Abstract
Lung deposition of inhaled drugs in ventilated neonates has been studied in models of questionable relevance. With conventional nebulizers, pulmonary deposition has been limited to 1% of the total dose. The objective of this study was to assess lung delivery of aerosols in a model of neonatal ventilation using a conventional and novel electronic micropump nebulizer. Aerosol deposition studies with 99mTc diethylenetriamine pentaacetate (99mTc-DTPA) were performed in four macaques (2.6 kg) that were ventilated through a 3.0-mm endotracheal tube (with neonatal settings (peak inspiratory pressure 12–14 mbar, positive end-expiratory pressure 2 mbar, I/E ratio 1/2, respiratory rate 40/min), comparing a jet-nebulizer MistyNeb (3-mL charge, 4.8 μm), an electronic micropump nebulizer operating continuously [Aeroneb Professional Nebulizer (APN-C); 0.5-mL charge, 4.6 μm], and another synchronized with inspiration [Aeroneb Professional Nebulizer Synchronized (APN-S); 0.5-mL charge, 2.8 μm]. The amount of radioactivity deposited into lungs and connections and remaining in the nebulizer was measured by a gamma counter. Despite similar amounts of 99mTc-DTPA in the respiratory circuit with all nebulizers, both APN-S and APN-C delivered more drug to the lungs than MistyNeb (14.0, 12.6, and 0.5% in terms of percentage of nebulizer charge, respectively; p = 0.006). Duration of delivery was shorter with APN-C than with the two other nebulizers (2 versus 6 and 10 min for the APN-S and the MistyNeb, respectively; p < 0.001). Electronic micropump nebulizers are more efficient to administer aerosols in an animal model of ventilated neonates. Availability of Aerogen's electronic micropump nebulizers offers new opportunities to study clinical efficacy and risks of aerosol therapy in ventilated neonates.
Similar content being viewed by others
Main
Treatment of lung diseases with inhaled medications is a challenge for mechanically ventilated patients, especially for the youngest ones. Therapeutic effects are thought to be limited by the combination of small endotracheal tube (ETT) diameter, low vital capacity, and mechanical ventilator settings, reducing drug delivery to the lungs (1,2). However, deposition pattern of inhaled drugs in ventilated neonates and young children remains largely unknown because the usual approach in older children and adults, based on studying radiolabeled aerosol distribution, has been contained to isolated investigations because of concern of ethical issues in this age range. When infants (10 ventilated and 13 nonintubated) who ranged from 1 to 4 kg were administered a mixture of 100 μg of albuterol and 99mTc diethylenetriamine pentaacetate (99mTc-DTPA) over 5 min with a conventional jet nebulizer, the proportion of dose delivered to the lungs was 0.22 ± 0.08% for ventilated and 0.28 ± 0.014% in the nonintubated infants (3).
Animal models have been used for mimicking such patients but with limited relevance because of differences in anatomy and the absence of underlying lung disease (4–9). Nonetheless, lung deposition has been consistently found to be low in these studies. In a model of anesthetized rabbits that were intubated with a 3.0-mm ETT, deposition of an aerosol administered via a spacer placed on the ventilator's inspiratory line or directly into the ETT ranged from 0.2 to 0.4% of the emitted dose (6,7). In conditions of uncontrolled ventilation in nonparalyzed rabbits, deposition reached a maximum of 5% of the emitted dose (7,9). The use of a jet nebulizer resulted in <1% of the charge deposited into the lungs of rabbits with a 3.5-mm ETT (4,5,8). Lung deposition was slightly improved by using an ultrasonic nebulizer with a small 10-mL cup (8) or by using nebulizers that were jet synchronized with ventilation rather than operating continuously (10).
A new generation of electronic micropump nebulizers was developed recently (11). One such nebulizer, the Aeroneb Professional Nebulizer System (Aeroneb Pro. Aerogen, Inc., Mountain View, CA), incorporates the OnQ aerosol generator, which consists of a membrane with ~1000 funnel-shaped apertures, in contact with a reservoir of fluid, vibrating at ultrasonic frequencies. This action extrudes fluid through the holes in the membrane, where surface tension and hydrodynamic effects result in breaking the extruded fluid into a stream of precisely controlled droplets. The size of the droplets is controlled primarily by the exit diameter of the apertures. This technology can produce precise particle sizes, with residual volume as low as microliters.
