Abstract
The fetal epidermal barrier undergoes rapid development during late gestation despite conditions injurious to the skin postnatally, i.e. prolonged exposure to water (urine) and noxious substances such as pancreatic chymotrypsin. Nevertheless, at birth, term newborns have a superb epidermal barrier. Concomitant with formation of the stratum corneum in utero, vernix caseosa forms a natural multifunctional cream separating the skin surface from the amniotic fluid with possible unique barrier properties. Therefore, we investigated the effect of native vernix, synthetic vernix, and Desitin® on penetration of chymotrypsin, a proteolytic enzyme present in both developing epidermis and meconium. α-Chymotrypsin penetration through test materials was conducted in vitro using a modified Franz diffusion cell. The presence of α-chymotrypsin in vernix and a possible inhibitory effect of vernix on α-chymotrypsin activity were investigated. Vernix films significantly impeded chymotrypsin penetration compared with controls during 24-h exposure experiments. α-Chymotryptic activity in vernix was undetectable, and vernix showed no endogenous inhibition of such activity. Both synthetic vernix and Desitin® significantly impeded α-chymotrypsin penetration compared with controls during 9-h exposure experiments. With respect to the developing epidermal barrier, these results are consistent with the hypothesis that vernix films retain endogenous (epidermal) chymotrypsin while preventing exposure to exogenous (pancreatic) chymotrypsin.
Similar content being viewed by others

Main
The intrauterine development of the human skin barrier as an interface between the internal and external environment is critical for postnatal survival of the organism. One of the most striking changes during late gestation of pregnancy is the presence of vernix caseosa on the fetal skin surface. Vernix is a viscous, whitish, pastelike material that overlies the fetal stratum corneum (1). By composition, vernix is mainly composed of water (80%), lipid (10.3%), and protein (9.1%) (2). It consists of a lipid matrix containing detached corneocytes derived from possible remnants of the epitrichium, the differentiating fetal epidermis, and the pilosebaceous unit (3,4). Vernix lipid is, thus, composed of two types of lipid: sebaceous lipid and stratum corneum lipid (5–8). The continuous (nonlamellar) phase of vernix lipid surrounding the cellular components has a low surface energy and results in a highly unwettable material located at the fetal skin surface (9). This interfacial hydrophobic material has been investigated as a defense against infection both pre- and postnatally with beneficial physicochemical properties providing barrier protection and facilitating development of the acid mantle (10–12).
Paradoxically, the fetal skin barrier undergoes rapid development during late gestation under conditions of total immersion in amniotic fluid. In vitro, skin culturists must raise human skin to an air interface to promote barrier development (13,14). This raises the biologic question of how the human fetus accomplishes this feat in utero. Amniotic fluid is a complex mixture of many bioactive constituents including electrolytes, lipids, amino acids, growth factors, cytokines, and enzymes (15,16). The presence of an unexpectedly high concentration of chymotrypsin in amniotic fluid has been reported as early as wk 18 of gestation (17). The source of this material is unknown, and its study could potentially elucidate new interactions in the fetal environment.
Chymotrypsin is a serine protease. Its activity and conformational stability are pH and temperature dependent (18,19). Maximal activity of chymotrypsin appears at pH 7–8 in contrast to its physiochemical stability, which is maximal under acidic conditions. The pH of amniotic fluid is approximately 7 (15). Consequently, the formation of the fetal epidermal barrier in amniotic fluid occurs at the optimum pH for chymotryptic activity. A functionally superb epidermal barrier is developed during late gestation, and superior epidermal barrier properties are detected in term newborn infants (20,21). It is interesting to note that epidermal barrier formation coincides with the presence of vernix formation in utero (22). This finding led us to hypothesize that vernix caseosa facilitates epidermal barrier formation and barrier homeostasis of fetal skin in utero by providing a barrier to impede the loss of biologic enzymes necessary for barrier differentiation and also by preventing the developing skin from incurring damage from noxious agents present in the intrauterine environment (Fig. 1).
