Abstract
With increasing pressure support ventilation (PSV), a form of pneumatically triggered ventilation, there can be an increase in wasted inspiratory efforts (neural inspiratory efforts that fail to trigger the ventilator). With neurally adjusted ventilatory assist (NAVA), a mode of ventilation controlled by the electrical activity of the diaphragm (EAdi), synchrony should be maintained at high levels of assist. The aim of this study was to evaluate the response to increasing levels of PSV and NAVA on synchrony and diaphragm unloading in lung-injured rabbits. Animals were ventilated on PSV or NAVA in random order, each at three levels. We measured neural and ventilator respiratory rates, EAdi, transdiaphragmatic pressure (Pdi), and tidal volume (Vt). At low PSV, 95% of neural efforts were triggered, compared with high PSV, where only 66% of the neural efforts were triggered. During NAVA, all neural efforts were triggered, regardless of level. Increasing NAVA levels reduced EAdi and Pdi-time products by 48% (p < 0.05) and 66% (p < 0.05). In contrast, increasing PSV did not reduce the diaphragm electrical activity-time product and increased the transdiaphragmatic pressure-time product (p < 0.05) due to the increased wasted efforts. We conclude that synchrony with the ventilator is an important determinant for diaphragm unloading.
Similar content being viewed by others
Main
Patient-triggered ventilation in the pediatric intensive care unit setting is common (1) and compared with conventional mechanical ventilation has been shown to improve Vt (2), work of breathing (2), and oxygenation (3) and to reduce blood pressure fluctuations (4) and transpulmonary pressure (5) in newborns. Despite these findings, a recent meta-analysis indicates that patient-triggered ventilation has no impact on mortality (6). One possible explanation for this may be that even though patient-triggered ventilation was used, synchronous ventilation may not have actually been achieved, an observation not reported in many trials.
A common form of patient-triggered ventilation is PSV, a mode of partial ventilatory assist that is triggered by pressure or flow, is pressure targeted, and flow cycled. It is generally believed that increasing the level of assist with PSV unloads the respiratory muscles (7,8). However, investigators have demonstrated there may be a significant amount of respiratory work to trigger the ventilator (9), and there may be wasted inspiratory efforts, where the patient makes an inspiratory effort, but the ventilator fails to trigger. These asynchronies are aggravated at higher levels of assist (9,10) and possibly at higher respiratory rates because expiratory time is too short to allow complete exhalation. Dynamic hyperinflation puts the diaphragm at a mechanical disadvantage, thereby affecting the ability to trigger the ventilator.
NAVA is a mode of partial ventilatory assist in which the ventilator is controlled by the electrical activity of the diaphragm (EAdi) (11). The EAdi represents the final neural output of the respiratory centers to the diaphragm. With NAVA, the pressure during inspiration is delivered in proportion to the EAdi; this proportionality factor can be adjusted. Depending on the patient's response to the delivered pressure, an increase in the NAVA level could potentially increase the pressure delivered by the ventilator (if the EAdi remains constant) or it could suppress the EAdi and hence deliver the same amount of assist or somewhere in between. This is different from PSV, which delivers a fixed pressure, independent of changes in respiratory drive.
Another important difference between NAVA and PSV is evident during hyperinflation, where pressure or flow triggering during PSV may be affected due to weakened pressure/flow generated by the respiratory muscles. Although the diaphragm is at a mechanical disadvantage at higher lung volumes, the EAdi signal is not decreased. In fact, the response to weakened mechanical output of the diaphragm is an increase in EAdi (12–14). With respect to cycling-off the ventilator breath, the neural expiration is not detected during PSV, which could lead to overinflation and excessive volume delivery, whereas with NAVA, cycling-off occurs when the diaphragm activity is turned off by the respiratory centers and hence should provide a more physiologic termination of the assist.