The aim of this study was to test the hypothesis that the Aeroneb Professional Nebulizer, an electronic micropump nebulizer developed by Aerogen, Inc., improves aerosol delivery in critical conditions such as neonatal ventilation, when compared with conventional nebulizers. The study was conducted in macaques that were chosen for their relevance in terms of anatomy and physiology to model ventilation in neonates. 99mTc-DTPA was used as tracer to assess aerosol deposition. Three different nebulizers were compared: a standard jet nebulizer (MistyNeb; Airlife) used in previous studies (12,13) and two electronic micropump nebulizers, the Aeroneb Professional Nebulizer operating continuously (APN-C) and a prototype Aeroneb Professional Nebulizer synchronized with regards to inspiration (APN-S).
METHODS
Animal model.
Four healthy macaque monkeys (two male) that weighed 2.5–2.8 kg and were a mean age of 44 mo were studied. Anesthesia was administered initially with an i.m. injection of xylazine (1 mg/kg) and ketamine (5 mg/kg). Macaques were intubated with a 3.0-mm internal diameter Portex uncuffed ETT and ventilated with a Draeger Babylog 2 ventilator (respiratory rate 40/min, peak inspiratory pressure 12–14 mbar, positive end-expiratory pressure 2 mbar, I/E ratio 1/2). The gas delivered into the circuit was neither heated nor humidified. Anesthesia was maintained with repeated injections of ketamine when necessary to suppress spontaneous respiration. Macaques were placed in the supine position on the gamma camera during all of the experiments. At the end of the experiments, macaques were awakened with Dopram (1 drop by nostril). They were extubated and then housed in their cages for a minimum of 2 d before a new experiment was initiated. The macaques were housed under conventional conditions in our laboratory and maintained in accordance with the Guide for the Care and the Use of Laboratory Animals.
99mTc-DTPA labeling.
The 99mTc-DTPA was prepared from a commercially available kit (Pentacis; CIS Bio International, France). This kit, which is under nitrogen atmosphere, contains a lyophilized, sterile, and apyogenous mixture of 9.10 mg of DTPA-CaNa3, 0.45 mg of SnCl2, and 2 H2O. Addition of sterile pyrogen-free Na-99mTcO4 from a commercial generator in 5 mL of 0.9% NaCl yielded an injectable solution of 99mTC-DTPA-CaNa3. The solution was mixed and allowed to stand for 5 min before use.
Aerosol administration.
The order of the nebulizers to be tested was randomized for each monkey. The nebulizers were tested with the fill volumes recommended by the manufacturers and based on the drug residual at the end of nebulization (determined gravimetrically). The MistyNeb (residual volume of 1.1 mL) was charged with 3-mL volume 99mTc-DTPA, whereas the APN-C and the APN-S (residual volume 0.1 mL) were charged with 0.5-mL volume. The 3-mL dose for the MistyNeb was selected as a representative median dose actually used with standard jet nebulizers during infant ventilation (most commonly albuterol sulfate, 2.5 mg in 3 mL). Each nebulizer was tested in every monkey (one nebulization with the three different nebulizers, respectively, for each monkey), resulting in 12 experiments for the four monkeys (three nebulizations × four monkeys). The same nebulizers (MistyNeb, APN-C, and APN-S) were used with the four monkeys.
The nebulizer charges (1110 MBq of 99m-DTPA in all cases) were controlled by counting the radioactivity in the syringe that contained 99mTc-DTPA in a gamma counter (Capintec, France) before and after charging the nebulizers. Then, the nebulizers were connected to the inspiratory line via a T-piece 10 cm from the Y-piece. Ventilator settings were adjusted to maintain constant delivery parameters as needed when the nebulizer was inserted and operated in the ventilator circuit. The MistyNeb was driven by oxygen at a flow of 6 L/min. The VMD produced by MistyNeb was 4.6 μm (Spraytech, Malvern, UK). Maintenance of ventilator parameters required substantial adjustments during the use of the MistyNeb. The APN-C produced aerosol continuously. The VMD produced by APN-C was 4.8 μm. The APN-S was synchronized to generate aerosol immediately before and during part of inspiration. The VMD produced by APN-S was 2.8 μm. Particle size distribution of the aerosol that reached the end of the ETT was also measured under experimental conditions and found to be 1.4 μm with each of the three nebulizers. Time for delivery was recorded for each experiment.
