Abstract
The field of adolescent medicine is unique as a subspecialty in that the practice of providing care to teenagers has always been viewed historically as a responsibility of generalists. Scientific advances in subspecialty fields such as endocrinology, gynecology, gastroenterology, infectious disease, and sports medicine were incorporated with considerable success into the general practices of not only pediatricians but also internists and family practitioners. However, societal changes in the past century began to shape the way health professionals thought about adolescents and their families and significantly influenced the practice of providing health care to adolescents. The most notable change, however, was the shift from the traditional role of providing anticipatory guidance to parents toward a reduction of risk-taking behaviors aimed directly at the adolescent. The subspecialty of adolescent medicine thus emerged as an amalgam of researchers, clinicians, and educators, who, through a variety of settings, hoped to advance science, moderate public and social policy, improve health care, and stimulate health promotion to this special population of patients.
Similar content being viewed by others
MAJOR SCIENTIFIC ADVANCES IN ADOLESCENT MEDICINE
Landmark scientific advances of the past century contributed greatly to the growth of the field of adolescent medicine. Some of these advances resulted from primary efforts to directly improve the health of adolescents, whereas others were derived from advances in other fields of medicine that secondarily benefited adolescents. Although at times it is difficult to distinguish between these two contributors toward change, the compilation of these scientific advances were instrumental in promoting the field of adolescent medicine. The physical and hormonal changes that define puberty have been elucidated, as have major psychological, cognitive, and behavioral developments characterizing the transition from childhood to adulthood. Great strides have been made in the management of mental illnesses and chronic medical illness, in technological advancements in the field of gynecology, and in the development of birth control methods. All have had a dramatic impact on furthering the discipline of adolescent medicine.
For the most part, the parent disciplines of pediatrics, psychiatry, internal medicine, and gynecology have had very little focus on the adolescent patient. The field of pediatrics has primarily focused on the health of the newborn, infant, and child; psychiatry has focused on adult depression, psychosis, and pharmacology; internal medicine has redirected its efforts toward geriatric medicine; and finally, gynecology has focused its efforts on reproductive cancer. There was an absolute need to serve a high prevalence of morbidity and mortality in a large and growing adolescent population. This need provided the opportunity for the adolescent medicine specialist to incorporate the contributions from the parent fields into a growing field that specifically addressed the needs of the adolescent patient.
Advances in the understanding of pubertal growth and development.
Research defining the processes of adolescent growth and physiologic development began in the 1930s with the descriptions by Greulich and Pyle (1) and Stuart (2) of the stages of pubertal growth and development. In the 1960s, Marshall and Tanner (3, 4) further defined standards for the stages of breast and pubic hair development in girls and genital and pubic hair development in boys. They also chronicled the timing of the onset of the growth spurt and the peak growth velocity in both boys and girls. In the 1950s, radiographic determination of skeletal age was discovered to be an excellent indicator of physiologic age and a valuable diagnostic tool for detecting pubertal abnormalities (5). During the 1960s, the major differences between the body composition of boys and girls were studied (6). In the 1970s, Frisch and McArthur (7) discovered a relationship between the percentage of body fat in adolescent girls and the onset of menarche. Recent data suggesting an earlier age of menarche in girls and acceleration in the height and weight of both girls and boys during the past century may have significant implications for establishing new standards for defining precocious or delayed puberty (8, 9).
Discoveries delineating the major hormonal events that trigger the visible physical changes of puberty contributed greatly to the understanding of adolescent growth and development. In the early 1970s, Boyar et al. (10) and Zumoff et al. (11) examined patterns of estradiol secretion in girls and patterns of testosterone secretion in boys. This group also discovered that an increase in both gonadotropins and GH during early adolescence provided a highly distinct biologic index for the identification of puberty (12, 13). Reiter and Grumbach (14) did further work on the neuroendocrine control of the onset of puberty. Other seminal observations in the 1970s included the discovery that elevated serum alkaline phosphatase levels, presumably of osseous origin, correlate with peak growth velocity at the height of the adolescent growth spurt (15, 16), and increases in hematocrit, presumably secondary to an androgen surge, are related to puberty in boys (17). All of these observations helped to clearly demarcate childhood from adolescence and thus delineate the field of adolescent medicine.
Advances in the psychological, cognitive, and behavioral development of adolescents.
The study of adolescent psychological, cognitive, and behavioral development dates back to the beginning of the 20th century. In 1904 Hall, often referred to as the “father of the psychology of adolescence,” reasoned that normal adolescence is a time of Sturm und Drang or “storm and stress” (18). Although this treatise had little scientific basis, the concept that adolescence is a time of great stress and turmoil was well accepted for decades. Psychoanalysts of the 1930s, among them Anna Freud, reinforced the concept that normal adolescence was characterized by a time of intrapsychic turmoil linked to the hormonal and bodily changes of puberty and related to the resolution of earlier childhood sexuality conflicts.
Through the 1930s and 1940s sociologist Lawrence K. Frank and his multidisciplinary team at the Adolescent Study Unit at Yale, studied body image and personality development in adolescents. He proposed that “adolescent rebellion” was normal adolescent behavior and that confusion and misunderstanding of normal adolescent development could lead to the poor medical care of teenagers (74).
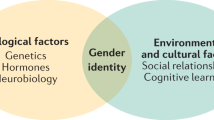
In the 1950s, Piaget and Inhelder (19) theorized that the most profound advancement in the cognitive development of adolescents, termed “formal operations,” was characterized by the development of the ability to reason and construct ideals. Erickson (20) theorized that the formation of a personal identity was based on the ability of the adolescent to perform formal cognitive operations. He also modified the classic psychoanalytic approach to adolescence by shifting the emphasis toward the psychosocial tasks of adolescence and away from the sole focus of biology. Erickson's eight stages of development form the basis of the current thinking that adolescence is a developmental stage that requires achievement of specific psychosocial tasks and challenges before the attainment of adulthood (20). Research in the 1960s confirmed that the alleged turmoil in adolescence was not, in fact, normative biologic behavior but a harbinger of psychopathology.
Elkind (21) contributed significantly to our understanding of the behavioral development of adolescents. In the 1960s and 1970s, he coined the terms, “imaginary audience”—adolescents believe that everyone is watching them—and “the personal fable”—adolescents believe that they are special, unique, and invulnerable to harm. Elkind (21) postulated that these powerful constructs make adolescents especially vulnerable to the influences and risks of the many social pressures of peer conformity, drug use and sexual activity. More recent work in the 1980s and 1990s by Garmezy (22) and Rutter (23) once more shifted the focus but now from a developmental behavioral model that emphasizes factors that predispose adolescents to risk behaviors to one that emphasizes the importance of adaptation, competence, efficacy, and resiliency as protective factors.
Whereas the biologic markers noted earlier tended to offer separation between childhood and early adolescence, much of the psychological and behavioral data helped to demarcate middle and late adolescence from adulthood. Thus, the field achieved definition and, with it, separation and ultimately subspecialty status.
Advances in adolescent mental health and psychopharmacology.
One of the greatest contributions to adolescent mental health during the past century was the recognition that not only depression but other mental health problems, including schizophrenia, anxiety disorder, and obsessive-compulsive disorder, often presented in adolescents. Moreover, the genetic and biochemical etiologies of these illnesses were explored and appreciated. Despite our improved understanding of these illnesses, however, little progress has been made in our understanding of teenage suicide as it continues to be the third most common cause of mortality in the adolescent age group. Suicide rates having remained constant for the past 30 y (24, 25).
