Abstract
In the two conditions juvenile polyps (JPs) and juvenile polyposis coli (JPC), colonic polyps may have overlapping histologic and phenotypic appearance, but JPC confers a significant risk for colon adenocarcinoma. Although not thought to contain adenomatous polyposis coli (APC) mutations, the status of β-catenin and full-length APC protein expression in JPs is not known. We evaluated β-catenin and full-length APC protein expression in JPs from children with JPs and JPC. Cases were identified through endoscopic procedure records. Immunohistochemistry was performed for β-catenin and full-length APC protein. Loss of heterozygosity at the APC gene locus on chromosome 5 was assessed using two APC-linked microsatellite markers. Polyp and normal colonic tissue were analyzed from 36 children with JPs and 9 with JPC. Both APC and β-catenin immunoreactivity were present in epithelial cells from all samples but in different patterns. In all normal colon and polyp samples, APC expression was cytoplasmic with maximal immunoreactivity in the goblet cells. In contrast, β-catenin immunoreactivity in epithelial cells was limited to the plasma membrane in normal colon but was both cytoplasmic and nuclear in all 45 JPs. No evidence of APC gene loss of heterozygosity was found. In polyps from children with JPs and JPC, nuclear β-catenin accumulation is a consistent feature, and it is not due to APC gene mutation or loss of full-length APC protein expression. Thus, β-catenin accumulation may be intrinsic to the formation of juvenile-type polyps through an as-yet-undefined mechanism.
Similar content being viewed by others
Main
Juvenile polyps (JPs; MIM 174900) are the most common type of colonic polyp in childhood. The polyps are usually composed of normal or cystically dilated crypts embedded in an abundant lamina propria (1). JPs are both histologically and genetically distinct from colonic adenomas. Whereas a great deal is known about the genetic progression that occurs during the adenoma-carcinoma sequence, less is known about the genetic alterations that occur in JPs.
Inactivation of both adenomatous polyposis coli (APC) alleles is thought to be an early event in the adenoma-to-carcinoma sequence (2). Truncating mutations, loss of heterozygosity (LOH), and hypermethylation of APC all would be expected to lead to loss of full-length APC protein. Thus, measurement of full-length APC protein can be used to screen tissues for the common causes of loss of APC function. One of the known functions of the normal APC protein is to facilitate the phosphorylation and degradation of β-catenin (3,4), and loss of APC function is thought to be responsible for the nuclear accumulation of β-catenin in colonic adenomas.
The molecular genetics of JPs are less well characterized than that of adenomatous polyps. Germline mutations in the SMAD-4 (5), bone morphogenic receptor 1A (6), and PTEN genes (7–9) have been reported in some but not all kindreds with multiple JPs (10,11). Neither germline nor somatic mutations in the APC gene have been commonly found in patients with JPs (12). We examined the status of β-catenin and full-length APC protein expression in JPs from children with largely solitary JPs and multiple juvenile polyposis coli (JPC) JPs in the colon.
METHODS
Patient selection.
Patients with JPs were identified through the records of endoscopic procedures performed at The Children's Hospital (Denver, CO) between January 1995 and September 1999 and from Jichi Medical School (Tochigi, Japan) between April 1996 and September 1998. In all cases, diagnosis was made from the clinical history, endoscopy, and histopathologic examination.
Data from follow-up procedures performed during the study period were included; however, routine follow-up or surveillance procedures were not conducted in all children. Demographic data were abstracted from the medical records. Once the required clinical data were obtained, the tissue samples were de-identified before immunohistochemical or genetic analysis.
Polyp descriptions.
One polyp from each patient was used for this study. The number of polyps was defined as the total number documented, whether at initial or subsequent procedures. Anatomic description was recorded as anorectal (distal, 4 cm); rectosigmoid, left-sided when found in the splenic flexure and/or descending colon, right-sided when found proximal to the splenic flexure (transverse colon, ascending colon, or cecum); and pan-colonic when found both distal and proximal to the splenic flexure.
Definition of the conditions JPs and JPC.
A JP was defined as a rounded, largely solitary (1–5) polypoid mass, with typical histologic features of a JP: crypts lined by mature epithelium and cysts distended with mucin and lined by nondysplastic epithelium, with lamina propria containing acute and chronic inflammation, sometimes with hemorrhage and granulation tissue (13). JPC was defined as the presence of 10 of more JPs or the presence of at least 1 JP in a first-degree relative of an index case of JPC (14). Familial JPC was defined as two or more first-degree relatives with JPC.
