Abstract
Premature newborn baboons [125 d (67%) gestation], exposed to a moderate-size patent ductus arteriosus (PDA) [pulmonary-to-systemic blood-flow-ratio (Qp/Qs) = 1.8] for 14 d, have impaired pulmonary function and arrested alveolar development and surface area when compared with age matched fetuses (140 d gestation). Pharmacologic closure of the PDA reduces the detrimental effects of preterm delivery on pulmonary function and surface area. We used preterm baboons (delivered at 125 d gestation and ventilated for 14 d) to study the effects of surgical PDA ligation on pulmonary function and alveolar surface area. After ligation (on day of life 6), ligated animals had lower Qp/Qs ratios [Qp/Qs (ligated, n = 10) = 1.00 ± 0.04; (nonligated, n = 12) = 2.05 ± 0.17; mean ± SD] and higher systemic blood pressures than nonligated control animals. Ventilation and oxygenation indices did not differ between the groups, during either the pre- or postoperative periods. Alveolar surface area measurements were made by digital image analysis and compared with measurements made from fetal lungs at 125 d (n = 6) and 140 d (n = 7) gestation. PDA ligation failed to improve the postnatal arrest in alveolar surface area. In contrast with pharmacologic closure of the PDA, surgical closure failed to improve either pulmonary function or alveolar surface area in baboons with a moderate PDA shunt.
Similar content being viewed by others
Main
Lung injury, superimposed on an immature lung, leads to bronchopulmonary dysplasia (BPD). BPD is now characterized primarily by impaired alveolar and vascular growth, rather than by extensive fibrosis, smooth muscle proliferation, and regional heterogeneity (1). A persistent patent ductus arteriosus (PDA) has been shown to impair pulmonary mechanics (2–4) and prolong the need for mechanical ventilation (5). Although numerous studies have found an association between the presence of a PDA and the development of BPD, there is little available information to indicate whether this is a cause-and-effect relationship (6,7). Most of the controlled clinical trials examining PDA treatments were not specifically designed to address this issue; nor has there been an appropriate animal model to test the hypothesis (8–10).
The premature baboon, delivered at 125 d gestation (67% of gestation, term = 185 d) has recently been used to explore the causes of BPD. The premature baboon has a similar neonatal course as the premature human delivered between 26 and 27 wk of gestation (11): they both develop respiratory distress and fail to close their PDA after birth. Despite antenatal glucocorticoids, surfactant treatment, total parenteral nutrition, low tidal volume ventilation, and low supplemental oxygen administration during the first 2 wk after delivery, premature baboons develop pulmonary histopathologic changes that are similar to those described in premature human infants with BPD (1,12).
Using this model, we have examined the effects of pharmacologic closure of a PDA (with ibuprofen) on the development of BPD (13). Ibuprofen decreased left-to-right ductus shunt and improved pulmonary compliance and ventilation indices. Ibuprofen treatment also had beneficial effects on lung morphology in the preterm newborn baboon. Digital image analysis showed significant improvement in alveolar surface area in ibuprofen-treated animals compared with control animals (that did not receive ibuprofen, and that had a persistent PDA during the first 2 wk after delivery) (13).
In the study reported below, we examined whether ductus ligation at 6 d after birth produced similar beneficial effects on lung development. Lungs obtained from premature baboons, mechanically ventilated during the first 2 wk after delivery, were examined by the same digital image analysis techniques that were used in the previous ibuprofen-treatment study (13). We found that, in contrast with pharmacologic closure with ibuprofen, surgical closure of the PDA offered no benefit for either pulmonary function or for alveolar development during the first 2 wk after delivery.
METHODS
Studies were performed at the Southwest Foundation for Biomedical Research Primate Center in San Antonio, TX and were approved by the Committee on Animal Research. A complete description of the details of animal care and the surgical procedures have been published elsewhere (1,12,14) (see also online data supplement for Refs. 1,12,14). Briefly, timed pregnant baboon (Papio papio) dams were delivered at 125 ± 1 d gestation (full term = 185 d) and their newborns were mechanically ventilated for 14 d. The dams did not receive antenatal glucocorticoids. At birth, the infants were weighed, sedated, intubated, and given surfactant (Survanta, courtesy of Ross Laboratories, Columbus, OH) before initiation of ventilator support (InfantStar, Infrasonics, San Diego, CA). Ventilator adjustments were made based on chest radiograph, clinical examination, arterial blood gas measurement, and tidal volume measurement (12). Target goals for PaO2 were 55–70 mm Hg, for PaCO2 45–55 mm Hg, and for tidal volume 4–6 mL/kg. Nutritional, fluid, transfusion, antibiotic, and blood pressure management have been previously described (12). None of the animals received postnatal steroids.