The field of adolescent psychopharmacology remains in its infancy. Until recently, data from adult studies on antidepressants, antipsychotic medications, anxiolytics, and mood stabilizers were extrapolated and adopted to treat these disorders in children and adolescents. Most studies examining the safety and efficacy of these medications in adolescents were carried out with small sample sizes, without placebo controls, or in larger mixed samples without adequate controls. The exceptions to this trend are the studies of psychostimulant medications and tricyclic antidepressants. The effectiveness of methylphenidate, amphetamines, and pemoline in the treatment of adolescent attention deficit and hyperactivity disorder was studied extensively from the late 1930s to the mid-1970s (26, 27). Research in the 1970s demonstrated the efficacy of tricyclic antidepressants in the treatment of the pediatric- and adolescent-specific conditions such as enuresis, obsessivecompulsive disorder, and attention deficit and hyperactivity disorder (28).
Although the studies relating to psychostimulant medications and tricyclic antidepressants represent only a small proportion of the studies that have been done to advance the field of adolescent pharmacology, their impact has been significant. As one of the areas of pharmacology that were studied in children and adolescents before being studied in adults, this research introduced and highlighted the principle that illnesses of childhood and adolescence are different from those of adults and thus need to be managed differently.
Advances in chronic disease management.
During the past 100 y, there has been little change in the incidence of the major chronic disorders of childhood (29). The numbers of children with previously fatal chronic illnesses surviving into adolescence, however, have increased dramatically. This is largely attributable to significant advances that occurred in solid organ transplantation, cancer chemotherapy, surgical techniques, and immunosuppressive and pharmacologic therapies. Specific landmark advances include the vastly improved survival rates of pediatric organ transplant recipients as well as the increased survival rates of children with cancer and cystic fibrosis. These survival rates were abysmal in the early part of the 20th century, yet today the 5-y survival rates of living related and cadaveric transplant recipients are reaching 75% to greater than 90%, and more than 60% of children diagnosed with cancer are cured (30, 31). Impressively, the median survival of patients with cystic fibrosis has doubled from 14 y in 1969 to 28 y in 1990 (32, 33), largely because of the development of specific medical therapies and transplantation technology that has arisen from our understanding of the pathophysiology of this disease (34) Ironically, the increasing longevity of children with chronic illnesses into adolescence results in these youngsters' participation in the same high-risk health behaviors that threaten the health of all adolescents. Additionally, as a result of increased longevity, adolescents with chronic illnesses continue to suffer long-term growth retardation, as well as the developmental and pubertal delay often associated with chronic illnesses and the therapies used to treat them.
Advances in gynecologic diagnostic and surgical techniques.
The technological advancements that have most dramatically influenced the health of adolescents and secondarily the establishment of the subspecialty of adolescent medicine in the 20th century fall into four general domains and include colposcopy, the Papanicolaou smear, laparoscopy, and newer microbiologic and immunologic techniques. Initially invented by Hinselmann in 1925 [as reviewed by Torres and Riopelle (35)], colposcopy contributed to our knowledge of the occurrence of the “transformation zone,” a prime site for human papillomavirus infection, and its role in the development of carcinoma of the cervix. It also proved to be invaluable in the evaluation of adolescent victims of sexual abuse. The development of the vaginal cytologic smear by Papanicolaou in 1943 reduced the death rate from invasive cervical cancer in adults by 70% but also profoundly influenced the practice of adolescent health care by introducing routine preventative gynecologic care for sexually active adolescent girls (36). Laparoscopy, first used by gynecologists for adults as an interventional surgical technique in the 1960s and 1970s (37), greatly advanced our understanding of the pathophysiology of pelvic inflammatory disease in teens and provided an acceptable alternative to laparotomy for the evaluation of young women with chronic pelvic pain. The specific application of new microbiologic and recombinant techniques to routine screening for chlamydial and gonococcal cervical infections in adolescents has played a significant role in the rapid diagnosis and prevention of teenage pelvic inflammatory disease and its sequelae.
Advances in hormonal contraception.
One of the more significant scientific advances affecting adolescent health is related to the development of hormonal forms of contraception. First developed in the 1930s, the birth control pill revolutionized contraception, as it provided a method that was simple, effective, and not related temporally to the actual intercourse event. Hormonal contraception enabled unmarried adolescent couples to more effectively separate sexual enjoyment from the procreative responsibilities that accompanied unprotected sexual intercourse. Furthermore, combined oral contraceptives continue to be used today to treat adolescent gynecologic disorders, including dysmenorrhea and polycystic ovarian syndrome.
Initially synthesized in the 1950s for the treatment of threatened abortion and endometriosis in adult women, reports of injectable depo-medroxyprogesterone acetate and implantable levonorgestrel as highly effective contraceptives began to appear in the 1960s. The convenience of these contraceptive methods proved to be highly attractive to the adolescent age group, particularly those teens with a history of pharmacologic noncompliance or a previous pregnancy.
The work of Haspel and Andriesse (38) and Yuzpe et al. (39) in the mid-1970s resulted in the development of the estrogen-only, as well as the estrogen-progesterone combination, “morning-after pill,” respectively. The use of the antiprogestin mifepristone (RU486) for first-trimester medical abortions was initially introduced in the late 1980s. These efforts were clearly directed at adults. Contrary to the concern that the availability of postcoital methods of contraception to adolescents discouraged the use of regular methods of contraception, recent studies demonstrated that the use of postcoital contraception actually increased adolescent visits for preventative gynecologic care and contraceptive counseling (40).
By setting clear boundaries for the definition of adolescence using both biologic and psychobehavioral markers, the specialty of adolescent medicine began to emerge as a substantial scientific, clinical, and educational domain. However, the critical scientific advances from work primarily carried out in younger or older individuals in the clinical areas of psychotropic and hormonal contraceptive pharmacology, chronic disease management, and gynecologic diagnostic technologies and treatment, which was now applied to teens, had a profound impact on advancing the field of adolescent medicine as a viable and legitimate subspecialty.
MAJOR CAUSES OF ADOLESCENT MORBIDITY AND MORTALITY
Impact of societal changes on adolescent health.
Scientific advances of the 20th century made a significant contribution to the decline in deaths from natural causes at all ages in the life cycle. Although the death rate from natural causes dropped 90% between 1933 and 1985, presumably preventable causes, such as violence, motor vehicle accidents, and suicide, emerged as the leading causes of death in adolescents in the latter three decades of the 20th century (41). It is not fully understood why adolescent morbidity and mortality related to such potentially preventable occurrences increased so dramatically.
Adolescents' unique relationship to their environment may, in part, explain this increase in morbidity and mortality. In contrast to the infant or young child, the adolescent is an organism that tends to be more highly sensitive to the influences of the broader global environment. The highly protective and controlled social environment of the family unit largely limits the direct exposure of infants and young children to broader societal influences. The environment of the adolescent, on the other hand, has increasingly become less controlled and less restrictive. The adolescent, in the throes of developing physical, social, and psychological independence has therefore become much more vulnerable to broad societal influences. Societal changes that have taken place during the past 100 y have undoubtedly influenced adolescent behaviors and health.
