Abstract
Recent studies indicate a severely reduced coronary flow reserve (CFR) in neonates with congenital heart disease. The significance of these studies remains debatable, as the ability of the anatomically normal neonatal heart to increase coronary flow is currently unknown. This study was designed to establish normal values for CFR in newborns after administration of adenosine [pharmacologic CFR (pCFR)] and as induced by acute hypoxemia (reactive CFR). Thirteen mechanically ventilated newborn lambs were studied. Coronary flow velocities were measured in the proximal left anterior descending coronary artery before and after adenosine injection (140 and 280 μg/kg i.v.) using an intracoronary 0.014-in Doppler flow-wire. Measurements were made at normal oxygen saturation (Sao2) and during progressive hypoxemia induced by lowering the fraction of inspired oxygen. CFR was defined as the ratio of hyperemic to basal average peak flow velocity. In a hemodynamically stable situation with normal Sao2, pCFR was 3.0 ± 0.5. pCFR decreased with increasing hypoxemia. Regression analysis showed a linear relation between Sao2 and pCFR (R = 0.86, p < 0.0001). Reactive CFR obtained at severe hypoxemia (Sao2 <30%) was 4.2 ± 0.8, and no significant further increase in coronary flow velocity occurred by administration of adenosine. Newborn lambs have a similar capacity to increase coronary flow in response to both pharmacologic and reactive stimuli as older subjects. Administration of adenosine does not reveal the full capacity of the newborn coronary circulation to increase flow, however, as the flow increase caused by severe hypoxemia is significantly more pronounced.
Similar content being viewed by others
Main
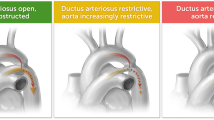
Hemodynamic problems in the neonatal period, often related to congenital heart defects, may affect coronary blood flow (1–3). The coronary physiology in newborns has become of greater importance as cardiac surgery for congenital heart defects is increasingly performed in the neonatal period. Coronary flow reserve (CFR) has been found to be useful in evaluating the effects of cardiac disease and pathologic hemodynamic conditions on coronary flow dynamics in adults (4–6). CFR is defined as the ratio of maximal coronary blood flow, as induced by reactive hyperemia or administration of vasodilators, divided by resting flow (4).
Recent studies performed with positron emission tomography (PET) have shown low CFR in neonates and infants with congenital heart disease (1, 7). The significance of these studies remains debatable, as the ability of the anatomically normal neonatal heart to increase coronary flow is currently unknown (1, 7). The objective of this study was to provide normal values for CFR in the normal neonatal heart by administration of adenosine [pharmacologic CFR (pCFR)] and by inducing acute hypoxemia [reactive CFR (rCFR)]. For this purpose, an intracoronary Doppler guide wire (IDGW) technique was used in the newborn lamb model.
METHODS
Animals.
Thirteen near-term lambs of mixed breed and sex were studied during the first day of life. Their gestational age calculated from the conception date was 132–134 d (term 145 d), and mean (range) weight was 3.7 kg (2.8–4.7 kg). The study was approved by The Animal Ethics Research Committee, Lund University.
Surgical procedures.
The pregnant ewes were premedicated with xylazine, 6–8 mg i.m., before transportation to the laboratory. After sedation with ketamine, 35 mg i.v., anesthesia was induced with thiopental, 650–800 mg i.v., and maintained with isoflurane in nitrous oxide/oxygen after intubation of the trachea. The lungs were ventilated with a Servo Ventilator 900 B (Siemens-Elema, Solna, Sweden). End-tidal Pco2 was kept at 4.5–6.0 kPa. Maintenance fluid with a balanced glucose/salt solution was given. Arterial pressure was monitored through an indwelling arterial cannula, and systolic blood pressure was maintained between 90 and 110 mm Hg by adjusting the isoflurane concentration and infusing Ringer's acetate as needed.
The lambs were delivered by cesarean section. The head was exteriorized, and a 3.5- or 4.0-mm inner diameter tracheal tube was inserted through an incision in the trachea, so the tip was located well above the carina. The tube was secured with ligatures around the trachea, which prevented any air leak. Catheters were inserted into the right jugular vein, and a 4-F introducer was placed in the right carotid artery. The lamb was then given 8 mg of ketamine and 0.4 mg of pancuronium i.v., and the umbilical cord was divided.