Gamma camera imaging.
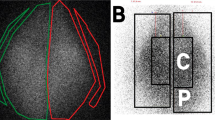
Immediately after the end of the aerosol delivery, the animals were scanned with a gamma camera (Orbiter 75; Siemens). Static acquisition was made during 60 s on a 128 × 128 matrix. The amount of radiolabeled DTPA deposited in the lungs and in the circuit components (T-piece, inspiratory limbs, Y-piece, ETT, expiratory limbs, and expiratory filter) was determined from the digitized images and using tissue attenuation coefficients derived from pertechnetate-macroaggregated albumin perfusion scanning of each macaque lung. The total body outline was determined by a rectangular region of interest, and the lungs were delineated using the perfusion scan regions of interest. The amount of radioactivity that remained in ETT and circuit components was determined using the same method with a 120-s static acquisition imaging. Corrections for decay of technetium were made on all measurements.
Statistical analysis.
A multivariate descriptive analysis was used to compare the three nebulizers according to their performances in terms of aerosol deposition into the lungs. The radioactivity deposited into the animal's lungs (one variable) and the radioactivity that remained in the nebulizer (one variable) were expressed as a percentage of the nebulizer charge. The radioactivity deposited into the different parts of the experimental settings—T-piece, inspiratory limb, Y-piece, ETT, expiratory limb and expiratory filter (six variables, corresponding to the circuit)—was expressed as the percentage of the nebulized activity (the nebulized activity was defined by the difference in the countings of the nebulizer before beginning nebulization and at the end of nebulization).
The principal components of analysis (PCA; SPAD software, Decisia 96–99, France) constructs an eight-dimensional space corresponding to the eight variables. Each observation is positioned in this space according to its score for each variable. Consequently, observations that have very similar scores in the different variables are closely related. One observation per macaque was made with each nebulizer, leading to four observations per nebulizer. Observations were named A1–A4 for the APN-S (category of observation A), B1–B4 for the APN-C (category of observation B), and C1–C4 for the MistyNeb (category of observation C). For a condensed display, the observations were also described using the center of gravity of all observations that belonged to the same category (A, B, and C).
The eight variables were placed on the graph, and their correlations with each axis were calculated. For example, on the graph, each observation has a coordinate on F1; each observation also has a score for the variable “lungs” so that the linear correlation between “lungs” and F1 can be calculated and represented as a vector on the graph. The vector is placed in a correlation circle, its direction and its length being determined by the correlation's value. This vector, representing the variable “lungs,” will be close to F1, long and directed toward the positive direction of F1 if the score of the linear correlation between “lungs” and F1 is positive and close to 1. The vector also points at observations on the graph in which the scores for the variable “lungs” are high. Each variable is positioned on the graph as a vector according to the values of its correlation with each of the two factors F1 and F2. These vectors, or “artificial variables,” are the PCA.
The three categories of observations—APN-C, APN-S, and MistyNeb—were also subjected to the DEMOD (DEscription of MODalities) procedure of SPAD that displays the statistical links between categories of observations and active variables. Differences between the three nebulizers (APN-S, APN-C, and MistyNeb) in radioactivity deposited into the lungs (expressed in percentage of the nebulizer charge) were tested by the nonparametric Kruskal-Wallis ANOVA. Differences between the Aeroneb Pro nebulizers (APN-S and APN-C) in radioactivity deposited into the lungs and in the nebulizer (expressed in percentage of the nebulizer charge), in different parts of the circuit connections (expressed in percentage of the nebulized activity), were tested by the nonparametric permutation test with general scores. Correlations between the variables “lung” and “nebulizer” were tested by the Spearman's rank-order correlation test. The different nonparametric tests were performed with the StatXact software. A p < 0.05 was considered statistically significant.