The aim of this study was to evaluate the influence of increasing levels of PSV and of NAVA on synchrony, EAdi, Pdi, the diaphragm electrical and mechanical energy expenditures (EAdi-time product and Pdi-time product per minute) and Vt in rabbits with acute lung injury. We hypothesized that with increasing NAVA levels, synchrony would be maintained, even at high levels of assist, and should deliver minimal increases in tidal volume. We expected increased tidal volume delivery and increased asynchrony with increasing levels of PSV.
METHODS
This study was approved by the St. Michael's Hospital Animal Care and Use Committee. Care and handling of the animals were in accord with the Canadian Council on Animal Care.
Animal preparation and instrumentation.
Twelve adult male New Zealand white rabbits (Charles River Labs, St. Constant, Quebec, Canada), with a mean body weight of 3.3 ± 0.9 kg, were studied. The animals were anesthetized with an intramuscular bolus of ketamine hydrochloride (35 mg/kg). Ketamine hydrochloride (10 mg/kg/h), xylazine (2 mg/kg/h), and lactated Ringer's solution (5 mL/kg/h) were continuously infused. Under this anesthetic protocol, animals are sedated but breathing spontaneously and have intact respiratory drive.
Arterial blood pressure (Pd 23, Gould Inc., Cleveland, OH) and blood for measurement of arterial blood gases (Ciba-Corning Model 248, Bayer, Leverkusen, Germany) were obtained from an ear artery. Transcutaneous oxygen saturation was measured with pulse oximetry (NONIN 8600 VTM, Nonin Medical Inc., Plymouth, MN) at the tail. Body temperature, measured with a rectal probe, was maintained between 37.5° and 39.0°C with a heated surgical table. The animals were tracheostomized and ventilated by a Servo ventilator 300 (Maquet Critical Care, Solna, Sweden).
Flow and Vt signals were obtained from the ventilator. Airway pressure was measured at the Y piece of the respiratory circuit. The EAdi was recorded from an array of electrodes mounted on an 8-F esophageal catheter, which also contained balloons for measurement of esophageal and gastric pressures. Pdi was calculated as gastric pressure minus esophageal pressure. Proper positioning of the catheter was allowed by online display of the electrocardiogram detected by the electrodes, and correllograms of EAdi signals (15). Esophageal balloon positioning was confirmed by the occlusion method (16).
Experimental protocol.
After instrumentation, the rabbits were ventilated with volume control (VT 6 mL/kg, positive end-expiratory pressure (PEEP) = 2 cm H2O, Fio2 = 50%, rate = 20/min). In eight animals, repeated boluses of pancuronium (0.05 mg i.v.) were administered until the EAdi was no longer detected to measure respiratory system compliance. In all animals, lung injury was performed by instilling (2.0 mL/kg) hydrochloric acid (pH 1.5) into the trachea and performing a recruitment maneuver (continuous positive airway pressure of 25 cm H2O for about 5 s). A second compliance measurement was taken after lung injury, and the animals were ventilated in volume control mode for 20 min or until the pancuronium wore off.
Each animal underwent both an incremental PSV run and an incremental NAVA run, the order of the mode being randomized by the flip of a coin (five of the animals underwent PSV first). For the incremental PSV runs, the lowest assist level was set to 4 cm H2O (PSVlo). The PSV level was increased in steps of 4 cm H2O every 5 min, until 16 cm H2O was reached, unless wasted efforts of ≥20-s duration were observed, and then this level was defined as the highest PSV (PSVhi). (Wasted efforts were defined as the presence of EAdi, with absence of airway pressure delivery.) The trigger variable was set in the middle of “the green region” (flow trigger approximately 0.35 L/min), and the cycling-off criteria were fixed at 5% of peak flow. Cycling-off criteria are not adjustable on the SV300. The rise time was set to 5%. The trigger sensitivity and rise time were similar for all animals and were not adjusted during the experiment.
In each animal, incremental NAVA was individually set by first determining the NAVAlo, as the level predicted to give an airway pressure of 4 cm H2O with the EAdi observed during PSVlo. This NAVA level (am arbitrary number) could vary between animals. Thereafter, the NAVA level was increased in steps of 0.2–0.4 (arbitrary units) (depending on the baseline value), until four steps had been tested (NAVAhi). This four-step increase in the NAVA level would be equivalent to 16 cm H2O in PSV if the EAdi value is not altered.