Diagram showing possible sites of action of pancreatic and epidermal chymotryptic enzyme on the fetal skin surface. In utero, vernix caseosa forms a film separating the amniotic fluid compartment from the developing epidermal barrier. The inset is a section of newborn skin stained with hematoxylin and eosin. The scale bar equals 50 μm.
After birth, diaper dermatitis is the most common cutaneous disorder of infancy and early childhood. Stool chymotrypsin, in combination with other enzymes, has been reported to have a high skin irritation potential (23–25). The level of irritancy corresponds to enzyme concentration and the pH condition of the test solution. Therefore, fecal enzymes under the diaper are believed to be a primary factor leading to and perpetuating this skin disorder (26). We also hypothesized that natural endogenous barrier films such as vernix may prevent the penetration of digestive enzymes from stool. Substantiation of this hypothesis supports leaving vernix on infant skin after birth. In a similar manner, vernix may protect the fetal skin from possible deleterious effects of meconium exposure in utero.
In this work, we studied the penetration of chymotrypsin through vernix films as a function of film thickness. The presence of chymotryptic activity in vernix and the possible inhibitory effect of vernix on enzyme activity were also investigated. The barrier properties of a synthetic vernix formulation and a common commercial ointment for treatment of diaper dermatitis were also studied and contrasted to native vernix.
METHODS
Materials.
α-Chymotrypsin TLCK treated from bovine pancreas, N-benzoyl-l-tyrosine-ethyl-ester (BTEE), bovine serum albumin (BSA), calcium chloride, sodium azide, and dodecyltrimethylammonium chloride (DTMAC) were purchased from Sigma Chemical Co.-Aldrich (St. Louis, MO). Chymotrypsin was used without further purification. HT-Tuffryn membrane, a hydrophilic polysulfone membrane with a pore size of 0.45 μm was purchased from Pall Corporation (Ann Arbor, MI). Desitin®, a commercial ointment for treating diaper dermatitis, was selected as a common benchmark. Desitin® consists of zinc oxide, butylated hydroxyanisole, cod liver oil, fragrance, lanolin, methylparaben, petrolatum, talc, and water. It shows a water vapor transport value of 1.8 ± 0.5 g/m2/h (27). A synthetic vernix formulation was prepared in the laboratory as a high internal phase water-in-oil emulsion. The emulsion had a high aqueous content (78% weight) with lipid composition of squalene, linoleic acid, cholesterol, ceramide III, cholesterol sulfate, triglyceride, lanolin, and beeswax. The synthetic vernix shows a water release rate and water vapor transport comparable to those of native vernix (27).
Vernix collection and spreading.
Vernix caseosa was collected from full-term infants born at University Hospital, Cincinnati, OH, with institutional review board approval and informed consent. It was immediately transferred into sterile airtight plastic tubes and kept at 4°C until used. Portions of samples contaminated with blood were discarded. All vernix samples were used within a month after collection. Vernix was spread into a uniform film over a HT-Tuffryn membrane using a special mechanical applicator (Accu Gate Fluid Spreader). This metered gate allows the vernix to flow through thereby controlling the film thickness applied. The applicator was held at a 45-degree angle and was drawn smoothly over the vernix to produce a uniform coating in which the thickness of the film obtained depends on the depth of the gate. The film thicknesses produced were 3, 6, or 9 mils or 76.2, 152.3, and 228.6 μm, respectively (1 unit mil equals to 25.4 μm).
Measurement of chymotrypsin activity.
The activity of α-chymotrypsin was assayed by continuous spectrophotometric monitoring of the hydrolysis of BTEE described by Hummel (28). The reaction cocktail contained 1.40 mL of 1.18 mM BTEE prepared in 25% methanol, 1.42 mL of 0.1 M Tris buffer pH 7.85, and 0.08 mL of 2 M calcium chloride. The reaction cocktail was monitored using SmartSpec-3000 Spectrophotometer and equilibrated at 25°C. The enzymatic reactions were initiated by the addition of 0.1 mL enzyme solution and the increase in absorbance at 256 nm was recorded every minute for 5 min. An increase in absorbance per minute (ΔA256/min) was obtained from the maximum linear rate. ΔA256/min was converted to amount of chymotrypsin using standard curve generated by α-chymotrypsin with a concentration range of 0.4–30 μg/mL (0.031–2.33 U/mL).
