Abstract
In a prospective clinical study, we investigated the inflammatory response in 88 neonatal subjects (43 boys and 45 girls) who underwent major abdominal surgery owing to congenital malformation involving the gastrointestinal tract and compared it with the response in 20 infants (8 boys, 12 girls; mean age, 4 mo) who underwent elective surgery for resolution of an existing temporary stoma. In both groups, plasma levels of endotoxin, IL-6, and C-reactive protein as well as leukocyte counts were determined during and after surgery. Endotoxin was measured by the Limulus amebocyte test, IL-6 by ELISA, and C-reactive protein by nephelometry. Statistical analyses were performed using the Wilcoxon signed-rank test. A significant increase in circulating endotoxin and a leukocyte shift was observed in the infant group only. Postoperatively, IL-6 levels peaked between 2 and 6 h and C-reactive protein after 24 h in the infant group. In contrast, no significant increase in the levels of endotoxin, IL-6, and C-reactive protein in plasma were observed during and after surgery in the neonatal subjects, except those with gastroschisis. Newborns with gastroschisis developed an inflammatory response after surgery that was less pronounced than the response of infants older than 4 mo. The finding that endotoxemia in newborns does not follow surgical trauma is most likely because of the absence of bacterial colonization of the gastrointestinal tract.
Similar content being viewed by others
Main
After surgical trauma the human organism reacts with various cellular and humoral mechanisms, which are summarized as the acute-phase response (1, 2). One major role of this reaction is to minimize organ damage and to trigger repair mechanisms. These events are controlled by a complex cascade of inflammatory mediators that can be measured in the circulation and can serve as clinical markers. Endotoxemia represents an early marker for surgical trauma. Several studies have clearly demonstrated that the level of endotoxin increases not only after major abdominal surgery but also during small invasive procedures like colonoscopy (3–5). After the increase of circulating endotoxin, IL-6 and CRP increase with a time delay of several hours. Both IL-6 and CRP are clinically acknowledged markers of the acute-phase response. In adults, the amount of surgical trauma is reflected by the magnitude of elevation observed in endotoxin, IL-6, and CRP plasma levels (6). In previous investigations we have shown that the level of circulating endotoxin increases during surgical procedures owing to translocation from the GI tract (3–6).
In contrast to infants and adults, newborns have almost no bacterial colonization of the intestinal tract. Several weeks are required for a regular gut flora to be established, and, in the meantime, the newborn bowel is protected by maternal immunoglobulins (7–9). The prospective study reported here aimed to compare the level of endotoxin in plasma and the acute-phase response between newborns and infants undergoing major abdominal surgery. The question of whether endotoxin, IL-6, and CRP may be used as inflammatory markers in newborns undergoing surgery was also addressed.
METHODS
From January 1992 to December 2000, two groups of pediatric patients were enrolled in this prospective study. The first group comprised 88 newborns (43 boys and 45 girls) who underwent abdominal surgery because of congenital malformation involving the GI tract. Twenty-nine (33%) of the babies were premature and 59 (67%) were mature. None of these children had been exposed to steroids. According to our standard procedure in the pediatric surgery division a single-shot antibiotic treatment was given to all patients. Table 1 shows the demographic and clinical data of this patient group. The second study group consisted of 20 infants (8 boys, 12 girls) with a mean age of 4 mo who underwent elective surgery for resolution of an existing temporary stoma. Table 2 shows the demographic and clinical data of this group.
Study protocol.
In both groups, blood was drawn from central venous catheters under sterile conditions. The heparinized blood (10 IU/mL) was then centrifuged at 2000 ×g for 15 min to obtain platelet-free plasma. Plasma was aliquoted and stored at −70°C for up to 3 mo until assayed. All time points of blood sampling were defined in relation to the surgical procedure to obtain comparable values for both patient groups as follows: 1, preoperatively; 2, after exposure of the situs; 3, before wound closure; 4, 2 h postoperatively; 5, 6 h postoperatively; 6, postoperative d 1; 7, postoperative d 2; 8, postoperative d 3; 9, postoperative d 4; 10, postoperative d 5; 11, postoperative d 6; and 12, postoperative d 7. The study was approved by the local ethical committee of the University of Ulm, and the parents of all patients gave informed consent.
Plasma endotoxin measurement.
