Abstract
Little is known about the microvascular perfusion of the skin postnatally. Skin microvascular parameters can be assessed noninvasively with orthogonal polarization spectral imaging (OPS), a technique where, through the use of special optics, a virtual light source is created at a depth of 1 mm within the tissue. The light is absorbed by the Hb, yielding an image of the illuminated Hb-carrying structures in negative contrast. In nine term (weight 2100–4470 g) and 28 preterm infants (weight 550–2070 g; gestational age 24–33 wk) red blood cell velocity and vessel diameter and density were determined off-line with the Cap-Image program in vessels video-recorded by OPS near the axilla on d 1 and 5 of life. Blood pressure, heart rate, hematocrit, and body and incubator temperature were noted. Vessel diameter ranged from 6 to 24 μm, vessel density from 219 to 340 cm/cm2 with no change between d 1 or 5 and no difference between term and preterm infants. Red blood cell velocity increased in preterm infants from d 1 [median 528 μm/s, 95% confidence interval (CI) 486–564 μm/s] to d 5 (median 570 μm/s; 95% CI 548–662 μm/s;p = 0.001) and correlated with the decrease in median hematocrit from 44% (CI 40%–60%) to 39% (CI 37%–43%) with r2 = −0.37 with a 95% CI −0.59 to −0.11, p = 0.006. Hematocrit correlates with red blood cell velocity in the microvessels of the skin. The new technology can be used to assess quantitative changes in the microvessels and thus allows noninvasive assessment of tissue perfusion in term and preterm infants.
Similar content being viewed by others
Main
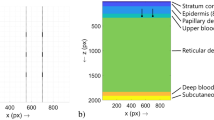
At birth, the skin is richly supplied by a dense subepidermal plexus that shows relatively little regional variation. Even the middle and deep dermis are richly endowed with vasculature. The mature pattern of capillary loops and of the subpapillary venous plexus is not present at birth. With exception of the palms, soles, and nail beds, the skin at birth has almost no papillary loops, but demonstrates a disorderly capillary network. By the end of the first week of life, the capillary network assumes a more orderly pattern. Papillary loops begin to appear as small superficial dilatations or buds in the second week and cooling of the skin appears to encourage maturation. The skin architecture in newborns is notably different from those of an adult. Whereas the latter regularly shows loops of capillaries running orthogonal to the surface of the skin, the neonate has a more horizontal structure, which is readily seen through the very thin upper layers (1–4).
Cardiac output normalized to mass is much higher in the newborn than in the adult. Because of the high resting cardiac output of neonates there is limited reserve to further augment blood flow under stress. Perfusion pressure is maintained by redistributing marginal cardiac output and oxygen supply to brain, heart, and adrenal gland. Under no stress conditions the skin has high blood flow in relation to its oxygen requirement. Assessment of skin perfusion is therefore of great interest, but there is only very scant data about the microcirculatory perfusion in the skin of term neonates and no data for preterm infants (5, 6). Density of perfused skin vessels has never been measured in neonates in vivo. Current methods for clinical investigation of the cutaneous microcirculation in patients are based on laser Doppler flowmetry and capillary videomicroscopy. Capillary videomicroscopy in the neonate so far has been limited to the vascular bed of the nailfold in term infants (6). Direct observation of vascular beds of other organs in humans has been difficult or even impossible because of the need for tissue transillumination and fluorescent dyes for contrast enhancement, or by the size of instruments required to obtain images. Using a similar basic technique described by Slaaf et al. (7), who reported an intravital microscopy technique with two orthogonal polarizers, Groner et al. (8) developed a hand-held portable instrument that allows access in patients to a variety of vascular beds. The OPS imaging technique has been incorporated into the CYTOSCAN A/R (Cytometrics, Philadelphia, PA, U.S.A.), which also allows measurements in incubators. The aim of the study was to determine whether this technique allows one to obtain images of the microcirculation in the skin of term and preterm infants and if these images can be used to quantitatively measure RBC velocity, vessel diameter, and vessel density in vivo.
METHODS
Imaging.
In OPS imaging, a virtual light source is created at a depth of approximately 1 mm within the tissue through the use of special optics. The light shining back through the tissue is absorbed by Hb, yielding an image of the illuminated vessel in negative contrast with a resolution of 1 pixel ≅ 1 μm. Because no fluorescent dyes are needed, it can be used in humans. The method has been validated for quantitative measurements of microcirculatory parameters in an animal model against intravital fluorescence microscopy (9). Figure 1 shows the instrument in an incubator obtaining images in a 24-wk gestational infant on d 1 of life.