The lamb was weighed, towel dried, placed in an open incubator, and covered with thin plastic sheets to reduce evaporative heat loss. Esophageal temperature was kept at 38–39°C with radiant heat lamps as needed. The tracheal tube was connected to a Servo Ventilator (model 900C; Siemens-Elema) in the pressure control mode. The initial ventilator settings were; inspiratory pressure 29 cm H2O (25 cm H2O + positive end expiratory pressure of 4 cm H2O), ventilatory rate 50/min; inspiratory time 50% of the cycle and the fraction of inspired oxygen (Fio2) 0.5. The ventilator settings were subsequently adjusted to maintain initial Pao2 at 6–8 kPa, and arterial pressure of carbon dioxide (Paco2) at 5–6 kPa.
An additional arterial catheter was placed in the umbilical artery. Adequate catheter positions were confirmed using fluoroscopy. The arterial catheters in the carotid and umbilical arteries were used to draw blood samples used for measurement of arterial blood gases and Hb and for continuous arterial blood pressure monitoring. When mean arterial blood pressure was <40 mm Hg, blood was taken from the ewe and 10 mL/kg was given to the lamb, unless the lamb's Hb simultaneously exceeded 150 g/L, in which case Ringer's acetate was used instead for volume expansion. Blood was likewise given (10 mL/kg) when Hb was <130 g/L. A total of 1 mmol/kg of sodium bicarbonate was given when the pH was <7.25 and base deficit was >5 mmol/L. Ketamine, 1 mg/mL in 5% glucose, was infused at a rate of 4 mL · kg−1 · h−1, and pancuronium was administered i.v. as needed to maintain paralysis. Sedation and analgesia after delivery were obtained with an initial i.v. bolus dose of 20 μg/kg of Fentanyl, followed by a continuous infusion of 10 μg · kg−1 · h−1.
The lamb was allowed to stabilize for at least 2 h after delivery. A left lateral thoracotomy was then performed in the fourth intercostal space. The lung was retracted, the pericardium was opened, and the arterial duct and ascending aorta were identified. The arterial duct was ligated. A precalibrated ultrasonic blood flow transducer of proper size (Transonic R or S series) was applied around the ascending aorta to measure cardiac output and was connected to Transonic T101 flow meter. ECG electrodes were sutured on the chest wall subcutaneously for continuous ECG monitoring, and a pulse-oximeter was placed on the tail for continuous monitoring of oxygen saturation (Sao2). Hemodynamic stabilization of 30–60 min was allowed before intracoronary measurements of coronary flow velocities were performed.
Experimental procedure.
A 4-F right coronary angiography catheter (Judkins) was advanced through the introducer in the right carotid artery to the aortic root. After identification of the left coronary artery by contrast injection (Omnipaque 240), selective left coronary angiography was performed. The IDGW was then advanced into the proximal left anterior descending coronary artery (LAD) through the coronary catheter, the position of the tip of the IDGW in the proximal LAD was confirmed by fluoroscopy, and the coronary catheter was then withdrawn to the ostium of the left coronary artery. The position of the IDGW was kept as constant as possible by securing it tightly within the coronary catheter and repeatedly conforming its position by fluoroscopy.
Measurements were made at Sao2 >90%, and the level of oxygenation was confirmed with blood gas analysis and pulse-oxymetry. In seven of the lambs, the Fio2 was then gradually lowered to reduce the Sao2, while all other ventilatory parameters were kept constant. The aim was to lower Sao2 stepwise and register hemodynamic and coronary flow variables at as many different levels of Sao2 as possible. When reduction of Fio2 to room air levels was inadequate to produce desired reduction in Sao2, nitrogen was added to inspired air and Fio2 was lowered further as needed (lowest Fio2 used, 0.09). Before each hemodynamic and coronary flow velocity measurement, the Sao2 was kept stabile for 2–3 min before measurements were performed. Sao2 was measured by pulse-oximeter and confirmed by simultaneous blood gas analysis at every second to third measurement. There was excellent correlation between the Sao2 registered with pulse-oximeter and Sao2 measured with blood gas analysis when simultaneous analysis was performed. The hemodynamic variables measured at each stage were heart rate, blood pressure, cardiac output, and LAD flow velocities before and after a bolus injection of adenosine. The lambs were killed with thiopental overdose when the experimental protocol had been completed.
Measurements of coronary flow velocities and coronary flow reserve.
