Abstract
Cardiovascular disease is an important cause of morbidity in recipients of renal transplants. The aim of the present study was to analyze the status of the arginine-creatine pathway in such patients, given the relationship between the arginine metabolism and both renal function and the methionine-homocysteine cycle. Twenty-nine children and adolescents (median age 13, range 6–18 years), who had received a renal allograft 14.5–82.0 months before, were recruited for the study. On immunosuppressive therapy, all patients evidenced an adequate level of renal function. Plasma concentrations of homocysteine and glycine were significantly higher, whereas urinary excretions of guanidinoacetate and creatine were significantly lower than controls. Urinary excretions of guanidinoacetate and creatine correlated positively with creatinine clearance. Urinary excretion of creatine was negatively correlated with plasma concentration of homocysteine. The demonstration of disturbances in the arginine-creatine pathway in patients with well-functioning renal transplants and in absence of chronic renal failure represents a novel finding. We speculate that the low urinary excretion of guanidinoacetate and creatine is probably related to the nephrotoxic effect of immunosuppressive therapy and to defective methylation associated with the presence of hyperhomocysteinemia.
Similar content being viewed by others
Main
Cardiovascular disease is one of the main causes of morbidity and mortality in children and young adults with end-stage renal disease, with an estimated risk of 20 cardiovascular events per 1000 patients per year (1). This risk persists after renal transplantation because of many factors such as hypertension, dyslipidemia, hyperhomocysteinemia, hyperparathyroidism, obesity, insulin resistance, posttransplant diabetes, and immunosuppressive therapy, among others (2–6).
Recently, increased plasma levels of asymmetrical and symmetrical dimethylarginine have been observed in patients with chronic kidney diseases (7–9). High levels of these molecules are related with cardiovascular risk and endothelial dysfunction. Asymmetrical dimethylarginine is a competitive inhibitor of nitric oxide synthase, and healthy, normally functioning endothelial cells depend upon the bioactivity of nitric oxide as an important physiologic mediator of vascular tone and vascular structure (10).
Figure 1 shows the metabolic pathway that leads from arginine to creatine and its relation with the methionine-homocysteine methylation cycle. Creatine is synthesized by a two-step mechanism involving l-arginine: glycine amidinotransferase (AGAT, EC 2.1.4.1) and guanidinoacetate methyltransferase (GAMT, EC 2.1.1.2), and is taken up by cells through a specific creatine transporter, CT1. The first step, forming guanidinoacetate, is greatly dependent on the level of renal function, and the second step requires methylation of guanidinoacetate with a methyl group transferred from S-adenosylmethionine (SAM). Taking into account the use of nephrotoxic immunosuppressive agents and the high prevalence of hyperhomocysteinemia in children and adolescents recipient of renal transplants (5), it is surprising that little attention has been paid to arginine metabolism in such patients. The aim of the present work was to measure the status of the arginine-creatine pathway and its relation with methylation cycle.
Relationship between the metabolic pathway from arginine to creatine and the methylation cycle. The abbreviations stand for: nitric oxide synthase (NOS), l-arginine:glycine amidinotransferase (AGAT), guanidinoacetate N-methyltransferase (GAMT), specific creatine transporter (CT1), methionine adenosyltransferase (MAT), S-adenosylhomocysteine hydrolase (SAHH), cystathionine β-synthase (CBS), methionine synthase (MS), betaine homocysteine methyltransferase (BHMT), tetrahydrofolate (THF).
PATIENTS AND METHODS
Twenty-nine patients aged 6–18 years (12.83 ± 4.02; 20 males, 9 females) were recruited for the study. All were deceased kidney transplant recipients followed up in our center, and were clinically stable at the time of the study. Clinical and biochemical characteristics of the patients are shown in Table 1. The study was performed to all transplanted children and adolescents between 2 and 20 years old. Exclusion criteria were the presence of hepatopathy and/or insulin-dependent diabetes mellitus.
Immunosuppressive therapy combined mycophenolate mofetil with tacrolimus (27 patients), cyclosporine A (1 patient), or sirolimus (1 patient). Eighteen children were also on prednisone. None of the patients received treatment with folic acid, vitamin B12, or statins.