Tissue samples.
Polyp tissue was obtained from 45 children with JPs, 36 unrelated patients with JPs, and 9 children from 7 different families with JPC. Samples of polyps and adjacent normal mucosa from all patients were analyzed.
Tissue preparation and antigen retrieval.
APC and β-catenin immunohistochemistry was performed on formalin-fixed, paraffin-embedded tissue using an antigen retrieval protocol as previously described (15). Serial sections (5 μm) were cut, deparaffinized in Hemo-D (Fisher Scientific, Houston, TX) and rehydrated in a series of graded alcohol:water solutions. Slides were then immersed in a 10× citrate buffer solution (Biogenex, San Ramon, CA) diluted 1:10 in distilled water and placed in a pressure cooker that contained water. Slides were microwaved for 20 min at high power, allowed to cool, then washed in Tris-buffered saline [TBS; 0.05 M of Tris and 0.15 M of NaCl (pH 7.6)].
Full-length APC immunohistochemistry.
APC immunohistochemistry was performed using a rabbit polyclonal anti-APC antibody that recognizes the last 20 amino acids of the C-terminus of the human APC protein (Santa Cruz Biotechnology, Santa Cruz, CA) and an avidin/biotin/immunoperoxidase method (15). After antigen retrieval, endogenous peroxidase activity was blocked by treating sections with 3% hydrogen peroxide in methanol for 10 min. Endogenous biotin was blocked with the Avidin/Biotin Blocking Kit (BioGenex) before incubation in Powerblock (BioGenex) diluted 1:10 in TBS that contained 1% BSA (Sigma Chemical Co., St. Louis, MO) and 0.05% Tween 20 (Sigma Chemical Co.) (TBX) for 15 min. Albumin was added to Power Block reagent to reduce the nonspecific background staining. Sections were then incubated for 1 h with a rabbit polyclonal anti-APC antibody diluted 1:200 (1 μg/mL) in TBX followed by washing in TBS (3× 5 min) and then incubated with biotinylated goat anti-rabbit IgG (Zymed, San Francisco, CA) diluted 1:200 in TBX for 30 min. After washing with TBS (3× 5 min), the Vectastain ABC kit (Vector Laboratories, Burlingame, CA) was used for detection with diaminobenzidine tetrahydrochloride (Biogenex) as the substrate. Negative control sections of each sample were incubated with 5 μg/mL of nonimmune rabbit IgG (Zymed) in place of a rabbit polyclonal anti-APC antibody. The specificity of the anti-APC antibody was also tested by absorption with a peptide corresponding to the last 20 amino acids of the C-terminus of human APC protein and by absorption with 1% agarose to exclude nonspecific binding of the polyclonal antibody to mucin. Slides were lightly counterstained with hematoxylin, dehydrated, and viewed under a light microscope. Tissues were graded positive for APC when definite brown staining was present in >10% of the epithelial cells.
β-Catenin immunohistochemistry.
β-Catenin immunohistochemistry was performed as previously described using a mouse monoclonal anti–β-catenin antibody (Transduction Laboratories, Lexington, KY) and an indirect immuno-alkaline phosphatase method (15). After antigen retrieval as described above, sections were incubated in Powerblock (Biogenex) diluted 1:10 in TBX for 15 min, followed by incubation with the mouse monoclonal anti–β-catenin antibody, diluted 1:50 (5 μg/mL) in TBX for 2 h. Sections were then washed with TBS (3× 5 min), followed by incubation with the secondary antibody, rabbit anti-mouse IgG (Dako, Glostrup, Denmark) diluted in PBS that contained 40% human serum (Gemini, Lexington, CA) for 30 min. Sections were then washed with TBS (3× 5 min) and incubated with an alkaline phosphatase–mouse anti-alkaline phosphatase complex [3.6 U/mL of alkaline phosphatase (Sigma Chemical Co.), 1% BSA, and 10% RU6 mouse antibody (Tissue Culture/Monoclonal Antibody Core Facility, University of Colorado Cancer Center, Denver, CO) in 0.05 M of Tris (pH 8.7)] for 1 h followed by signal detection using the substrate new fuchsin (Sigma Chemical Co.). Negative control sections of each sample were incubated with 1 μg/mL of nonimmune mouse IgG (Dako) in place of the anti–β-catenin antibody. Slides were then counterstained with hematoxylin, dehydrated, and viewed under light microscope. Tissues were graded positive for nuclear β-catenin when nuclear immunoreactivity was present in >10% of the epithelial cells.