Study of enzyme stability.
α-Chymotrypsin was prepared in 0.1 M of citrate buffer (0.4 mg/mL) with or without the presence of 0.25 mg/mL of BSA. Citrate buffer used was pH 3, 4, 5, and 6, and the buffer was prewarmed at 37°C before an addition of α-chymotrypsin. The enzyme solutions were then stored at 37°C in a thermostatic water bath, and an aliquot of the solution was taken at appropriate intervals for the residual activity assay described earlier.
Penetration study of chymotrypsin.
To evaluate barrier protective properties, uniform films of vernix and test materials including synthetic vernix and Desitin® were spread on to HT-Tuffryn membrane using the Accu Gate spreader. Test films were mounted on modified Franz diffusion cells between donor and receptor compartments (Fig. 2). The receptor compartments were stirred and maintained at 37°C by thermostatted heating-stirring modules. The receptor solution was 0.1 M of citrate buffer at pH 3, containing 0.25 mg/mL of BSA to prevent enzyme adsorption on the glass wall and 0.02% sodium azide to retard microbial growth. The experiment was initiated by addition of α-chymotrypsin in pH 3 0.1 M citrate buffer (0.4 mg/mL or 31.1 U/mL) into the donor chamber. Samples of receptor fluid were collected at predetermined time intervals and were replaced with an appropriate volume of buffer. The collected samples were investigated for the presence of α-chymotrypsin over time by continuous spectrophotometry. Penetration studies were carried out over a 24-h period. A Franz cell system containing only HT-Tuffryn membranes served as a control.
Presence of α-chymotrypsin in vernix.
Citrate buffer (pH 3) with either 0.26% or 0.13% DTMAC was selected as an extracting medium. One hundred milligrams of vernix was homogenized in 2 mL of extracting medium using Tissue Tearor homogenizer for at least 1 min. The resulting vernix suspension was centrifuged at 7000 rpm, and the clear supernatant was measured for the presence of α-chymotrypsin.
Inhibitory effect of vernix on α-chymotrypsin activity.
α-Chymotrypsin solution was prepared in 0.1 M of citrate buffer pH 3 to yield a concentration of either 1.55 or 31.1 U/mL. Native vernix was added to the chymotrypsin solution (50 mg/mL) and was homogenized for 1 min using a Tissue Tearor homogenizer. The experiment was conducted over ice to minimize enzyme autodegradation. After 2 h, the supernatant was removed for measurement of the remaining enzyme activity compared with control chymotrypsin solutions without the presence of vernix.
RESULTS
Enzyme stability.
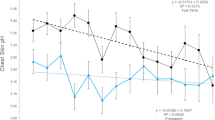
The effects of pH on the stability of α-chymotrypsin activity in citrate buffer are shown in Figure 3. The results are reported as residual activity of α-chymotrypsin with respect to initial enzyme activity in citrate buffer at pH 3, 4, 5, and 6. The activity of α-chymotrypsin decreased with increasing buffer pH. α-Chymotrypsin in buffer pH 3 at 37°C was stable for at least 24 h; therefore, citrate buffer pH 3 was selected as a medium used in the penetration study. Figure 3b shows the effect of additional protein (BSA) concentration on enzyme stability. The addition of 0.25 mg/mL of BSA did not decrease enzyme stability over 24 h and did not affect spectrophotometric measurement of enzyme activity.
(a) Effect of pH on the stability of α-chymotrypsin at 37°C. Enzymatic stability was inversely proportional to the pH of the solution. Chymotrypsin in citrate buffer pH 3 (•), 4 (○), 5 (▾), and 6 (Δ). (b) Effect of BSA on the stability of α-chymotrypsin in pH 3 citrate buffer. The addition of BSA at 0.25 mg/mL did not significantly decrease enzymatic stability. Chymotrypsin in citrate buffer pH 3 with BSA (•) and without BSA (○).