PEEP was the same during both the PSV and NAVA runs and was titrated according to Allo et al. (17). PEEP was not changed during the protocol and was 7.8 ± 2.4 cm H2O for both modes. Fio2 was set to 50% in all but two animals (40% Fio2) and remained unchanged.
EAdi signal processing.
EAdi signals were processed with computer algorithms that (i) ascertained that the electrode array was positioned appropriately near the diaphragm; (ii) eliminated the influence of the ECG, motion–induced disturbances, background noise, and disturbances from the mains (12,18,19); and (iii) calculated the root mean square value for sequential EAdi segments of 16-ms duration (12,18). The processed EAdi wave form is used to control the mechanical ventilator and is also displayed online and stored for later analysis.
Method for NAVA.
NAVA is a mode of partial ventilatory assist in which the pressure delivered by the ventilator is proportional to the EAdi (11). Figure 1 demonstrates tracings in one rabbit breathing on NAVA after acute lung injury.
During NAVA, to adjust the level of pressure delivered by the ventilator, the EAdi is multiplied by a number. This number is referred to as the NAVA level and is the proportionality factor between EAdi and pressure delivered. An increase in the NAVA level equals more pressure delivered if the EAdi (i.e. respiratory drive) does not decrease. With NAVA, the assist is triggered when the EAdi exceeds a threshold increment and is cycled-off when the EAdi falls below a percentage (default 80%) of peak inspiratory activity.
Data analysis.
Analysis of EAdi and the respiratory variables was performed offline. For both NAVA and PSV, an average of the variables was calculated for the last minute of the 5-min runs. Breath-by-breath analysis was performed on the EAdi and Pdi signals, without any feedback about ventilator parameters (the investigator was blinded to the ventilator flow and airway pressure), and then breath-by-breath analysis was performed on the ventilator-flow signal without feedback about EAdi and Pdi. Vt was obtained by integration of the flow signal.
Ventilator timings (ventilator Ti and ventilator Te) were determined from the flow signal. Neural inspiratory time (neural Ti) and neural expiratory time (neural Te) were defined from the EAdi signal. Neural respiratory rate and ventilator rate were counted, independently from each other by an investigator blinded to the ventilation mode. EAdi- and Pdi-based diaphragm energy expenditures were calculated per minute as the products of the mean inspiratory EAdi or Pdi and the neural inspiratory time and the neural respiratory rate. The trigger delays were calculated as the time between the onset of EAdi and the onset of ventilator flow. The off-cycling delays were calculated as the time between the onset of neural Te and the onset of expiratory flow.
Statistics.
As there were three to four steps tested with either mode, to allow for comparisons, the data were divided into three levels of assist in each mode (NAVAlo, NAVAmed, and NAVAhi and PSVlo, PSVmed, and PSVhi), as described by others (20). All variables were analyzed for NAVAlo, NAVAmed, NAVAhi and PSVlo, PSVmed, and PSVhi with nonparametric tests for repeated- measures analysis of variance (ANOVA) (Friedman repeated-measures ANOVA on ranks) (Sigmastat, Jandel Scientific, San Rafael, CA). The Student-Neuman-Keuls method was used for all pairwise multiple comparisons. A significant difference was defined as p < 0.05.
RESULTS
One minute after lung injury, the mean Pao2/Fio2 was 208.6 ± 117 [mean ± standard deviation (SD)]. Respiratory system compliance was reduced after the injury by 41 ± 13%. Arterial blood pressure decreased only slightly from the beginning of the protocol (84 ± 11 over 78 ± 15) to the end of the protocol (63 ± 8 over 55 ± 12), p < 0.05.
