Abstract
The objectives of the present study were to define the contribution of β2-adrenoceptors(β2-ARs) agonists to renal physiology and to investigate whether over-expression of renal β2-ARs might be implicated in the pathogenesis of renal dysfunction in children as an adverse effect of β2-AR activation. The renal functional responses to the systemic injection of the β2-AR agonist terbutaline in Wistar rats over-expressing renal β2-AR were compared with those of nontreated rats. Furthermore, we evaluated intrarenal β2-AR expression in 34 children (age 2–15 y) and the changes in serum creatinine levels of 99 children (age 1–15 y) who received β2-AR agonists. The animal study showed that the suppression of glomerular function by terbutaline was associated with a reduction in systemic blood pressure and over-expression of renal β2-ARs. Moreover, in rats over-expressing renal β2-ARs, administration of terbutaline resulted in a high mortality rate after a lipopolysaccharide challenge. The clinical study showed that renal β2-AR expression gradually increased with age and was up-regulated by steroid therapy. These findings indicate that the renal dysfunction caused by β2-AR agonists can be explained, at least partly, by enhanced β2-AR expression in the kidney. This may have important implications for the use of β2-AR agonists in the treatment of sick children with, for example, steroid therapy or endotoxemia.
Similar content being viewed by others
Main
β2-adrenoceptor (β2-AR) agonists are used as standard agents in the treatment of bronchial asthma and chronic bronchitis. The majority of the β2-AR agonists is eliminated via the kidneys in an unchanged form and it is likely that the compound will exert pharmacological effects during its passage along the nephron. However, these pharmacological effects have, to our knowledge, not been taken into consideration when using these compounds in clinical practice because the significance of β2-ARs in the regulation of renal function remains unclear.
Renal β2-ARs in the rat are predominantly localized to the renal tubular epithelia and the membranes of smooth muscle cells in the renal vasculature (1). From this morphologic evidence, the possibility arises that β2-AR activation may impact on glomerular function and thereby sodium and water handling at different nephron segments. We recently demonstrated that injection into the kidney of an adenoviral construct expressing the human β2-AR gene induced a widespread increase in β2-AR expression in the renal glomeruli and tubules, which was associated with enhanced glomerular filtration and sodium re-absorption as a consequence of over-activation of renal β2-ARs (2). Since the level of β2-AR expression will importantly determine the magnitude of β2-AR-mediated responses following administration of a β2-AR agonist (3), the density of intrarenal β2-AR expression may determine the impact of β2-AR agonists on renal function. However, there have been no studies evaluating the relationship between intrarenal β2-AR expression and the effects of β2-AR agonists on kidney function.
Major adverse effects of β2-AR agonists could occur as a result of activation of an increased density of β2-ARs (4,5) which would suggest that the level of renal β2-AR expression might be linked to detrimental effects when β2-AR agonists are given therapeutically. In an attempt to address this issue, an in vivo rat model was used in which there was an over expressions of β2-ARs, and a study undertaken, firstly, to clarify the possible role of β2-AR agonists in the regulation of glomerular filtration and secondly, to determine the significance of intrarenal over-expression of β2-ARs on the renal effects of β2-AR agonists. On the basis of these results, we explored what factors might modulate intrarenal expression of β2-ARs in physiologic and pathophysiological conditions in children and assessed potential adverse renal effects of β2-ARs agonist given therapeutically.
MATERIALS AND METHODS
Reagents.
An adenovirus Expression Vector kit was obtained from Takara Biomedicals (Shiga, Japan). [125I] cyanopindolol ([125I] CYP) was obtained from Perkin Elmar Life Science (Tokyo, Japan). Rabbit anti-human β2-AR primary antibody (β2-AR H-73, sc-9042) was obtained from Santa Cruz Biotechnology Inc. (Santa Cruz, CA). The secondary antibody(peroxidase-anti rabbit IgG polyclonal antibody) and Histofine assay kit were supplied from Nichirei corp. (Tokyo, Japan). ICI 118,551 was obtained from Funakoshi Co. (Tokyo, Japan). The cAMP ELISA kit was supplied by Amersham International Plc (Little Chalfont, Buckinghamshire, UK). Unless stated, all other reagents were obtained from Sigma Chemical Co. Chemical Co (St. Louis, MO).
Morphologic analysis.