Calculation of vessel diameter, RBC velocity, and vessel density.
Images were created using the CYTOSCAN A/R, stored on videotape, and analyzed off-line. Vessel diameter, vessel density, and RBC velocity were measured with the well-established Cap-Image (Dr. Zeindl GmBH, Heidelberg, Germany) program (10) in as many vessels as possible per observation area. To measure the diameter, a vessel is selected from the image on the video screen and a line is placed perpendicularly between the outer edges of the microvessel (Fig. 2). RBC velocity is measured using a technique called line-shift diagram, which requires a 10-s video sequence in which the tissue reveals little movement. Line-shift diagram is a space/time representation that can be used to calculate the velocity of particles moving along a line. The pixels in a line drawn down the middle of a vessel are lined up horizontally, with the time being represented by the x axis and the line itself forms the y axis. Red cells or plasma gaps traveling along the line thereby produce diagonal stripes in the line-shift diagram. From the slope and the length of these stripes, the distance the object has moved during a certain time period can be determined and the velocity calculated. The maximum velocities that can accurately be measured are approximately 1.5 mm/s, so under physiologic conditions it is impossible to measure velocity in arterioles. Vessel density is defined as the length of RBC-perfused vessels per observation unit area and is given as centimeters per square centimeters. Using the Cap-Image software program, the perfused vessels within the defined area are traced and the length of the marked vessels calculated per area of observation (11). In this article, the expression “vessel density” refers to RBC-perfused microvessels.
Measurement of vessel diameter and RBC velocity. Image of the skin of a preterm infant with a gestational age of 24 wk on d 5. RBC velocity is measured by drawing a line down the center of the vessel (1); the pixels along the line are displayed on the screen over the observation period and aligned vertically in a space-time diagram (not shown). To measure a diameter, a line is placed perpendicular between the outer edges of the microvessel (2–5). The Cap-Image software program calculates vessel diameter and RBC velocity. Vessel diameters were 24 μm (2), 43 μm (3), 5 μm (4), and 8 μm (5). Large vessels (3) disappear into deeper layers of the skin and are difficult to get into focus, so RBC velocity cannot be determined. On the other hand, in very small vessels (4), the line for the line shift diagram might not stay in the vessel for 10 s, so RBC velocity determination is inaccurate. The arrow points at lanugo hair, which is frequently seen in images of very premature infants.
Quantitative measurement of vessel density, vessel diameter, and RBC velocity using OPS imaging all have been validated against fluorescent intravital microscopy in the hamster dorsal skinfold model and the rat liver (8, 9, 12).
Subjects.
OPS imaging was performed on d 1 and 5 of life in term and preterm infants after parental consent. The study was approved by the ethics committee of the medical faculty of the Ludwig-Maximilians University Munich.
Premature infants were nursed in incubators at ambient temperatures and term neonates in open cribs. Optimal site evaluation was done in the preterm infants dressed only with a diaper in incubators. Measurements were attempted on various sites, namely the head, abdomen, flank, sternum, and extremities. The probe was placed next to the infant's skin with the least possible contact to avoid pressure against the skin. Lubricating the skin with normal saline improved imaging. Measurements were started when the infants settled down and went to sleep. In preterm infants, MAP was recorded either via an arterial line (BD, Franklin Lakes, MJ) with an Ohmeda Statham transducer (Ohmeda PPD, Liberty Corner, NJ, U.S.A.), if in place, or oscillometrically (Dinamap Vital Data Monitor, Critikon, Norderstedt, Germany). Heart rate and body core temperature were also recorded with a skin probe over the liver as was incubator temperature. The general state of the microcirculation was clinically assessed with a semiquantitative score, taking into account capillary refill time, skin color, and temperature of the extremities (Table 1). Capillary refill time is a frequently used clinical test in which moderate pressure is applied on the skin –in newborns mostly over the sternum—for 1–2 s, and the time until return to baseline color is measured (13). Hematocrit values were determined by centrifugation within 4 h of the OPS measurement.
Statistics.