The levels of endotoxin in plasma were measured by the LAL test (5, 6). The LAL test is a two-step end point colorimetric assay that is performed in microtiter plates (Greiner Co., Nürtingen, Germany). The following solutions were prepared: (A) endotoxin lysate (Pyroquant Co., Walldorf, Germany) solubilized in pyrogen-free water according to the manufacturer's recommendations; (B) pefachrome (Dietzenbach, Germany), a chromogenic substrate at a concentration of 10 μmol in 6.6 mL of pyrogen-free water; (C) 0.2 M NaCl, 0.05 M Tris/HCl (pH 9.0); and (D) 20% acetic acid. In brief, plasma samples were diluted 1:10 with pyrogen-free water and heat inactivated for 10 min at 75°C. Fifty microliters of the pretreated samples was added to 50 μL of solution A and incubated for 30 min at 37°C. Thereafter, 100 μL of solution B diluted with solution C (1:2) was added and incubated for a further 3 min at 37°C. The reaction was then stopped by adding 200 μL of solution D. Changes in the extinction coefficient were measured spectrophotometrically at a wavelength of 405 nm (SLT Co., Salzburg, Austria). The relative units of endotoxin per milliliter (EU/mL) present in the unknown samples were determined by performing a comparison with the standard curve generated by the dilution of EC5-standard (Pyroquant Co., Walldorf, Germany). The lower and upper detection limits were 0.015 EU/mL and 1.5 EU/mL, respectively. The intra- and interassay variation coefficients of 30 determinations were <8%, as routinely determined for low and high endotoxin levels.
Assessment of plasma mediators.
CRP was measured using a Behring nephelometer II (Behring Co., Marburg, Germany), as described previously (5, 6). In brief, polystyrene particles coated with antibodies against CRP were mixed with plasma samples. Agglutination of the mixture was measured by determining the changes in intensity of the scattered light in the nephelometer. The CRP concentration in the unknown samples was then calculated by performing a comparison with the standard curves generated by dilution of a known concentration. Plasma levels of IL-6 were measured by ELISA (Bierman et Co, Bad Nauheim, Germany) according to the manufacturer's recommendation and as described previously (5, 6).
Statistical analysis.
The Mann-Whitney U test was used to determine the statistical significance of the measurements. The Wilcoxon signed-rank test was applied to determine the differences between the AUC of both groups. A p < 0.05 was considered statistically significant. All statistical analyses were performed using the statistical software program SPSS for Windows 6.1 (SPSS Inc., Chicago, IL, U.S.A.).
RESULTS
Plasma endotoxin.
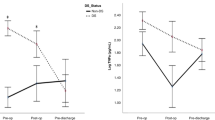
In the infant group, endotoxin levels in plasma increased 1.5-fold (p < 0.05) after exposure of the situs and up to 3.5-fold at the end of the surgical intervention (Fig. 1A). Endotoxin levels remained significantly elevated until the first postoperative sampling and declined to normal values thereafter. In contrast, in the newborn group, no significant increase of endotoxin levels in plasma was observed during and after surgery. The difference between the AUC values of both groups was statistically significant (p < 0.005). Furthermore we found no difference among the endotoxin levels of term and preterm newborns. But there was a significant age-related increase of endotoxin levels in plasma at the time of surgery (p < 0.048).
Plasma levels of endotoxin (A), IL-6 (B) and CRP (C) in 80 newborns, 8 newborns with gastroschisis, and 20 infants who underwent abdominal surgery. Blood was collected at the following times: 1, preoperatively; 2, after exposure of the situs; 3, before wound closure; 4, 2 h postoperatively; 5, 6 h postoperatively; 6, 1 d postoperatively; 7, 2 d postoperatively; 8, 3 d postoperatively; 9, 4 d postoperatively; 10, 5 d postoperatively; 11, 6 d postoperatively; and 12, 7 d postoperatively. The data are presented as median and AUC.
Inflammatory mediators.
Inflammatory mediators significantly increased in a time-dependent manner in the infant group, whereas no significant change was observed in the newborns, except in those with gastroschisis (Fig. 1, B and C). IL-6 increased markedly at the end of the operation and remained elevated until postoperative d 1 in the newborns with gastroschisis and in infants; however, the increase was significantly lower (AUC, p < 0.05) in newborns with gastroschisis compared with the infants.