Penetration of α-chymotrypsin through test membranes.
Figure 4a shows the total cumulative amount of α-chymotrypsin penetration through vernix films of different thickness compared with the control (HT-Tuffryn membrane only). The result demonstrates that vernix, at all film thicknesses, showed a significant effect to prevent penetration of α-chymotrypsin compared with the control at all time points up to 24 h. Figure 4b presents the same data focusing on the total cumulative amount of α-chymotrypsin penetrating vernix films of different thickness. As shown, the presence of chymotrypsin was barely detectable in the receptor compartment after 1 h at all levels tested. The extent of chymotrypsin penetration was inversely proportional to vernix film thickness, but there was no significant difference among film levels at 24 h due to data scatter.
Effect of vernix films to impede penetration of α-chymotrypsin. Vernix films were spread at different film thicknesses; 0 (▪), 3 (•), 6 (Δ), and 9 (♦) mils, on HT-Tuffryn membranes. The results are reported as mean ± SE. (a) All vernix films significantly impeded chymotrypsin penetration compared with the control (HT-Tuffryn membrane), p < 0.01. (b) Chymotrypsin penetration was inversely proportional to the vernix film thickness; however, no significant differences were detected between groups (n = 3 per thickness).
Figure 5a shows α-chymotrypsin penetration through similar films of vernix, synthetic vernix, and Desitin® spread on HT-Tuffryn membrane compared with the control (HT-Tuffryn membrane). At 6 h, α-chymotrypsin penetration through all test films was at least 23-fold lower than that of the HT-Tuffryn membrane control. This result demonstrates that thin films of test materials (3 mils thick) significantly prevented penetration of α-chymotrypsin compared with controls throughout the 9-h study. Figure 5b presents the same data focusing on the total cumulative amount of α-chymotrypsin penetrating through the test material films. The presence of α-chymotrypsin was undetectable until the second hours with vernix and synthetic vernix as the test film membranes. This figure shows higher amounts of α-chymotrypsin penetrating through synthetic vernix compared with native vernix. The results, however, were not significantly different due to high variability. α-Chymotrypsin penetration through Desitin® was very low with no detectable enzyme activity at any time point of the experiment.
Comparison of effect of vernix, synthetic vernix, and Desitin® on the penetration of α-chymotrypsin. Test materials [vernix (○), synthetic vernix (▴), Desitin® (♦), and control (▪)] were spread to a thickness of 3 mils on HT-Tuffryn membrane. The results are reported as mean ± SE, n = 3 per test membrane. (a) All test materials significantly impeded α-chymotrypsin penetration compared with the control (HT-Tuffryn membrane), p < 0.001. (b) Expansion of lower panel in a.
Presence of α-chymotrypsin in native vernix.
α-Chymotrypsin activity was assayed in native vernix samples as shown in Table 1. Standard curves of α-chymotrypsin, generated using buffer containing 0.26% and 0.13% DTMAC, provided detection limits of 0.062 and 0.049 U/mL, respectively. Increasing DTMAC concentrations lowered the sensitivity of the spectrophotometric measurement, thereby affecting measurable α-chymotrypsin activity. Clear supernatant, obtained after homogenization of vernix and an extracting medium, containing either 0.26% or 0.13% DTMAC, showed values below the detection limits measured by spectrophotometric determination of absorbance at 256 nm. Therefore, 50 mg of vernix contained less than 0.049 U of α-chymotrypsin.
Inhibitory effect of vernix on α-chymotrypsin activity.
Inhibitory effect of vernix on α-chymotrypsin activity was studied in the representative experiment presented in Figure 6. Residual activity of α-chymotrypsin is presented as the percentage of relative activity compared with control. Two hours after homogenization of vernix in either 1.55 or 31.1 U/mL α-chymotrypsin, the relative activity of α-chymotrypsin compared with control remained at 98.0 ± 2.1% or 99.6 ± 2.4%, respectively. Based on these results, native vernix does not significantly inhibit α-chymotrypsin activity.