Although a direct causal link between societal changes and adolescent health is often difficult to forge, there are a number of clear associations that cannot be totally neglected. First, the post-World War II baby boom created a demographic shift in which the number of 10- to 20-y-olds in the United States increased from 30 to 40 million by the early 1960s, reflecting a global boom in the adolescent population. The geographic separation of this large population of youth from their homes and familiar societal influences promoted the development of group norms and behaviors that often differed from those of society in general. Traditional religious, work, and interpersonal values were increasingly rejected by youth in the 1960s. This led to increasing sexual experimentation with multiple partners outside of marriage, the wide use of illicit drugs, cigarettes and alcohol, and secondary as well as postsecondary school failure. Second, the women's rights movement had an indirect, yet profound influence on the health of both young men and women. The birth control movement and the idea of emancipation for modern women, initiated by Margaret Sanger, included the right of each woman to decide for herself whether she would become a mother, and if so, when. These changes, influenced by the women's rights movement, gave young couples the opportunity to express and experiment with their sexuality while maintaining control over their ability to become pregnant or carry a pregnancy to term. Alternatively, the “sexual revolution,” ushered in at the same time, had several serious adverse effects on the health of youth. Increasing experimentation with multiple sexual partners and inconsistent contraceptive practices contributed significantly to rising rates of sexually transmitted infections (STIs) and teenage pregnancy. The global AIDS epidemic is partial evidence to support some of the adverse effects of the “sexual revolution.”
The rapidly expanding adolescent population combined with strong societal influences affecting the health of the adolescent patient likely together played a significant role in stimulating the growth of the field. The subspecialty of adolescent medicine is unlike most others, however, in that it is not an organ-specific subspecialty. Similar to neonatology, adolescent health focuses on all aspects of patients belonging to a certain age group. An essential motivating force behind the development of adolescent medicine relates to the unique aspects of the physical, psychological, developmental, and social needs of the adolescent patient. Specifically, the health-care providers who take care of the adolescent patient need to be equipped with special interdisciplinary skills to address the often-complex intertwining of medical, developmental, and psychosocial issues characteristic of the adolescent patient.
The epidemiology of high-risk adolescent behaviors has become a domain of intense study, and adolescent medicine specialists have placed much of their efforts and resources into this general area. Research of high-risk behaviors has examined adolescent experimentation with emerging sexuality, experimentation with tobacco products, illicit drugs, and alcohol, involvement in violence, work- and sports-related injuries, and the development of disordered eating habits relating to issues of distorted body image. Much of the recent research and programatic efforts in the field of adolescent medicine relate to improving our understanding of the causative factors of these behaviors and the preventative strategies to use for the serious consequences of these behaviors.
Sexuality.
In each era of recorded history adolescent sexuality emerged as a prime concern of responsible adults. Although adolescent sexual behaviors are integral to normal adolescent development, we have begun to understand what factors place some adolescents at greater risk from the consequences of participating in these behaviors, and how to mitigate the more serious outcomes of these behaviors.
During the first half of the 20th century nonhormonal contraception or abstinence were the only forms of birth control. With the development of effective antibiotic treatment of gonorrhea and syphilis in the 1940s and the development of “the pill” in the 1950s, however, the limited popularity among teens of nonhormonal contraception began to wane, and abstinence became a less and less frequently adhered-to behavior. An effect of the reduction of support for public health programs aimed at preventing STI in the 1950s and as a result of the “sexual revolution” of the 1960s, teenage pregnancy and birth rates rose in the 1970s, as did the prevalence of penicillinresistant strains of gonorrhea and viral STIs, such as human papilloma virus and herpes simplex virus type 2. Further, the identification of HIV and the AIDS epidemic in the 1980s prompted researchers to clarify which, of many factors, predisposed adolescents to the consequences of these sexual behaviors. Thus, the need to effectively prevent the sequelae of certain sexual behaviors rose to the forefront of public health and social policy concerns (42). Because of their interest and expertise in taking care of the adolescent patient, many of these efforts were lead by subspecialists in adolescent medicine.
Researchers learned that some sexual behaviors are associated with an early age of menarche, lower parental education, limited access to health information, difficulty accessing health services, lack of economic opportunities, and lower socioeconomic status (42, 43). Investigators also learned that childbearing by adolescents may be associated with poor obstetric outcomes, low birth weight babies, and psychosocially disadvantaged children (44). Finally, researchers found that improperly treated gynecologic infections were causally linked to infertility and cervical human papilloma virus infection with its potential for cervical cancer.
Targeted public health efforts to reduce the problems associated with emerging teenage sexuality resulted in a decline in both the pregnancy and birth rates in industrialized countries worldwide during the past three decades and in the incidence of syphilis, gonorrhea, and chlamydia during the past 10 y. Between 1988 and 1995, there was an increase in condom use. A decline in the use of the pill and diaphragm coincided with an increase in condom and long-acting implantable or injectable hormone use (45, 46). Numerous studies indicated that declines in teen pregnancy and STI rates might be influenced by a number of factors. These include 1) increased emphasis on teenage sex education and the motivation by young people to achieve higher levels of education (47); 2) the improved effectiveness of contraceptives; 3) an increase in the use of contraceptives at the time of first intercourse (45, 46); 4) an increase in abstinence rates (48); and 5) an increasingly widespread availability of confidential and accessible contraceptive services.
Cigarettes.
Since the 1920s, cigarette-advertising campaigns have focused on even younger audiences (49), and smoking was promoted as a symbol of independence, emancipation, rebelliousness, and autonomy. The prevalence of smoking among adolescents remained relatively constant from the 1970s throughout the mid- 1980s (50). There was a dramatic increase in cigarette use from 1991 to 1997, with a notable increase in smoking rates among adolescent girls. Very recently, however, there was a significant decrease in overall tobacco use rates from 1997 to 2001 (51).
The 1996 landmark U.S. Food and Drug Administration decision to enact regulations limiting the accessibility and appeal of tobacco products to young people was based on the following findings: 1) the highest lung cancer mortality rates were seen among those who began smoking before the age of 15 y (52); 2) more than 82% of adults acknowledged that they smoked their first cigarette before the age of 18 y; 3) individuals who start smoking in their early teen years were more likely to be heavy smokers than those who began smoking as adults; and 4) the powerful effect of tobacco company advertising on youth smoking rates was demonstrated when, 3 y after the introduction of the R.J. Reynolds tobacco company's Joe Camel campaign, the proportion of smokers younger than 18 y chose Camels and rose from 0.5% to 32.8% (53). The association of smoking with high-risk behaviors was highlighted by results of the 1998 National Household Survey on Drug Abuse. Adolescents age 12-17 y who currently smoked cigarettes were 11.4 times more likely to use illicit drugs and 16 times more likely to drink heavily than nonsmoking adolescents (54).
The use of psychoactive drugs has been a universal phenomena through all ages and cultures; however, substance abuse as a major adolescent issue did not emerge until the 1960s. Heroin use, in particular, was a leading cause of morbidity and mortality among adolescents even though the abuse of other substances was rapidly emerging (55). The morbidity associated with heroin use, including hepatitis and participation in drugrelated criminal activity, spurred the creation of policies and programs specifically directed at fighting the opiate problem. In the late 1960s and early 1970s methadone maintenance programs emerged in hospitals and community settings. These targeted programs were often an important stimulus to the formal organization of comprehensive health services for youth via the adolescent medicine movement.
Peak adolescent drug use occurred in the late-1970s to the mid-1980s, and then decreased, with a concurrent decline in methadone maintenance clinics. A reversal of this trend was seen in the early 1990s with a resurgence of drug use documented in 8th, 10th, and 12th graders by the Monitoring the Future study and 12- through 17-y-olds by the National Household Survey on Drug Abuse. Currently, accidental trauma including motor vehicle accidents, suicide, and homicide account for 75% of all deaths in the 15- to 24-y-old population, but alcohol accounts for 25-50% of all such deaths (56). Alcohol is the drug of choice for high school and college students and has been shown to be a gateway drug for other substances of abuse. Use of alcohol by young adolescents has been directly linked to risk of adult alcoholism. The genetics of alcohol abuse has been well studied and proven. During the past two decades, we have come to appreciate the waxing and waning quality of adolescent substance abuse, requiring an ongoing vigilance among primary caregivers as well as adolescent medicine specialists to recognize early trends in changing adolescent attitudes and beliefs about the dangers associated with particular drugs (56). This is particularly important because of the increasing availability, potency, and purity of drugs the world over.
