average SBP and DBP ≥10% during sleep) or a “nondipper” (decrease <10%) (21). BP index (mean ambulatory BP divided by the 95th percentile for pediatric ambulatory BP) was calculated.
Fasting blood was drawn for adiponectin, glucose, insulin, liver enzymes, high sensitivity C-reactive protein (hs-CRP), creatinine, renin, aldosterone, HA1c, LDL, high-density lipoprotein, TG, and cholesterol levels. Urinary creatinine and microalbumin measurements were obtained from two random mid-stream urinary specimens obtained from all subjects. All tests except adiponectin measurement were performed in the Montefiore Medical Center's clinical laboratory.
The lipid panel and Hb A1c were interpreted according to the American Diabetes Association clinical practice recommendations (22). The remaining serum tests were compared with standardized normal values. Microalbuminuria was defined as an albumin-to-creatinine ratio ranging between 30 and 300 mg/g creatinine (23). Homeostasis model assessment of insulin resistance (HOMA-IR) was calculated using the formula [fasting serum insulin (uIU/mL) × fasting serum glucose (mg/dL)] × 0.002246 (24). The estimated glomerular filtration rate (eGFR) was calculated with the Schwartz formula (25).
Serum total adiponectin concentration (μg/mL) was measured at the Diabetes Research Center at the Albert Einstein College of Medicine using a commercially available radio immunoassay (Linco Research, St. Louis, MO). Blood samples obtained at the study visit were allowed to clot at room temperature for 30 min, then centrifuged at 4°C for 15 min at 2500 rpm. Serum was stored at −80°C until the day of measurement. The assay was carried out in duplicate at the same time in one batch to minimize interassay variability. The assay (26) has a sensitivity of 1 ng/mL. The interassay and the intra-assay coefficients are (1.78-6.21%) and 3.9%, respectively. To ensure reproducibility, samples were analyzed at two different occasions using the same technique. The correlation between results was 0.72, p < 0.01.
Data analysis.
Categorical variables are presented as relative frequencies, and their associations with obese subgroups were tested for significance using Fisher's exact tests. Continuous variables, not normally distributed, are presented as medians and interquartile ranges, and associations with subgroups were tested for significance using the Mann-Whitney tests. Normally distributed continuous variables are presented as means ± standard deviations, with differences between subgroups were assessed by two-tailed t tests. Bivariate correlations between various measures of BP indexes and adiponectin levels were examined using Spearman correlation.
Variables with significant correlations with the outcome variable (BP parameter) of magnitude 0.2 or greater were selected for the initial multivariate linear regression model, along with those variables considered clinically important or potential effect modifiers of adiponectin. Two multivariate regression models were derived to examine the relationships of adiponectin and other variables with outcomes: 1) 24-h mean SBP and 2) 24-h mean DBP. The confounding effects of gender and race (27–29) were examined, and were found not to be statistically significant. Female gender had a significantly negative correlation with SBP and remained in the model as an independent predictor.
Statistical and database software used included STATA 9.2 (Stata Corporation, College Station, TX) and Microsoft Office Excel 2003 (Microsoft Corporation, Redmond, WA), respectively. Statistical significance for all analyses was set at two-sided p < 0.05.
RESULTS
Study population.
Forty-one obese adolescents were studied, 15 of whom had T2DM (Table 1). Mean age was 14.2 ± 2.3 y (range, 10-20 y). Fifty-one person were male. Thirty-nine percent were African American and 61% were Hispanic. Mean BMI z score was 2.34 ± 0.32. Fifty-four percent, 19%, and 27% had casual BP in the hypertensive, prehypertensive, and normotensive range, respectively. Gender distribution between the two groups differed, with a significantly greater percentage of females in the T2DM group (p = 0.02). There were no significant differences between the groups in regard to age, eGFR, ethnicity, or prevalence of casual hypertension. Although BMI z score was not statistically different between the two groups, WHR was significantly greater in those with T2DM.
Biochemical parameters.
Compared with published normative data (29), adiponectin levels were reduced in our obese cohort (6.6 μg/mL ± 2.6); levels were lower but not significantly different in black adolescents compared with Hispanics, and in males compared with females. Adiponectin levels were significantly lower in obese adolescents with blunted SBP dipping compared with those with normal SBP dipping (5.96 ± 1.7 and 7.71 ± 3.5), respectively, p = 0.059. Obese diabetics tended to have lower adiponectin levels and statistically different HOMA, HbA1c, urinary microalbumin compared with obese nondiabetics (mean adiponectin levels 5.6 ± 2.0, 7.2 ± 2.8, respectively, p = 0.07). hsCRP levels were elevated in this cohort.