LOH at APC loci.
Cystic epithelium and lamina propria domains were separated by microdissection of the paraffin-embedded JPs using a sterile scalpel blade. DNA was extracted and purified using ethanol, Gene Releaser (Murfeesboro, TN), and proteinase K. The DNA was then amplified using 32P-labeled primers targeting the microsatellites D5S346 and D5S107, both surrounding the APC gene locus on chromosome 5. The PCR products were electrophoresed on a 6% polyacrylamide gel, dried, and exposed via a phosphorimager screen (Molecular Dynamics, Sunnyvale, CA).
Statistical analysis.
Statistical analyses were performed using Statistical Analysis System (SAS) Version 6.13. Mann-Whitney test was used for comparisons of continuous variables between groups. A p < 0.05 was considered significant.
The study was approved by both the Colorado Multiple Institutional Review Board and the Jichi Medical School Review Board. Informed consent was not required.
RESULTS
During the study period, 45 children with colonic JPs were identified: 9 (20%) had JPC and 36 (80%) had JPs. The mean age was 5.2 ± 3.2 y (range 1.0–17.0). The children with JPs were on average younger than those with JPC (64% of the JP group were <5 y of age compared with 11% of the JPC group; p < 0.05). There were no differences in gender or ethnicity between the two groups.
Rectal bleeding was a presenting complaint in almost all children (98% of JPC and 100% of JPs). As expected, children with JPC had more polyps than those with JPs (median 17 versus 1.4, respectively; p = 0.003). Of the nine children with JPC, five had 10 or more polyps. The other four children with JPC had <10 polyps but were relatives of index cases with JPC. Polyps were confined to the left side of the colon (anorectal, rectosigmoid, or descending) in 96% in the JP group, whereas all nine children with JPC had a pan-colonic distribution of polyps. The mean symptom duration (7–8 mo) was similar in both the JP and JPC groups.
APC immunohistochemistry.
APC immunoreactivity was present in ≥80% of cells from normal colonic tissue from all 45 samples (Fig. 1A). Maximal APC immunoreactivity was present in the cytoplasm of goblet cells but was absent from the mucus vacuoles. It is not clear why full-length APC is maximally expressed in the goblet cell lineage, but this is the same pattern that we have reported in adult colonic mucosa (15). APC immunoreactivity was present at all levels of the colonic crypt, with similar staining intensity along the length of the crypt. There were no major differences in the pattern of APC immunoreactivity between samples from the proximal and distal colon. The overall pattern of APC immunoreactivity is similar to that reported in the normal colonic mucosa of adults (15). No immunoreactivity was present in sections that were treated with nonimmune rabbit IgG, in place of the anti-APC antibody (negative control). The APC immunoreactivity was totally absorbed by incubation with the immunizing peptide, but no loss of staining was observed after absorption with 1% agarose.
Immunohistochemical staining of normal colonic tissues adjacent to a JP using a rabbit polyclonal anti-APC antibody (A; brown chromogen) and a mouse monoclonal anti–β-catenin antibody (B; red chromogen). (C) Negative control for APC using the rabbit polyclonal anti-APC antibody absorbed with the C-terminal 20–amino acid peptide of APC. (D) Negative control for β-catenin using an isotype-specific irrelevant mouse MAb. (A) Maximal APC immunoreactivity is present in the cytoplasm of goblet cells. (B) β-catenin immunoreactivity is predominantly localized to the plasma membrane without nuclear accumulation. Magnification: ×20. All slides were counterstained with hematoxylin.
Abundant APC immunoreactivity was present in the epithelial cells of all 45 JPs examined (Fig. 2A and C). No APC immunoreactivity was present in cells of the stroma. No staining was observed when nonimmune rabbit IgG was used in place of the anti-APC antibody (Fig. 2E). There was no difference in the pattern or intensity of the APC immunoreactivity between polyps from children with JPs and those with JPC (Fig. 3A and C).