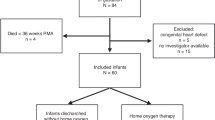
Animals were randomized before delivery to either ductal ligation (ligation) at 6 d after birth or no intervention (control). This time point was chosen because the animals are relatively stable from a cardiopulmonary standpoint (see Fig. 1) and because previous experience has shown that the animals do not tolerate the surgery before day of life 5–6. Animals in the ligation group underwent ductus ligation, using standard surgical techniques, after induction of anesthesia with ketamine (10 mg/kg), and fentanyl (20 μg/kg), and muscle relaxation with pavulon (0.1 mg/kg). Animals in the control group did not receive anesthesia or sham surgery because our intention was to mimic the clinical care of human newborns.
Comparison of indices of (A) pulmonary-to-systemic blood flow ratio (Qp/Qs), (B) mean systemic blood pressure (mean BP), (C) ventilation index (VI), (D) dynamic compliance per kilogram body weight, (E) oxygenation index (OI), and (F) fluid intake and urine (fluid) output, in control (n = 12) and ligation (n = 10) groups. Values are mean ± SD. Values between the study groups were similar before the day of ligation (day 6). After the ligation, Qp/Qs (p < 0.001, on days 7–14, ANOVA) and mean BP values (p < 0.001, on days 7–14, ANOVA) were significantly different between the study groups. VI, OI, Compliance, fluid intake, and fluid output were not significantly different between the study groups. Vertical arrow indicates the day of ligation.
We studied the newborns for the first 14 d after birth since beyond 14 d there is a high likelihood that the animals would develop septicemia or pneumonia (1). Because sepsis plays a significant role in the development of chronic lung disease in the preterm, the presence of septicemia or pneumonia in the animals would significantly alter our ability to detect differences due to other interventions. X-rays were obtained daily and surveillance cultures were obtained while the animals were alive; histologic examinations were performed at necropsy. None of the animals in the control or ligation groups developed septicemia or pneumonia during the study period.
Pulmonary function testing was performed using the VitalTrends plethysmograph system (VT1000, Vitaltrends Technology, New York, NY). The reproducibility and sensitivity of this system has been described previously (12). Compliance measurements were of the respiratory system as a whole and were corrected for body weight. Oxygenation index [=mean airway pressure (cm H2O) × FiO2 × 100/PaO2] and ventilation index (=peak inspiratory pressure × ventilator rate × PaCO2/1000) were calculated at the same times.
A complete echocardiographic exam, including assessment of ductal patency, was performed daily using an 8-mHz transducer interfaced with a Biosound AU3 echocardiographic system (Genoa, Italy) (15,16).
Findings in these study animals related to the clinical course, cardiovascular performance, and proinflammatory cytokines have been published elsewhere (14).
Control fetuses.
Lung tissue was also obtained from 125-d gestation fetuses and from fetuses (140-d gestation) that remained in utero for the equivalent 14-d newborn experimental period. Fetuses were delivered by cesarean section and euthanized before breathing.
Lung morphometry and digital image analysis.
At necropsy, the right lower lobe was removed, weighed, and intrabronchially fixed with phosphate-buffered 4% paraformaldehyde at 20 cm H2O constant pressure for 24 h. After fixation, the volume of the right lower lobe was determined by volume displacement and subsequently processed for light microscopy (12). The right lower lobe was cut into four pieces of equal thickness. Tissue sections from each of the right lower lobe pieces were obtained following a stratified random sampling procedure and 27–33 sections were photographed with a ×10 objective (17).
Digital image analysis of the gray-scale photographs was performed by adapting the algorithm of Tschanz and Burri (18) into a macro for ImagePro 5.0 (Media Cybernetics, Silver Spring, MD). Each photographic image was processed with the macro to thin, or skeletonize, the alveolar septa on the two-dimensional section into a network of lines that were a single pixel in thickness (18). The number and length of primary septal segments and secondary crests were tallied and summed to obtain the total alveolar surface area for the right lower lobe (19).
Statistics.