RESULTS
All animals were submitted to the whole study without any incident. Deposition in the lungs in this model of intubated and ventilated macaques was significantly different between the nebulizers (Fig. 1) with an ~25-fold greater lung deposition of 99mTc-DTPA with both Aeroneb Pro nebulizers than with MistyNeb (14.0% of the nebulizer charge with APN-S, 12.6% with APN-C, and 0.5% with MistyNeb; p = 0.006; Table 1). With APN-S, the volume deposited into the lung ranged between 61 and 119 μL (median 70 μL) in 6 min of nebulization time; with APN-C, the volume deposited in the lung ranged between 48 and 103 μL (median 63 μL) in 2 min of nebulization time; and with MistyNeb, the volume deposited in the lung ranged between 12 and 39 μL (median 15 μL) in 10 min of nebulization time. APN-C delivered four times more aerosol into the lungs than MistyNeb in one fifth of the time.
Figure 2 summarizes the results as analyzed by the PCA. The three categories of observations (A for APN-S, B for APN-C, and C for MistyNeb) were clearly separated from each other. The principal opposition on F1 was between the observations related to the MistyNeb nebulizer (circles C1–C4 on Fig. 2) that clearly clustered by their gravity center (square MistyNeb on Fig. 2) on the right and the observations related to the APN-S nebulizer (circles A1–A4 on Fig. 2) whose gravity center (square APN-S on Fig. 2) was on the left. The vector corresponding to the variable nebulizer was directed to the right toward MistyNeb observations, indicating that the C1–C4 observations were mainly characterized by high residual radioactivity in the MistyNeb nebulizer (positive correlation between F1 and the nebulizer active variable, r = 0.92). On the opposite, the vectors corresponding to the active variables ETT, lungs, and filter were negatively correlated with F1 (respectively, r = −0.83, r = −0.79, and r = −0.66) and were directed toward the APN-S observations (A1–A4). This suggests that these observations are characterized by high levels of radioactivity in the lungs, in the ETT, and in the filter.
PCA characterizing the three types of nebulizers according to the radioactivity deposited in the animals' lungs and the radioactivity remaining in the different parts of the experimental settings. The eight vectors representing active variables are underlined. The 12 observations (three experiments by monkey) are in bold circles and italic characters: A1–A4, observations of monkeys that were treated with the APN-S; B1–B4, observations of monkeys that were treated with the APN-C; C1–C4, observations of monkeys that were treated with the MistyNeb. The gravity centers for the three nebulizers are in bold squares and straight characters. The percentage of variance explained by each factor F1 and F2 is indicated in italics.
A secondary effect appeared on F2, allowing another categorization separating the APN-C observations (B1–B4), in positive coordinates of F2, from the two others. The vectors corresponding to the Y tube and the expiratory tubes were directed toward the observations B1–B4 and did correlate with F2 (r = 0.74 and 0.76, respectively), indicating greater loss of aerosol in those locations.
These categorizations were characterized statistically by DEMOD. Observations with the APN-S nebulizer were statistically characterized by the variables filter (p = 0.001), ETT (p = 0.01), and lungs (p = 0.03), whereas observations with the APN-C nebulizer were characterized by Y-piece (p = 0.005) and expiratory limb (p = 0.03). Observations with the MistyNeb nebulizer correlated only with the variable nebulizer (p = 0.002).
The most significant finding of the ACM analysis was the opposition between the “lung” vector and the “nebulizer” vector (negative correlation of −74%). To calculate the significance for this correlation, we performed a nonparametric test with the two variables, showing with this test a −0.80% correlation coefficient (p = 0.003). This indicated that the performances of the Aeroneb Pro nebulizers, as defined by aerosol lung deposition, are due mainly to the low residual volume. When APN-C and APN-S were compared in terms of statistical differences, the nonparametric tests showed that activity in the nebulizer, the T piece, and the Y piece was significantly higher with the APN-C than with the APN-S (p < 0.05 in all cases), whereas activity in the filter was significantly higher with the APN-S than with the APN-C (p < 0.05).