The postoperative course of CRP levels in plasma differed between the two patient groups. Newborns with gastroschisis demonstrated increasing CRP levels, reaching a maximum at postoperative d 3. In the remaining newborns, only small increases were observed in the CRP levels, with the maximum increase (13 mg/L) being reached at postoperative d 3 and 4. In contrast, the infants, who were older and had a smaller amount of surgical trauma (replacement of artificial stoma), demonstrated increases in CRP levels that were up to 10 times higher (maximal value, 97 mg/L), peaking at 24 h after surgery. In all cases, the CRP levels decreased to normal on postoperative d 5. Similar to the finding for IL-6, the AUC value calculated for CRP was significantly higher in the infant group compared with the newborn group (p < 0.005).
No significant leukocyte count elevations were observed in newborns at postoperative d 1, whereas a significant increase in the total number of leukocytes appeared in the infant group (Fig. 2). In addition, the relative amount (percentage of total leukocytes) of mature/immature neutrophils changed from 28%/8% preoperatively to 24%/34% at postoperative d 1 in the infant group (p < 0.05), whereas no significant difference was observed among the newborns (42%/10% preoperatively versus 44%/14% at postoperative d 1).
Clinical outcome.
The clinical data of all patients in the newborn group are detailed in Table 1. Operations had to be repeated in 10 newborns for indications including ileus, gastroesophageal reflux, anastomotic stenosis, abscess, and insufficient drainage of saliva. Seven newborns had a fatal outcome. Reasons for death included cardiac arrest, pulmonary insufficiency, pulmonary bleeding, liver failure, and severe malformation (Edwards syndrome). Table 2 shows the demographic and clinical data of all patients in the infant group. In this group, no patient died and only one patient was reoperated on because of ileus.
DISCUSSION
To the best of our knowledge, this is the first study comparing the endotoxin levels and inflammatory mediators between newborns and infants during and after abdominal surgery. The results indicate that endotoxin, IL-6, and CRP levels in plasma did not increase in the newborn subjects in general, whereas newborns with gastroschisis and small infants demonstrated significant increases. It is well known that newborns have virtually no bacterial colonization of the intestinal tract and several weeks are required for a regular gut flora to be established (7–9). Furthermore their immune systems are not mature. Thus, postoperative infections are difficult to detect in these patients because the classic inflammatory variables are not fully characterized (10–14). This is one reason why many infections in newborns are not diagnosed and treated early enough or sufficiently.
Elevations of the leukocyte count and inflammatory mediators such as CRP and IL-6 are generally accepted as clinical markers of infection complicating the postoperative course. This is mainly based on clinical experience with adults, who respond to surgical trauma first with a significant increase of circulating endotoxin followed by a cascade of inflammatory mediators such as IL-6 and CRP. Our results differ from those of other authors, who found increased cytokine levels and acute-phase reaction in neonates after abdominal surgery (15–17). Although the inflammatory response in newborns is still not fully characterized, our data clearly demonstrate that newborns respond to surgical trauma only with a mild increase of leukocytes and no increase of endotoxin, IL-6, and CRP levels in plasma. Although neutrophils in newborns are deficient in bactericidal/permeability-increasing protein (18), the lack of inflammatory cytokines in these patients is most likely because of the absence of endotoxin. Studies in animals have shown that newborn mice differ from adult mice in chemokine and cytokine expression to ozone, but not to endotoxin (19). With respect to the diagnostic value of measuring inflammatory markers, our data indicate that the levels of endotoxin and acute-phase proteins IL-6 and CRP in plasma do not adequately reflect the acute-phase response in newborns. In contrast, infants older than 4 mo react like adults and demonstrate a strong increase in inflammation variables after surgery. It should be noted that the surgical procedures performed on these subjects were less invasive than those performed on patients in the neonatal group. This suggests that the amount of available endotoxin, which was higher in the infant group, may be more important in triggering the acute-phase reaction than the surgical trauma itself.
The major source of circulating endotoxin during abdominal surgery is the GI tract, which is influenced by the surgical trauma; this trauma leads to the translocation of endotoxin into the circulatory system and subsequent induction of several synthesized acute-phase proteins (20). In newborn animals, early development of shock after stomach rupture could be attributed to endotoxin translocation and endotoxemia (21). In our study, significantly elevated endotoxin levels in plasma were detected in infants and, although less pronounced, in newborns with gastroschisis.