Coronary flow velocities were measured with a 0.014-in-diameter (0.36 mm) IDGW (Flowire, Cardiometrics, Inc, Mountain View, CA, U.S.A.). It is equipped with a 15-MHz piezoelectric ultrasound transducer at its tip that permits velocity acquisition with a high pulse repetition frequency (up to 90 kHz) from a sampling depth of 5 mm. This forward-directed ultrasound beam with a 25° divergent angle samples a large proportion of the coronary flow profile. Blood flow velocities are determined from the Doppler frequency shift based on the difference between the transmitted and returning signals, calculated from the Doppler equation. The velocity data are processed by on-line fast Fourier transformation.
After IDGW was placed in the proximal LAD, baseline flow velocity data were obtained at this position once a stable Doppler signal was achieved (Fig. 1). This was accomplished by means of torque adjustment with attention to the amplitude display until a high-quality signal had been attained.
Continuous flow velocity profiles and audio signals along with simultaneous ECG were displayed and recorded on videocassette. Doppler flow velocity spectra were analyzed on-line to determine average peak velocity (APV), where APV is the time average value of the instantaneous peak velocity samples over the last two cardiac cycles. Diastolic peak flow velocity (PFVd) and systolic peak flow velocity (PFVs) were measured off-line and averaged over three cardiac cycles.
Once baseline flow velocity data had been obtained, a bolus of i.v. adenosine 140 μg/kg was injected into the catheter in the right jugular vein. Flow velocity spectra were registered for 60 s after each bolus (Fig. 2). pCFR was defined as the ratio of the highest registered APV after administration of adenosine to baseline APV. For ensuring that true maximal coronary flow velocity was obtained by adenosine, a double dose of adenosine (280 μg/kg) was given at the initial measurements in each lamb. This did not result in any significant increase in LAD flow velocity compared with the 140-μg/kg dose. rCFR was defined as the ratio of the highest registered APV at severe hypoxemia (mean Sao2, 11.4%) to baseline APV at normal oxygen saturation (mean Sao2, 94.7%.)
CFR measurement in the LAD at normal Sao2. The bottom of figure shows the coronary flow profile before (left) and after (right) administration of adenosine. The APV before administration of adenosine was 9.1 cm/s, and the maximal APV after administration of adenosine was 30.0 cm/s, which gives a CFR of 3.3.
Measurements and calculations.
Arterial pressures were measured with pressure transducers referenced to atmospheric pressure with zero obtained at the midchest position. The signal was averaged electronically to obtain mean pressures. Heart rate was obtained from continues ECG monitoring. Blood gas tensions, pH, Sao2, and Hb were measured with a Radiometer OSM 3 blood gas analyzer (Radiometer, Copenhagen, Denmark). Sao2 was additionally continuously monitored by OXImeter pulse-oximeter (Radiometer).
Statistical analysis.
Results are presented as mean (SD). Hemodynamic values, arterial blood gases, and coronary flow parameters were analyzed using ANOVA for repeated measures. When significant differences were found, they were further tested for significance by post hoc tests. Linear and logarithmic regression analysis was used to calculate correlation coefficients (r). P < 0.05 was considered significant.
RESULTS
Blood gases and general hemodynamics.
Sao2, blood gases, heart rate, blood pressure, cardiac output, and stroke volume at different stages of the experimental protocol are presented in Table 1. The administration of adenosine did not result in any significant changes in heart rate or blood pressure. During the hypoxemia part of the experiment, no significant changes were observed in pH, base excess, Pco2, cardiac output, or stroke volume. Heart rate and blood pressure did not change significantly with moderate hypoxemia (Sao2, 60–90%). With more pronounced hypoxemia (Sao2, 30–60%) heart rate increased significantly and blood pressure was reduced. At extreme hypoxemia (Sao2 <30%), blood pressure increased again (Table 1).
Coronary flow dynamics.
Hemodynamic and coronary flow data in the newborn lambs at normal oxygen saturation are shown in Tables 1 and 2. With progressive hypoxemia, the APV increased significantly as illustrated in Figure 3, and regression analysis showed an inverse linear correlation between log(Sao2) and APV (R = −0.90, R2 = −0.81, F = 274.0, p < 0.0001). PFVd also increased with progressive hypoxemia as illustrated in Figure 4, and an analogue inverse linear correlation was found between log(Sao2) and PFVd (R = −0.79, R2 = −0.62, F = 99.7, p < 0.0001). PFVs increased with progressive hypoxemia but not as consistently as PFVd. Regression analysis showed a significant negative linear correlation between Sao2 and PFVs (R = −0.66, R2 = −0.44, F = 44.5, p < 0.0001). The changes in coronary flow velocities at different levels of Sao2 are shown in Table 2.