Figure 2 demonstrates the tracings in one rabbit breathing with NAVAlo, NAVAhi, PSVlo, and PSVhi. At PSVlo, the animal demonstrated large phasic EAdi and successfully triggered breaths for every neural inspiratory effort. At PSVhi, wasted efforts occurred that increased the magnitude of EAdi and Pdi when compared with the successfully triggered breaths at PSVhi, where there was immediate deactivation and unloading of the diaphragm. With NAVA, there was a progressive reduction in the mean inspiratory EAdi and Pdi with progressive increases in the NAVA level. Different from PSV, we did not observe wasted efforts; even at the highest NAVA levels.
Example of tracings obtained in one rabbit breathing on NAVAlo and NAVAhi and PSVlo and PSVhi. EAdi (top tracings), airway pressure (Paw, measured at the Y piece), and flow tracings (measured at the ventilator), and Pdi (bottom tracings) are demonstrated for one rabbit at NAVAlo (A), NAVAhi (B) and PSVlo (C) and PSVhi (D).
Group mean data of Vt and diaphragmatic efforts for the low, medium, and high NAVA and PSV levels are presented in Figure 3. The peak airway pressure was comparable for the NAVAlo [3.52 (2.5–5.4) cm H2O] and PSVlo [3.9 (2.7–5.0) cm H2O] runs (Fig. 3A). With increasing PSV, the highest level of support was approximately fourfold, 15.1 (14.4–17.6, p < 0.05) cm H2O. With a mean four-time increase in the NAVA level, the highest level of support reached 5.7 (4.0–6.8) cm H2O. Vt increased much more with increasing PSV (p < 0.05) than with increasing NAVA (Fig. 3B). The increase in Vt with increasing NAVA level was small and reached significance at the highest level only. In accordance with the Vt data, transpulmonary pressure increased significantly with increasing PSV (3.4 to 8.1 cm H2O, p < 0.05), whereas with increasing NAVA, transpulmonary pressure was not significantly changed (2.9 to 3.1 cm H2O) (Tables 1 and 2).
Airway pressure, Vt, Pdi-time product, and EAdi-time product for NAVAlo, NAVAmed, and NAVAhi and PSVlo, PSVmed, and PSVhi. Group data (median with quartiles). (A) Peak airway pressure (above PEEP) for PSVlo, PSVmed, and PSVhi and NAVAlo, NAVAmed, and NAVAhi. (B) Vt for PSVlo, PSVmed, and PSVhi and NAVAlo, NAVAmed, and NAVAhi. (C and D) EAdi and Pdi-time products for PSVlo, PSVmed, PSVhi and NAVAlo, NAVAmed, and NAVAhi. *Significantly different from low level, and †indicates significantly different from medium level, p < 0.05.
The minute pressure-time product of the diaphragm (Fig. 3C) and the minute EAdi-time product (Fig. 3D) both decreased significantly (p < 0.05) with progressive increases in NAVA, whereas with increasing PSV, there was an initial reduction from PSVlo to PSVmed (p < 0.05), followed by a significant increase from PSVmed to PSVhi (p < 0.05). The EAdi per breath and Pdi swings per breath followed the same behavior (Tables 1 and 2).
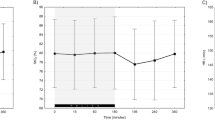
The trigger delays increased more with increasing PSV (90–228 ms, p < 0.05) than with increasing NAVA (76–96 ms, p < 0.05) (Fig. 4A). Although not significant, there was a trend for the off-cycling delays to increase more with increasing PSV (Fig. 4B).
Trigger delay and cycling-off delay for PSVlo, PSVmed, and PSVhi and NAVAlo, NAVAmed, and NAVAhi. Group data (median with quartiles). (A) Trigger delay for PSVlo, PSVmed, and PSVhi and NAVAlo, NAVAmed, and NAVAhi. (B) Cycling-off delay for PSVlo, PSVmed, and PSVhi and NANAlo, NAVAmed, and NAVAhi. *Significantly different from low level, and †Significantly different from medium level, p < 0.05.