The study protocol was approved by the Ethics Committee of Clinic Research of Cruces Hospital, and patients' parents gave written informed consent.
Laboratory procedures.
Biologic data in blood and urine correspond to single measurements performed on samples collected at the same time. Samples were taken in the morning after an overnight fasting and before taking their daily medication. The collection was carried out at the time of their regular visits to the hospital for follow-up. Blood samples were cooled in an ice-water bath and immediately centrifuged at 1000× g for 5 min at 4°C. The platelet-poor plasma and urine were aliquoted and stored at −40°C until the assay was performed, usually within a few days.
Albumin, homocysteine, and creatinine were measured using standard laboratory techniques. Estimated GFR (eGFR) was calculated by the Schwartz's formula (11). The quantification of plasma and urinary amino acids (arginine, methionine, ornithine, and glycine) was carried out with a Biochrom 30 ionic chromatograph (Gomensoro, Madrid). The instrument has a specific program to separate the amino acids using Biochrom Ultropak 4 and Ultropak 8 columns. The mobile phases are commercialized as a kit (Biochrom Reference 80-2098-05). After postcolumn derivatization with ninhydrin, the absorbance is monitored at 440 and 570 nm.
Guanidinoacetate and creatine were quantified using a published method (12) with slight modifications. 13C2-guanidinoacetate and d3-creatine were used as internal standards. N-(tert-butyldimethylsilyl)-N-methyltrifluoroacetamide (Sigma Chemical Co., Aldrich, Madrid) was preferred for the derivatization of the liquid-liquid extracts instead of synthesizing the trimethylsilyl derivatives because it produced more intense fragments. Guanidinoacetate and creatine were separated and quantified on a Hewlett Packard GC 6890 gas chromatograph using a Hewlett Packard 5973 mass selective detector on a capillary column HP-5MS (30 m × 0.25 mm, 0.25 μm) (Supelco, Bellefonte, PA). The oven temperature was 120°C at injection, and this was maintained for 3 min, then raised by 3°C/min to 170°C, and finally raised by 15°C/min to 300°C and isothermally maintained for 5 min. Injector temperature were 275°C with a 1:5 split ratio, and source and quadruple detector temperatures were 230°C and 150°C, respectively. Helium was used as the carrier gas under a pressure of 0.5 bars. The ions measured were m/z 220 and 221 for guanidinoacetate and 13C2-guanidinoacetate, and m/z 360 and 363 for creatine and d3-creatine, respectively. Results for guanidinoacetate and creatine are expressed as mmol/mol creatinine.
Statistical analysis.
The SPSS version 12.0 was used as statistical software. Descriptive statistics are presented as median and interquartile range. Spearman's ρ test was used to evaluate relationship between continue variable. Statistically significant differences between groups were analyzed using the Kruskall Wallis test. The Kendall τ test was used to measure correlations between ordinal-level variables and the strength of their relationships. All probability values are two-tailed and the level of significance required was p < 0.05.
RESULTS
Biochemical profile in plasma and urine.
Results are presented in Table 2. Posttransplant renal function was excellent, with a median value for creatinine clearance (estimated by height) as high as 91 mL/min/1.73 m2 (76.8–103.0). Thirteen patients showed chronic renal insufficiency (CRI) I (eGFR > 90), 12 with CRI II (eGFR 60–90), and 1 with CRI III (eGFR 30–60). Only 13 of the 29 transplanted patients showed moderately elevated values of plasma creatinine (13).
Median value for plasma homocysteine level was clearly elevated (9.0 μM) (p < 0.001), and 12 of the patients (41%) showed values above the 97th percentile of controls (14). In comparison with reference values (15), transplanted children presented higher plasma values for arginine and glycine (p = 0.128 and p = 0.083, respectively) and normal plasma values for methionine, ornithine, and citrulline. It should be noted that urinary excretion of guanidinoacetate and creatine were significantly lower in our patients than in healthy children (p = 0.006 and p < 0.001, respectively). Urinary excretion of methionine and glycine were also below the reference values (15) (p = 0.016 and p < 0.001, respectively).