CFR and maximal coronary flow.
The pCFR at normal Sao2 was 3.0 (0.5). With progressive hypoxemia, the pCFR was reduced, and at severe hypoxemia (Sao2 <30%), it was almost exhausted, with pCFR 1.1 (0.1). Regression analysis showed a linear relation between Sao2 and pCFR (R = 0.86, R2 = 0.74, F = 135.6, p < 0.0001;Fig. 5).
Severe hypoxemia (Sao2 <30%) resulted in significantly higher (p < 0.0001) coronary flow velocities than what was obtained by adenosine administration at normoxia (Fig. 6). The rCFR was 4.2 (0.8). At Sao2 between 30 and 100%, the maximal coronary flow velocities obtained after adenosine administration were fairly constant. Administration of adenosine at severe hypoxemia (Sao2 <30%) resulted in insignificant further increase in coronary flow velocities, as shown in Figure 6, and as indicated by a CFR of 1.1 at Sao2 <30%.
Data compare APV (mean and SE) in the LAD at rest (basal) and maximal APV after administration of adenosine at severe hypoxemia (Sao2 <30%) and after adenosine administration at severe hypoxemia. There is a significant difference (p < 0.0001) between all values shown except hypoxemia (APV 27.1 cm/s) and hypoxemia + adenosine (APV 30.0 cm/s).
DISCUSSION
The main result of this study is the determination of pCFR in a normal neonatal heart in a stable hemodynamic condition. The results provide a reference interval for pCFR in the newborn lamb model with possible applicability to humans.
Measurements of CFR unavoidably involve exposure to radiation or administration of drugs with potential serious side effects or both and therefore cannot be performed in healthy human neonates. As CFR studies in healthy neonates are entirely lacking and CFR measurements in healthy human neonates with the currently available methods may prove unfeasible because of ethical restraints, we used an experimental lamb model to determine CFR in the normal newborn heart.
In this study, pCFR in the newborn lambs was similar or slightly lower than has been documented in children and adults (5, 8–11). A normal adult heart can increase coronary flow/myocardial perfusion by maximally 2.5 to 4 times the resting value, but normal pCFR values for adults are somewhat different for each method and vasodilator used (5, 6, 9, 12, 13). CFR can be measured with PET techniques, cine magnetic resonance imaging, and Doppler ultrasound (1, 7, 9, 12, 13). In the newborn lamb, experimental studies using the radioactive microspheres method have shown a high myocardial perfusion compared with older animals (14–16). High basal myocardial perfusion may be associated with reduced CFR; this has led to speculations that CFR in the newborn is generally lower than in older subjects (1, 16).
CFR can be reduced if basal flow is increased as a result of myocardial hypertrophy or if maximal flow is reduced by functional disturbance of the microcirculation (6, 17). Severe myocardial hypertrophy, high ventricular pressures, and decreased oxygen saturation commonly associated with congenital heart defects can affect both basal and maximal coronary flow and therefore might reduce CFR (1, 7, 14, 18, 19).
The PET technique has been used to measure CFR in human neonates who are surgically treated for congenital heart disease, and transthoracic Doppler has been used to describe coronary flow dynamics at rest in neonates (1–3, 7). With further refinement of the noninvasive Doppler technique, it is likely that it can be used to measure CFR in neonates with congenital heart defects (2, 3, 20). Available studies applying the PET technique to measure pCFR in neonates who undergo surgery for congenital heart defects have reported a CFR in the range 1.2–1.6 (1, 7). No healthy control subjects were included, but the CFR was low compared with what has been measured by IDGW and PET on older healthy children and young adults (5, 10, 11, 21). One of the questions left unanswered by these studies was whether the pCFR obtained in the neonates with surgically corrected congenital heart defects is pathologic, caused by the heart defect or recent surgery, or is a normal value for the neonatal heart. The results of our study point in the direction that neonates with surgically corrected congenital heart defects may have pathologically low CFR and could be at increased risk of myocardial ischemia during any situation that increases myocardial oxygen demand (1, 7).