Inhibitory effect of vernix on α-chymotrypsin activity. Vernix was homogenized in either 31.1 or 1.55 U/mL α-chymotrypsin. Residual enzymatic activity was measured and reported as relative activity (%) ± SD, n = 3. Control represents chymotrypsin solution without the presence of vernix. The results show no significant inhibitory effect of vernix on enzymatic activity.
DISCUSSION
As early as wk 5 of gestation, the embryo is covered by a single-cell epithelium derived from ectoderm. By the end of the second trimester, the major structures of stratified epidermis can be detected, but stratum corneum formation is scant. Vernix caseosa is a viscous, whitish substance coating the fetal skin surface during the last trimester. Morphologically, Agorastos et al. (3) reported a cellular component of vernix, a finding confirmed and extended by our laboratory (4). Electron micrographs show the presence of fetal corneocytes surrounded by unstructured vernix lipid. The production of vernix coincides with the presence of a terminally differentiated epidermis as evidenced by the formation of the stratum corneum. These findings support a possible role of vernix in the process of barrier formation in in utero; however, the mechanism is not clearly understood. Of interest, other properties of vernix have been investigated showing antimicrobial (10,11,29,30), moisturizing (31), cleansing (32), and barrier repair (33) properties.
In the process of terminal differentiation, several metabolic enzymes are required for formation of a competent epidermal barrier. Phospholipase-A2, β-glucocerebosidase, and stratum corneum chymotryptic enzyme (SCCE) are major enzymes responsible for barrier differentiation and homeostasis. Phospholipase-A2 and β-glucocerebosidase are required for the transformation of phospholipids into free fatty acids (FFAs) and of glycosylceramides into ceramides, respectively. An increase in FFAs and ceramides within the interstices of the stratum corneum leads to formation of intercellular lamellar units, which are critical for the epidermal permeability barrier (34). SCCE is known to contribute to the cell shedding process by catalyzing the degradation of intercellular cohesive structures, i.e. corneodesmosomes, at the skin surface (35). This process, known as desquamation, precisely matches the continuous de novo production of the epidermal barrier from the underlying nucleated epidermal cells.
Given the critical role of SCCE in desquamation, loss of this enzyme could lead to corneocyte retention and hyperkeratosis as is commonly seen in certain skin disorders (36). Overexpression of SCCE may result in deterioration of stratum corneum integrity and cohesion (37). Hachem et al. (37) have shown that an increase in serine protease activity provokes a significant decrease in the density of corneodesmosomes, which can be reversed by a co-application of serine protease inhibitor. Therefore, an imbalance of SCCE by either over- or underexpression may play a significant part in impaired permeability function and skin pathophysiology.
The fetal skin barrier develops during late gestation in a totally aqueous environment. Given the fact that the external surface of the fetal organism directly faces the amniotic fluid, dilution or depletion of enzymes required for barrier development can hypothetically occur (Fig. 1b). The present study, therefore, focuses on the barrier effect of vernix on the penetration of SCCE. Bovine chymotryptic enzyme was used as a model for human SCCE in the experiments because it has a size, structure, and catalytic activity similar to those of SCCE (38). The results demonstrate for the first time that vernix functions as a natural barrier to impede penetration of chymotryptic enzymes. Hypothetically, a surface film of vernix in utero, positioned between the fetus and the amniotic fluid, impedes the loss of chymotryptic enzyme (SCCE) from the developing fetal barrier, thereby providing an optimum concentration of enzyme for desquamation. Whether such desquamation occurs prenatally or postnatally is unknown. Vernix itself contains numerous corneocytes (4), but it is not known whether these cells arise from the pilosebaceous unit or the interfollicular epidermis.