Correlations between parameters.
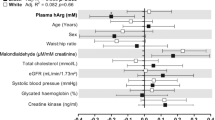
Table 3 summarizes the statistically significant correlations observed between urinary excretion of guanidine-compounds and the amino acid profile. It is worth pointing out that eGFR correlated positively with the urinary excretions of both guanidinoacetate and creatine (r = 0.559, p = 0.002 and r = 0.636, p < 0.001, respectively) (Fig. 2).
Urinary excretions of guanidinoacetate and creatine related positively with urinary excretions of arginine and glycine. In addition, urinary excretion of creatine was positively correlated with the excretion of guanidinoacetate, methionine, and ornithine in urine, whereas it correlated negatively with the plasma concentration of glycine and homocysteine. It is noteworthy the negative correlation present between urinary excretion of creatine and the level of plasma homocysteine (r = −0.531, p = 0.004) (Fig. 3).
Plasma concentrations of arginine and methionine were significantly correlated too (r = 0.480, p = 0.008). Further, plasma glycine was negatively correlated with the creatinine clearance (r = −0.612, p = 0.001) and urinary creatine (r = −0.536, p = 0.003), but positively with the level of plasma homocysteine (r = 0.744, p < 0.001), as well as with creatinine (r = 0.601, p = 0.001). Finally, there was a correlation between plasma homocysteine and prealbumine (r = 0.587, p = 0.002) and also with the patient's age (r = 0.575, p = 0.002). We did not observe statistically significant correlations between plasma homocysteine and body mass index, or between plasma arginine and glycine concentrations and their corresponding urinary excretion.
DISCUSSION
In this study, we have first observed that children with stable kidney transplants under treatment with chronic immunosuppresors present increased plasma arginine and glycine levels, whereas low urinary excretions of guanidinoacetate and creatine. These findings suggest low activities of the enzymes AGAT, which gives rise to the formation of guanidinoacetate from arginine, and of GAMT, which facilitates methylation of this compound to form creatine (Fig. 1). The demonstration of disturbances in the arginine-creatine pathway in patients with well-functioning kidney grafts represents a novel finding.
The kidney plays an important but not an exclusive role in the metabolism of arginine. In adult animals, AGAT and GAMT are highly expressed in the kidney and pancreas, and GAMT is found in high levels on liver and pancreas too. AGAT, GAMT, and CT1 are also prominent in CNS, skeletal muscles, myocardium, and intestine (16). The intestine plays also a major role, producing citrulline from glutamine and glutamate. Afterwards, citrulline is converted into arginine in the kidney, mostly returning later to the circulation (17). The renal enzymes that produce arginine from citrulline (argininosuccinate synthetase and argininosuccinate lyase) are present in the proximal tubular cells (18). Therefore, body arginine content does not depend exclusively on the dietary intake, because the kidney can produce this amino acid even with an arginine-free diet (19). Glycine is thought to be beneficial to ischemia-reperfusion injury in the kidney, preventing chronic hypoxia (20). However, glycine clearance is diminished in our patients. Urinary glycine is related with eGFR, as well as the rest of the measured urinary amino acids, so this could be the reason why glycine clearance is reduced. In addition, as we can see in Table 3, urinary glycine has a strong correlation with guanidinoacetate, which is a strong marker for renal failure. Therefore, patients with reduced level of urinary guanidinoacetate or eGFR could have diminished glycine clearance as a result of their renal failure.