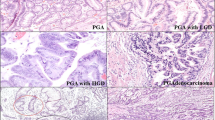
Immunohistochemical staining of a JP using a rabbit polyclonal anti-APC antibody (A and C; brown chromogen) and a mouse monoclonal anti–β-catenin antibody (B and D; red chromogen). APC immunoreactivity is present in the cytoplasm of epithelial cells of the JPs (A and C), whereas β-catenin immunoreactivity is present in both the cytoplasm and the nucleus of the epithelial cells (B and D). No immunoreactivity is present in negative control slides that were stained with nonimmune rabbit IgG (E) and nonimmune mouse IgG (F). Magnification: ×40 in A and B; ×20 in C–F; ×60 in insets in A–D. All slides were counterstained with hematoxylin.
Immunohistochemical staining of a polyp from a child with JPC and from a child with a JP using a rabbit polyclonal anti-APC antibody (A and C; brown chromogen) and a mouse monoclonal anti–β-catenin antibody (B and D; red chromogen). APC immunoreactivity is present in the cytoplasm of epithelial cells of the JPC (A) and JP (C), whereas β-catenin immunoreactivity is present in both the cytoplasm and the nucleus of the epithelial cells (B and D). Magnification: ×100.
β-Catenin immunohistochemistry.
In the normal colon, β-catenin expression was predominantly localized to the plasma membrane at all levels of the colonic crypt (Fig. 1B). No nuclear β-catenin was seen in cells at any level of the crypt. There was no significant difference in β-catenin staining pattern between the proximal and distal colonic mucosa. This pattern of immunoreactivity was seen in all 45 samples of the normal colon examined and is similar to that previously reported in the normal mucosa of adults (15).
In all 45 of the JPs, abundant β-catenin immunoreactivity was present in both the cytoplasm and the nucleus of epithelial cells (Fig. 2B and D). The cytoplasmic and nuclear β-catenin immunoreactivity was present in >80% of the epithelial cells in 42 (93%) of 45 (Fig. 2D) and in ˜50% of the epithelial cells in 3 (7%) of 45 (Fig. 2B). There was no difference in the β-catenin staining pattern in the polyps from children with JPs compared with JPC (Fig. 3B and D). No staining was observed when nonimmune mouse IgG was used in place of the anti–β-catenin antibody (Fig. 2F).
APC LOH. Adequate epithelial and normal tissue was obtained to analyze 15 of the JPs for LOH at the APC locus. The 15 samples included 9 JPs and 6 JPC polyps. LOH at the APC locus was not detected in any of the samples (Fig. 4). Two of the polyps showed evidence of microsatellite instability at the APC locus.
LOH analysis at the APC locus in JPs. Three domains from each of seven polyps were microdissected, from which DNA was extracted and amplified at two loci associated with APC: D5S107 (A) and D5S346 (B). Domains 1 and 2 from each polyp are from cystic epithelium, and domain 3 was taken from the lamina propria. Lane 4-2 did not amplify in either gel. There was no evidence of LOH at the APC gene locus from six of the polyps, with cystic epithelium from sample 5-2 demonstrating microsatellite instability (J.C., unpublished observation). In sample 7-2, LOH is not fully excluded at D5S107, but this is extremely unlikely as a result of the expression of full-length APC within the epithelium of this polyp, the presence of both alleles in D5S346, and an uncharacteristic pattern of LOH preceding APC mutation on the opposite allele. Thus, the allele change in 7-2 (D5S107) likely represents microsatellite instability, not LOH. Domains were compared for the presence of both alleles, with the lamina propria considered the normal tissue. In all 15 polyps examined, the lamina propria alleles matched those alleles of one of the epithelial domains microdissected.
DISCUSSION
In this article, we report evidence of common dysregulation of β-catenin in the epithelial cells of JPs from children with both single or few (JP) and multiple (JPC) JPs. JPs are hamartomas that have a distinctive composition of nondysplastic-appearing epithelial cells, with mucus filled and cystically dilated glands embedded in an inflamed-appearing lamina propria. The epithelial cells of some JPs undergo dysplastic or adenomatous transformation (14), and dysplastic changes are seen more commonly in JPC than in JPs (16).
Some families with JPC have germline mutations in the SMAD-4 gene (17), which codes for a transcription factor that mediates the regulatory activity of transforming growth factor-β (TGF-β) (5). TGF-β is normally an antiproliferative factor for epithelial cells. Therefore, biallelic loss of SMAD-4 function might lead to unregulated growth of the affected cells. Other germline mutations linked to familial JPC include the PTEN gene, which codes for a phospholipid and phosphoprotein phosphatase (7,8), and the bone morphogenic receptor 1A gene, which codes for a serine threonine kinase receptor (a member of the TGF-β receptor SMAD superfamily) (6). Neither the biochemical consequences of these germline mutations nor the other somatic mutational events that occur in JPs are fully known.