BP measurements and parameters.
Although 22 subjects (53.7%) were diagnosed to be hypertensive using casual BP readings, only 8 (19.5%) had ABP measurements above 95% for height and gender. Most subjects (82%) classified to have casual hypertension had systolic hypertension, 9% had diastolic hypertension, and 9% had both systolic and diastolic hypertension.
Twenty-one study participants (51%) and 11 (27%) had impaired SBP and DBP dipping, respectively. The mean SBP dipping was impaired in this obese cohort with a mean dip of just 8.7 ± 6.9%. Comparing 24-h ABP variables of obese diabetic to obese nondiabetic subgroup, only 24-h heart rate was statistically different (p = 0.04). A trend toward higher DBP parameters in the obese group with T2DM was observed.
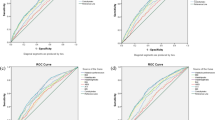
Table 2 presents bivariate correlations between adiponectin and various ABP parameters for this obese cohort. ABP parameters and indexes significantly correlated with adiponectin levels are presented. Similar statistically significant correlations were observed when these relationships were examined in each group separately (Figs. 1 and 2).
Determinants of 24-h SBP and DBP.
In a multivariable linear regression model, lower adiponectin and albumin levels; female gender; and higher hs-CRP and cholesterol levels were associated with higher 24-h SBP measurements. On the other hand, lower HOMA and adiponectin levels; and higher hs-CRP and HbA1c levels were associated with higher 24-h DBP, Table 3.
The two obese subgroups of this cohort were comparable in many demographic, biochemical, and BP parameters, and were treated as one group when building the regression models. Besides the known CV risk factors and the rapid phase reactants such as hs-CRP, albumin, cholesterol, and male gender shown in Table 3; 24-hr SBP, a reduction of 1.3 μg/mL in adiponectin level was associated with a 1 mm Hg increase in SBP.
Determinants of DBP included higher hs-CRP and AST, and lower adiponectin levels; a reduction of 0.7 μg/mL in adiponectin level was associated with a 1 mm Hg increase in DBP (Table 3; 24-hr DBP).
DISCUSSION
We demonstrate in this young cohort of obese adolescents with and without T2DM that adiponectin levels were independently associated with 24-h SBP and DBP. We also show that several adverse markers of CV risk, including impaired BP dipping, elevated hs-CRP levels, and reduced adiponectin levels affected both diabetic and nondiabetic obese adolescents almost to the same extent. Adiponectin levels were reduced, with no statistically significant difference between obese adolescents with or without T2DM. This might be due to the comparable demographics of the two subgroups, especially age, ethnicity, and BMI z scores, which are all known to affect adiponectin levels (25–27). Adiponectin levels also did not differ by gender in our study; this may be attributed to the morbid obesity and its independent effect on reduced adiponectin levels. In addition, gender was neither a confounding factor nor had an interaction with other variables and remained statistically significant in the 24-h SBP model.
The important role played by adiponectin in the pathogenesis of CV disease is highlighted by the relationships we found between ABP parameters and adiponectin. Adiponectin levels were decreased in adolescents with blunted SBP dipping compared with those without blunted dipping. This is consistent with previous data from Della et al. (30) showing lower adiponectin levels in nondippers. Other investigators (31) have examined the relationship between adiponectin and left ventricular mass index (LVMI) in an adult hypertensive population and showed that plasma adiponectin concentration in the hypertensive group was significantly lower than that in the nonhypertensive group, and that LVMI was significantly higher in the hypertensive group, with a significant inverse correlation between plasma adiponectin and LVMI. The significant potential CV risk of decreased adiponectin in obesity is further underscored by our finding that adiponectin was an independent determinant of 24-h SBP in this relatively young population.
Although BMI z score and WHR were significantly correlated in this study, WHR and not BMI z score was significantly different between the two obese groups, as the second reflects the relationship between height and weight whereas the first measures the proportion by which fat is distributed around the torso. In our study, BMI and WHR were inversely correlated to adiponectin levels and positively to BP levels, but did not reach sufficient significance to remain in the model.