For comparison between d 1 and 5 within the groups, paired Student t test for parametric data or the Wilcoxon signed rank test for nonparametric data (score and capillary refill time) and between-group Mann-Whitney nonparametric tests were used. For correlation, the Spearman rank two-way test was applied. All calculations were done with GraphPad Prism 3.0 for Windows 95 (GraphPad Software, San Diego, CA, U.S.A.).
RESULTS
A total of 37 infants, 9 normotensive and normothermic term and 28 preterm, were studied on d 1 and 5. Gestational ages ranged from 24 to 41 wk, birth weight from 550 g to 2070 g in preterm and 2100 g to 4470 g in term infants. Clinical data for the preterm infants are shown in Table 2. There was no significant difference for any of the clinical data between d 1 and 5 except for a significant weight loss, lower incubator temperature, and lower hematocrit on d 5. According to the clinical score, none of the infants showed evidence of an impaired microcirculation and only five infants had blood pressures at the lower limit for their gestational age. At the time of measurement, two received catecholamine infusions and two were treated with steroids for hypotension.
Evaluation of optimal site for measurements.
The best images were obtained from the skin of the inner upper arm. In preterm infants, many areas of the skin and particularly the forehead and the temples are covered with lanugo hair, which may interfere with the imaging. Other parts of the body, such as the flanks, the chest, or the abdomen are prone to movement artifacts from breathing, and infants are quite sensitive to light touch and start to wiggle. Overall, it was easier to obtain good quality images in preterm infants because of their thin, well-vascularized skin. In term infants, skin folds were always seen and the images could not be focused as well as in preterm infants. Moistening the skin with normal saline improved imaging, in particular in term infants. With the very low energy of the light source used, no negative effects to the skin, even in the very preterm infants, could be detected. The capillary network appeared more disorderly in the images obtained on d 1 in comparison to d 5, both in preterm and term infants as described in the literature (1–4). No attempt was made to quantify these changes.
Microcirculatory parameters.
Inasmuch as recording time and capillary visualization varied, a different number of vessels in each infant and at each day was measured. From 74 recordings, 1,356 determinations of vessel diameter and RBC velocity were possible (mean ± SD: 18 ± 12 vessels per patient and day; range: 5–83). Vessel density was calculated from five images per patient and day. RBC velocity in vessels with diameters >20 μm could not be measured reliably because these vessels were deeper in the cutis and therefore yielded a fuzzier image and had only very short straight segments. Vessel diameter and RBC velocity were therefore determined in small, well-visualized vessels with microvessel diameters from 6 to 24 μm. Distribution of the diameters are shown in Figure 3. As described in “Methods,” vessels needed to be fairly stable for approximately 10 s to calculate RBC velocity. Very small capillaries with diameters <5 μm were usually unsuitable inasmuch as the slightest movement moved the line out of the vessel and velocity measurements were not reliable. In larger vessels, the line stayed within the vessel for most of the 10-s time period and velocity measurements were more accurate. Due to the immaturity of the microvasculature of the newborn, skin arterioles and venules could not be differentiated with certainty. RBC velocities ranged from 150 to 1100 μm/s with a median of 497 μm/s. Spatial variation in RBC velocity in the same individual at the same time point was pronounced in some subjects with differences up to 544 μm/s in preterm and 844 μm/s in term infants. The mean differences in RBC velocities at a given measuring time were 524 ± 157 μm/s for term and 364 ± 120 μm/s for preterm infants with 95% confidence interval (CI) from 446 to 603 μm/s for term and 312 to 416 μm/s for preterm infants. Coefficients of variation were 30 ± 7 μm/s and 26 ± 8 μm/s in term, 22 ± 8 μm/s and 19 ± 8 μm/s in preterm infants on d 1 and 5, respectively. In term infants, there was no difference with regard to vessel diameter, density, or RBC velocity between d 1 and 5 (Table 3). Vessel density, diameter, and RBC velocity did not differ between the term and preterm infants. In preterm infants, on d 5 we found no difference in vessel diameter or density, but RBC velocity was significantly higher (Table 3). Vessel diameter and vessel density did not correlate with any of the clinical data such as gestational age, heart rate, or BP. We found, however, a statistically significant negative correlation (Fig. 4) between hematocrit and RBC velocity (r = −0.3731 with a 95% CI −0.5899 to −0.1062, p = 0.006). There was no correlation between incubator temperature and RBC velocity. Leukocytes either rolling along the vessel wall or as gaps in the RBC column could only be observed occasionally.