Nuclear β-catenin accumulation occurs commonly in colonic adenomas (15), where it is thought to be due to biallelic loss of APC function (2,18). In adenomas, dysregulation of β-catenin is thought to be integral to the process of carcinogenesis by leading to activation of the Tcf/Lef transcription factor and increased transcription of pro-proliferative genes such as myc and cyclin D1. We have now demonstrated the same type of dysregulation of β-catenin in the nondysplastic epithelial cells of JPs, but in this case, it seems to be independent of loss of APC function because abundant full-length APC protein is present in the epithelial cells, no evidence of APC LOH was found, and a previous study of one family did not find APC mutations in JPs (12). Thus, β-catenin accumulation independent of APC occurs commonly in JPs, and it could be one of the earliest steps in the development of JPs.
Our β-catenin immunohistochemical results are somewhat different from the only previous report of β-catenin localization in JPs. Back et al. (19) found focal nuclear accumulation of β-catenin in all six polyps from patients with JPC and in four of seven solitary JPs. The authors concluded that APC gene mutations could, in theory, explain their finding of nuclear β-catenin in polyps from patients with juvenile polyposis but noted that APC mutations were not commonly found in hamartomas. Our results strongly suggest that the nuclear accumulation of β-catenin in JPs is not due to biallelic inactivation of the APC gene, because abundant full-length APC protein was present in all of the JPs examined and no evidence of LOH of APC was detected in any of the JPs tested. The possibility that β-catenin accumulation may be independent of APC is based on the presence of full-length APC protein expression in the polyps. The common genetic (truncating mutations, LOH) and nongenetic (methylation) alterations of APC that have been identified in colonic neoplasia all would be expected to lead to loss of full-length APC protein expression. However, we did not evaluate nontruncating APC mutations that could theoretically account for the observed nuclear accumulation of β-catenin (20). This should be evaluated in future studies.
It is not clear why we observed more consistent, more diffuse, and stronger nuclear β-catenin staining than that reported by Back et al. (19), but it could be due to technical differences in the immunohistochemical protocols. Both studies used a similar antigen retrieval protocol and the same anti–β-catenin antibody, but it is possible that differences in fixation, antibody concentrations, or other reagent differences could have caused different intensity of staining. The absence of nuclear immunoreactivity in the normal mucosa in our study suggests that the nuclear staining in the JPs is evidence of genuine dysregulation of β-catenin in the polyps and not a technical artifact.
Nuclear accumulation of β-catenin may also occur in Peutz-Jeghers hamartomas. Back et al. (19) found focal nuclear staining in 12 Peutz-Jeghers polyps. APC mutations have not been found in Peutz-Jeghers polyps; thus, this is probably also a non–APC-mediated dysregulation of β-catenin. It is interesting that Herter et al. (21) did not find nuclear β-catenin in six Peutz-Jeghers polyps, again suggesting technical variability in β-catenin immunohistochemical protocols. Another report showed scattered cells with nuclear β-catenin accumulation at the base of normal murine colonic crypts that do not have APC mutations (22). Thus, there are now several examples of nuclear β-catenin accumulation in normal and neoplastic colonic mucosa that is not dependent on APC gene mutations. The non-APC mechanisms that are responsible for β-catenin accumulation in hamartomas remain to be determined.
The stromal elements of JPs have classically been thought to be the site of abnormal growth control in hamartomas. The landscaper hypothesis was proposed to explain the development of dysplasia and cancer in the epithelial component of hamartomatous polyps (23). According to the landscaper hypotheses, an abnormal stroma affects the development of the nearby epithelial cells in a manner that predisposes to dysplasia (24). Our observation of the universal presence of nuclear β-catenin in the epithelial component suggests that either the landscaper effect occurs early and diffusely in JPs or that the landscaper hypothesis is incorrect and the epithelial component is abnormal from the onset. The latter interpretation is supported by the recent detection of allelic loss of SMAD-4 in both the epithelial and stromal components of polyps from patients with familial JPC as a result of SMAD-4 germline mutations (24). This suggests a common clonal origin of both compartments in JPs rather than a landscaper effect (24). β-Catenin accumulation seems to be a universal and an early event in JPs, in a manner similar to that found in adenomatous polyps (25).