In addition to the presence of SCCE within the fetal epidermal barrier, chymotryptic enzymes have been identified in amniotic fluid during mid gestation (17). The source of chymotrypsin in amniotic fluid is unknown (Fig. 1a). Pancreatic chymotrypsin is a normal constituent of fetal feces (meconium). Chymotrypsin in combination with other lipolytic and proteolytic enzymes present in meconium has been reported to possess barrier irritation potential in vivo (23,24,39). The degree of irritancy corresponds to the enzyme concentration and the pH of the environment (23). Low concentrations of proteolytic enzymes under alkaline conditions cause as much skin irritation as high enzymatic concentrations under acidic conditions (23). Due to the protective property demonstrated in this study, vernix not only potentially prevents the loss of epidermal chymotryptic enzyme required for barrier homeostasis but also protects the nascent fetal barrier from damage caused by potentially harmful chymotryptic enzymes present in amniotic fluid. No inhibitory effect of vernix on chymotryptic activity was detected. The protective barrier properties of vernix, therefore, are due to mechanical obstruction or occlusion. Taken altogether, the results indicate a novel mechanism whereby natural skin creams may regulate fetal barrier homeostasis in utero.
In the extrauterine environment, the ability of vernix to prevent penetration of chymotrypsin may also be beneficial for the infant. Leaving vernix in situ at the time of birth may protect infant skin from exogenous contact with stool chymotrypsin and other noxious agents present in feces or urine. Chymotrypsin, in the presence of alkaline urine within the diaper area, has been reported to be a primary factor causing the skin irritation seen in diaper dermatitis (26). The protective barrier property of vernix can be closely matched by other nonnatural barrier films. Thus, a formulated synthetic vernix as well as Desitin®, a commercial ointment for treating diaper dermatitis, partially prevented or completely blocked chymotrypsin penetration, respectively (Fig. 5). It can be inferred from our results that native vernix, synthetic vernix, and Desitin® may potentially prevent or alleviate diaper dermatitis or other skin disorders caused by the irritating effect of chymotryptic enzyme. Of note, vernix and its synthetic equivalent are approximately 10 times less occlusive to water vapor transport than commercial lipid ointments, such as Desitin® (see Materials section). Vernix films provide a water vapor transport in the range reported to facilitate barrier repair (40). Total occlusion of the skin by vapor impermeable ointments has been shown to increase microbial infection of immature skin and to hinder barrier repair (41–43). Because the management and prevention of diaper dermatitis aim to keep the area dry, to prevent long-term contact with urine or fecal enzymes, and to promote barrier repair of damaged skin, therefore, either native vernix or synthetic vernix formulations may have advantages over commercial ointments such as of Desitin®.
In conclusion, this study shows that thin films of a naturally occurring emollient, vernix caseosa, provide a protective barrier to penetration of potentially injurious substances such as chymotryptic enzyme. This property is due to mechanical obstruction rather than enzyme inhibition. Native vernix itself contains no detectable enzyme activity. A thin film of vernix in utero, therefore, may function to prevent loss of endogenous chymotrypsin from the underlying epidermis while preserving the microstructure of developing stratum corneum and protecting the epidermal barrier from noxious substances in the amniotic fluid. The multifunctionality of vernix supports the recommendation that vernix be left in place on the skin surface at birth.