The interaction of arginine and glycine stimulated by AGAT, mainly expressed in the proximal tubular cells, gives rise to the formation of ornithine and guanidinoacetate. As reported herein, urinary excretion of guanidinoacetate is highly dependent on the eGFR. In rabbits with chronic renal failure (21–23), and in nondialyzed adult patients with chronic renal insufficiency (24), a correlation between low serum concentrations of guanidinoacetate and deficit in AGAT activity has been reported. The present finding of low urinary excretion of guanidinoacetate in kidney transplanted children and adolescents with normal or nearly only normal renal function suggests that other contributing factors, more than reduced kidney mass, may also be involved. Kiyatake et al. (25), studied gentamicin nephrotoxicity in rats, and concluded that guanidinoacetate was a more sensitive indicator of renal injury than conventional indicators, such as urine N-acetyl-β-d-glucosaminidase and β2-microglobulin. Therefore, the possible nephrotoxic effect of immunosuppressive therapy should be considered in our group. Despite there are no studies regarding its potential effect on AGAT activity, it is known that both cyclosporine A and tacrolimus may have a deleterious effect upon renal tubular function (26). These immunosuppressors could also cause endothelial dysfunction, acting on the NO production within proximal cells. The reduced endothelial NO production in renal transplants due to these immunosuppressors, may cause hypertension and contribute to the high risk of developing premature atherosclerosis observed in patients with renal transplants (27,28).
The methylation of guanidinoacetate by the enzyme GAMT in the liver produces creatine, which is liberated toward tissues and taken into the cells through the specific creatine transporter, CT1. This methyl group is transferred from SAM, which becomes S-adenosylhomocysteine (SAH). Both SAM and SAH can be further hydrolyzed to homocysteine and adenosine (29). Homocysteine can be methylated to regenerate methionine in all cells (transmethilation) by the folate/B12-dependent methionine synthase reaction, and additionally by the betaine-homocysteine methyltransferase reaction in liver and kidney (30,31) (Fig. 1).
Our results, showing that plasma arginine and methionine concentrations were significantly correlated and that urinary excretion of creatine was correlated positively with urinary excretions of methionine, but negatively with plasma level of homocysteine, indicate that those disturbances observed in the arginine-creatine pathway were intimately related to methionine-homocysteine metabolism. In patients with renal failure a decreased ratio of SAM/SAH has been reported (32), thus transmethylation reactions could be secondarily disturbed. The high plasma values of homocysteine present in kidney transplanted patients may be also associated with parallel increases in plasma SAH and secondary inhibition of methyltransferases such as GAMT.
The findings related to methionine-homocysteine metabolism merit also a brief comment. Plasma homocysteine concentration increases significantly with age as already shown by Vilaseca et al. (14). However, in the current study, no correlation was found between plasma homocysteine concentration and body mass index, in accordance with the findings of other authors (33). Such relationship is controversial, because positive (34,35) or even negative associations (36) have been also published. The significant relation found between plasma concentrations of homocysteine and prealbumine may be explained by the fact that methionine, precursor of homocysteine, comes from dietary protein and prealbumine is a biologic marker of protein intake.
The data presented herein should be also analyzed taking into account that approximately 10-fold more l-arginine is metabolized to creatine than is used for nitric oxide synthesis (37). If the conversion to guanidinoacetate is impaired, the accumulation of arginine and its derivative asymmetrical dimethylarginine will further compromise the function of nitric oxide synthase, and thus have a negative effect on endothelial function, and potentially increased the cardiovascular risk inherent to the use of immunosuppressive agents. In addition, l-arginine supplementation has been proved to restore the formation of nitric oxide, thus improving renal function and reducing the inflammation in the renal allografts (38).
Whether a low systemic production of creatine may be an additional factor for the development of neurologic complications in kidney transplant recipients remains controversial (39). Creatine plays a major role in the storage and transmission of high-energy phosphates, as well as in the neuronal growth and axonal lengthening. Although it was assumed that systemic carnitine was essential to supply energy to the brain but nowadays there is evidence that all cells in the CNS can also synthesize creatine from arginine. The absence of expression of CRT1 in astrocytes reinforces the idea that under normal conditions the creatine used by the brain is synthesized mainly in the CNS (40). All patients with inherited creatine deficiency syndromes (AGAT deficiency, GAMT deficiency, and CT1 deficiency) reveal developmental delay/regression, mental retardation, and severe disturbance of their expressive and cognitive speech. The common feature of all creatine deficiency syndromes is the severe depletion of creatine/phosphocreatine in the brain (41). The beneficial effect of early creatine supplementation in a patient with AGAT deficiency would indicate, however, that systemic carnitine may be taken into the brain and restore normal neuronal functioning (42).