CONCLUSION
In summary, we report evidence that nuclear accumulation of β-catenin occurs in the epithelial component of JPs in children with both JPs and JPC. The mechanism for the dysregulation of β-catenin is not known but seems to be independent of inactivation of the APC gene, because abundant full-length APC protein is present in the epithelial cells of JPs and there is no evidence of LOH of APC in the polyps.
Abbreviations
- APC:
-
adenomatous polyposis coli
- JP:
-
juvenile polyps
- JPC:
-
juvenile polyposis coli
- LOH:
-
loss of heterozygosity
- TGF-β:
-
transforming growth factor-β
References
Jass JR, Williams CB, Bussey HJ, Morson BC 1988 Juvenile polyposis–a precancerous condition. Histopathology 13: 619–630
Powell SM, Zilz N, Beazer-Barclay Y, Bryan TM, Hamilton SR, Thibodeau SN, Vogelstein B, Kinzler KW 1992 APC mutations occur early during colorectal tumorigenesis. Nature 359: 235–237
Munemitsu S, Albert I, Souza B, Rubinfeld B, Polakis P 1995 Regulation of intracellular beta-catenin levels by the adenomatous polyposis coli (APC) tumor-suppressor protein. Proc Natl Acad Sci USA 92: 3046–3050
Rubinfeld B, Albert I, Porfiri E, Fiol C, Munemitsu S, Polakis P 1996 Binding of GSK3β to the APC-β-catenin complex and regulation of complex assembly. Science 272: 1023–1026
Howe JR, Roth S, Ringold JC, Summers RW, Jarvinen HJ, Sistonen P, Tomlinson IP, Houlston RS, Bevan S, Mitros FA, Stone EM, Aaltonen LA 1998 Mutations in the SMAD4/DPC4 gene in juvenile polyposis. Science 280: 1086–1088
Howe JR, Bair JL, Sayed MG, Anderson ME, Mitros FA, Petersen GM, Velculescu VE, Traverso G, Vogelstein B 2001 Germline mutations of the gene encoding bone morphogenetic protein receptor 1A in juvenile polyposis. Nat Genet 28: 184–187
Lynch ED, Ostermeyer EA, Lee MK, Arena JF, Ji H, Dann J, Swisshelm K, Suchard D, MacLeod PM, Kvinnsland S, Gjertsen BT, Heimdal K, Lubs H, Moller P, King MC 1997 Inherited mutations in PTEN that are associated with breast cancer, cowden disease, and juvenile polyposis. Am J Hum Genet 61: 1254–1260
Olschwang S, Serova-Sinilnikova OM, Lenoir GM, Thomas G 1998 PTEN germ-line mutations in juvenile polyposis coli. Nat Genet 18: 12–14
Huang SC, Chen CR, Lavine JE, Taylor SF, Newbury RO, Pham TT, Ricciardiello L, Carethers JM 2000 Genetic heterogeneity in familial juvenile polyposis. Cancer Res 60: 6882–6885
Marsh DJ, Roth S, Lunetta KL, Hemminki A, Dahia PL, Sistonen P, Zheng Z, Caron S, van Orsouw NJ, Bodmer WF, Cottrell SE, Dunlop MG, Eccles D, Hodgson SV, Jarvinen H, Kellokumpu I, Markie D, Neale K, Phillips R, Rozen P, Syngal S, Vijg J, Tomlinson IP, Aaltonen LA, Eng C 1997 Exclusion of PTEN and 10q22–24 as the susceptibility locus for juvenile polyposis syndrome. Cancer Res 57: 5017–5021
Houlston R, Bevan S, Williams A, Young J, Dunlop M, Rozen P, Eng C, Markie D, Woodford-Richens K, Rodriguez-Bigas MA, Leggett B, Neale K, Phillips R, Sheridan E, Hodgson S, Iwama T, Eccles D, Bodmer W, Tomlinson I 1998 Mutations in DPC4 (SMAD4) cause juvenile polyposis syndrome, but only account for a minority of cases. Hum Mol Genet 7: 1907–1912
Leggett BA, Thomas LR, Knight N, Healey S, Chenevix-Trench G, Searle J 1993 Exclusion of APC and MCC as the gene defect in one family with familial juvenile polyposis. Gastroenterology 105: 1313–1316
Cheryl M, Pappin A 1997 Polyps and neoplasms of the gastrointestinal tract in childhood and adolescence. Perspect Pediatr Pathol 120: 127–171
Hoffenberg EJ, Sauaia A, Maltzman T, Knoll K, Ahnen DJ 1999 Symptomatic colonic polyps in childhood: not so benign. J Pediatr Gastroenterol Nutr 28: 175–181