The intrarenal distribution of β2-AR expression was determined by immunohistochemistry using a Histofine assay kit according to the protocols specified by the manufacturer (Nichirei Co., Tokyo, Japan). Renal tissues were fixed in 3% buffered formaldehyde and embedded in paraffin. Sections were cut to a thickness of 2–3 μm, blocked in 1% BSA and reacted with rabbit anti-human β2-AR antibody as a primary antibody. They were then washed in PBS and reacted with a secondary antibody which was an anti-rabbit IgG horseradish peroxidase. After washing again, the sections were reacted with diaminobenzide and counterstained with hematoxyline, dehydrated and photographed.
The distribution of β2-AR staining in the renal tubule was evaluated using an arbitrary 0 to 6+ scale. The preset grading criteria for β2-AR staining were as follows: 0+ when <10% cortical tubular cells were positive; 1+ when 10 to <20% cortical tubular cells were positive; 2+ when 20 to <30% cortical tubular cells were positive; 3+ when 30 to <40% cortical tubular cells were positive; 4+ when 40 to <50% cortical tubular cells were positive; 5+ when 50 to <60% cortical tubular cells were positive; 6+ when 60 to <80% cortical tubular cells were positive. For glomerular β2-AR staining, glomeruli in the kidney biopsies were scored semi-quantitatively by estimating a proportion of β2-AR-positive staining within the glomerulus as follows: Value 0 accounts for negative,; 1 for 1 to 50% positive; and 2 for >50% positive staining.
Biochemical measurements.
Rat serum and urine creatinine levels in rats were determined using a creatinine assay kit following the protocols specified by the Sigma Chemical Co. Chemical Co. GFR was expressed as creatinine clearance rate (Ccr, mL/min/100 g weight). Rat serum and urinary sodium (Na+) or potassium (K+) concentrations were measured using a spectrophotometer (7170, Hitachi, Japan). The fractional excretions of sodium (FENa) or of potassium (FEK) were calculated using standard formulae from the serum and urine sodium or potassium, and the serum and urine creatinine. Human samples for serum creatinine were measured using an enzymatic technique validated by the General Clinical Research Center at Teikyo University (Inter-assay coefficient of variation was 0.8%). Rat urinary cAMP was estimated using a commercially available ELISA kit, in which the assay was based on the competition between unlabelled cAMP and a fixed quantity of peroxidase-labelled cAMP for a limited number of binding sites on a cAMP specific antibody.
β2-AR binding assay.
Membrane fractions from rat tissues were extracted following the method described by Lefkowitz et al. (3) with minor modifications (2). Membrane preparations (25 μg) were incubated with [125I] CYP (15–315 pmol/L) in binding buffer, either alone, or with 20 μM alprenolol which was used for the determination of nonspecific binding. The incubation was carried out at 37°C for 1h in a total volume of 500 μL followed by rapid filtration on GF/C filters and three washings with 750 μL ice-cold binding buffer. β-AR density (Bmax) was determined using linear regression analysis of saturation isotherm data, which were linearly transformed to give a Scatchard plot (Prizm4.0, GraphPad Software Inc, CA). Receptor density (measured in femtomoles) was normalized to mg of membrane protein. The protein concentration was assayed using a micro protein determination kit.
Animal study.
All procedures and protocols were approved by the Teikyo University Guide for the Care and Use of Laboratory Animals. Four-week-old Wistar rats were fed a standard laboratory diet (126mEq of Na+/kg and 118mEq of K+/kg food) and had free access to water. Three experimental protocols were used.
Protocol 1.
To investigate the dose-dependent effect of a β2-AR agonist on blood pressure (BP) and renal function. After a 7-d acclimatization period, 5-wk-old rats were injected IP with various doses of the β2-AR agonist, terbutaline (1–10−4 × 27.4 μg/kg) or PBS. The β2-AR antagonist, ICI 118,551 (3.14 μg/kg), was given IP 2 h before the injection of terbutaline (27.4 μg/kg). The rats were housed in metabolic cages for urine collection and 24 hours later were killed after an overdose of sodium pentobarbitone. Blood and urine samples were collected for measurement of Ccr, FENa, and FEK. Systolic BP was measured at 3 h post-drug administration by means of a tail cuff sphygmomanometer using an automated system with a photoelectric sensor (KN-201-1, Natsume Seisakusho Co. Tokyo, Japan).
Protocol 2.