Violence.
Throughout the past century, societal and cultural violence has been widespread and seriously affected the health and welfare of adolescents on an international scale and across all political and geographic boundaries. Associated with this sociocultural trend, we have observed the emergence of significant levels of adolescent interpersonal violence. In the United States, homicide has become the second leading cause of adolescent death nationwide and first in the urban centers. Adolescent homicide rates have increased dramatically since the mid-1980s to the mid-1990s. Most poignantly, between 1985 and 1994, homicide rates for adolescent boys ages 15 to 19 y increased 166%, surpassing rates for males of all other groups except those ages 20 to 24 y. Firearm-related deaths accounted for 97% of this increase (57). Although the late 1990s saw a slight decline in youth violence (58), adolescents continue to be twice as likely as adults and 10 times more likely than the elderly to be victims of violence (59).
Research in recent years recognized the significant impact of exposure to violence on children and teens as a major determinant to subsequent violent behavior. They have easy access to firearms, alcohol, and drugs, as well as a constant source of violent material from the media, home computers, and video technology. Violent behavior has been linked with poverty, violence in the home, the availability of handguns in the home, exposure to violent television programs, the use of alcohol and illicit drugs, mental illness, and the proliferation of gang activity (58, 60–62). Criminal behavior, often associated with gang activity and interpersonal violence, has resulted in high rates of youth imprisonment. The effectiveness of teen violence prevention strategies aimed at reducing firearm-related deaths is undergoing vigorous study. A number of studies indicate that more-restrictive handgun availability laws are associated with lower rates of homicide and suicide (61), yet efforts aimed at preventing gun use are difficult to sell to many adolescents. Efforts at nonviolent conflict resolution are now being tried with teens.
Sports- and work-related injuries.
During the past 40 y the number of adolescents participating in organized extramural and intramural sports has increased dramatically. Currently some 30 million adolescents and children participate in organized sports within the community, and 3.5 million boys and 2 million girls are members of school sports teams (63). This increased participation in sports is certainly a positive health behavior that is enjoyable, helps to promote teamwork and social skills, and may provide the basis for life-long patterns of fitness and exercise. However, increased participation has also resulted in a greater number of sports injuries, either from the stress of overuse or from trauma during practice or play. Multiple studies have reported injury rates ranging from a low of 3% to, depending on the degree of inclusion of minor injuries, a high of 20%. The evaluation and management of acute injuries and the prevention of long-term sequelae have become a routine part of adolescent health care. Decisions must be made on whether participation should be allowed or when a young person might return to full activity after an injury.
As children with chronic illnesses increasingly survive into their teen years, it has become a common issue for physicians to decide whether to permit sports participation for young people with physiologic deficits, using medications, or having only one paired organ. Often the need to improve self-image and maximize normality in the face of illness motivates the adolescent, the family, and the physician to accept some risk rather than uniformly to deny participation (64).
During the past two decades there has been a major increase in the number of adolescents who are working, with that number now estimated to be more than 5 million each year (65). Approximately 25% of 15-y-olds and nearly half of 16- and 17-y-olds are working (66). Most adolescent jobs take place after school, are part time, and are in the fast food service, retail, construction, or commercial fishing industries (67). An estimated 1 to 2 million adolescents are working beyond the current limits of child labor laws either because of excessive hours or involvement with dangerous machinery prohibited for use by teens (67).
Part-time employment is seen as a valuable experience for adolescents as it provides an introduction to habits and attitudes that will serve as the foundation for a lifelong adult work career. Earning a salary gives the adolescent an opportunity for individuation, independence, and the positive self-image that accompanies paying, at least in part, his or her own way. However, introducing adolescents into the workplace carries with it the risks of diversion from educational goals and the trauma often associated with the lowest paying and most dangerous jobs.
Among the numerous documented adverse consequences of adolescent employment, the most serious is the high rate of work-related injury (68). Boys between the ages of 16 and 17 y are at the highest injury risk with the greatest danger associated with newspaper delivery and agricultural activities. Machinery used for manufacturing, loading and unloading products, or agricultural work produces lacerations, crush injuries, and amputations. Exposure to toxic chemicals such as formaldehyde, dust, or asbestos may exacerbate asthma, as well as cause other health-related problems in the future. Noisy machinery may contribute to hearing loss. In addition, working more than 20 h/wk has been associated with problem behaviors such as substance abuse, sleep and exercise deprivation, and less time spent with family and on schoolwork (56).
Obesity and eating disorders.
The prevalence of obesity in adolescents has increased over the past 30 y. The NHANES III (1988-1994) study revealed that 11% of adolescents 12-17 y of age were obese and 14% were at risk for obesity (69). These data reflect an untoward upward trend for obesity, which approximated only 5% in both the NHANES I (1971-1974) and NHANES II surveys (1976-1980). The most significant reason for this dramatic increase appears to be a sedentary lifestyle adopted by many teens, including increased television watching and video game and computer use, as well as the ingestion of a higher calorie diet with a higher fat content (70). Although a large number of teens are involved in sports on a team or recreational level, the majority is not. This is particularly so among inner city youth and those in lower socioeconomic groups.
The recent increased incidence of type 2 diabetes among adolescents appears to be linked to the increase in teen obesity. This has provided for greater collaboration between pediatric endocrinologists and adolescent medicine specialists. Hyperlipidemia is being diagnosed with greater frequency in obese adolescents, and dietary management is the mainstay of treatment. Functional ovarian hyperandrogenism or polycystic ovary syndrome often first manifests itself during adolescence and has also been linked to obesity and type 2 diabetes.
During the past quarter century, the incidence of other eating disorders such as anorexia nervosa and bulimia nervosa has also increased (71). Many experts attribute the increasing prevalence of anorexia nervosa and bulimia to societal shifts in fashion and style among adolescents. The trend of the miniskirt and the “Twiggy” look in the 1960s certainly contributed to the desire to be thin. In the 1970s and 1980s, this model of fashion was not the norm. However, in the 1990s, the waif look adopted by female models, singers, and actresses soon became popular with teenage girls.
Currently, 0.5% and 1-3% of adolescent girls meet the DSM IV criteria for anorexia nervosa and bulimia, respectively. More importantly, in the most recent Youth Risk Behavior Survey of 1999, 30% of high school students consider themselves overweight, and 43% had tried to lose weight in the past 30 d (24). Eating disorders are seen in all socioeconomic groups and are being seen increasingly in boys. Extensive research has demonstrated that those who suffer from anorexia nervosa have low bone density and are at risk for osteoporosis and vertebral fractures (72). The best response to treatment of such disorders is through a multidisciplinary approach including nutritional supplementation as well as psychopharmacologic agents.
Youngsters surviving into the second decade of life with serious childhood illness patterns coupled with the much larger cohort of healthy-appearing teens who silently carried the burden of later life killers such as adult hypertension and obesity may never, by themselves, have stimulated the evolution of the subspecialty of adolescent medicine. But these cohorts of emerging adolescents in combination with the social and environmental factors of emerging sexuality, tobacco, alcohol, and drug use, violence, work and sports injuries, and aberrant nutritional patterns collectively produced the increasing morbidity and proved to be the major impetus for creation of this subspecialty.
EMERGENCE AND FORMALIZATION OF THE FIELD
The field of adolescent medicine developed as a halfcentury-long consequence of the emergence of several significant scientific advances, major societal changes relating to teen behaviors, and a striking increase in adolescent morbidity and mortality. By the mid-20th century, the convergence of the science and the clinical morbidity had attained sufficient momentum to launch the formal discipline. As the necessity to create new policies in response to the growing unmet needs of adolescents became evident, a small group of physicians caring for adolescents began to take on an advocacy role. The result, as viewed from the start of the 21st century, was the establishment of the academic discipline of adolescent medicine.