Inverse correlation of hematocrit with RBC velocity in preterm infants. The significant decrease in hematocrit from d 1 to 5 correlated inversely with the significant increase in mean RBC velocity [Spearman correlation (two-tailed):r2 = −0.4 with 95% CI −0.6 to −0.1 and p = 0.006. Linear fit p = 0.0005].
DISCUSSION
We have shown that microcirculatory parameters of the skin can be measured in absolute values in neonates and even in very preterm infants. OPS imaging may offer new perspectives in clinical monitoring because it permits easy, portable access to a variety of vascular beds without image-enhancing dyes. The small size of the handheld instrument makes measurements possible in the incubator. Because the light source is cold and does not damage or even heat the skin, OPS can be used in extremely preterm infants with gestational age as low as 23–24 wk. CAP-Imaging follows individual pixels and does not allow the measurement of blood flow velocity. Hence, flow motion was not assessed in the current study.
Even though capillary microscopy has been used in adults with microangiopathy for nearly 30 y, there are only a very few publications about its use in neonates (6, 14–16). These studies were restricted to nailfold capillaroscopy in term infants during the first week of life.
Diameters of skin capillaries have not been previously reported in newborns. Our data are in accordance with capillary diameters measured with nailfold capillaroscopy, where values between 6 and 15 μm were found (6). A 0.4–0.5-μm thick endothelial surface coat reduces functional capillary volume. An additional fluid layer of 0.4–0.6 μm appears to be present between flowing RBCs and capillary wall with the thickness of the RBC exclusion zone dependent on RBC velocity (17). With the CYTOSCAN A/R, the diameter is measured as the width of the RBC column present in the vessel. True anatomical vessel diameter therefore could be underestimated (18). In adults, where OPS images have mostly been obtained sublingually, larger vessels are well-visualized and arterioles and venules can be differentiated. In the neonate, vessels larger than 25–30 μm are deeper in the dermis and only small loops can be observed before the vessel disappears into the deeper layer. The mean diameter of the vessels measured in our study was approximately 8 μm and, therefore, at the lower end of vessel size that can be perfused by neonatal RBC. Measurements of deformability and geometry of neonatal erythrocytes indicate that the average neonatal erythrocyte can enter cylindrical tubes with an internal diameter of 3.8 μm and more, whereas the average adult erythrocyte can enter tubes with diameter of 3.4 μm and more (19).
Preterm infants had significantly higher RBC velocities on d 5 of life. RBC velocities inversely correlated with hematocrit and our preterm infants experienced a significant decrease in hematocrit from d 1 to 5, probably due to iatrogenic blood loss. Norman et al. (6) determined capillary blood cell velocity in the nailfold capillaries of term infants at d 2–7 after birth. The overall values reported are similar to our findings, with a range from 40 to 1200 μm/s and a mean of 380 ± 210 μm/s. Similar to our results, they found no correlation between capillary blood cell velocity and skin temperature, MAP, or postnatal age. However, a significant correlation was found between the log capillary blood cell velocity and the skin prick hematocrit. Hematocrit, which is frequently elevated in newborns, seemed to be of major importance for skin capillary perfusion. The investigators suggested that the increased resistance in capillary flow may be due not only to the increase in the number of red cells but also to the larger size of the RBCs in the newborns. In a second study, Norman et al. (15) found an inverse relationship between high hematocrit levels in postnatally polycythemic infants and very low capillary blood cell velocity (110 μm/s). Capillary blood cell velocity increased in a strong nonlinear relationship, with a reduction in hematocrit as a result of an exchange transfusion (210 μm/s; healthy controls 300 μm/s) (16). RBC velocity as reported by us and by Norman et al. (6) does not significantly differ from the values found in nailfold low capillary blood cell velocity of healthy adults (100–500 μm/s). The total neonatal peripheral blood flow has been found to be twice as high in adults (20). Because earlier morphologic descriptions of the neonatal cutaneous microvasculature revealed poor skin vascularization (1–3), the higher peripheral blood flow in newborns is more likely to bypass the superficial skin vessels through deeper vascular beds, which suggests an increased flow resistance in the neonatal skin capillaries.