DISCUSSION
This study demonstrated that the two electronic micropump nebulizers (APN-S and APN-C) deposit higher amounts of aqueous aerosols into the lungs (12.6 and 14.0% of the nebulizer charge, respectively) than the conventional MistyNeb nebulizer (0.5% of the nebulizer charge) in an animal model of neonatal ventilation. This high efficiency is due mainly to the low residual volume of these devices (ACM analysis).
Aerosol delivery is influenced by numerous factors, including aerosol characteristics (particle size, shape, density, etc.), concentration of the aerosol, ventilating parameters (flow, humidity, etc.), the device, electrostatic charge, technique of using the device, patient interface, and host factors (airway geometry, pathology, breathing pattern, etc.). Change in any one of these alters the amount of aerosol delivered and deposited. The ventilator settings were adjusted, as necessary, when the jet nebulizer was operated in the ventilator circuit, and all experiments were made under similar flow and pressure conditions. Therefore, physiologic parameters could not interfere with the way the aerosol was distributed in the circuit connections or in the lungs.
Despite substantial differences between the airway of the macaque and that of humans (14), the macaque is a relevant model to predict the aerosol deposition in human lung. The morphology of our 2.6-kg mean weight macaques corresponded to normal-weight human infants at 34 or 35 wk of gestation or to low-weight, full-term infants. The main difference between our model and the usual circumstances of neonatal ventilation was that our macaques had normal airways and lungs. Furthermore, medication delivery in a normal lung may differ from a sick lung. Deposition may differ between a sedated healthy animal model and active neonates with spontaneous breathing and lung or airway disease. However, this study was designed as a preclinical assessment of the electronic micropump nebulizers to determine their efficiency in conventional ventilator settings. Further validation in critical care will need clinical studies, which this first step will now make acceptable.
DTPA was chosen because it is a stable tracer that is unaffected by oxidation and whose dynamics in the respiratory tract is similar to any other aqueous aerosol (15). Although there were some interindividual differences in aerosol deposition, possibly as a result of variable leak associated with the uncuffed ETT, APN-C and APN-S nebulizers were consistently more efficient than MistyNeb and lung deposition was in the same range for both Aeroneb Pro nebulizers. The performance of these devices pertains only to the specific conditions and techniques under which the devices were tested. The study, limited to four macaques, provided a sufficient number of observations to apply the PCA statistical approach.
The 0.5% of the nebulizer charge lung deposition and the 23% of the nebulizer charge residual volume obtained with the MistyNeb are consistent with previously reported data in other animal models of infants. In a model that simulated 4-kg infants, Coleman et al. (12) demonstrated that flow rate through the MistyNeb increases the deposition by impaction, and that residual volume was ~35% of the dose that remained in the MistyNeb. Therapeutic aerosols that are produced with these standard jet nebulizers are widely used in intubated neonates, particularly in infants who are at high risk for developing chronic lung disease. The success of this approach has been found variable, especially when compared with other delivery systems. A recent meta-analysis (16) concluded that the delivery of inhaled steroids to ventilator-dependent infants had very small effects on the occurrence of chronic lung disease, likely because of an inappropriate mode of delivery. Indeed, the use of a metered-dose inhaler and a spacer device may be more efficient than a conventional jet nebulizer for delivering both salbutamol and budesonide in neonates (17,18).
The design of the electronic micropump nebulizers is such that the fill volume required to produce the aerosol is much lower than with the MistyNeb (0.5 versus 3 mL). The higher efficiency at lower fill volumes means that APN-C deposits to the lungs in 30 s a volume of aerosol equivalent to that deposited by the MistyNeb after 10 min. The ability of both Aeroneb nebulizers to deliver in 2–6 min 25 times more aerosol in the lungs than the MistyNeb can in 10 min may have positive implications in the treatment of critically ill infants.