Our study was limited by its small sample size; this may have affected which variables could be included in the final model based on their significance level. The cross-sectional study design, while demonstrating an independent association between adiponectin and systolic and diastolic ABP, does not allow a cause-and-effect relationship to be established. Additionally, the racial composition of the study population was limited to minorities, which may limit the generalizability of our findings. However, the study also has unique strengths, especially the use of ambulatory BP monitoring, which provides superior assessment of BP compared with office measurements (19). Additionally, using ABPM allowed us to show blunted SBP dipping, which may represent one of the earliest abnormalities in BP patterns in this obese cohort.
Adiponectin levels inversely correlate with ABP parameters in obese adolescents. Larger studies are needed to examine the relationship between adiponectin and mechanisms of BP regulation. In addition, further studies to examine interventions with potential BP lowering effect via modulating adiponectin levels are warranted.
Abbreviations
- ABPM:
-
ambulatory blood pressure monitoring
- BP:
-
blood pressure
- DBP:
-
diastolic BP
- HbA1c:
-
hemoglobin A1c
- hsCRP:
-
high sensitivity C-reactive protein
- HOMA:
-
homeostasis model assessment of insulin resistance
- LVMI:
-
left ventricular mass index
- SBP:
-
systolic BP
- TG:
-
triglycerides
- T2DM:
-
type 2 diabetes mellitus
- WHR:
-
waist to hip ratio
References
Rocchini AP 2002 Childhood obesity and a diabetes epidemic. N Engl J Med 346: 854–855
Grinstein G, Muzumdar R, Aponte L, Vuguin P, Saenger P, DiMartino-Nardi J 2003 Presentation and 5-year follow-up of type 2 diabetes mellitus in African-American and Caribbean-Hispanic adolescents. Horm Res 60: 121–126
Din-Dzietham R, Liu Y, Bielo MV, Shamsa F 2007 High blood pressure trends in children and adolescents in national surveys, 1963 to 2002. Circulation 116: 1488–1496
Ouchi N, Kihara S, Funahashi T, Matsuzawa Y, Walsh K 2003 Obesity, adiponectin and vascular inflammatory disease. Curr Opin Lipidol 14: 561–566
Fruhbeck G 2004 The adipose tissue as a source of vasoactive factors. Curr Med Chem Cardiovasc Hematol Agents 2: 197–208
Ekmekci H, Ekmekci OB 2006 The role of adiponectin in atherosclerosis and thrombosis. Clin Appl Thromb Hemost 12: 163–168
Matsuzawa Y 2006 The metabolic syndrome and adipocytokines. FEBS Lett 580: 2917–2921
Furuhashi M, Ura N, Higashiura K, Miyazaki Y, Murakami H, Hyakukoku M, Shimamoto K 2005 Low adiponectin level in young normotensive men with a family history of essential hypertension. Hypertens Res 28: 141–146
Matsuzawa Y 2005 Adiponectin: identification, physiology and clinical relevance in metabolic and vascular disease. Atheroscler Suppl 6: 7–14
Lam KS, Xu A 2005 Adiponectin: protection of the endothelium. Curr Diab Rep 5: 254–259
Koerner A, Kratzsch J, Kiess W 2005 Adipocytokines: leptin-the classical, resistin-the controversical, adiponectin-the promising, and more to come. Best Pract Res Clin Endocrinol Metab 19: 525–546
Rahmouni K, Correia ML, Haynes WG, Mark AL 2005 Obesity-associated hypertension: new insights into mechanisms. Hypertension 45: 9–14
Reilly JJ, Dorosty AR, Emmett PM 2000 Avon Longitudinal Study of Pregnancy and Childhood Study Team Identification of the obese child: adequacy of the body mass index for clinical practice and epidemiology. Int J Obes Relat Metab Disord 24: 1623–1627
American Diabetes Association 2003 Standards of medical care for patients with diabetes mellitus. Diabetes Care 26: S33–S50
Raji A, Seely EW, Bekins SA, Williams GH, Simonson DC 2003 Rosiglitazone improves insulin sensitivity and lowers blood pressure in hypertensive patients. Diabetes Care 26: 172–178
Khaodhiar L, Blackburn GL 2001 Results of expert meetings: obesity and cardiovascular disease. Obesity assessment. Am Heart J 142: 1095–1101
National High Blood Pressure Education Program Working Group on High Blood Pressure in Children and Adolescents 2004 The fourth report on the diagnosis, evaluation, and treatment of high blood pressure in children and adolescents. Pediatrics 114: 555–576.