Emergence of an academic discipline of adolescent medicine.
The precursor of a formal adolescent medicine initiative appears to have its origins in England in the late 19th century. In 1884, physicians caring for adolescent boys in boarding schools joined together organizing the Medical Officers of Schools Association (73). The first listing in Index Medicus of a published document under the topic of adolescence was by Hall, entitled, “Adolescence: Its Psychology and its Relations to Anthropology, Sociology, Sex, Crime, Religion and Education” [reviewed in Heald (74)]. The first article describing an ambulatory program entirely devoted to adolescents was published by Gates in Archives of Pediatrics [reviewed in Heald (74)].
Sometime after World War I, medical services exclusively for college students were developed at large universities to offer health care to an increasing number of youth that were away from home. The Grant Study, a multidisciplinary project examining healthy, normal undergraduates, was published at the time. Concurrently, primary- and secondary-level private boarding schools in the United States began to use school physicians to develop comprehensive student health services just as had occurred in England almost 50 y earlier (73).
In 1941, a symposium on adolescence was held under the auspices of the American Academy of Pediatrics. Most of the studies presented were the work of college health and boarding school physicians. The themes that emerged from this meeting related to physical fitness, emotional health, and nutrition in adolescents. This meeting is considered by many as the initiating force incorporating adolescent medicine into the domain of pediatric practice. Soon after this, a few medical school departments of pediatrics established academic divisions specifically targeted to the care of adolescent patients and the study and teaching of this unique field.
The first adolescent inpatient unit was opened in 1951 at Boston Childrens Hospital, under the directorship of J. Roswell Gallagher. This unit, among its many accomplishments, initiated the first academic training program in adolescent medicine. Other academic programs soon followed, and later in that decade the U.S. military began to establish specific medical services for adolescents living with their parents on military bases (73). At that time, most of the adolescent medicine research, clinical care, and training efforts was performed by pediatric subspecialists in endocrinology, gastroenterology, and cardiology with assistance from psychologists and psychiatrists (74).
In the middle of the 20th century several professional organizations began to sponsor meetings to teach adolescent health care. In 1955, the American Academy of Pediatrics offered a round table format exclusively discussing adolescence, and 9 y later the American College of Physicians had a 5-d course on the medical care of the adolescent patient.
The first academically complete program in adolescent medicine was initiated in the Bronx by the Division of Adolescent Medicine at Montefiore Medical Center/Albert Einstein College of Medicine in 1967. The program consisted of an exclusive adolescent inpatient unit caring for all medical, surgical, gynecologic, and behavioral problems of teens, an outpatient arm including a juvenile detention facility health service, a separate research laboratory unit, and a social psychology program. These comprehensive adolescent patient services as well as the research experience provided a rich learning environment for the education of postdoctoral fellows, residents, and medical students (75).
The federal government began the funding of adolescent medicine training programs in the 1960s. The Children's Bureau, under Arthur Lesser, supported a fellowship training program in Adolescent Health at the Children's Hospital in Washington, DC, directed by Felix Heald. Several other Children's Bureau-sponsored programs followed in other major cities (76). This initiative ultimately matured and expanded in the late 1970s into the current Department of Health and Human Services, Maternal and Child Health Bureau funding of multidisciplinary training programs in adolescent medicine. In 1965, Felix Heald and Somer Sturgis began a series of annual 3-d seminars at the Children's Hospital in Washington, DC, sponsored by the Children's Bureau grant, which drew primarily pediatric academic faculty to discuss issues and concerns targeted at the adolescent. By 1968, close to two dozen attendees at the Heald-Sturgis seminar formed the Society for Adolescent Medicine (SAM).
The stated goals of SAM were “to improve the quality of health care for adolescents, to encourage the investigation of normal growth and development during adolescence, to study those diseases that affect adolescents, to stimulate the creation of health services for adolescents, to increase communication among health professionals who care for adolescents, and to foster and improve the quality of training of those individuals providing health care to adolescents” (77). Subsequently, other organizations with a primary adolescent health focus were created. The more prominent of these include the North American Society for Pediatric and Adolescent Gynecology, the Society for Research in Adolescence, and the International Society for Eating Disorders. SAM held its first business meeting in 1969, its initial scientific symposium in conjunction with the American Academy of Pediatrics in 1970, and its first independent SAM-sponsored research meeting in 1973. The latter two research forums were organized by Michael I. Cohen. In the spring of 1976, the American Pediatric Society and the Society for Pediatric Research sponsored the first adolescent research session at this annual pediatric academic conference. Heald and Cohen cochaired this initial session for the two sponsoring societies. Each year since, new scientific data have had numerous forums for debate and discussion.
The American Academy of Pediatrics formed the Committee on Adolescence in 1976 to help the executive leadership by better informing their discussions of teen issues. It had previously been known as the Committee on Juvenile Delinquency (1955-1964) and then the Committee on Youth (1965-1976). The Committee on Adolescence has been at the forefront in formulating policies on adolescent health issues from confidentiality and substance abuse screening to the role of the pediatrician in routine adolescent health screening or dealing with the complexity of teenage reproductive issues. In 1979, the Academy formally organized a Section on Adolescent Health, which has been instrumental in providing continuing medical education in the field of adolescent medicine for the practicing pediatrician.
Evolving law on confidentiality, consent, and reproductive rights for adolescents.
Coincident with the emerging attention to adolescent health needs was a rapid evolution of the laws and practices that governed the ability of adolescents to consent to their own care and, when necessary, to receive such care with confidentiality protected. Contributing to this evolution were decisions of the U.S. Supreme Court, decisions within state courts, advances in public health laws, and the increasing recognition by medical societies of the need to publicly support the rights of adolescents to access health care.
In a series of decisions, the U.S. Supreme Court provided the basis for emerging adolescent health care rights. In 1973, the Roe v. Wade decision established the right of women to termination of pregnancy, regardless of age. Although subsequent decisions of the Supreme Court upheld the constitutionality of state laws requiring either parental consent or parental notification for a minor to receive an abortion, even those decisions recognized the need to provide an alternative route for consent, or “judicial bypass,” for those circumstances in which the teenager was unwilling or unable to seek parental consent. In 1972, the Supreme Court ruled that it was a violation of the constitutional right to privacy to preclude the prescription of contraceptives to unmarried adults, and 5 y later, the Court extended these Fourteenth Amendment rights to minors. In so doing, the Court stated “Rights do not mature magically at adulthood,” implying an evolution of health care rights in accord with the adolescents' emerging ability to understand the consequences of consenting to or refusing care.
Within individual states, there were continuing decisions recognizing and defining the concepts of the emancipated minor and the mature minor. Since the earliest days of English law, adolescent parents were considered to be emancipated, free to consent to their own care and the care of their children. In addition, by the end of the 1960s, all 50 states had public health law provisions allowing adolescents to receive care for the evaluation or treatment of STIs without parental knowledge or consent (78). This heralded the movement to establish free clinics in large urban centers to treat STIs as well as an initiative to develop hospital-based clinics for the same purpose. Within a decade, such provisions were extended to the treatment of alcohol and substance abuse.
In 1989 several national medical organizations, including the American Academy of Pediatrics, the American Academy of Family Physicians, and the American College of Obstetricians and Gynecologists, issued a joint statement advancing the right to “Confidentiality in Adolescent Health Care” (79). That statement, although recognizing that in many circumstances the involvement of parents in adolescent medical decision making was to be encouraged as valuable, concluded that health professionals had an ethical obligation to provide the best possible care and counseling to their adolescent patients and that “Ultimately, the health risks to the adolescent are so impelling that legal barriers and deference to parental involvement should not stand in the way of needed care” (79).