Although APN-S was a prototype device that was expected to be more efficient than APN-C, because aerosol generation was synchronized with regards to inspiratory phases of the ventilator, both Aeroneb Pro nebulizers delivered similar amounts of aerosols in the lungs. They differed in the residual volume and in the amount of aerosol deposited in the various parts of the circuit. The most relevant way to assess the differences was to express the deposition in the circuit as a percentage of the activity of aerosol nebulized and not as a percentage of the nebulizer charge, which is more relevant to quantify lung deposition (Table 1).
Particle size of the aerosols at the outlet of the nebulizers was similar with MistyNeb and APN-C (MMAD 4.6 and 4.8 μm, respectively) and smaller for the APN-S (MMAD 2.8 μm). At the end of the ETT, particle size distribution was similar with the three nebulizers, with a 1.4-μm MMAD (GS1 cascade impactor; California Measurement, CA). Residual volume was significantly higher with the APN-C than with the APN-S, possibly because of increased impaction losses in the barrel of the nebulizer connector with continuous aerosol generation, which means that the nebulized activity was higher with the APN-S than with the APN-C. However, there was no significant difference in terms of aerosol deposited in the lung. In vitro experiments (data not shown) have revealed an aerosol delivery at the end of the ETT two times higher with the APN-S than with the APN-C, and the countings in the filter placed on the expiratory circuit in our in vivo model of ventilation was significantly higher with the APN-S than with the APN-C. These data show that the aerosol deposited in the lung expressed in percentage of aerosol reaching the extremity of the ETT is lower with APN-S in comparison with APN-C. This discrepancy may be an effect of greater exhaled aerosol with the APN-S, which correlates with high deposition in the ETT and which cannot be simulated in vitro. This result can be explained by the synchronization between the aerosol production and the ventilator settings, which may not be optimized. The higher residual and amount of aerosol deposited in the T piece with the APN-C may be because larger aerosol droplets produced continuously at a high flow rate have an impact at the outlet of the nebulizer and in the T piece. Generally, deposition of large particles in the circuit is probably the explanation for why VMD of the aerosols generated by the three nebulizers are the same at the end of the ETT. In this study, APN-C may be considered more efficient than the APN-S as it allows deposition of similar amounts of aerosol in a significantly shorter period of time. However, insights into the differences in deposition between the two devices suggest that further adjustments to the aerosol size and generation pattern may offer greater efficiencies. Further work is required in this area.
The performance of the APN-C and APN-S, if applied to generate therapeutic aerosols, should result in much higher efficiency than what has been reported with previous generations of nebulizers. The primary concern with conventional nebulizers in neonatal ventilation has been the risk to undertreat patients. In contrast, the more efficient electronic micropump nebulizers may lead to concern related to safety profile, particularly for medications with dose-related potentials for adverse effects, such as inhaled corticosteroids in extremely premature infants. Pharmacokinetic and clinical studies will help to better determine appropriate dosing and implications of reduced treatment times and rapidity of drug action (19) with these new electronic micropump nebulizers.
Abbreviations
- APN-C:
-
Aeroneb Professional Nebulizer operating continuously
- APN-S:
-
Aeroneb Professional Nebulizer Synchronized
- ETT:
-
endotracheal tube
- PCA:
-
principal components of analysis
- 99mTC-DTPA:
-
99mTc diethylenetriamine pentaacetate
References
Ahrens RC, Ries RA, Popendorf W, Wiese JA 1986 The delivery of therapeutic aerosols through endotracheal tubes. Pediatr Pulmonol 2: 19–26
Cole CH 2000 Special problems in aerosol delivery: neonatal and pediatric considerations. Respir Care 45: 646–651