Figure 5 shows for both PSV (solid circles) and NAVA (empty circles) the relationship between the neural respiratory rate and the ventilator rate for all levels of assist in all animals. With NAVA at all levels, there were no wasted efforts (Table 1); this was not the case for PSV where the number of neural efforts could exceed the ventilator rate. The number of wasted efforts increased during higher levels of PSV. At PSVlo, 95% of the neural efforts were triggered, and with PSVhi, only 66% of the neural inspiratory efforts were triggered (Table 2).
DISCUSSION
This present study demonstrates in intubated rabbits with acute lung injury a systematic worsening in ventilator synchrony with increasing PSV, only permitting diaphragm unloading within a limited range of PSV levels. Further increasing PSV caused increased diaphragmatic activity due to ineffective triggering, accompanied by large increases in Vt delivery and transpulmonary pressure. With increasing NAVA, the diaphragm was progressively more unloaded, with low mean airway pressures and Vt, and there were no ineffective efforts.
Due to the fundamental differences between PSV and NAVA, it was not possible to obtain a direct, matched comparison of PSV and NAVA. This is mainly because during NAVA, there is no pressure or volume target, but rather the animal's respiratory control mechanisms limit pressure delivery by adjusting the respiratory drive. This means that even though the NAVA level was increased four times (same as PSV), we never reached a fourfold increase in delivered pressure because the animal reduced the respiratory drive progressively as the NAVA level was increased.
The results of this study also demonstrate that NAVA can unload the respiratory muscles at both low and high levels, whereas conventional PSV may only be able to unload within a small range of assist levels. PSV at high levels of assist may cause severe asynchrony and may even increase the work performed by the respiratory muscles during wasted efforts. Therefore, the findings of this study also illustrate the usefulness of monitoring the EAdi wave form during setting of conventional PSV levels.
Sinderby et al. and Beck et al. have demonstrated that increasing lung volume worsens the transmission of neural activity into ventilation (12–14). Therefore, unlike pneumatic trigger and cycling, which may function best when the respiratory mechanics and diaphragm strength are normal, NAVA may be more reliable with increasing impairment of respiratory mechanics and muscle function. This is because as the respiratory impairment worsens, the signals used to control PSV become progressively weaker, whereas the EAdi signals increase to compensate for the respiratory impairment. As demonstrated in this study, the synchrony between the ventilator's assist and inspiratory effort is well maintained even at very high levels of NAVA. To our knowledge, this is the first demonstration of a mode that can maintain synchrony between neural breathing efforts and ventilator assist regardless of the “assist” level. Of course, these results were obtained in an animal model of acute lung injury in which the responses are likely to be more uniform than in babies with respiratory distress syndrome.
To our knowledge, there are no data available about the incidence of wasted efforts during PSV in infants. We have previously reported severe patient ventilator asynchrony in intubated and mechanically ventilated infants breathing on synchronized intermittent mandatory ventilation (21). In a mixed population of babies deemed ready for extubation, we observed significant trigger and cycling-off delays, resulting in 53% of the total breathing cycle being asynchronous (21).
In adults, Fabry et al. (22) and Leung et al. (9) have demonstrated wasted efforts during PSV that increased with increasing levels of PSV. Leung et al. showed that the pressure-time product of the diaphragm increased during the wasted efforts, but different from the present study, they still found a decrease in the pressure-time product when all breaths (triggered and not triggered) were considered. Work by other groups has since demonstrated that the asynchrony during PSV is due to dynamic hyperinflation (20). Our current results in rabbits of increased diaphragm energy expenditure at high levels of PSV are different from our previous study in ventilated adult patients, where increasing PSV reduced the EAdi and Pdi consistently. This is likely due to the fact that respiratory rates in our previous study were comparably lower (23 bpm), and no wasted efforts were observed (23).