School-based clinics.
Another venue in which governmental policy influenced the growth of the field of adolescent medicine was in fostering the establishment of school-based health centers. For more than a century, schools have been a site for health-care initiatives including immunizations, vision and hearing screening, scoliosis screening, and sports preparticipation physicals. Over the last 15 y, however, schools have become more comprehensive community-based health centers providing a multitude of services to adolescents and families (80). Edwards et al. (81) claimed school-based clinics were an effective vehicle in reducing pregnancy rates in adolescents. This work stimulated the interest of organizations such as the Robert Wood Johnson Foundation to fund the development and expansion of school-based clinics.
Not-for-profit foundations began funding school-based health centers in the late 1980s, thus joining the governmental initiatives. School-based health centers have been the site of interdisciplinary care for adolescents and have also become a site for specific health-care initiatives such as asthma education or addressing specific risk-taking behaviors. This has fostered a partnership with traditional school educators to address mental health and family education initiatives.
A body of literature takes form.
Dale Garell initiated the publication of an Adolescent Medicine Newsletter in 1965, which became the official informational publication of SAM in 1968 and was the forerunner of the current SAM journal. In 1980, SAM launched the Journal of Adolescent Health Care, under the founding editorship of H. Verdain Barnes. Currently, a series of other journals dedicated to the field of adolescent medicine exist and include Adolescence, Journal of Research on Adolescence, Journal of Adolescent Research, Journal of Youth and Adolescence, Journal of the North American Society for Pediatric and Adolescent Gynecology, and Adolescent Medicine: State of the Art Reviews.
The codification of the body of literature in adolescent medicine began in the mid-1960s with the first adolescent health-care textbook, Medical Care of the Adolescent by J. Roswell Gallagher. Several more quickly followed, including The Adolescent Patient by William A. Daniel, Jr; Adolescent Sexuality in Contemporary America—Personal Values and Sexual Behavior Ages 13-19 by Robert C. Sorensen; Comprehensive Adolescent Health Care, edited by Friedman, Schonberg, Fisher, and Alderman; Adolescent Health Care: A Practical Guide by Neinstein; and Pediatric and Adolescent Gynecology by Emans, Laufer, and Goldstein.
Philanthropic and private foundation initiatives.
The 1980s saw a dramatic increase of funding for research and training programs in adolescent medicine by the nongovernmental sector. Much of this was stimulated by advances in the science of adolescent developmental biology and psychology. In 1982, The Robert Wood Johnson Foundation funded programs linking academic medical centers with local health agencies (74). Four years later, this same foundation began funding the establishment of school-based clinics. The success of this latter initiative led the way for many state governments to fund similar health programs in schools. Starting in 1986, the Carnegie Corporation of New York sponsored publication of three major treatises and numerous position papers on the status of adolescents in the United States, which grew out of deliberations of the 10-y term of Carnegie's Council on Adolescent Development led by David Hamburg and Ruby Takanishi.
In 1988, the American Medical Association (AMA) established a Department of Adolescent Health that emerged as a recommendation of a seminal report on adolescent health funded by this group. In the early 1990s this AMA department, under the leadership of Arthur Elster, moved the health promotion of adolescents to the forefront with the development of Guidelines for Adolescent Preventive Services (GAPS). By leading a team of health professionals in adolescent medicine, mental health, nutrition, infectious diseases, and public policy, the AMA, via its GAPS program, recognized that the effective health care of adolescents must address the morbidity associated with high-risk sexual activity, substance abuse, eating disorders and obesity, and school problems. Initiatives such as GAPS highlighted health promotion. The American Academy of Pediatrics, in conjunction with the Maternal and Child Health Bureau, developed a similar health promotion initiative called Bright Futures, which uniquely included aspects of the adolescent's role in the community. Both GAPS and Bright Futures included parenting and anticipatory guidance standards for parents of adolescents.
International initiatives.
Adolescent medicine had its origins in England in the late 19th century, with a small group of physicians who cared for adolescent boys in boarding schools. This group ultimately formed the Medical Officers Schools Association in 1884. In the early and mid-20th century, with the economic downturn and two major global conflicts in Europe, interest in academic adolescent medicine waned on an international level.
Although currently there are adolescent medicine training programs internationally, there are no fellowship programs outside North America that provide certification and credentialing. Divisions of adolescent medicine and attendant fellowship programs exist in Canada. The founders of these Canadian units were trained in the United States in the 1960s and started programs in Montreal and Toronto in the late 1960s and early 1970s. Martin Wolfish was one such leader.
Physicians practice adolescent medicine throughout Europe and Israel, with a growing contingent in Latin America. International adolescent medicine societies such as the International Association of Adolescent Health, which evolved out of the 4th International Symposium on Adolescent Health held in Sydney, Australia, in 1987, draw hundreds of attendees to their meetings. International conferences in adolescent medicine are also held in Europe, Latin America, and Australia. These organizations and their conferences have fostered the growth of the field in these nations. Moreover, they have provided a venue for collegial communication, as well as presentation of scientific advancements in regions where the numbers of adolescent medicine specialists are small and dispersed geographically. In some countries, there are programs with a targeted disease orientation reflecting the interest of the responsible medical leadership. Unfortunately, there are few adolescent medicine specialists who practice in Asia and Africa, despite the critical need.
According to the records of SAM at the time of the preparation of this manuscript, there are 105 members residing outside North America (personal communication). This represents approximately 7% of the SAM membership. The American Academy of Pediatrics Section of Adolescent Health has three members from South and Central America (personal communication). The challenges of further developing the field of adolescent medicine at an international level are many. Numerous countries have restricted health budgets and so have few economic resources to fund adolescent-specific services. Currently, these nations do have maternal-child health aid programs, and the hope is that some of these programs will extend their services to engage the adolescent patient. Second, many nations have cultural and religious norms that do not recognize adolescence as a distinct group with unique healthcare needs. This is often a serious barrier to establishing special services for the adolescent, who is perceived, in such settings, as either an older child or a young adult. Finally, there are significant areas of the world where the established medical systems do not recognize adolescent medicine as a discipline distinct from pediatrics, internal medicine, obstetrics and gynecology, or family practice.
Adolescent medicine—a boarded subspecialty in pediatrics.
As various academic and governmental units were coalescing to form the infrastructure needed to support a new field of pediatric endeavor, a seminal event occurred in 1976 to solidify the subspecialty. All the pediatric societies formed the Task Force on Pediatric Education chaired by C. Henry Kempe. The report of the Task Force, published in 1978, gave prominence and legitimacy to the subspecialty and, ultimately, led to sub-board certification, accreditation of training, and the emergence of formal curricula for the preparation of future clinicians and investigators (82, 83). The American Board of Pediatrics administered the first examination for sub-board certification in adolescent medicine in November 1994 after several years of intense debate among many in the field. Among the 295 pediatricians who sat for the first examination, 76.6% passed. The test was administered in 1997, 1999, and 2001. As of March 2002 there were 489 Diplomates of the American Board of Pediatrics who were also Board Certified in Adolescent Medicine. In 1998 the Accreditation Council on Graduate Medical Education through its Pediatric Residency Review Committee process reviewed 18 adolescent medicine fellowship-training programs, and 16 were accredited. As of March 2002, there were 25 adolescent medicine fellowshiptraining programs accredited by the Accreditation Council of Graduate Medical Education.