The vessel density is used as a measure of tissue perfusion. Because only the RBC perfused vessels are counted, it is also an indirect measure of the oxygen delivery. We did not find any difference between the term and preterm infants or within the groups at the two different time points with regard to vessel density. Because we believe that the vessel density is a valuable parameter for the assessment of nutritive flow, we conclude that none of the studied infants had an impairment of microvascular perfusion. None of the studied preterm infants were in shock or hypotensive, yet, even so, two received catecholamines and two cortisone for BP support at the time of measurement. For visual description of microcirculation we used a clinical score as shown in Table 1. None of the infants revealed clinical signs of an impaired microcirculation.
In a preliminary study, De Backer et al. (21) examined sublingual capillary density and blood flow velocity in healthy volunteers and patients with septic and cardiogenic shock. They found a changed perfusion pattern in septic shock with markedly reduced numbers of perfused capillaries, especially of small vessels. They also observed an increased number of capillaries where flow was transient or absent. In patients with cardiogenic shock, capillary density was decreased and RBC conglomerates could be visualized in the venules. These measurements were only semiquantitative by implementing three horizontal and three vertical lines onto the visual field and counting the numbers of vessels with flow that crossed these lines. Schaudig et al. (22) reported a decrease in functional capillary density with a decrease in RBC velocity during cardiopulmonary bypass applying OPS imaging to the sublingual mucosa of adults.
Changes in microcirculation play a crucial role in the development of organ failure, but so far mainly macrocirculatory parameters, such as BP, cardiac output, and whole body oxygen delivery are measured. Capillary refill time is an easy but relatively subjective measurement with an endpoint that is difficult to define and is influenced significantly by environmental factors. OPS imaging may offer new perspectives in clinical monitoring because it allows for easy, portable access to a variety of vascular beds, and this without image enhancement with dyes. In adults, it has been used sublingually and directly on organs during surgery. In contrast, laser Doppler flowmetry gives only a semiquantitative index of superficial tissue perfusion. Because of the relatively high degree of penetration, not only are the papillary capillaries included, but also the arterial and venous vessels of the superficial and middle layers of skin. In addition, the equipment is cumbersome and measurements in infants nursed in incubators difficult.
Time discrete near infrared photoplethysmography might also be a promising technology to assess microcirculatory changes. It entails a more detailed analysis of the signal used in pulse oximetry. We have shown that near infrared photoplethysmography could be used as a semiquantitative method for measuring changes in microcirculation in preterm infants with impaired perfusion after receiving a colloid bolus (23). So far, there is no commercially available probe and no possibility to use the standard pulse oximetry probe.
In conclusion, in premature infants the transdermal application of OPS was noninvasive and provided quantitative data of microvascular diameter and RBC velocity. OPS imaging allows direct observation of RBC rheology in vivo and enables monitoring of the microcirculatory response to therapy, and thus may become a valuable clinical tool. This, however, will require a standardized and automated analysis routine that has been validated as a true measure of tissue perfusion. At present, the calculations have to been done off-line and are rather time-consuming, which limits its current clinical use.
Abbreviations
- BP:
-
blood pressure
- MAP:
-
mean arterial pressure
- OPS:
-
orthogonal polarization spectral
- RBC:
-
red blood cell
References
Perera P, Kurban AK, Ryan TJ 1970 The development of the cutaneous microvascular system in the newborn. Br J Dermatol 82( suppl 5): 86–91
Schwalm H 1934 Die Hautkapillaren bei Neugeborenen. Arch Kinderheilkd 103: 129–137
Mayer K 1921 Observation on the capillaries of the normal infant. Am J Dis Child 22: 381–387
Ryan TJ 1998 Development of the cutaneous circulation. In: Polin RA, Fox WW (eds) Pathophysiology of the Fetus and Neonate. WB Saunders, Philadelphia, 752–761