Active expiration during the inflation cycle has been demonstrated in preterm babies mechanically ventilated with time-cycled, pressure-limited ventilators (24–26). As well, Beck et al. (21) reported in intubated babies the occurrence of continued delivery of assist during mandatory breaths, despite the cessation of inspiratory EAdi. To our knowledge, varying the cycling-off criteria on the work of breathing and on patient-ventilator interaction have not been studied in infants. Chiumello et al. (27) showed in adult patients recovering from acute lung injury that changes in cycling-off criteria did not affect the work of breathing. In this study, we used a cycling-off criterion of 5% of peak inspiratory flow. For a small stiff lung with a fast time constant, this seems reasonable. Although not excessive, the cycling-off delays during PSV measured in this study were longer than with NAVA and increased with increasing PSV levels. The consequence of this delayed cycling-off is delayed or ineffective triggering of the subsequent inspiration. Regarding the mechanism, several studies have demonstrated that prolonged delivery of assist into neural expiration causes a reflex increase in the neural expiratory time (21,28,29). However, Younes et al. (29) indicated that the reflex prolongation of neural expiration may not be sufficient and that patients may sustain an increase in dynamic hyperinflation and trigger delays with pneumatic triggering. Our findings of incrementing trigger delays with increasing PSV could be in support for dynamic hyperinflation. When NAVA was implemented (i.e., neural cycling-off), we did not observe the same increases in Vt, reduced respiratory rates, or prolonged neural expiration, suggesting that NAVA interferes less with natural breathing pattern than PSV.
Regarding the influence of the rate of assist delivery on breathing pattern, Chiumello et al. (27) demonstrated that increasing the rate of rise of pressure delivery reduced the ventilator inspiratory time for a given pressure support level, whereas for a given rise time, increasing the pressure support lengthened the ventilator inspiratory time. In this study, in which the rise time was fixed, we also observed an increase in ventilator Ti with increasing PSV (Tables 1 and 2).
Critique of the method.
It could be suggested that the occurrence of wasted efforts at high levels of pressure support observed in this study were caused by a technical problem with the ventilator or that the trigger threshold was set too high. We are confident that the design of the study eliminated the influence of the mechanical performance of the ventilator and respiratory circuit because the same equipment was used during all conditions. As well, the trigger used in the study was a flow trigger (sensitivity was the same in all animals) and has been demonstrated to be more appropriate than pressure triggering in small infants with respiratory distress (30).
The use of a trigger-sensing device located in the inspiratory limb of the ventilator circuit and not at the airway may have affected our results; however, a comparison of flow-triggering in several infant ventilators demonstrated that the Servo300 is one of the most sensitive (31) despite that the flow sensor is within the ventilator (and not at the Y piece). Considering that others have also reported increased wasted efforts with different ventilators and proposed that dynamic hyperinflation is likely the cause of increasing asynchrony, placement of the pneumatic trigger sensor closer to the Y piece may have reduced the severity of the asynchrony, but not necessarily eliminated it.
Blood gas values presented in this study were obtained after short periods of different ventilator settings and perhaps should not be interpreted as representative of how these modes affect blood gases in the long term.
CONCLUSIONS
In acute lung injury, the physiologic response to increasing PSV and increasing NAVA are different. With NAVA, only small increases in airway pressure are required to unload the diaphragm, whereas pneumatically triggered PSV may fail to unload the diaphragm because of wasted inspiratory efforts, and may provide excessive transpulmonary pressures.