Thus, the academic field of adolescent medicine joined the ranks of other subspecialties in pediatrics, having emerged as a unique product of an extraordinary century filled with scientific advances and sociopolitical changes.
CONCLUSIONS
The field of adolescent medicine was borne out of scientific advances from a wide variety of disciplines, changes in societal mores, and the explosion of technology that occurred during the 20th century. The past 100 y of clinical practice and research have provided a wealth of information that has improved our understanding of the biologic and physical development of adolescents as well as the epidemiology of high-risk adolescent behaviors. The challenge for all providers of health care to adolescents, as we enter the new millennium, is to continue to examine the effect of these high-risk behaviors and to develop mechanisms to address and limit the impact of these behaviors, just as the scientists and practitioners of the 20th century made great strides in treatment and cure of medical illnesses. With a broad base of scientific knowledge, formalization of an academic field, and strong government and organizational support, many of us in adolescent medicine are energized by these factors and can only envision continued growth and maturation of this field.
REFERENCES
Greulich WW, Pyle SI 1950 Radiographic Atlas of Skeletal Development of the Hand and Wrist, 2nd ed . Stanford University Press, Stanford, CA, pp 1 – 256
Stuart HC 1938 Normal growth and development during adolescence . N Engl J Med 234 : 666 – 672, 693-700, 732–738
Marshall WA, Tanner JM 1969 Variations in pattern of pubertal changes in girls . Arch Dis Child 44 : 291 – 303
Marshall WA, Tanner JM 1970 Variations in the pattern of pubertal changes in boys . Arch Dis Child 45 : 13 – 23
Acheson RM, Vicinus JH, Fowler GB 1966 Studies in the reliability of assessing skeletal maturity from x-rays . Hum Biol 38 : 204 – 218
Brozek J 1966 Body composition: models and estimation equations . Am J Phys Anthropol 24 : 239 – 246
Frisch RE, McArthur JW 1974 Menstrual cycles: fatness as a determinant of minimum weight for height necessary for their maintenance or onset . Science 185 : 149 – 151
Wyshak G, Frisch RE 1982 Evidence for a secular trend in age of menarche . N Engl J Med 306 : 1033 – 1035
Herman-Giddens ME, Slora EJ, Wasserman RC, Bourdony CJ, Bhapkar MV, Koch GG, Hasemeier CM 1997 Secondary sex characteristics and menses in young girls seen in office practice: a study from the pediatric research in office settings network . Pediatrics 99 : 505 – 512
Boyar RM, Wu RH, Roffwarg H, Kapen S, Weitzman ED, Hellman L, Finkelstein JW 1976 Human puberty: 24-hour estradiol in pubertal girls . J Clin Endocrinol Metab 43 : 1418 – 1421
Zumoff B, Bradlow HL, Finkelstein J, Boyar RM, Hellman L 1976 The influence of age and sex on the metabolism of testosterone . J Clin Endocrinol Metab 42 : 703 – 706
Boyar R, Finkelstein J, Roffwarg H, Kapen S, Weitzman E, Hellman L 1972 Synchronization of augmented luteinizing hormone secretion with sleep during puberty . N Engl J Med 287 : 582 – 586
Finkelstein JW, Roffwarg HP, Boyar RM, Kream J, Hellman L 1972 Age-related change in the twenty-four hour spontaneous secretion of growth hormone . J Clin Endocrinol Metab 35 : 665 – 670
Reiter EO, Grumbach MM 1982 Neuroendocrine control mechanisms and the onset of puberty . Annu Rev Physiol 44 : 595 – 613
Salz JL, Daum F, Cohen MI 1973 Serum alkaline phosphatase activity during adolescence . J Pediatr 82 : 536 – 537
Bennett DL, Ward MS, Daniel WA 1976 The relationship of serum alkaline phosphatase concentrations to sex maturity ratings in adolescents . J Pediatr 88 : 633 – 636
Daniel WA Jr 1973 Hematocrit: maturity relationship in adolescence . Pediatrics 52 : 388 – 394
Hall GS 1904 Adolescence: Its Psychology and Its Relations to Anthropology, Sociology, Sex, Crime, Religion, and Education . D. Appleton and Company, New York
Piaget J, Inhelder B 1958 The Growth of Logical Thinking from Childhood to Adolescence . Basic, Books, New York, pp 1 – 384
Erikson E 1966 Eight ages of man . Int J Psychiatry 2 : 281 – 307
Elkind D 1998 All Grown Up and No Place To Go: Teenagers in Crisis, rev. ed . Perseus Books, Cambridge, MA, pp 40 – 45
Garmezy N 1991 Resilience in children's adaptation to negative life events and stressed environments . Pediatr Ann 20 : 459 – 460, 463–466
Rutter M 1979 Protective factors in children's response to stress and disadvantage . In: Kent MW, Rolf JE (eds) Primary Prevention of Psychopathology, Vol. 111—Social Competence in Children . University Press of New England, Hanover, NH, pp 49 – 74
Centers for Disease Control and Prevention. CDC Surveillance Summaries June 9, 2000 Morb Mortal Wkly Rep 2000 ; 49 ( No.SS-5 )
Weist MD, Ginsburg G, Shafer M 1999 Progress in adolescent mental health . AdolescMedSTARS 10 : 165 – 173
Bradley C 1938 The behavior of children receiving benzedrine . Am J Psychiatry 94 : 577 – 585
Barkley RA 1977 A review of stimulant drug research with hyperactive children . J Child Psychol Psychiatry 18 : 137 – 165
Daly JM, Wilens T 1998 The use of tricyclic antidepressants in children and adolescents . Pediatr Clin North Am 45 : 1123 – 1135
Gortmaker SL, Sappenfield W 1984 Chronic childhood disorders: prevalence and impact . Pediatr Clin North Am 31 : 3 – 18
Siegel EG, Mahan JD, Johnson RS 1994 Solid organ transplantation in adolescents: the blessing and the curse . Adolesc MedSTARS 5 : 293 – 309
Mulhern RK, Ochs J 1994 Caring for adolescent cancer survivors: surveillance and intervention for delayed sequelae of malignancy and its treatment . Adolesc Med-STARS 5 : 259 – 269
Birnkrant DJ, Hen J Jr, Stern RC 1994 The adolescent with cystic fibrosis . Adolesc MedSTARS 5 : 249 – 258
Fitzsimmons SC 1993 The changing epidemiology of cystic fibrosis . J Pediatr 122 : 1 – 9
Shennib H, Adoumie R, Noirclerc M 1992 Current status of lung transplantation for cystic fibrosis . Arch Intern Med 152 : 1585 – 1588
Torres JE, Riopelle MA 1993 History of colposcopy in the United States: chronology of colposcopy development worldwide . Obstet Gynecol Clin North Am 20 : 1 – 6
Beach RK Cervical findings and the Pap smear . In: Friedman SB, Fisher MM, Schonberg SK, Alderman EM (eds) Comprehensive Adolescent Health Care, 2nd ed . Mosby, St. Louis, MO, pp 1057 – 1072
Perissat J, Collet D, Monguiloon N 1998 Advances in laparoscopic surgery . Digestion 590 : 606 – 618
Haspel AA, Andriesse R 1973 The effect of large doses of estrogens post coitum in 2000 women . Eur J Obstet Gynaecol Reprod Biol 3 : 113 – 117
Yuzpe AA, Thurlow HJ, Ramzy I, Leyshon JI 1974 Post-coital contraception—a pilot study . J Reprod Med 13 : 53 – 58