To investigate whether an extensive distribution of renal β2-AR expression is involved with glomerular function, adenoviral transgenes containing the human β2-AR(adeno-β2-AR) were constructed (6) and delivered into the rat kidney by means of an IP injections (2). After a 7-d acclimatization period, the rats were anesthetized with pentobarbitone (50 mg/kg, IP) and the right kidney was exposed via a retroperitoneal incision. A 50 μL sample of the virus (1 × 109 total virus particles) was injected into the right kidney using a 25-gauge needle attached to a 1 mL syringe. Four weeks after the administration of the adenoviral vector, the β2-AR agonist (terbutaline, 274 μg/kg) was injected IP into the rats. Untreated rats were injected IP with an equal volume of PBS. The rats were housed in metabolic cages for urine collection and twenty-four hours later were killed with an overdose of sodium pentobarbitone. Blood, urine, and kidneys were collected for assay. BP was monitored at 0, 3, 6, 12, 24 h after the terbutaline or PBS injections.
Protocol 3.
To investigate whether β2-AR agonists could impact on survival following an endotoxic challenge, we used a rat model of endotoxemia elicited by co-injection of terbutaline (274 μg/kg) and LPS (Escherichia coli O127:B8, 5 mg/kg). To induce a severe bacterial infection in the rats, LPS was injected IP to control and adeno-β2-AR rats 4 wk after the administration of the adenoviral vectors. The β2-AR agonist, terbutaline was administered IP 2 h before the injection of LPS. Each animal was housed in its own metabolic cage for 24 h to evaluate survival rate.
Clinical study.
The study was conducted in accordance with the Declaration of Helsinki and was approved by the Ethical Committees of Teikyo University Hospital. Two clinical studies were performed.
A primary objective was to determine the intrarenal distribution of β2-AR expression. This was done using renal tissues obtained from 53 children with hematuria and/or proteinuria who had been admitted for renal biopsies at Teikyo University Hospital between 1996 and 2004. The archival human renal biopsy samples were identified by means of immunostaining using labeling with a β2-AR antibody. Renal tissues with tubular atrophy or interstitial fibrosis and inflammation were excluded from this clinical study. To validate the distribution of β2-AR expression from 2–15 y old, we utilized the semi-quantitative grading scale of β2-AR expression in renal tissues from 23 children (control group) who had normal creatinine clearances (>80 mL/mim/1.73m2) and who had not received β2-AR agonists, steroid or immunosuppressive therapy at the time of the biopsy. Furthermore, to assess the potential effect of steroid on renal β2-AR expression, we analyzed the distribution of renal β2-AR expression in 11 children (steroid group) with nephrotic syndrome who had received standard steroid therapy (predonine or predonisolone at a dose of 2 mg/kg/d for more than 4 wk).
To estimate whether the decline in GFR was more pronounced in children treated with systemic β2-AR agonists, a retrospective chart review was conducted for 99 patients (age 1–15 y) with respiratory tract symptoms who had been enrolled in the Department of Pediatrics in Teikyo University Hospital. These patients who visited between 2003 and 2005 for upper respiratory infection, bronchitis, asthma, or pneumonia and had collected blood samples during the evening were eligible for this secondary study. Some patients (β2-AR agonist group) received oral β2-AR agonists, such as tulobuterol, 0.04 mg/kg/d, or procaterol, 1.25 μg/kg/d, or tulobuterol transdermal therapy (tulobuterol; 0.5 mg/d <15kg body weight, or 1 mg/d ≥15kg body weight) while the remainder (control group) did not receive any of these medications. Children with a history of chronic heart, lung, liver, kidney and metabolic diseases before this visit to the hospital were excluded from the study. Exclusion criteria also included treatment with steroids.
Statistics.
The results were expressed as mean ± SEM. Statistical analysis was undertaken using the ANOVA or Kruskal-Wallis test followed by a Bonferroni/Dunnett test or Scheffé test for multiple comparisons. In the time-course changes of BP and serum creatinine levels, the statistical difference was evaluated using two-way ANOVA. The unpaired t-test was used for the comparison of Ccr between ICI 118,551-treated and the nontreated rats or for comparison of β2-AR density between control and adeno-β2-AR rats. The unpaired t-test was also used for comparison of characteristics and histologic scores between control and steroid groups. The relationship between histologic scores and age or the relationship between doses of terbutaline and BP or Ccr was tested using the Spearman rank correlation analysis. Survival curves for control and adeno-β2-AR rats were generated according to the Kaplan-Meier method and compared using a log-rank test. p < 0.05 was considered statistically significant.