Beinder E, Trojan A, Bucher HU, Huch A, Huch R 1994 Control of skin blood flow in pre- and full-term infants. Biol Neonate 65: 7–15
Norman M, Herin P, Fagrell B, Zetterström R 1988 Capillary blood cell velocity in full-term infants as determined in skin by videophotometric microscopy. Pediatr Res 23: 585–588
Slaaf DW, Tangelder GJ, Reneman RS, Jäger K, Bollinger A 1987 A versatile incident illuminator for intravital microscopy. Int J Microcirc Clin Exp 4: 391–397
Groner W, Winkelman JW, Harris AG, Ince C, Bouma GJ, Messmer K, Nadeau RG 1999 Orthogonal polarization spectral imaging: a new method for study of the microcirculation. Nat Med 5: 1209–1212
Harris AG, Sinitsina I, Messmer K 2000 Quantitative analysis of orthogonal polarization spectral images validation in the hamster dorsal skinfold chamber. In: Messmer K (ed) Progress in Applied Microcirculation. Karger, Basel, 21–31
Klyscz T, Jünger M, Jung F, Zeintl H 1997 Cap image—a new kind of computer-assisted video image analysis system for dynamic capillary microscopy. Biomed Tech 42: 168–175
Nolte D, Zeintl H, Steinbauer M, Pickelmann S, Messmer K 1995 Functional capillary density: an indicator of tissue perfusion?. Int J Microcirc Clin Exp 15: 244–249
Langer S, Harris AG, Biberthaler P, von Dobschuetz E, Messmer K 2001 Orthogonal polarization spectral imaging as a tool for the assessment of hepatic microcirculation. A validation study. Transplantation 71: 1249–1256
Strozik KS, Pieper CH, Cools F 1998 Capillary refilling time in newborns—optimal pressing time, sites of testing and normal values. Acta Paediatr 87: 310–312
Norman M, Herin P, Fagrell B 1992 An evaluation of skin capillary blood flow determinations in neonates using a computerized videophotometric method. Microvasc Res 43: 276–284
Norman M, Fagrell B, Herin P 1992 Effects of neonatal polycythemia and hemodilution on capillary perfusion. J Pediatr 121: 103–108
Norman M, Fagrell B, Herin P 1993 Skin microcirculation in neonatal polycythaemia and effects of haemodilution. Interaction between haematocrit, vasomotor activity and perfusion. Acta Paediatr 82: 672–677
Vink H, Duling BR 1996 Identification of distinct luminal domains for macromolecules, erythrocytes, and leukocytes within mammalian capillaries. Circ Res 79: 581–589
Harris AG, Sinitsina I, Messmer K 2000 The Cytoscan Model E-II, a new reflectance microscope for intravital microscopy: comparison with the standard fluorescence method. J Vasc Res 37: 469–476
Ruef P, Linderkamp O 1999 Deformability and geometry of neonatal erythrocytes with irregular shapes. Pediatr Res 45: 114–119
Wu PYK, Wong WH, Guerra G, Miranda R, Godoy RR, Preston B, Schoentgen S, Levan NE 1980 Peripheral blood flow in the neonate. I. Changes in total, skin and muscle blood flow with gestational and postnatal age. Pediatr Res 14: 1374–1378
De Backer D, Creteur J, Vincent J-L 2000 Use of orthogonal polarization spectral imaging in intensive care. In: Messmer K (ed) Progress in Applied Microcirculation. Karger, Basel, 104–109
Schaudig S, Schiessler C, Harris AG, Reichenspurner HC, Messmer K, Christ F 2001 Intravital microscopy in humans during and following circulatory arrest for surgery in the ascending aorta. J Vasc Res 38: 514A( abstr)
Genzel-Boroviczeny O, Müller C, Christ F 2000 Assessment of microcirculation in VLBW infants by near infra red and red photoplethysmography. Pediatr Res 47: 399A( abstr)
Acknowledgements
The authors thank Cytometrics, Philadelphia, PA, U.S.A., for providing the instrument.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Genzel-Boroviczény, O., Strötgen, J., Harris, A. et al. Orthogonal Polarization Spectral Imaging (OPS): A Novel Method to Measure the Microcirculation in Term and Preterm Infants Transcutaneously. Pediatr Res 51, 386–391 (2002). https://doi.org/10.1203/00006450-200203000-00019
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/00006450-200203000-00019
This article is cited by
-
Peripheral perfusion index percentiles for healthy newborns by gestational age and sex in China
Scientific Reports (2020)
-
Mechanical microenvironment as a key cellular regulator in the liver
Acta Mechanica Sinica (2019)
-
Flow dynamics analyses of pathophysiological liver lobules using porous media theory
Acta Mechanica Sinica (2017)
-
The vulnerable microcirculation in the critically ill pediatric patient
Critical Care (2016)
-
Microcirculatory mechanisms in postnatal hypotension affecting premature infants
Pediatric Research (2013)