Our sample size was limited both by the expense of the model and our attempt to limit the use of this precious animal resource. In our previous study, we detected a significant increase in alveolar surface area (an increase of 364 cm2, or 26%, compared with fetal controls) in animals treated with ibuprofen to close their PDA (13). We used a larger number of newborn animals in the current study, and calculated that this number of animals should enable us to detect an increase in alveolar surface area of 240 cm2 (or 17%) with a two-sided significance level of 5%, and a probability of 80%.
Data are presented as mean ± SD. Between groups differences were compared by analysis of variance (ANOVA), unpaired t test, or the Mann-Whitney rank sum test were appropriate. Statistical results were generated using Statview (SAS Institute, San Francisco) software.
RESULTS
Twenty-two newborn animals (control = 12, ligation = 10) were ventilated for 14 d. All animals had a patent ductus on day 6 (the day of planned ductus ligation). There were no differences between the 2 groups in birth weight (control = 403 ± 13, ligation = 405 ± 13 g), sex (% male: control = 58%, ligation = 70%), gestation (control = 125 ± 1, ligation = 125 ± 1 d), or in any of the measured parameters before the time of planned ductus ligation (day 6) (see below).
Before ductus ligation, both groups had similar systemic blood pressures and similar degrees of left-to-right PDA shunt [as reflected by the pulmonary-to-systemic blood flow ratios (Qp/Qs)] (Fig. 1). The ductus in the control group stayed open throughout the 14-d experiment; the average Qp/Qs ratio for the control group fluctuated between 1.7 and 2.3 from days 7 through 13 (average Qp/Qs ratio = 2.05 ± 0.17) (Fig. 1). Animals in the ligation group had higher mean systemic blood pressures (Fig. 1B), and higher systolic and diastolic pressures (data not shown) at all times after the ligation. There were no differences in the fluid intake and urine output between the two groups (Fig. 1); nor were there differences between the two groups in base deficit, serum bicarbonate, or need for dopamine/dobutamine administration during the 14-d treatment course (data not shown).
There were no differences in ventilation index, dynamic compliance, or oxygenation index between the two groups, during both the preoperative and postoperative periods (Fig. 1).
At necropsy, there were no differences in the histopathologic findings between the two groups. Both groups exhibited varying degrees of inflation. Atelectasis was usually associated with the presence of mucus plugs in a few bronchiolar lumens. In the regions with well-inflated parenchyma, the saccular walls were dilated and few secondary crests/alveoli were evident. Bronchopneumonias and septic emboli were not identified. Airway and vascular lesions were not evident.
We performed digital image analysis to obtain the total alveolar surface area for the right lower lobe [using the algorithm of Tschanz and Burri (18)]. The total alveolar surface area increased significantly with advancing gestation (compare 140-d gestation fetal lung with 125-d gestation fetal lung) (Fig. 2). In contrast, there was no increase in the total alveolar surface area if the fetuses were delivered prematurely and ventilated for 14 d (Fig. 2). Furthermore, ductus ligation did not lead to an increase in total alveolar surface area (Fig. 2). The lack of impact of ductus ligation on alveolar surface area contrasts with the previously reported increase in alveolar surface area observed with ibuprofen treatment (13) (Fig. 2).
Digital image analysis of total alveolar surface area of the right lower lobe in fetuses (125 and 140 d gestation) and 14-d-old premature newborn baboons (see Methods section). Values are mean ± SD, n = number of animals. *p < 0.05, groups compared with the 125-d gestation fetus. †p < 0.05, groups compared with the 140-d gestation fetus. (A) Total alveolar surface area in fetuses (125 and 140 d gestation) and 14-d-old premature newborns [with an open ductus (Nb cont) or a ligated ductus (Nb ligat)]. Total alveolar surface area increased with advancing gestation (compare 125 d fetus with 140 d fetus). There was no increase in surface area after 14 d in preterm newborns with either an open ductus or a ligated ductus. (B) Data extrapolated from previously reported experiments (13) using fetuses (125 and 140 d gestation) and 14-d-old premature newborns [with an open ductus (Nb cont) or a ductus that was closed with ibuprofen (Nb ibup)]. In this set of experiments, there was an increase in surface area (compared with 125 d gestation fetuses) when ibuprofen was used to close the preterm newborn ductus (Nb ibup).