RESULTS
Animal study.
The findings from the protocol 1 study are presented in Fig. 1 and show that terbutaline (1–10−4 × 27.4 μg/kg) suppressed BP and Ccr in a dose-dependent way. The suppression of BP and glomerular function was prevented by the prior administration of the β2-AR antagonist, ICI 118,551, which most likely blocked β2-AR activation. These findings suggested the possibility that the action of β2-AR agonists to decrease Ccr was partially dependent on a reduction in systemic BP. On the other hand, in the terbutaline (1–10−4 × 27.4 μg/kg)-treated rats there was no significant change in FENa and FEK (data not shown).
Effects of β2-AR agonist (terbutaline) on BP and Ccr. (A) Dose-dependent BP responses 3 h after terbutaline(1–10−4 × 27.4 μg/kg) injection into rats. Each n = 4. (B) Concentration-dependent decreases in Ccr 24 h after terbutaline (1–10−4 × 27.4 μg/kg) injection into rats. All n = 4. Data are mean ± SEM. *p < 0.05 vs. rats with β2-AR antagonist (▪) or ICI 118,551 (▴ 3.14 μg/kg) injection.
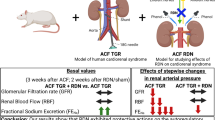
Over-expression of renal adeno-β2-ARs in vivo using IP injection of the adenoviral construct has been found to result in a widespread increase in β2-AR density within glomeruli and tubular epithelial cells (2). Indeed, using this approach in the present study, it was evident that the β-AR density of both kidneys in the adeno-β2-AR rats (499 ± 48 fmol/mg protein, n = 4) was significantly (p < 0.05) higher than that in control rats (152 ± 11 fmol/mg protein, n = 4), indicating that the administration of adeno-β2-AR had caused an over-expression of β2-AR in the kidney. The findings of the protocol 2 study are given in Fig. 2 and show the time-course changes in BP and Ccr after terbutaline injection into control rats and adeno-β2-AR-treated rats. BP levels in both rats were significantly (p < 0.05) depressed after the treatment with terbutaline, reaching the lowest level at 3 h, and then returning to baseline at 24 h. This pattern and magnitude of change were identical in both control and adeno-β2-AR-treated rats. Moreover, Ccr levels in both control and adeno-β2-AR rats were also depressed 24 h after terbutaline injection. A surprising observation was that the magnitude of the decrease in Ccr in the adeno-β2-AR-treated rats was significantly (p < 0.05) larger compared with that in the control rats (Fig. 2B).
BP and Ccr at baseline and during follow-up monitoring after terbutaline (274 μg/kg) injection in control (○) and adeno-β2-AR (▪)-treated rats. (A) Time course changes in BP after the terbutaline challenge. Each n = 4. (B) Changes in Ccr 24 h after terbutaline injection (Ter) or PBS injection (PBS). Each n = 5. Data are mean ± SEM. *p < 0.05 vs baseline (time 0). †p < 0.05 vs. control rats; §p < 0.05 vs. PBS rats.
Urinary cAMP levels were significantly (p < 0.05) increased by the addition of terbutaline in the adeno-β2-AR-treated rats but not in control rats (Fig. 3A). The findings suggested that there was an excessive activation of β2-AR in the adeno-β2-AR-treated rat kidney. The protocol 3 study demonstrated that, under conditions of renal β2-AR over-activation, 66% of the adeno-β2-AR rats which received terbutaline succumbed to the LPS challenge within 16 h (Fig. 3B, p < 0.05). In sharp contrast, although the same dose of terbutaline was injected, all of the control rats survived.
Changes in urinary cAMP and survival rates. (A) Changes in urinary cAMP levels 24 h after terbutaline (Ter: 274 μg/kg) injection or PBS injection (PBS) into control (▪) and adeno-β2-AR (•)-treated rats. Each n = 5. Data are mean ± SEM. †p < 0.05 vs. control rats; §p < 0.05 vs. PBS rats. (B) Survival rates in control and adeno-β2-AR-treated rats pretreated with LPS (5 mg/kg) and terbutaline (274 μg/kg). Mortality of rats was followed over a period of 24 h. Each n = 6.
Clinical study primary objectives: Intrarenal distribution of β2-AR expression in the kidney.