The increase in LAD flow velocities in response to progressive hypoxemia in our study is in concordance with earlier studies performed in the newborn lamb using the radioactive microspheres method to measure myocardial perfusion (14, 22). These studies have shown an increase in myocardial perfusion with progressive hypoxemia and a maximal increase up to 3.77 times the resting flow value when hypoxemia was severe (14, 22). As coronary flow increases with hypoxemia and pCFR is dependent on resting flow and maximal coronary flow after administration of a vasodilator, we expected to find pCFR linearly reduced during hypoxemia as shown in Figure 5.
In the current study, the increase in coronary flow velocity with progressive hypoxemia followed an exponential pattern, and at severe hypoxemia, coronary flow velocities significantly exceeded what was obtained by administration of adenosine alone. The rCFR therefore was higher (4.2) than the pCFR (3.0) and slightly higher than the previous experimental lamb studies have indicated (14, 22). Our results are similar to those of Reller et al.(23), which showed that severe acute hypoxemia in the fetal lamb causes coronary flow to exceed what can be obtained by administration of adenosine alone. In Reller's study, nitric oxide was shown to be a modulator of the increased flow at severe hypoxemia, as the difference in flow velocity obtained by severe hypoxemia and by administration of adenosine was abolished by administration of nitric oxide synthase inhibitor N-nitro-l-arginine (23). The mechanism for hypoxemia-induced increase in coronary flow is controversial and has not been studied in newborns. It may be explained by increased coronary shear-stress that causes a release of endothelium-derived nitric oxide and vasodilatory prostaglandins that can increase coronary flow additionally by a mechanism different from adenosine (23–25).
Methods and limitations.
Measurements of coronary flow velocities and CFR with the IDGW have been validated extensively both in vitro and in vivo(26, 27). The IDGW measures flow velocity, not volume flow, but a close linear correlation has been shown between coronary flow velocity measured by the IDGW and volume flow measured by electromagnetic circumflex flow probes (26). The IDGW has been shown to cause negligible flow disturbance in coronary arteries as small as 1.2 mm in diameter, and even if our study was performed in small animals, the 0.014-in diameter wire is unlikely to have affected the coronary flow (26).
Coronary flow becomes dependent on coronary perfusion pressure when the coronary bed is maximally dilated (4). Coronary perfusion pressure was not measured during this experiment but is closely related to mean arterial blood pressure. Mean blood pressure was not increased at severe hypoxemia compared with normoxemia (Table 1). The higher maximal coronary flow at severe hypoxemia therefore is unlikely to be explained by higher coronary perfusion pressure.
Both continuous i.v. infusion and intracoronary bolus injections of adenosine have been shown to produce similar CFR values (28, 29). The i.v. bolus dose of adenosine used in this study produces a sustained coronary hyperemia that is at least equal to that produced by continuous infusion, and it was chosen as it was assumed to cause less general hemodynamic effects than a continuous infusion (28). We feel confident that true maximal coronary flow velocity was measured in our study, as a double dose of adenosine did not result in higher CFR values.
This study was performed in anesthetized lambs, and thoracotomy was performed. The surgery was necessary to close the arterial duct, as left to right shunt may have large effects on coronary flow (3, 30). Mechanical ventilation and anesthesia might have effects on basal coronary flow and CFR, but data obtained in anesthetized mechanically ventilated children have shown CFR values comparable to values obtained in adults who were not subject to anesthesia (5, 10). Even if a small increase in myocardial blood flow induced by ketamine has been described in dogs, available studies in newborn lambs have shown that the drug has no significant effects on heart rate, mean arterial pressure, and systemic vascular resistance and is thereby unlikely to have affected myocardial blood flow in this study (31).
CONCLUSION
Newborn lambs have a similar capacity to increase coronary flow in response to both pharmacologic and reactive stimuli as older subjects. Administration of adenosine, however, does not reveal the full capacity of the newborn coronary circulation to increase its flow, as the flow increase caused by severe hypoxemia is significantly more pronounced.