Abbreviations
- BTEE:
-
N-benzoyl-l-tyrosine-ethyl-ester
- DTMAC:
-
dodecyltrimethyl ammonium chloride
- ΔA256/min:
-
increase in absorbance per minute
- SCCE:
-
stratum corneum chymotryptic enzyme
References
Holbrook KA, Hoff MS 1984 Structure of the developing human-embryonic and fetal skin. Semin Dermatol 3: 185–202
Hoeger PH, Schreiner V, Klaassen IA, Enzmann CC, Friedrichs K, Bleck O 2002 Epidermal barrier lipids in human vernix caseosa: corresponding ceramide pattern in vernix and fetal skin. Br J Dermatol 146: 194–201
Agorastos T, Hollweg G, Grussendorf EI, Papaloucas A 1988 Features of vernix caseosa cells. Am J Perinatol 5: 253–259
Pickens WL, Warner RR, Boissy YL, Boissy RE, Hoath SB 2000 Characterization of vernix caseosa: water content, morphology, and elemental analysis. J Invest Dermatol 115: 875–881
Nicolaides N 1971 The structures of the branched fatty acids in the wax esters of vernix caseosa. Lipids 6: 901–905
Downing DT, Strauss JS 1974 Synthesis and composition of surface lipids of human skin. J Invest Dermatol 62: 228–244
Rissmann R, Groenink H, Weerheim A, Hoath S, Ponec M, Bouwstra J 2006 New insights into ultrastructure, lipid composition and organization of vernix caseosa. J Invest Dermatol 126: 1823–1833
Oku H, Mimura K, Tokitsu Y, Onaga K, Iwasaki H, Chinen I 2000 Biased distribution of the branched-chain fatty acids in ceramides of vernix caseosa. Lipids 35: 373–381
Youssef W, Wickett RR, Hoath S 2001 Surface free energy characterization of vernix caseosa. Potential role in waterproofing the newborn infant. Skin Res Technol 7: 10–17
Akinbi HT, Narendran V, Pass AK, Markart P, Hoath S 2004 Host defense proteins in vernix caseosa and amniotic fluid. Am J Obstet Gynecol 191: 2090–2096
Yoshio H, Tollin M, Gudmundsson GH, Lagercrantz H, Jornvall H, Marchini G, Agerberth B 2003 Antimicrobial polypeptides of human vernix caseosa and amniotic fluid: implications for newborn innate defense. Pediatr Res 53: 211–216
Visscher MO, Narendran V, Pickens W, Laruffa AA, Meinzen-Derr J, Allen K, Hoath S 2005 Vernix caseosa in neonatal adaptation. J Perinatol 25: 440–446
Fartasch M, Ponec M 1994 Improved barrier structure formation in air-exposed human keratinocyte culture systems. J Invest Dermatol 102: 366–374
Supp AP, Wickett RR, Swope VB, Harriger MD, Hoath SB, Boyce ST 1999 Incubation of cultured skin substitutes in reduced humidity promotes cornification in vitro and stable engraftment in athymic mice. Wound Repair Regen 7: 226–237
Lentner C 1981 Geigy Scientific Tables, Unit of Measurement, Body Fluids, Composition of the Body, Nutrition. Ciba-Geigy Corporation West Caldwell 197–212
Gulbis B, Gervy C, Jauniaux E 1998 Amniotic fluid biochemistry in second-trimester trisomic pregnancies: relationships to fetal organ maturation and dysfunction. Early Hum Dev 52: 211–219
Carrere J, Figarella C, Guy O, Thouvenot JP 1986 Human pancreatic chymotrypsinogen A: a non competitive enzyme immunoassay, and molecular forms in serum and amniotic fluid. Biochim Biophys Acta 883: 46–53
Lozano P, Diego T, Iborra JL 1997 Dynamic Structure/function relationships in the a-chymotrypsin deactivation process by heat and pH. Eur J Biochem 248: 80–85
Simon LM, Laszlo K, Kotorman M, Szajani B 2001 A comparative study of the conformational stabilities of trypsin and chymotrypsin. Acta Biol Szegediensis 45: 43–49
Rutter N, Hull D 1979 Water loss from the skin of term and preterm babies. Arch Dis Child 54: 858–868
Harpin VA, Rutter N 1983 Barrier properties of the newborn infant's skin. J Pediatr 102: 419–425
Hardman MJ, Moore L, Ferguson MJ, Byrne C 1999 Barrier formation in the human fetus is patterned. J Invest Dermatol 113: 1106–1113
Andersen PH, Bucher AP, Saeed L, Lee PC, Davis JA, Maibach HI 1994 Faecal enzymes: in vivo human skin irritation. Contact Dermatitis 30: 152–158