The clinical characteristics and data for the subjects in the primary study are shown in Table 1. The cause of hematuria and/or proteinuria in the control group was associated with minimal change nephropathy in 12 patients, mesangial proliferative nephropathy in two patients, Henöch-schönline purpura nephritis in 3 patients, and IgA nephropathy in 6 patients. By contrast, the histologic diagnosis in the steroid group was minimal change nephrotic syndrome in 7 patients, Henöch-schönline purpura nephritis in two patients, lupus nephritis in one patient, and IgA nephropathy in one patient. It can be seen in Table 1 that the histologic scores for renal glomerular and tubular β2-AR expression in the steroid group were higher (p < 0.05) compared with control group. Since the subjects in the steroid group were younger than those in the control group, the serum creatinine levels in the steroid group were significantly (p < 0.05) lower than those in the control group. However, there was no difference between the two groups with respect to renal characteristics (BUN (blood urea nitrogen), serum creatinine, proteinuria) and blood pressure. Figure 4 shows immunohistochemical staining for β2-AR expression in the kidney biopsies of the control and steroid groups. Immunoreactivity for the β2-AR was mainly localized in distal tubular epithelia in the control group and, to a lesser extent, in the proximal tubules of an adolescent boy (Fig. 4A), indicating that the frequency of tubular β2-ARs in the adolescent boy were higher than those in the young boy (Fig. 4C) in the physiologically normal kidney. On the other hand, in the steroid group, a high frequency of β2-ARs were detected not only in the distal nephron segments but also in proximal tubular epithelia in the renal tissue of an adolescent girl (Fig. 4B) and a young boy (Fig. 4D). In addition, we also detected some β2-AR signals in the glomeruli (Fig. 4A, B, D) although it was not possible to detect this receptor on the glomeruli of a young boy (Fig. 4C). Table 2 shows the changes in histologic scores for renal β2-AR expression and renal characteristics in the control and steroid groups with an age ranging from 2- to 15-y-old. In the control group, measurable β2-AR expression in the renal tubules was observed in children 5 y old and older, and the degree of elevation was related to increasing age.
Immunohistochemical detection of renal β2-AR expression in the control group (A) 10 y old, (C) 6 y old and steroid group (B) 11 y old and (D) 2 y old. In the control group, renal β2-AR staining was mainly found in the distal tubules (large arrow, A, C) and, to a lesser extent, in the proximal tubules and glomeruli (small arrow, A). By contrast, the kidneys in patients receiving steroid therapy showed strong staining of β2-AR in the proximal and distal tubules (large arrow, B, D) and in the glomeruli (small arrow, B, D).
Secondary objectives: Changes in serum creatinine levels.
Table 3 presents the serum creatinine levels at the time of the hospital visit and it was apparent that it gradually increased with age in both control and β2-AR agonist groups. The serum creatinine levels did not show a significant change in those individuals given systemic β2-AR agonists, but they tended to be higher compared with the control group.
DISCUSSION
In this animal study, we present two findings indicating that the decline in glomerular filtration induced by β2-AR activation could be associated with the reduction in systemic BP and over-expression of renal β2-ARs. Importantly, in adeno-β2-AR-treated rats with an enhanced β2-AR expression, the magnitude of the reduction in Ccr induced by the β2-AR agonist was larger compared with that obtained in the control rats. This finding was intriguing in that over-activation of renal β2-AR accelerated the agonist-induced renal dysfunction. Furthermore, in the adeno-β2-AR-treated rats, administration of the β2-AR agonist resulted in a marked mortality rate after the LPS challenge, suggesting that the fatal actions of β2-AR agonists must be taken into consideration when using the drug in clinical practice. Thus, the question arose as to what factors were involved in the β2-AR over-expression in the human kidney.
The expression of β2-ARs can be regulated in a variety of physiologic and pathphysiological conditions (7). Using rabbit anti-human β2-AR antiserum that had been validated to cross react with human β2-ARs and 0.033% 3′,3′-diamino benzidine tetrachloride as a chromogen, immunoreactivity was found to be mainly localized in the distal tubules of kidney biopsies from children from 2- to 15-y-old. Interestingly, with increasing age, a more extensive distribution was noted along the renal distal tubules whereas only a rather faint amount of β2-AR was found in the renal proximal tubules with increasing age. These findings demonstrated that β2-AR distribution in the human kidney, at least in the distal tubule, was age-dependent. Furthermore, the additional important finding arising from the clinical study was that an extensive distribution of β2-AR expression existed in the kidney biopsies from children receiving steroid therapy. The findings may provide evidence that the glucocorticoid is able to up-regulate the number of β2-ARs in the kidney as well as in a range of other tissues and cells (8,9). Moreover, both steroid and β2-AR were implicated on the maintenance of glomerular filtration and tubular sodium absorption. The extensive distribution of β2-AR in the tubules suggests a possibility that steroid treatment enhances the stimulatory effect of β2-AR on renal tubular activity. Taken together, the present study would indicate that β2-AR expression and distribution within the kidney were changed by age and influenced by steroid treatment. However, immunoreactivity for the β2-AR in the steroid group shown in Fig. 4 was only patients in their age group. Increasing the number of patients in the steroid group will provide more enough evidence that steroid increases β2-AR expression in the kidney.