Iwamoto M, Ahnen DJ, Franklin WA, Maltzman TH 2000 Expression of beta-catenin and full-length APC protein in normal and neoplastic colonic tissues. Carcinogenesis 21: 1935–1940
Giardiello FM, Hamilton SR, Kern SE, Offerhaus GJ, Green PA, Celano P, Krush AJ, Booker SV 1991 Colorectal neoplasia in juvenile polyposis or juvenile polyps. Arch Dis Child 66: 971–975
Howe JR, Ringold JC, Summers RW, Mitros FA, Nishimura DY, Stone EM 1998 A gene for familial juvenile polyposis maps to chromosome 18q21.1. Am J Hum Genet 62: 1129–1136
Miyoshi Y, Ando H, Nagase H, Nishisho I, Horii A, Miki Y, Mori T, Utsunomiya J, Baba S, Petersen G, Hamilton S, Kinzler K, Vogelstein B, Nakamura Y 1992 Germ-line mutations of the APC gene in 53 familial adenomatous polyposis patients. Proc Natl Acad Sci USA 89: 4452–4456
Back W, Loff S, Jenne D, Bleyl U 1999 Immunolocalization of beta catenin in intestinal polyps of Peutz-Jeghers and juvenile polyposis syndromes. J Clin Pathol 52: 345–349
Hamada F, Bienz M 2002 A Drosophila APC tumour suppressor homologue functions in cellular adhesion. Nat Cell Biol 4: 208–213
Herter P, Kuhnen C, Muller KM, Wittinghofer A, Muller O 1999 Intracellular distribution of beta-catenin in colorectal adenomas, carcinomas and Peutz-Jeghers polyps. J Cancer Res Clin Oncol 125: 297–304
van de Wetering M, Sancho E, Verweij C, de Lau W, Oving I, Hurlstone A, van der Horn K, Batlle E, Coudreuse D, Haramis AP, Tjon-Pon-Fong M, Moerer P, van den Born M, Soete G, Pals S, Eilers M, Medema R, Clevers H 2002 The beta-catenin/TCF-4 complex imposes a crypt progenitor phenotype on colorectal cancer cells. Cell 111: 241–250
Kinzler KW, Vogelstein B 1998 Landscaping the cancer terrain. Science 280: 1036–1037
Woodford-Richens K, Williamson J, Bevan S, Young J, Leggett B, Frayling I, Thway Y, Hodgson S, Kim JC, Iwama T, Novelli M, Sheer D, Poulsom R, Wright N, Houlston R, Tomlinson I 2000 Allelic loss at SMAD4 in polyps from juvenile polyposis patients and use of fluorescence in situ hybridization to demonstrate clonal origin of the epithelium. Cancer Res 60: 2477–2482
Hao XP, Pretlow TG, Rao JS, Pretlow TP 2001 Beta-catenin expression is altered in human colonic aberrant crypt foci. Cancer Res 61: 8085–8088
Acknowledgements
Professor Ken Saito, Department of Pathology, Jichi Medical School, provided some of the tissue samples.
Author information
Authors and Affiliations
Corresponding author
Additional information
This study was supported by The Department of Veterans Affairs Merit Review Program, National Cancer Institute (CA88007 and CA90231) and the Tissue Culture/Monoclonal Antibody Core, University of Colorado Cancer Center.
Rights and permissions
About this article
Cite this article
Iwamoto, M., Hoffenberg, E., Carethers, J. et al. Nuclear Accumulation of β-Catenin Occurs Commonly in the Epithelial Cells of Juvenile Polyps. Pediatr Res 57, 4–9 (2005). https://doi.org/10.1203/01.PDR.0000148062.57051.8F
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/01.PDR.0000148062.57051.8F
This article is cited by
-
Sonic hedgehog signaling controls gut epithelium homeostasis following intestinal ischemia–reperfusion in a rat
Pediatric Surgery International (2019)
-
Accelerated intestinal epithelial cell turnover after bowel resection in a rat is correlated with inhibited hedgehog signaling cascade
Pediatric Surgery International (2016)
-
Immunohistological evidence for Wnt-signaling activation in Peutz-Jeghers polyposis
Pediatric Surgery International (2010)