DISCUSSION
Premature newborn baboons, exposed to a moderate-size PDA shunt for 2 wk, have decreased pulmonary function and arrested alveolar development (13) (Fig. 2). We previously found that pharmacologic closure of the PDA, with ibuprofen, prevented the deterioration in both pulmonary function and alveolar development (Fig. 2) (13). In contrast, we found that surgical ligation of the PDA did not alter pulmonary mechanics or the evolution of histologic BPD during the first 2 wk after birth. We used the same digital imaging techniques to evaluate alveolar surface area that we used in the prior ibuprofen-treatment study (13).
It is possible that the trauma of surgical ligation, itself, will have obscured the effects of PDA closure on postnatal lung development. Airway aspirates from infants that develop BPD contain proinflammatory cytokines/chemokines (like IL-6 and IL-8) during the first days after delivery (20–25). Premature delivery and mechanical ventilation of preterm baboons have also been shown to increase proinflammatory cytokines/chemokines (1,12,13). However, in studies we have previously reported, IL-6 and IL-8 expression did not seem to differ between control animals (with a PDA) and those with a surgically ligated ductus (14).
It is possible that differences in alveolar development, between the control and ligation groups, may have been more apparent if the animals had been exposed to larger left-to-right PDA shunts (Qp/Qs > 3:1). However, in our previous study, significant improvement in alveolar development occurred even after similar size PDA shunts (Qp/Qs = 1.8 ± 0.2) were closed pharmacologically (Fig. 2) (13).
In the ibuprofen-treatment experiments, ibuprofen was started at 24 h after birth and ductus closure occurred on day 3 (13). In contrast, in the current experiments, surgical closure was not performed until day 6 (because preterm baboons do not tolerate surgery before this time). It is possible that the 3 extra days of exposure to the left-to-right PDA shunt in our current experiments will have contributed to the lack of improvement in alveolar growth in the ligated animals.
At this time, it is unclear whether the beneficial effects of ibuprofen are due to its effect on the ductus left-to-right shunt or are due to some other pharmacologic effect that might promote alveolarization. It is worth noting that ibuprofen-induced ductus closure, like surgical ductus ligation, did not seem to affect the expression of IL-6 or IL-8 (the cytokines most commonly associated with the development of BPD in this model) (13).
Our findings are consistent with the limited amount of data available from clinical studies. There is little evidence to suggest that surgical ductus closure prevents the evolution of BPD (26). If anything, recent population-based, observational studies have suggested just the opposite, namely, that surgical ligation may act as an independent risk factor for the development of BPD (9,27). In the only published controlled trial to compare pharmacologic closure of the PDA with surgical ligation (28), infants that were treated pharmacologically with indomethacin required shorter durations of CPAP than those treated surgically (p = 0.06).
Ductus ligation is associated with several known morbidities: thoracotomy, postoperative myocardial dysfunction (29), hypotension (30), pneumothorax, chylothorax, infection, and vocal cord paralysis (8,30); neonatal transport to another facility may be required if surgical expertise is not readily available. In sum, ductus ligation, while eliminating one potential cause for neonatal morbidity, may introduce another set of problems. We suggest that a careful evaluation of both the desired and achievable goals of ductus ligation be performed before committing infants to routine or early surgical closure.
Abbreviations
- BPD:
-
bronchopulmonary dysplasia
- PDA:
-
patent ductus arteriosus
- Qp/Qs:
-
pulmonary to systemic blood flow ratio
References
Coalson JJ, Winter VT, Siler-Khodr T, Yoder BA 1999 Neonatal chronic lung disease in extremely immature baboons. Am J Respir Crit Care Med 160: 1333–1346
Stefano JL, Abbasi S, Pearlman SA, Spear ML, Esterly KL, Bhutani VK 1991 Closure of the ductus arteriosus with indomethacin in ventilated neonates with respiratory distress syndrome. Effects of pulmonary compliance and ventilation. Am Rev Respir Dis 143: 236–239