There is increasing evidence that β2-AR agonists can reduce BP and renal function (10–12). Stephanopoulos et al. (10) reported that β2-AR agonists significantly decreased diastolic BP in children with asthma. On the other hand, Hashimoto et al. (11) indicated that urine flow, glomerular filtration, renal blood flow, free water clearance and excretion of electrolytes were reduced by administration of β2-AR agonists which was associated with a concomitant fall in systemic BP. Interestingly, in the adeno-β2-AR rats, the reduction in Ccr caused by the β2-AR agonist appeared to involve some other factors besides the fall in arterial BP, suggesting the possibility that activation of intrarenal β2-AR expression was able to modify renal function. Administration of the β2-AR agonist significantly enhanced the generation of the second-messenger cAMP via activation of renal β2-AR (13). Indeed, it was evident that there was a significant elevation in urinary cAMP in the adeno-β2-AR-treated rats, which received terbutaline. However, the mechanisms whereby renal function was modulated through intracellular signals via intrarenal β2-ARs remain unclear.
The elevation of β-AR density in the right kidney began quickly after the IP injection of the adeno-β2-AR, and reached peak levels 3–4 wks after the delivery (2). Interestingly, β-AR density in the left uninjected kidney was also increased but this took place slowly over 1–2 wks. This implied that the adenovirus from the right kidney had spread to other organs including the left kidney. In fact, an increased β2-AR expression was also found in the liver and lung. The adenovirus encoding β2-AR passed into the systemic circulation following IP injection which would have resulted in deposition in the contralateral kidney, liver and lung and caused expression in that area. Therefore, the changes of Ccr in the animal study (Protocol 2) resulted from β2-AR overexpression in both right and left kidneys. However, there was no evidence that the β2-AR system was overexpressed in the heart and vessels (aorta), suggesting that these β2-AR systems were not involved in the regulation of renal function (2).
The possible adverse effects of β2-AR agonist given by mouth and by inhalation have been discussed in earlier reports (4,5,14). Importantly, the major detrimental actions of β2-AR agonists occur as a result of excessive activation of β2-AR. This issue was addressed by examining the action of β2-AR agonists on renal function in the adeno-β2-AR rats, which showed that terbutaline caused a significant reduction of Ccr in these rats. Moreover, acute renal failure was easily induced by the LPS challenge (15) as a consequence of the fall in Ccr induced by the β2-AR agonists, which resulted in a high mortality rate in the adeno-β2-AR rat. Previously, it was suggested that the use of fenoterol was associated with asthma mortality. The mechanisms whereby fenoterol might cause the excess death were not clearly explained (7). Therefore, it may cause death either by an acute toxic effect or by other effects including renal injury and damage. In patients over-expressing β2-AR in the kidney, such as children receiving steroid therapy, the administration of β2-AR agonists may put them at particular risk for a significant adverse reaction to the drug.
In summary, the animal study emphasized the possibility that the use of β2-AR agonist was associated with major problems, such as hypotension or renal failure. Moreover, the clinical study indicated that serum creatinine levels in patients receiving β2-AR agonists were not different from those in control children, suggesting that the potential hypotension and renal dysfunction following β2-AR agonist treatment would not be a major clinical problem in children. However, these effects of β2-AR agonists may become a major adverse risk factor in sick children receiving steroid therapy or in children with sepsis who may be over-expressing renal β2-AR. An increased understanding of the pharmacological basis of β2-AR function in the kidney should provide important new information relevant to the clinical use of β2-AR agonists in airway diseases.