Fok TF, Monkman S, Dolovich M, Gray S, Coates G, Paes B, Rashid F, Newhouse M, Kirpalani H 1996 Efficiency of aerosol medication delivery from a metered dose inhaler versus jet nebulizer in infants with bronchopulmonary dysplasia. Pediatr Pulmonol 21: 301–309
Flavin M, MacDonald M, Dolovich M, Coates G, O'Brodovich H 1986 Aerosol delivery to the rabbit lung with an infant ventilator. Pediatr Pulmonol 2: 35–39
Cameron D, Arnot R, Clay M, Silverman M 1991 Aerosol delivery in neonatal ventilator circuits: a rabbit lung model. Pediatr Pulmonol 10: 208–213
O'Callaghan C, Hardy J, Stammers J, Stephenson TJ, Hull D 1992 Evaluation of techniques for delivery of steroids to lungs of neonates using a rabbit model. Arch Dis Child 67: 20–24
Fok TF, al-Essa M, Monkman S, Dolovich M, Girard L, Coates G, Kirpalani H 1997 Delivery of metered dose inhaler aerosols to paralyzed and nonparalyzed rabbits. Crit Care Med 25: 140–144
Fok TF, al-Essa M, Monkman S, Dolovich M, Girard L, Coates G, Kirpalani H 1997 Pulmonary deposition of salbutamol aerosol delivered by metered dose inhaler, jet nebulizer, and ultrasonic nebulizer in mechanically ventilated rabbits. Pediatr Res 42: 721–727
Dubus JC, Rhem R, Dolovich M 2001 Delivery of salbutamol pressurized metered-dose inhaler administered via small-volume spacer devices in intubated, spontaneously breathing rabbits. Pediatr Res 50: 384–389
Turpeinen M, Nikander K 2001 Nebulization of a suspension of budesonide and a solution of terbutaline into a neonatal ventilator circuit. Respir Care 46: 43–48
Smart JR 2002 A brief overview of novel liquid-based inhalation technologies. Drug Deliv Syst Sci 2: 67–71
Coleman DM, Kelly HW, McWilliams BC 1996 Determinants of aerosolized albuterol delivery to mechanically ventilated infants. Chest 109: 1607–1613
Kelly HW, Keim KA, McWilliams BC 2003 Comparison of two methods of delivering continuously nebulized albuterol. Ann Pharmacother 37: 23–26
Martonen TB, Katz IM, Musante CJ 2001 A nonhuman primate aerosol deposition model for toxicological and pharmaceutical studies. Inhal Toxicol 13: 307–324
Diot P, Galinier E, Grimbert D, Bugeon S, Valat C, Lemarié E, Diot E, Baulieu JL, Besnard JC, Guilloteau D 2001 Characterization of 99m Tc-DTPA aerosols for lung permeability studies. Respiration 68: 313–317
Lister P, Iles R, Shaw B, Ducharme F 2000 Inhaled steroids for neonatal chronic lung disease. Cochrane Database Syst Rev CD002311
Arnon S, Grigg J, Nikander K, Silverman M 1992 Delivery of micronized budesonide suspension by metered dose inhaler and jet nebulizer into a neonatal ventilator circuit. Pediatr Pulmonol 13: 172–175
Lugo RA, Kenney JK, Keenan J, Salyer JW, Ballard J, Ward RM 2001 Albuterol delivery in a neonatal ventilated lung model: nebulization versus chlorofluorocarbon and hydrofluoroalkane-pressurized metered dose inhalers. Pediatr Pulmonol 31: 247–254
Fink JB Aerosol delivery to ventilated infant and pediatric patients. Respir Care 49: 653–665 2004
Author information
Authors and Affiliations
Corresponding author
Additional information
This study was funded in part by Aerogen, Inc. (Mountain View, CA).
Rights and permissions
About this article
Cite this article
Dubus, J., Vecellio, L., De Monte, M. et al. Aerosol Deposition in Neonatal Ventilation. Pediatr Res 58, 10–14 (2005). https://doi.org/10.1203/01.PDR.0000156244.84422.55
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/01.PDR.0000156244.84422.55
This article is cited by
-
Performance and Feasibility of Therapeutic Vibrating Mesh Nebulizer for Ventilation Lung Scan
Journal of Medical and Biological Engineering (2022)
-
Nebulized fusion inhibitory peptide protects cynomolgus macaques from measles virus infection
Nature Communications (2022)
-
Aerosol drug delivery to spontaneously-breathing preterm neonates: lessons learned
Respiratory Research (2021)
-
A whole lung in silico model to estimate age dependent particle dosimetry
Scientific Reports (2021)
-
In vitro comparison between inspiration synchronized and continuous vibrating mesh nebulizer during trans-nasal aerosol delivery
Intensive Care Medicine Experimental (2020)