Gold MA, Stewart BA 2000 The impact of using emergency contraception on reproductive behavior among sexually active adolescents in an inner-city clinic: a retrospective review . JAH 26 : 96
Fingerhut LA, Kleinman JC 1989 Trends and current status in childhood mortality, U.S. 1900-1985 . In: Vital and Health Statistics Series 3, no. 26 . National Center for Health Statistics, Hyattsville, MD, pp 1 – 43
Singh S, Darroch JE 2000 Adolescent pregnancy and childbearing: levels and trends in developed countries . Fam Plann Perspect 32 : 14 – 23
Panchaud C, Singh S, Feivelson D, Darroch JE 2000 Sexually transmitted diseases among adolescents in developed countries . Fam Plann Perspect 32 : 24 – 32, 445
Fraser AM, Brockert JE, Ward RH 1995 Association of young maternal age with adverse reproductive outcomes . N Engl J Med 332 : 113 – 117
Abma JC, Chandra A, Mosher WD, Peterson LS, Piccinini LJ 1997 Fertility, family planning, and women's health: new data from the 1995 national survey of family growth . Vital Health Stat 23 : 1 – 11
Piccinino LJ, Mosher WD 1998 Trends in contraceptive use in the United States: 1982-1995 . Fam Plann Perspect 30 : 4 – 10, 45
Santow G, Bracher M 1999 Explaining trends in teenage childbearing in Sweden . Stud Fam Plann 30 : 169 – 182
Darroch J, Singh S 1999 Why is Teen Pregnancy Declining, the Role of Abstinence, Sexual Activity, and Contraceptive Use . The Alan Guttmacher Institute, New York, pp 1 – 23
Gostin L, Arno PS, Brandt AM 1997 FDA regulation of tobacco advertising and youth smoking: historical, social and constitutional perspectives . JAMA 277 : 410 – 418
Nelson DE, Giovino GA, Shopland DR, Mowery PD, Mills SL, Eriksen MP 1995 Trends in cigarette smoking among US adolescents, 1974 through 1991 . Am J Public Health 85 : 34 – 40
Grunbaum J, Kann L, Kinchen SA 2002 Youth Risk Behavior Surveillance—United States, 2001 . MMWR Morb Mortal Wkly Rep 51 : 62
[No authors listed] 1999 Cigarette smoking among high school students—11 states, 1991-1997 . MMWR Morb Mortal Wkly Rep 48 : 686 – 692
Di Franza JR, Richards JW, Paulman PM, Wolf-Gillespie N, Fletcher C, Jaffe RD, Murray D 1991 RJR Nabisco's cartoon camel promotes Camel cigarettes to children . JAMA 266 : 3149 – 3153
Substance Abuse and Mental Health Services Administration, Office of Applied Studies 1999 Summary of Findings from the 1998 National Household Survey on Drug Abuse . U.S. Department of Health and Human Services, Rockville, MD, pp 1 – 138
Chemical Dependency Research Working Group 1994 Methadone Treatment Works: A Compendium for Methadone Maintenance Treatment . New York State Office of Alcoholism and Substance Abuse Services, pp 1 – 63
Comerci GD, Schwebel 2000 Substance abuse: an overview Adolesc Med STARS 11 : 79 – 101
Centers for Disease Control and Prevention 1996 Trends in rates of homicide, United States: 1985-1994 . MMWR Morb Mortal Wkly Rep 45 : 460 – 464
Pratt HD, Greydanus DE 2000 Adolescent violence concepts for a new millennium . AdolecMedSTARS 11 : 103 – 125
Hennes H 1998 A review of violence statistics among children and adolescents in the United States . Pediatr Clin North Am 45 : 269 – 280
Williams KR 1984 Economic sources of homicide: re-estimating the effects of poverty and inequality . Am Soc Rev 49 : 283 – 289
Freed LH, Vernick JS, Hargarten SW 1998 Prevention of firearm-related injuries and deaths among youths . Pediatr Clin North Am 45 : 427 – 438
Melzer-Lange MD 1998 Violence and associated high-risk health behavior in adolescents: substance abuse, sexually transmitted diseases, and pregnancy of adolescents . Pediatr Clin North Am 45 : 307 – 317
Dyment PG (ed) 1991 Sports Medicine: Health Care for Young Athlete, 2nd ed . American Academy of Pediatrics, Elk Grove Village, IL, pp 147 – 161
[No authors listed] 1994 Medical conditions affecting sports participation . Pediatrics 94 : 757 – 760
Cogbill TH, Busch HM Jr, Stiers GR 1985 Farm accidents in children . Pediatrics 76 : 562 – 566
Kipke MD (ed) 1999 Risks and Opportunities: Synthesis of Studies on Adolescence . National Academy Press, Washington, DC, p 43
Landrigan PJ, Pollack SH, Godbold JH, Belville MA 1995 Occupational injuries: epidemiology, prevention and treatment . AdolecMedSTARS 6 : 207 – 215
Belville R, Pollack SH, Godbold J, Landrigan PJ 1993 Occupational injuries among working adolescents in New York State . JAMA 269 : 2754 – 2759
Troiano RP, Flegal KM 1998 The causes and health consequences of obesity in children and adolescents . Pediatrics 101 : 497 – 504
Dietz WH Jr, Gortmaker SL 1985 Do we fatten our children at the television set? . Pediatrics 75 : 807 – 812
Becker AE, Grinspoon SK, Klibanski A, Herzog DB 1999 Eating disorders . N Engl J Med 340 : 1092 – 1098
Bachrach LK, Guido D, Katzman D, Litt IF, Marcus R 1990 Decreased bone density in adolescent girls with anorexia nervosa . Pediatrics 86 : 440 – 447
Gallagher JR 1982 The origins, development and goals of adolescent medicine . J Adolesc Health Care 3 : 57 – 63
Heald F 1992 History of adolescent medicine: a personal perspective . In: Friedman SB, Fisher M, Schonberg SK (eds) Comprehensive Adolescent Health Care, 1st ed . Quality Medical Publishing, St. Louis, MO, pp 15 – 18
Hein K, Cohen MI, Litt IR, Schonberg SK, Meyers MM, Marks A, Sheehy AJ 1980 Juvenile detention: another boundary issue for physicians . Pediatrics 66 : 239 – 245
MacKenzie RG, Fisher MM 1998 The society for adolescent medicine's role in promoting education . J Adolesc Health 23S : 135 – 142
Brown RC, Cromer BA, Brookman RR, Moore E 1998 Introduction . J Adolesc Health 23S : 133 – 134
Holder AR 1985 Legal Issues in Pediatrics and Adolescent Medicine, 2nd ed . Yale University Press, New Haven, pp 123 – 145
American Academy of Pediatrics, Committee on Adolescence, Position Paper: Confidentiality in Adolescent Health Care RE 9151-1989, reaffirmed 1993
Kipke MD (ed) 1999 Risks and Opportunities: Synthesis of Studies on Adolescence . National Academy Press, Washington, DC, pp 22 – 23
Edwards LF, Steinman ME, Arnold KA, Hadanson EY 1980 Adolescent pregnancy prevention services in high school clinics . Fam Plann Perspect 12 : 6 – 14
Report by the Task Force on Pediatric Education 1978 The Future of Pediatric Education . Evanston, IL
Cohen, MI 1980 Importance, implementation, and impact of the adolescent medicine components of the report of the Task Force on Pediatric Education . J Adolesc Health 1 : 1 – 8
Acknowledgements
The authors thank S. Kenneth Schonberg, Susan Coupey, Stanford Friedman, and Laurence Finberg for their thoughtful reviews of this manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Alderman, E., Rieder, J. & Cohen, M. The History of Adolescent Medicine. Pediatr Res 54, 137–147 (2003). https://doi.org/10.1203/01.PDR.0000069697.17980.7C
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/01.PDR.0000069697.17980.7C