Abbreviations
- adeno- β2-AR:
-
Adenoviral transgenes containing the human β2-adrenoceptor
- β2-AR:
-
β2-adrenoceptors
- BP:
-
blood pressure
- BUN:
-
blood urea nitrogen
- Ccr:
-
creatinine clearance rate
- CYP:
-
cyanopindolol
- FENa:
-
fractional excretion of sodium
- FEK:
-
fractional excretion of potassium
- LPS:
-
lipopolysaccharide
- Ter:
-
terbutaline
References
Boivin V, Jahns R, Gambaryan S, Ness W, Boege F, Lohse MJ 2001 Immunofluorescent imaging of β1- and β2-adrenergic receptors in rat kidney. Kidney Int 59: 515–531
Nakamura A, Imaizumi A, Yanagawa Y, Kohsaka T, Johns EJ 2004 β2-adrenoceptor activation attenuates endotoxin-induced acute renal failure. J Am Soc Nephrol 15: 316–325
Maurice JP, Hata JA, Shah AS, White DC, McDonald PH, Dolber PC, Wilson KH, Lefkowitz RJ, Glower DD, Koch WJ 1999 Enhancement of cardiac function after adenoviral-mediated in vivo intracoronary β2-adrenergic receptor gene delivery. J Clin Invest 104: 21–29
Sears MR, Lotvall J 2005 Past, present and future-β2-adrenoceptor agonists in asthma management. Respir Med 99: 152–170
Geumei A, Miller WF, Paez PN, Gast LR 1975 Evaluation of a new oral β2-adrenoceptor stimulant bronchodilator, terbutaline. Pharmacology 13: 201–211
Kypson AP, Peppel K, Akhter SA, Lilly RE, Glower DD, Lefkowitz RJ, Koch WJ 1998 Ex vivo adenovirus-mediated gene transfer to the adult rat heart. J Thorac Cardiovasc Surg 115: 623–630
Emilien G, Maloteaux JM 1998 Current therapeutic uses and potential of β-adrenoceptor agonists and antagonists. Eur J Clin Pharmacol 53: 389–404
Davies AO, Lefkowitz RJ 1980 Corticosteroid-induced differential regulation of β-adrenergic receptors in circulating human polymorphonuclear leukocytes and mononuclear leukocytes. J Clin Endocrinol Metab 51: 599–605
Mano K, Akbarzadeh A, Townley RG 1979 Effect of hydrocortisone on β-adrenergic receptors in lung membranes. Life Sci 25: 1925–1930
Stephanopoulos DE, Monge R, Schell KH, Wyckoff P, Peterson BM 1998 Continuous intravenous terbutaline for pediatric status asthmaticus. Crit Care Med 26: 1744–1748
Hashimoto K, Shintani S, Yamashita S, Tei S, Takai M, Tsutsui M, Kawamura K, Ohkawa T, Hiyama T, Yabuuchi Y 1979 Pharmacological properties of procaterol, a newly synthesized, specific β2-adrenoceptor stimulant. Part II. Effects on the peripheral organs. Nippon Yakurigaku Zasshi 75: 333–364 (Japanese)
Lundvall J, Hillman J, Gustafsson D 1981 β-Adrenergic regulation of the capillary exchange and resistance function In: Vanhoutte PM, Lensen I (eds) Vasodilation,. Raven Press, New York, pp 107–116
Verghese MW, Synyderman R 1983 Hormonal activation of adenylate cyclase in macrophage membranes is regulated by guanine nucleotides. J Immunol 130: 869–873
Inman WH, Adelstein AM 1969 Rise and fall of asthma mortality in England and Wales in relation to use of pressurised aerosols. Lancet 2: 279–285
Nakamura A, Imaizumi A, Yanagawa Y, Niimi R, Kohsaka T, Johns EJ 2005 Adenoviral delivery of the β2-adrenoceptor gene in sepsis: a subcutaneous approach in rat for kidney protection. Clin Sci 109: 503–511
Author information
Authors and Affiliations
Corresponding author
Additional information
Supported by a Grant-in-Aid for Scientific research from the Ministry of Education, sports, Science and Technology, Japan (17590845) [A.N.].
Rights and permissions
About this article
Cite this article
Nakamura, A., Niimi, R., Imaizumi, A. et al. Renal Effects of β2-Adrenoceptor Agonist and the Clinical Analysis in Children. Pediatr Res 61, 129–133 (2007). https://doi.org/10.1203/01.pdr.0000249998.24772.3b
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/01.pdr.0000249998.24772.3b