Szymankiewicz M, Hodgman JE, Siassi B, Gadzinowski J 2004 Mechanics of breathing after surgical ligation of patent ductus arteriosus in newborns with respiratory distress syndrome. Biol Neonate 85: 32–36
Barlow AJ, Ward C, Webber SA, Sinclair BG, Potts JE, Sandor GG 2004 Myocardial contractility in premature neonates with and without patent ductus arteriosus. Pediatr Cardiol 25: 102–107
Cotton RB, Stahlman MT, Berder HW, Graham TP, Catterton WZ, Kover I 1978 Randomized trial of early closure of symptomatic patent ductus arteriosus in small preterm infants. J Pediatr 93: 647–651
Rojas MA, Gonzalez A, Bancalari E, Claure N, Poole C, Silva-Neto G 1995 Changing trends in the epidemiology and pathogenesis of neonatal chronic lung disease. J Pediatr 126: 605–610
Marshall DD, Kotelchuck M, Young TE, Bose CL, Kruyer L, O'Shea TM 1999 Risk factors for chronic lung disease in the surfactant era: a North Carolina population-based study of very low birth weight infants. North Carolina Neonatologists Association. Pediatrics 104: 1345–1350
Clyman RI, Chorne N 2007 Patent ductus arteriosus: evidence for and against treatment. J Pediatr 150: 216–219
Chorne N, Leonard C, Piecuch R, Clyman RI 2007 Patent ductus arteriosus and its treatment as risk factors for neonatal and neurodevelopmental morbidity. Pediatrics 119: 1165–1174
Laughon MM, Simmons MA, Bose CL 2004 Patency of the ductus arteriosus in the premature infant: is it pathologic? Should it be treated?. Curr Opin Pediatr 16: 146–151
Clyman RI, Chan CY, Mauray F, Chen YQ, Cox W, Seidner SR, Lord EM, Weiss H, Wale N, Evan SM, Koch CJ 1999 Permanent anatomic closure of the ductus arteriosus in newborn baboons: the roles of postnatal constriction, hypoxia, and gestation. Pediatr Res 45: 19–29
Yoder BA, Siler-Khodr T, Winter VT, Coalson JJ 2000 High-frequency oscillatory ventilation: effects on lung function, mechanics, and airway cytokines in the immature baboon model for neonatal chronic lung disease. Am J Respir Crit Care Med 162: 1867–1876
McCurnin DC, Seidner S, Chang LY, Waleh N, Ikegami M, Petershack JA, Yoder BA, Giavedoni L, Albertine KH, Dahl MJ, Wang ZM, Clyman R Ibuprofen-induced ductus arteriosus closure: physiological, histological and biochemical effects on the premature lung. Pediatrics (in press)
McCurnin DC, Yoder BA, Coalson J, Grubb P, Kerecman J, Kupferschmid J, Breuer C, Siler-Khodr T, Shaul PW, Clyman R 2005 Effect of ductus ligation on cardiopulmonary function in premature baboons. Am J Respir Crit Care Med 172: 1569–1574
Seidner SR, Chen Y-Q, Oprysko PR, Mauray F, Tse MM, Lin E, Koch C, Clyman RI 2001 Combined prostaglandin and nitric oxide inhibition produces anatomic remodeling and closure of the ductus arteriosus in the premature newborn baboon. Pediatr Res 50: 365–373
Yoder B, Martin H, McCurnin DC, Coalson JJ 2002 Impaired urinary cortisol excretion and early cardiopulmonary dysfunction in immature baboons. Pediatr Res 51: 426–432
Chang LY, Subramaniam M, Yoder BA, Day BJ, Ellison MC, Sunday ME, Crapo JD 2003 A catalytic antioxidant attenuates alveolar structural remodeling in bronchopulmonary dysplasia. Am J Respir Crit Care Med 167: 57–64
Tschanz SA, Burri PH 2002 A new approach to detect structural differences in lung parenchyma using digital image analysis. Exp Lung Res 28: 457–471
McCurnin DC, Pierce RA, Chang LY, Gibson LL, Osborne-Lawrence S, Yoder BA, Kerecman JD, Albertine KH, Winter VT, Coalson JJ, Crapo JD, Grubb PH, Shaul PW 2005 Inhaled NO improves early pulmonary function and modifies lung growth and elastin deposition in a baboon model of neonatal chronic lung disease. Am J Physiol Lung Cell Mol Physiol 288: L450–L459
Naik AS, Kallapur SG, Bachurski CJ, Jobe AH, Michna J, Kramer BW, Ikegami M 2001 Effects of ventilation with different positive end-expiratory pressures on cytokine expression in the preterm lamb lung. Am J Respir Crit Care Med 164: 494–498
Speer CP 2006 Inflammation and bronchopulmonary dysplasia: a continuing story. Semin Fetal Neonatal Med 11: 354–362
Kotecha S, Wilson L, Wangoo A, Silverman M, Shaw RJ 1996 Increase in interleukin (IL)-1 beta and IL-6 in bronchoalveolar lavage fluid obtained from infants with chronic lung disease of prematurity. Pediatr Res 40: 250–256