The latter group exhibited mild endotoxemia. This could probably be explained by bacterial contamination of the exterior GI tract. The increase of endotoxin levels in the plasma of newborns with gastroschisis can also be explained by the fact that the peritoneal cavity is open at delivery, thereby allowing the peritoneum to absorb endotoxins from outside. Another explanation could be the fact that after surgery the bowels are compromised in a closed abdomen, which could lead to a decrease of intestinal blood circulation. A decrease of intestinal blood circulation and a decrease of bowel movements with stasis of the intestinal fluids could increase bacterial colonization and, after a disturbance of the gut barrier, lead to endotoxin translocation.
The severe reflux that occurs on the first postoperative days may contribute further to rapid bacterial colonization of the stomach and upper GI tract. Infants older than 4 mo already have physiologic bacterial colonization of the GI tract; therefore, they can develop both endotoxemia and an acute-phase response. Conversely, because newborns lack bacterial colonization of the GI tract, no endotoxin translocation should occur, as reflected by our findings. In a recent study investigating 68 preterm infants whose gestational age ranged between 27 and 33 wk, serum endotoxin was detected in 28 cases by means of a conventional chromogenic Limulus test (22). We found no difference among the endotoxin levels of term and preterm newborns. Because most newborns in our study underwent abdominal surgery immediately after cesarian section (Table 1), interference with immunoglobulins by breast-feeding can be excluded as a reason for the absence of endotoxemia. Our results also differ from those of Scheifele et al. (23) who detected endotoxemia in 33% of blood culture-negative neonates with suspected sepsis. One explanation for this discrepancy could be that a significant proportion of blood cultures in the study of Scheifele et al. (23) were falsely negative because blood cultures are very often negative in newborns owing to the minimal volumes of blood routinely cultivated at this age. It has not been shown that early onset bacteremia as examined by these authors results from intestinal colonization. It may be rather related to exogenous sources of Gram-negative aerobic bacteria such as the mother's genital tract or contaminated i.v. devices.
In conclusion, during abdominal surgery newborns exhibit neither endotoxemia nor subsequent mediator release, which is in sharp contrast to the response of infants older than 4 mo. Our findings support the view that bacterial colonization of the GI tract is necessary to trigger the acute-phase response.
Abbreviations
- CRP:
-
C-reactive protein
- GI tract:
-
gastrointestinal tract
- LAL test:
-
Limulus amebocyte test
- EU:
-
endotoxin units
- AUC:
-
area under the curve
References
Dowton SB, Colten HR 1988 Acute phase reactants in inflammation and infection. Semin Hematol 25: 84–90
Fasching G, Kurz R, Wendler M 1988 Effect of surgery on inflammation parameters. Z Kinderchir 43: 3–5
Boelke E, Storck M, Buttenschoen K, Berger D, Hannekum A 2000 Endotoxemia and mediator release during cardiac surgery. Angiology 51: 743–749
Berger D, Bolke E, Huegel H, Seidelmann M, Hannekum A, Beger HG 1995 New aspects concerning the regulation of the post-operative acute phase reaction during cardiac surgery. Clin Chim Acta 239: 121–130
Bolke E, Jehle PM, Storck M, Nothnagel B, Stanescu A, Orth K 2001 Endotoxin release and endotoxin neutralizing capacity during colonoscopy. Clin Chim Acta 303: 49–53
Boelke E, Jehle PM, Nothnagel B, Storck M, Orth K 2000 A prospective randomized study on endotoxemia, mediator release and morbidity in conventional, compared with laparoscopic cholecystectomy. Minim Invasive Ther Allied Technol 9: 387–392
Eibl MM, Wolf HM, Furnkranz H, Rosenkranz A 1990 Prophylaxis of necrotizing enterocolitis by oral IgA-IgG: review of a clinical study in low birth weight infants and discussion of pathogenic role in infection. J Clin Immunol 10( 6 suppl): 72–77