SAH is recognized as an important inhibiting factor of DNA methylation (31). Therefore, it remains possible that decreased cellular methylation may also affect brain formation of creatine in transplanted subjects. The potential CNS damage should be especially considered in infants with congenital NS who receive renal transplantation early in life and represent a high-risk population for neurologic impairment (43,44). Studies using brain proton magnetic resonance spectroscopy may be useful in the follow-up of these cases (45). The possible beneficial effect of early carnitine supplementation remains to be proved.
We conclude that plasma amino acids levels and urinary excretion of guanidinoacetate and creatine should be regularly monitored in pediatric patients with kidney transplants who represent a high-risk population due premature atherothrombosis and neurologic complications.
Abbreviations
- AGAT:
-
l-arginine:glycine amidinotransferase
- CNS:
-
Central nervous system
- CRI:
-
Chronic renal insufficiency
- CT1:
-
Specific creatine transporter
- eGFR:
-
Estimated glomerular filtration rate
- GAMT:
-
Guanidinoacetate methyltransferase
- SAH:
-
S-adenosylhomocysteine
- SAM:
-
S-adenosylmethionine
References
Parekh RS, Carroll CE, Wolfe RA, Port FK 2002 Cardiovascular mortality in children and young adults with end-stage disease. J Pediatr 141: 191–197
Silverstein DM, Palmer J, Polinsky MS, Brass C, Conley SB, Baluarte HJ 2000 Risk factors for hyperlipidemia in long-term pediatric renal transplant recipients. Pediatr Nephrol 14: 105–110
Hjelmesaeth J, Midtvedt K, Jenssen T, Hartmann A 2001 Insulin resistance after renal transplantation. Diabetes Care 24: 2121–2126
Greenspan LC, Gitelman SE, Leung MA, Glidden DV, Mathias RS 2002 Increased incidence of post-transplant diabetes mellitus in children: a case-control analysis. Pediatr Nephrol 17: 1–5
Aldamiz-Echevarria L, Sanjurjo P, Vallo A, Aquino L, Perez-Nanclares G, Gimeno P, Rueda M, Ruiz JI, Urreizti R, Rodriguez-Soriano J 2002 Hyperhomocysteinemia in children with renal transplants. Pediatr Nephrol 17: 718–723
Aldamiz-Echevarria L, Sanjurjo P, Vallo A, Aguirre M, Perez-Nanclares G, Gimeno P, Rueda M, Ruiz JI, Rodriguez-Soriano J 2003 Genetic and metabolic determinants of increased plasma plasminogen activator inhibitor-1 activity in children with renal transplants. Pediatr Nephrol 18: 749–755
Mendes Ribeiro AC, Brunini TM, Ellory JC, Mann GE 2001 Abnormalities in l-arginine transport and nitric oxide biosynthesis in chronic renal and heart failure. Cardiovasc Res 49: 697–712
Fleck C, Schweitzer F, Karge E, Busch M, Stein G 2003 Serum concentrations of asymmetric (ADMA) and symmetric (SDMA) dimethylarginine in patients with chronic kidney diseases. Clin Chim Acta 336: 1–12
Busch M, Fleck C, Wolf G, Stein G 2006 Asymmetrical (ADMA) and symmetrical dimethylarginine (SDMA) as potencial risk factors for cardiovascular and renal outcome in chronic kidney disease–possible candidates for paradoxical epidemiology?. Amino Acids 30: 225–232
Böger RH, Bode-Böger SM, Szuba A, Tsao PS, Chan JR, Tangphao O, Blaschke TF, Cooke JP 1998 Asymmetric dimethylarginine (ADMA): a novel risk factor for endothelial dysfunction. Circulation 98: 1842–1847.