Abbreviations
- APV:
-
average peak flow velocity
- CFR:
-
coronary flow reserve
- Fio2:
-
fraction of inspired oxygen
- IDGW:
-
intracoronary Doppler guide wire
- LAD:
-
left anterior descending coronary artery
- Paco2:
-
arterial pressure of carbon dioxide
- pCFR:
-
pharmacologic coronary flow reserve
- PET:
-
positron emission tomography
- PFVd:
-
diastolic peak flow velocity
- PFVs:
-
systolic peak flow velocity
- rCFR:
-
reactive coronary flow reserve
- Sao2:
-
oxygen saturation
References
Donnelly JP, Raffel DM, Shulkin BL, Corbett JR, Bove EL, Mosca RS, Kulik TJ 1998 Resting coronary flow and coronary flow reserve in human infants after repair or palliation of congenital heart defects as measured by positron emission tomography. J Thorac Cardiovasc Surg 115: 103–110
Oskarsson G, Pesonen E 2000 Coronary flow abnormalities in neonates with aortic stenosis. J Pediatr 137: 875–877
Harada K, Tamura M, Orino T, Yasuoka K 2001 Coronary blood flow assessed by transthoracic echocardiography in neonates. Pediatr Cardiol 22: 189–193
Hoffman JI 1984 Maximal coronary flow and the concept of coronary vascular reserve. Circulation 70: 153–159
Skalidis EI, Kockiadakis GE, Koukouraki SI, Parthenakis FI, Karkavistas NS, Vardas PE 1999 Phasic coronary flow pattern and flow reserve in patients with left bundle branch block and normal coronary arteries. J Am Coll Cardiol 33: 1338–1346
Hildick-Smith DJR, Shapiro LM 2000 Coronary flow reserve improves after aortic valve replacement for aortic stenosis: an adenosine transthoracic echocardiography study. J Am Coll Cardiol 36: 1889–1896
Yates RW, Marsden PK, Badawi RD, Cronon BF, Anderson DR, Tynan MJ, Maisey MN, Baker EJ 2000 Evaluation of myocardial perfusion using positron emission tomography in infants following a neonatal arterial switch operation. Pediatr Cardiol 21: 111–118
Egashira K, Inou T, Hirooka Y, Yamada A, Urabe Y, Takeshita A 1993 Evidence of impaired endothelium dependent coronary vasodilation in patients with angina pectoris and normal coronary angiograms. N Engl J Med 328: 1659–1664
Hamaoka K, Onouchi Z, Ohmochi Y, Sakata K 1995 Coronary arterial flow-velocity dynamics in children with angiographically normal coronary arteries. Circulation 92: 2457–2462
Giulia Gagliardi M, Crea F, Polletta B, Bassano C, La Vigna G, Ballerini L, Ragonese P 2001 Coronary microvascular endothelial dysfunction in transplanted children. Eur Heart J 22: 254–260
Itoi T, Oka T, Hamaoka K 2001 Abnormal coronary flow reserve in a 13-year-old girl with an absent left circumflex coronary artery. Pediatr Cardiol 22: 165–166
Sakuma H, Koskenvuo JW, Niemi P, Kawada N, Toikka JO, Knuuti J, Laine H, Saraste M, Kormano M, Hartiala JJ 2000 Assessment of coronary flow reserve using fast velocity-encoded cine MR imaging: validation study using positron emission tomography. AJR Am J Roentgenol 175: 1029–1033
Saraste M, Koskenvuo J, Knuuti J, Toikka J, Laine H, Niemi P, Sakuma H, Hartiala J 2001 Coronary flow reserve: measurement with transthoracic Doppler echocardiography is reproducible and comparable with positron emission tomography. Clin Physiol 21: 114–122
Fischer DJ 1984 Increased regional myocardial blood flows and oxygen deliveries during hypoxemia in lambs. Pediatr Res 18: 602–606
Fisher DJ, Heymann MA, Rudolph AM 1981 Myocardial consumption of oxygen and carbohydrates in newborn sheep. Pediatr Res 15: 843–846
Mainwaring RD, Mentzer RM, Ely SW, Rubio R, Berne RM 1985 The role of adenosine in the regulation of coronary blood flow in newborn lambs. Surgery 98: 540–545
Rajappan K, Rimoldi OE, Dutka DP, Ariff B, Pennell DJ, Sheridan DJ, Camici PG 2002 Mechanisms of coronary microcirculatory dysfunction in patients with aortic stenosis and angiographically normal coronary arteries. Circulation 105: 470–476
Lowensohn HS, Khouri EM, Gregg DE, Pyle RL, Patterson RE 1976 Phasic right coronary artery blood flow in conscious dogs with normal and elevated right ventricular pressures. Circ Res 39: 760–776