Abbreviations
- EAdi:
-
electrical activity of the diaphragm
- NAVA:
-
neurally adjusted ventilatory assist
- NAVAhi:
-
highest NAVA level
- NAVAlo:
-
lowest NAVA level
- Pdi:
-
transdiaphragmatic pressure
- PSV:
-
pressure support ventilation
- PSVhi:
-
highest pressure support level
- PSVlo:
-
lowest pressure support level
- Vt:
-
tidal volume
References
Farias JA, Frutos F, Esteban A, Flores JC, Retta A, Baltodano A, Alia I, Hatzis T, Olazarri F, Petros A, Johnson M 2004 What is the daily practice of mechanical ventilation in pediatric intensive care units? A multicenter study. Intensive Care Med 30: 918–925
Jarreau PH, Moriette G, Mussat P, Mariette C, Mohanna A, Harf A, Lorino H 1996 Patient-triggered ventilation decreases the work of breathing in neonates. Am J Respir Crit Care Med 153: 1176–1181
Cleary JP, Bernstein G, Mannino F, Heldt GP 1995 Improved oxygenation during synchronized intermittent mandatory ventilation in neonates with respiratory distress syndrome: a crossover study. J Pediatr 126: 407–411
Hummler H, Gerhardt T, Gonzales A, Claure N, Everett R, Bancalari E 1996 Influence of different methods of synchronized mechanical ventilation on ventilation, gas exchange, patient effort, and blood pressure in premature neonates. Pediatr Pulmonol 22: 305–313
Schulze A, Gerhardt T, Musante G, Schaller P, Claure N, Everett R, Gomez-Marin O, Bancalari E 1999 Proportional assist ventilation in low birth weight infants with acute respiratory disease: a comparison to assist/control and conventional mechanical ventilation. J Pediatr 135: 339–344
Greenough A, Sharma A 2005 Optimal strategies for newborn ventilation-a synthesis of the evidence. Early Hum Dev 81: 957–964
Tokioka H, Kinjo M, Hirakawa 1993 The effectiveness of pressure support ventilation for mechanical ventilatory support in children. Anesthesiology 78: 880–884.
Brochard L, Pleskwa F, Lemaire F 1987 Improved efficacy of spontaneous breathing with inspiratory pressure support. Am Rev Respir Dis 136: 411–415
Leung P, Jubran A, Tobin MJ 1997 Comparison of assisted ventilator modes on triggering, patient effort, and dyspnea. Am J Respir Crit Care Med 155: 1940–1948
Nava S, Bruschi C, Rubini F, Palo A, Iotti G, Braschi A 1995 Respiratory response and inspiratory effort during pressure support ventilation in COPD patients. Intensive Care Med 21: 871–879
Sinderby C, Navalesi P, Beck J, Skrobik Y, Comtois N, Friberg S, Gottfried SB, Lindström L 1999 Neural control of mechanical ventilation. Nat Med 5: 1433–1436
Sinderby C, Beck J, Weinberg J, Spahija J, Grassino A 1998 Voluntary activation of the human diaphragm in health and disease. J Appl Physiol 85: 2146–2158
Beck J, Sinderby C, Lindstrom L, Grassino A 1998 Effects of lung volume on diaphragm EMG signal strength during voluntary contractions 1998. J Appl Physiol 85: 1123–1134
Sinderby C, Spahija J, Beck J, Kaminski D, Yan S, Sliwinski P 2001 Diaphragm activation during exercise in chronic obstructive pulmonary disease. Am J Respir Crit Care Med 163: 1637–1641
Beck J, Sinderby C, Lindström L, Grassino A 1996 Influence of bipolar electrode positioning on measurements of human crural diaphragm EMG. J Appl Physiol 81: 1434–1449
Baydur A, Behrakis PK, Zin WA, Jaeger M, Milic-Emili J 1982 A simple method for assessing the validity of the esophageal balloon technique. Am Rev Respir Dis 126: 788–791
Allo JC, Beck JC, Brander L, Brunet F, Slutsky AS, Sinderby CA 2006 Influence of neurally adjusted ventilatory assist (NAVA) and PEEP on breathing pattern in rabbits with acute lung injury. Crit Care Med 34: 1e–8e
Sinderby CA, Beck JC, Lindström LH, Grassino AE 1997 Enhancement of signal quality in esophageal recordings of diaphragm EMG. J Appl Physiol 82: 1370–1377
Sinderby C, Lindström L, Grassino A 1995 Automatic assessment of electromyogram quality. J Appl Physiol 79: 1803–1815