Schwartz GJ, Haycock GB, Edelmann CM Jr Spitzer A 1976 A simple estimate of glomerular filtration rate on children derived from body weight and plasma creatinine. Pediatrics 58: 259–263
Arias A, Garcia-Villoria J, Ribes A 2004 Guanidinoacetate and creatine/creatinine levels in controls and patients with urea cycle defects. Mol Genet Metab 82: 220–223
Behram RE, Kliegman RM, Jenson HB 2004 Nelson Textbook of Pediatrics. 17th ed. Madrid, Spain, Elsevier Science Ed pp 2404
Vilaseca MA, Moyano D, Ferrer I, Artuch R 1997 Total homocysteine in pediatric patients. Clin Chem 43: 690–692
Shih VE 2003 Amino Acid Analysis. Blau N, Duran M, Blaskovics ME, Gibson KM Physician's Guide to the Laboratory Diagnosis of Metabolic Disease. Heidelberg, Germany, Springer-Verlag 11–26
Braissant O, Henry H, Villard AM, Speer O, Wallimann T, Bachmann C 2005 Creatine synthesis and transport during rat embryogenesis: spatiotemporal expression of AGAT, GAMT and CT1. BMC Dev Biol 5: 9
Morris SM 2004 Enzymes of arginine metabolism. J Nutr 134: 2743S–2747S
Scibior D, Czeczot H 2004 [Arginine–metabolism and functions in the human organism]. Postepy Hig Med Dosw (Online) 58: 321–332
Brosnan ME, Brosnan JT 2004 Arginine metabolism: enzymology, nutrition, and clinical significance. J Nutr 134: 2791S–2795S
Yin M, Zhong Z, Connor HD, Bunzendahl H, Finn WF, Rusyn I, Li X, Raleigh JA, Mason RP, Thurman RG 2002 Protective effect of glycine on renal injury induced by ischemia-reperfusion in vivo. Am J Physiol Renal Physiol 282: F417–F423
Kuroda M 1993 Study on impaired metabolism of guanidinoacetic acid in chronic renal failure rabbits with special reference to impaired conversion of arginine to guanidinoacetic acid. Nephron 65: 605–611
Al Banchaabouchi M, Marescau B, Van Marck E, D'hooge R, De Deyn PP 2001 Long-term effect of partial nephrectomy on biological parameters, kidney histology, and guanidino compound levels in mice. Metabolism 50: 1418–1425
Tofuku Y, Muramoto H, Kuroda M, Takeda R 1985 Impaired metabolism of guanidinoacetic acid in uremia. Nephron 41: 174–178
Marescau B, Nagels G, Possemiers I, De Broe ME, Because I, Billiouw JM, Lornoy W, De Deyn PP 1997 Guanidino compounds in serum and urine of nondialyzed patients with chronic renal insufficiency. Metabolism 46: 1024–1031
Kiyatake I, Nakamura T, Koide H 2004 Urinary guanidinoacetic acid excretion as an indicator of gentamicin nephotoxicity in rats. Ren Fail 26: 339–344
McLin VA, Girardin E, Lecoultre C, Mentha G, Belli DC 2005 Glomerular and tubular function following orthotopic liver transplantation in children. Pediatr Transplant 9: 512–519
Morris ST, McMurray JJ, Rodger RS, Farmer R, Jardine AG 2000 Endothelial dysfunction in renal transplant recipients maintained on cyclosporine. Kidney Int 57: 1100–1106
Takeda Y, Miyamori I, Furukawa K, Inaba S, Mabuchi H 1999 Mechanisms of FK 506-Induced hypertension in the rat. Hypertension 33: 130–136
Handy DE, Scolaro J, Chen J, Huang P, Loscalzo J 2004 l-arginine increases plasma homocysteine in apoE−/−/iNOS−/− double knockout mice. Cell Mol Biol 50: 903–909
Finkelstein JD 1998 The metabolism of homocysteine: pathways and regulation. Eur J Pediatr 157: S40–S44
Yi P, Melnyk S, Pogribna M, Pogribny IP, Hine RJ, James SJ 2000 Increase in plasma homocysteine associated with parallel increases in plasma S-adenosylhomocysteine and lymphocyte DNA hypomethylation. J Biol Chem 275: 29318–29323
Perna AF, Ingrosso D, Galletti P, Zappia V, De Santo NG 1996 Membrane protein damage and methylation reactions in chronic renal failure. Kidney Int 50: 358–366