Scott A 1958 A study of the action of chymotrypsin on the skin. J Invest Dermatol 30: 201–205
Visscher MO, Hoath SB 2003 Diaper dermatitis. Maibach AH Handbook of Irritant Dermatitis. Springer-Verlag Berlin 37–51
Berg RW 1988 Etiology and pathophysiology of diaper dermatitis. Adv Dermatol 3: 75–98
Tansirikongkol A 2006 Development of a synthetic vernix equivalent, and its water handling and barrier protective properties in comparison with vernix caseosa. Dissertation, University of Cincinnati Cincinnati, OH
Hummel BW 1959 A modified spectrophotometric determination of chymotrypsin, trypsin and thrombin. Can J Physiol Pharmacol 37: 1393–1399
Marchini G, Lindow S, Brismar H, Stabi B, Berggren V, Ulfgren AK, Lonne-Rahm S, Agerberth B, Gudmundsson GH 2002 The newborn infant is protected by an innate antimicrobial barrier: peptide antibiotics are present in the skin and vernix caseosa. Br J Dermatol 147: 1127–1134
Tollin M, Bergsson G, Kai-Larsen Y, Lengqvist J, Sjovall J, Griffiths W, Skuladottir GV, Haraldsson A, Jornvall H, Gudmundsson GH, Agerberth B 2005 Vernix caseosa as a multi-component defense system based on polypeptides, lipids and their interactions. Cell Mol Life Sci 62: 2390–2399
Bautista MI, Wickett RR, Visscher MO, Pickens WL, Hoath SB 2000 Characterization of vernix caseosa as a natural biofilm: comparison to standard oil-based ointments. Pediatr Dermatol 17: 253–260
Moraille R, Pickens W, Visscher MO, Hoath S 2005 A novel role for vernix caseosa as a skin cleanser. Biol Neonate 87: 8–14
Hoath SB, Pickens W 2003 The biology of vernix. Hoath SB, Maibach H Neonatal Skin: Structure and Function. Marcel Dekker New York 193–210
Madison KC 2003 Barrier function of the skin: “La Raison d'Etre” of the epidermis. J Invest Dermatol 121: 231–241
Horikoshi T, Igarashi S, Uchiwa H, Brysk H, Brysk MM 1999 Role of endogenous cathepsin D-like, and chymotrypsin-like proteolysis in human epidermis desquamation. Br J Dermatol 141: 453–459
Johnson B, Horn T, Sander C, Kohler S, Smoller BR 2003 Expression of stratum corneum chymotryptic enzyme in ichthyoses and squamoproliferative processes. J Cutan Pathol 30: 358–362
Hachem JP, Crumrine D, Fluhr J, Brown BE, Feingold KR, Elias PM 2003 pH directly regulates epidermal permeability barrier homeostasis, and stratum corneum integrity/cohesion. J Invest Dermatol 121: 345–353
Skytt A, Stromqvist M, Egelrud T 1995 Primary substrate of recombinant human stratum corneum chymotryptic enzyme. Biochem Biophys Res Commun 211: 586–589
Caplan RM 1966 The irritant role of feces in the genesis of perianal itch. Gastroenterology 50: 19–23
Visscher M, Hoath SB, Conroy E, Wickett RR 2001 Effect of semipermeable membranes on skin barrier repair following tape stripping. Arch Dermatol Res 293: 491–499
Edwards WH, Conner JM, Soll RF 2004 The effect of prophylactic ointment therapy on nosocomial sepsis rates and skin integrity in infants with birth weight of 501 to 1000 g. Pediatrics 113: 1195–1203
Aly R, Shirley C, Cunico B, Maibach HI 1978 Effect of prolonged occlusion on the microbial flora, pH, carbon dioxide and transepidermal water loss on human skin. J Invest Dermatol 71: 378–381
Proksch E, Holleran WM, Menon GK, Elias PM, Feingold KR 1993 Barrier function regulates epidermal lipid and DNA synthesis. Br J Dermatol 128: 473–482
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Tansirikongkol, A., Wickett, R., Visscher, M. et al. Effect of Vernix Caseosa on the Penetration of Chymotryptic Enzyme: Potential Role in Epidermal Barrier Development. Pediatr Res 62, 49–53 (2007). https://doi.org/10.1203/PDR.0b013e318067b442
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/PDR.0b013e318067b442
This article is cited by
-
Clustering-based preprocessing method for lipidomic data analysis: application for the evolution of newborn skin surface lipids from birth until 6 months
Analytical and Bioanalytical Chemistry (2018)