Tullus K, Noack GW, Burman LG, Nilsson R, Wretlind B, Brauner A 1996 Elevated cytokine levels in tracheobronchial aspirate fluids from ventilator treated neonates with bronchopulmonary dysplasia. Eur J Pediatr 155: 112–116
Groneck P, Gotze-Speer B, Oppermann M, Eiffert H, Speer CP 1994 Association of pulmonary inflammation and increased microvascular permeability during the development of bronchopulmonary dysplasia: a sequential analysis of inflammatory mediators in respiratory fluids of high-risk preterm neonates. Pediatrics 93: 712–718
Ikegami M, Jobe AH 2002 Postnatal lung inflammation increased by ventilation of preterm lambs exposed antenatally to Escherichia coli endotoxin. Pediatr Res 52: 356–362
Cassady G, Crouse DT, Kirklin JW, Strange MJ, Jonier CH, Godoy G, Odrezin GT, Cutter GR, Kirklin JK, Pacifico AD, Collins MV, Lell WA, Satterwhite C, Philips JB 1989 A randomized, controlled trial of very early prophylactic ligation of the ductus arteriosus in babies who weighed 1000 g or less at birth. N Engl J Med 320: 1511–1516
Kabra NS, Schmidt B, Roberts RS, Doyle LW, Papile L, Fanaroff A, Trial of Indomethacin Prophylaxis in Preterms Investigators 2007 Neurosensory impairment after surgical closure of patent ductus arteriosus in extremely low birth weight infants: results from the Trial of Indomethacin Prophylaxis in Preterms. J Pediatr 150: 229–234, 234 e1
Gersony WM, Peckham GJ, Ellison RC, Miettinen OS, Nadas AS 1983 Effects of indomethacin in premature infants with patent ductus arteriosus: results of a national collaborative study. J Pediatr 102: 895–906
Noori S, Friedlich P, Seri I, Wong P 2007 Changes in myocardial function and hemodynamics after ligation of the ductus arteriosus in preterm infants. J Pediatr 150: 597–602
Moin F, Kennedy KA, Moya FR 2003 Risk factors predicting vasopressor use after patent ductus arteriosus ligation. Am J Perinatol 20: 313–320
Acknowledgements
We thank all the personnel who support the BPD Resource Center: the animal husbandry group led by Drs. D. Carey and M. Leland, the NICU staff (H. Martin, D. Correll, L. Kalisky, L. Nicley, R. Degan, S. Salazar, S. Ali), Deborah Catland, N.N.P., and the Wilford Hall Medical Center neonatal fellows who assist in the care of the animals, and the UTHSCSA pathology staff (L. Buchanan, K. Symank, Y. Valdes and K. Mendoza) who perform necropsies. Francoise Mauray performed the artwork. We would especially thank Vickie Winter, who has skillfully managed to categorize and keep track of all the tissue samples and animal data over the years and Dr. Jackie Coalson, who provided invaluable leadership, guidance, and scientific oversight for the BPD Resource Center and with whom we have had many thought provoking discussions.
Author information
Authors and Affiliations
Corresponding author
Additional information
Supported in part by NIH Grants HL63399, HL52636 BPD Resource Center, P51RR13986 Primate Center facility support; HL63397 (to L.-Y.C.); HL46691, HL56061 and a gift from the Jamie and Bobby Gates Foundation (to R.I.C.).
Rights and permissions
About this article
Cite this article
Chang, L., McCurnin, D., Yoder, B. et al. Ductus Arteriosus Ligation and Alveolar Growth in Preterm Baboons With a Patent Ductus Arteriosus. Pediatr Res 63, 299–302 (2008). https://doi.org/10.1203/PDR.0b013e318163a8e4
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/PDR.0b013e318163a8e4
This article is cited by
-
Perinatal origins of bronchopulmonary dysplasia—deciphering normal and impaired lung development cell by cell
Molecular and Cellular Pediatrics (2023)
-
Patent ductus arteriosus, bronchopulmonary dysplasia and pulmonary hypertension—a complex conundrum with many phenotypes?
Pediatric Research (2023)
-
Impact of patent ductus arteriosus shunt size and duration on risk of death or severe respiratory morbidity in preterm infants born in China
European Journal of Pediatrics (2022)
-
Patent ductus arteriosus shunt elimination results in a reduction in adverse outcomes: a post hoc analysis of the PDA RCT cohort
Journal of Perinatology (2021)
-
Post-ligation cardiac syndrome is associated with increased morbidity in preterm infants
Journal of Perinatology (2018)