Gianouli E, Webster K, Roberts D, Younes M 1999 Response of ventilator-dependent patients to different levels of pressure support and proportional assist. Am J Respir Crit Care Med 159: 1716–1725
Beck J, Tucci M, Emeriaud G, Lacroix J, Sinderby C 2004 Prolonged neural expiratory time induced by mechanical ventilation in infants. Pediatr Res 55: 747–754
Fabry B, Guttman J, Eberhard L, Bauer T, Haberthur C, Wolff G 1995 An analysis of desynchronization between spontaneously breathing patient and ventilator during inspiratory pressure support. Chest 107: 1387–1394
Beck J, Gottfried SB, Navalesi P, Skrobik Y, Comtois N, Rossini M, Sinderby C 2001 Electrical activity of the diaphragm during pressure support ventilation in acute respiratory failure. Am J Respir Crit Care Med 164: 419–424
Greenough A, Morley CJ, Davis JA 1983 Interaction of spontaneous breathing with artificial ventilation in pre-term babies. J Pediatr 103: 769–773
Field D, Milner AD, Hoplin IE 1985 Manipulation of ventilator settings to prevent active expiration against positive pressure inflation. Arch Dis Child 60: 1036–1040
Bernstein G, Heldt G, Mannino FL 1994 Increased and more consistent tidal volumes during SIMV in newborn infants. Am J Respir Crit Care Med 150: 1444–1448
Chiumello D, Pelosi P, Taccone P, Slutsky A, Gattinoni L 2003 Effect of different inspiratory rise time and cycling off criteria during pressure support ventilation in patients recovering from acute lung injury. Crit Care Med 31: 2604–2610
Kondili E, Prinianakis G, Anastasaki M, Georgopoulos D 2001 Acute effects of ventilator settings on respiratory motor output in patients with acute lung injury. Intensive Care Med 27: 1147–1157
Younes M, Kun J, Webster K, Roberts D 2002 Response of ventilator-dependent patients to delayed opening of exhalation valve. Am J Respir Crit Care Med 166: 21–30
Dimitriou G, Greenough A, Laubscher B, Yamaguchi N 2001 Comparison of airway pressure-triggered and airflow triggered ventilation in very immature infants. Acta Paediatr 90: 445–447
Nishimura M, Hess D, Kacmarek RM 1995 The response of flow-triggered infant ventilators. Am J Respir Crit Care Med 152: 1901–1909
Acknowledgements
The authors thank M. Norman Comtois for his technical assistance and Dr. Yumiko Imai for her advice on the lung injury model and Dr. Guillaume Emeriaud for reviewing the manuscript.
Author information
Authors and Affiliations
Corresponding author
Additional information
Supported in part by the Canadian Institutes for Health Research and the Canada Foundation for Innovation. These data were presented in abstract format at the American Thoracic Society meeting in May 2004.
Rights and permissions
About this article
Cite this article
Beck, J., Campoccia, F., Allo, JC. et al. Improved Synchrony and Respiratory Unloading by Neurally Adjusted Ventilatory Assist (NAVA) in Lung-Injured Rabbits. Pediatr Res 61, 289–294 (2007). https://doi.org/10.1203/01.pdr.0000257324.22406.93
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/01.pdr.0000257324.22406.93
This article is cited by
-
Comparison of extubation success using noninvasive positive pressure ventilation (NIPPV) versus noninvasive neurally adjusted ventilatory assist (NI-NAVA)
Journal of Perinatology (2020)
-
Neurally adjusted ventilatory assist mitigates ventilator-induced diaphragm injury in rabbits
Respiratory Research (2019)
-
Effects of neurally adjusted ventilatory assist on air distribution and dead space in patients with acute exacerbation of chronic obstructive pulmonary disease
Critical Care (2017)
-
Monitoring of Electrical Activity of the Diaphragm Shows Failure of T-Piece Trial Earlier than Protocol-Based Parameters in Prolonged Weaning in Non-communicative Neurological Patients
Neurocritical Care (2017)
-
Feasibility of neurally adjusted positive end-expiratory pressure in rabbits with early experimental lung injury
BMC Anesthesiology (2015)