Wollesen F, Brattström L, Refsum H, Ueland PM, Berglund L, Berne C 1999 Plasma total homocysteine and cysteine in relation to glomerular filtration rate in diabetes mellitus. Kidney Int 55: 1028–1035
Jacques PF, Bostom AG, Wilson PW, Rich S, Rosenberg IH, Selhub J 2001 Determinants of plasma total homocysteine concentration in the Framingham Offspring cohort. Am J Clin Nutr 73: 613–621
Koehler KM, Romero LJ, Stauber PM, Pareo-Tubbeh SL, Liang HC 1996 Vitamin supplementation and other variables affecting serum homocysteine and methylmalonic acid concentrations in elderly men and women. J Am Coll Nutr 15: 364–376
Ganji V, Kafai MR 2003 Demographic, health, lifestyle, and blood vitamin determinants of serum total homocysteine concentrations in the third National Health and Nutrition Examination Survey, 1988–1994. Am J Clin Nutr 77: 826–833
Castillo L, Beaumier L, Ajami AM, Young VR 1996 Whole body nitric oxide synthesis in healthy men determined from [15N]arginine-to-[15N]citrulline labelling. Proc Natl Acad Sci USA 93: 11460–11465
Vos IH, Rabelink TJ, Dorland B, Loos R, Van Middelaar B, Grone HJ, Joles JA 2001 l-arginine supplementation improves function and reduces inflamation in renal allografts. J Am Soc Nephrol 12: 361–367
Ponticelli C, Campise MR 2005 Neurological complications in kidney transplant recipients. J Nephrol 18: 521–528
Braissant O, Henry H, Loup M, Eilers B, Bachmann C 2001 Endogenous synthesis and transport of creatine in the rat: an in situ hybridization study. Brain Res Mol Brain Res 86: 193–201
Schulze A 2003 Carnitine deficiency syndromes. Mol Cell Biochem 244: 143–150
Battini R, Alessandrì MG, Leuzzi V, Moro F, Tosetti M, Bianchi MC, Cioni G 2006 Arginine:glycine amidinotransferase (AGAT) deficiency in a newborn: early treatment can prevent phenotypic expression of the disease. J Pediatr 148: 828–830
Laakkonen H, Lonnqvist T, Uusimaa J, Qvist E, Valanne L, Nuutinen M, Ala-Houhala M, Majamaa K, Jalanko H, Holmberg C 2006 Muscular dystonia and athetosis in six patients with congenital nephrotic syndrome of the Finnish type (NPHS1). Pediatr Nephrol 21: 182–189
Aldamiz-Echevarría L, Vallo A, Sanjurjo P, Gonzalez-Lamuño P, Elorz J, Prieto JA, Andrade F, Rodriguez-Soriano J 2007 Essential fatty acid deficiency profile in patients with nephrotic-range proteinuria. Pediatr Nephrol 22: 533–540
Leuzzi V 2002 Inborn errors of creatine metabolism and epilepsy: clinical features, diagnosis, and treatment. J Child Neurol 3: 3S89–3S97
Author information
Authors and Affiliations
Corresponding author
Additional information
This work was supported by a grant from the “Public Health Department,” Basque Government (Grant 2006111068).
Rights and permissions
About this article
Cite this article
Andrade, F., Rodríguez-Soriano, J., Prieto, J. et al. The Arginine-Creatine Pathway is Disturbed in Children and Adolescents With Renal Transplants. Pediatr Res 64, 218–222 (2008). https://doi.org/10.1203/PDR.0b013e318176180e
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/PDR.0b013e318176180e
This article is cited by
-
High plasma guanidinoacetate-to-homoarginine ratio is associated with high all-cause and cardiovascular mortality rate in adult renal transplant recipients
Amino Acids (2019)
-
LC-QTOF-MS-based targeted metabolomics of arginine-creatine metabolic pathway-related compounds in plasma: application to identify potential biomarkers in pediatric chronic kidney disease
Analytical and Bioanalytical Chemistry (2016)