Claud EC, Walker WA 2001 Hypothesis: inappropriate colonization of the premature intestine can cause neonatal necrotizing enterocolitis. FASEB J 15: 1398–1402
Harmsen HJ, Wildeboer-Veloo AC, Raangs GC, Wagendorp AA, Klijn N, Bindels JG, Welling GW 2000 Analysis of intestinal flora development in breast-fed and formula-fed infants by using molecular identification and detection methods. J Pediatr Gastroenterol Nutr 1: 61–67
Pizzini C, Mussap M, Plebani M, Fanos V 2000 C-reactive protein and serum amyloid A protein in neonatal infections. Scand J Infect Dis 32: 229–235
Tomsic Matic M, Derganc M, Wraber B, Primozic J 2000 Interleukin-6 (IL-6) and soluble receptors for interleukin-2 (sIL-2R) in the diagnosis of early severe infection in the critically ill newborns. Pflugers Arch 440( 5 suppl): R75–R77
Delmas J, Monneret G, Lapillonne A, Basson E, Isaac C, Bienvenu F, Putet G, Bienvenu J 2000 Procalcitonin and C-reactive protein kinetics in neonates with group B streptococcus infection. Ann Biol Clin 58: 208–211
Hansen AB, Verder H, Staun-Olsen P 2000 Soluble intercellular adhesion molecule and C-reactive protein as early markers of infection in newborns. J Perinat Med 28: 97–103
Gomez R, Romero R, Ghezzi F, Yoon BH, Mazor M, Berry SM 1998 The fetal inflammatory response syndrome. Am J Obstet Gynecol 179: 194–202
Ito H, Kishikawa T, Yamakawa Y, Toda T, Tsunooka H, Masaoka A, Ando S 1983 Serum acute phase reactants in pediatric patients especially in neonates. Jpn J Surg 13: 506–511
Grant HW, Chuturgoon AA, Kenoyer DG, Doorasamy T 1997 The adaptive immune response to major surgery in the neonate. Pediatric Surg Int 12: 490–493
Tsang TM, Tam PK 1984 Cytokine response of neonates to surgery. J Pediatr Surg 29: 794–797
Levy O, Martin S, Eichenwald E, Ganz T, Valore E, Carroll SF, Lee K, Goldmann D, Thorne GM 1999 Impaired innate immunity in the newborn: newborn neutrophils are deficient in bactericidal/permeability-increasing protein. Pediatrics 104: 1327–1333
Johnston CJ, Oberdorster G, Gelein R, Finkelstein JN 2000 Newborn mice differ from adult mice in chemokine and cytokine expression to ozone, but not to endotoxin. Inhal Toxicol 12: 205–224
Boelke E, Jehle PM, Beier A, Wiedeck H, Steinbach G, Storck M, Orth K 2001 Inflammatory response during abdominal and thyroid surgery: a prospective clinical trial on mediator release. Shock 16: 334–339
Goto M, Yoshioka T, Hase T, Tani T, Zeller WP 1999 A mechanism for shock following stomach rupture in the newborn. Pediatr Int 41: 374–378
Okumura A, Hayakawa F, Kato T, Kuno K, Watanabe K 1999 Correlation between the serum level of endotoxin and periventricular leukomalacia in preterm infants. Brain Dev 21: 378–381
Scheifele DW, Melton P, Whitchelo V 1981 Evaluation of the limulus test for endotoxemia in neonates with suspected sepsis. J Pediatr 98: 899–903
Acknowledgements
The authors thank Prof. Dr. D. Berger, Dr. B. Poch, and Dr. D. Birk for their contributions in the operating theater and M. Seidelmann for her excellent technical assistance in the laboratory. Furthermore, Dr. T. Weber is thanked for helpful discussions.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bölke, E., Jehle, P., Trautmann, M. et al. Different Acute-Phase Response in Newborns and Infants Undergoing Surgery. Pediatr Res 51, 333–338 (2002). https://doi.org/10.1203/00006450-200203000-00012
Issue Date:
DOI: https://doi.org/10.1203/00006450-200203000-00012
This article is cited by
-
Noninfectious influencers of early-onset sepsis biomarkers
Pediatric Research (2022)
-
Procalcitonin versus C-reactive protein: review of kinetics and performance for diagnosis of neonatal sepsis
Journal of Perinatology (2019)
-
Preventively enteral application of immunoglobulin enriched colostrums milk can modulate postoperative inflammatory response
European Journal of Medical Research (2013)
-
Lipopolysaccharide-binding protein, lipopolysaccharide, and soluble CD14 in sepsis of critically ill neonates and children
Intensive Care Medicine (2007)
-
Different Proinflammatory Cytokine Serum Pattern in Neonate Patients Undergoing Open Heart Surgery. Relevance of IL-8
Journal of Clinical Immunology (2005)