Watanabe N, Awa S, Akagi M, Ando Y, Oki N, Waragai T, Hosaki A, Kawamata H, Kamisaka K 2000 Effects of heart rate and right ventricular pressure on right coronary arterial flow and its systolic versus diastolic distribution in a variety of congenital heart disease in children. Pediatr Int 42: 476–482
Noto N, Karasawa K, Kanamaru H, Ayusawa M, Sumitomo N, Okada T, Harada K 2002 Non-invasive measurements of coronary flow reserve in children with Kawasaki disease. Heart 87: 559–565
Bengel FM, Hauser M, Duvernoy CS, Kuehn A, Ziegler SI, Stollfuss JC, Beckmann M, Sauer U, Muzik O, Schwaiger M, Hess J 1998 Myocardial blood flow and coronary flow reserve late after anatomical correction of transposition of the great arteries. J Am Coll Cardiol 32: 1955–1961
Bernstein D, Teitel DF 1990 Myocardial and systemic oxygenation during severe hypoxemia in ventilated lambs. Am J Physiol 258: H1856–H1864
Reller MD, Burson MA, Lohr JL, Morton MJ, Thornburg KL 1995 Nitric oxide is an important determinant of coronary flow at rest and during hypoxemic stress in fetal lambs. Am J Physiol 269: H2074–H2081
Park KH, Rubin LE, Gross SS, Levi R 1992 Nitric oxide is a mediator of hypoxic coronary vasodilatation. Relation to adenosine and cyclooxygenase-derived metabolites. Circ Res 71: 992–1001
Koller A, Sun D, Kaley G 1993 Role of shear stress and endothelial prostaglandins in flow- and viscosity-induced dilation of arterioles in vitro. Circ Res 72: 1276–1284
Doucette JW, Corl PD, Payne HM, Flynn AE, Goto M, Nassi M, Segal J 1992 Validation of a Doppler guide wire for intravascular measurement of coronary artery flow velocity. Circulation 85: 1899–1911
Vanyi J, Bowers T, Jarvis G, White CW 1993 Can an intracoronary Doppler wire accurately measure changes in coronary blood flow velocity?. Cathet Cardiovasc Diagn 29: 240–246
Kern MJ, Deligonul U, Tatineni S, Serota H, Aguirre F, Hilton TC 1991 Intravenous adenosine: continuous infusion and low dose bolus administration for determination of coronary vasodilator reserve in patients with and without coronary artery disease. J Am Coll Cardiol 18: 718–729
Jeremias A, Filardo SD, Whitbourn RJ, Kernoff RS, Yeung AC, Fitzgerald PJ, Yock PG 2000 Effects of intravenous and intracoronary adenosine 5′-triphosphate as compared with adenosine on coronary flow and pressure dynamics. Circulation 101: 318–323
Toorop GP, Hardjowijono R, Dalinghaus M, Gerding AM, Koers JH, Zijlstra WG, Kuipers JR 1987 Myocardial blood flow and VO2 in conscious lambs with an aortopulmonary shunt. Am J Physiol 252: H681–H686
Burrows FA, Norton JB, Fewel J 1986 Cardiovascular and respiratory effects of ketamine in the neonatal lamb. Can Anaesth Soc J 33: 10–15
Acknowledgements
We thank Edgar Hernandez-Andrade, MD, and research nurses Ingela Mattisson-Sandström, Ulla Ganestam, Laura Darcy, and Annica Maxedius for excellent assistance during the experiments.
Author information
Authors and Affiliations
Corresponding author
Additional information
Supported by grants from the Swedish Heart Lung Foundation, Stockholm; The Crafoord Foundation, Lund; the Swedish Medical Research Council, Stockholm; The Swedish Heart-Children's Association, Stockholm; the University Hospital of Lund; and the Medical Faculty of Lund University.
Rights and permissions
About this article
Cite this article
Óskarsson, G., Pesonen, E., Gudmundsson, S. et al. Coronary Flow Reserve in the Newborn Lamb: An Intracoronary Doppler Guide Wire Study. Pediatr Res 55, 205–210 (2004). https://doi.org/10.1203/01.PDR.0000103932.09752.D6
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/01.PDR.0000103932.09752.D6
This article is cited by
-
Coronary flow and reactivity, but not arrhythmia vulnerability, are affected by cardioplegia during cardiopulmonary bypass in piglets
Journal of Cardiothoracic Surgery (2013)