Ettinger LM, Freeman K, DiMartino-Nardi JR, Flynn JT 2005 Microalbuminuria and abnormal ABP in adolescents with type 2 diabetes mellitus. J Pediatr 147: 67–73
Urbina E, Alpert B, Flynn J, Hayman L, Harshfield GA, Jacobson M, Mahoney L, McCrindle B, Mietus-Snyder M, Steinberger J, Daniels S 2008 ABP monitoring in children and adolescents: recommendations for standard assessment. A Scientific Statement From the American Heart Association Atherosclerosis, Hypertension, and Obesity in Youth Committee of the Council on Cardiovascular Disease in the Young and the Council for High Blood Pressure Research. Hypertension 52: 433–451
White WB, Dey HM, Schulman P 1989 Assessment of the daily blood pressure load as a determinant of cardiac function in patients with mild-to-moderate hypertension. Am Heart J 118: 782–795
Verdecchia P, Schillaci G, Guerrieri M, Gatteschi C, Benemio G, Boldrini F, Porcellati C 1990 Circadian blood pressure changes and left ventricular hypertrophy in essential hypertension. Circulation 81: 528–536
American Diabetes Association 2005 Standards of medical care in diabetes. Diabetes Care 28: S4–S36
Babazono T, Takahashi C, Iwamoto Y 2004 Definition of microalbuminuria in first-morning and random spot urine in diabetic patients. Diabetes Care 27: 1838–1839
Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC 1985 Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia 28: 412–419
Schwartz GJ, Haycock GB, Edelmann CM Jr, Spitzer A 1976 A simple estimate of glomerular filtration rate in children derived from body length and plasma creatinine. Pediatrics 58: 259–263
Yildiz BO, Suchard MA, Wong ML, McCann SM, Licinio J 2004 Alterations in the dynamics of circulating ghrelin, adiponectin, and leptin in human obesity. Proc Natl Acad Sci USA 101: 10434–10439
Bacha F, Saad R, Gungor N, Arslanian SA 2005 Does adiponectin explain the lower insulin sensitivity and hyperinsulinemia of African-American children?. Pediatr Diabetes 6: 100–102
Bottner A, Kratzsch J, Muller G, Kapellen TM, Bluher S, Keller E, Bluher M, Kiess W 2004 Gender differences of adiponectin levels develop during the progression of puberty and are related to serum androgen levels. J Clin Endocrinol Metab 89: 4053–4061
Butte NF, Comuzzie AG, Cai G, Cole SA, Mehta NR, Bacino CA 2005 Genetic and environmental factors influencing fasting serum adiponectin in Hispanic children. J Clin Endocrinol Metab 90: 4170–4176
Della Mea P, Lupia M, Bandolin V, Guzzon S, Sonino N, Vettor R, Fallo F 2005 Adiponectin, insulin resistance, and left ventricular structure in dipper and nondipper essential hypertensive patients. Am J Hypertens 18: 30–35
Hong SJ, Park CG, Seo HS, Oh DJ, Ro YM 2004 Associations among plasma adiponectin, hypertension, left ventricular diastolic function and left ventricular mass index. Blood Press 13: 236–242
Author information
Authors and Affiliations
Corresponding author
Additional information
Supported by The Kidney and Urology Foundation of America grant number 4272387 (I.F.S.).
Rights and permissions
About this article
Cite this article
Shatat, I., Freeman, K., Vuguin, P. et al. Relationship Between Adiponectin and Ambulatory Blood Pressure in Obese Adolescents. Pediatr Res 65, 691–695 (2009). https://doi.org/10.1203/PDR.0b013e31819ea776
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/PDR.0b013e31819ea776
This article is cited by
-
Plasma Sfrp5 and adiponectin levels in relation to blood pressure among obese children
Journal of Human Hypertension (2017)
-
Circadian and ultradian cardiovascular rhythmicity in obese children
European Journal of Pediatrics (2016)
-
Association of adiponectin and metabolic syndrome in adolescents: the caspian- III study
Journal of Diabetes & Metabolic Disorders (2015)
-
Correlation between adipocytokines and AGE products in diabetic and non-diabetic patients with myocardial infarction
Research on Chemical Intermediates (2015)