Abstract
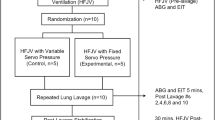
Perfluorocarbons have been shown to reduce the inflammatory process generated by alveolar macrophages in vitro. The aim of this study was to evaluate the impact of different ventilator modalities such as partial liquid ventilation (PLV), conventional ventilation (CV), and high-frequency oscillatory ventilation (HFOV) on the release of inflammatory mediators in vivo. Acute lung injury was induced in 30 male piglets by repeated saline lavage (arterial oxygen tension, <60 mm Hg; fraction of inspired oxygen, 1.0). Thereafter, animals were randomly assigned to one of five groups of six animals each:1) 24 h of CV;2) 24 h of CV plus surfactant therapy (S+CV);3) 24 h of HFOV plus surfactant therapy (S+HFOV);4) 1 h of PLV followed by 23 h of CV (PLV); and 5) 24 h of CV without previous lung injury (control group). Piglets randomized to S+CV or S+HFOV received natural surfactant (100 mg/kg). PLV with FC-77 was started in an initial dose of 30 mL/kg over 30 min followed by 0.5 mL·kg−1·min−1 for another 30 min. After 1 h of PLV the animals were conventionally ventilated for 23 h. Before acute lung injury and after 24 h the number of inflammatory cells and the levels of IL-6, leukotriene B4, and tumor necrosis factor-α were measured in the bronchoalveolar lavage fluid. Additionally, the oxygenation index and the histopathologic damage were evaluated. Before acute lung injury, the number of inflammatory cells and the levels of mediators in bronchoalveolar lavage fluid were not different among the groups. After 24 h, the number of granulocytes in the PLV group was as low as in the control group. leukotriene B4 and IL-6 levels were found to be elevated in all groups except the control group (p < 0.01). The release of leukotriene B4 and IL-6 was lowest in the PLV group when compared with S+HFOV, S+CV, or CV (p < 0.05). No differences among the groups were detected for tumor necrosis factor-α. Although the concentrations of leukotriene B4 and IL-6 after PLV were lowest in the PLV group, histopathologic evidence of damage and the oxygenation index in the PLV group did not differ from that found in the S+CV or S+HFOV groups. In conclusion, PLV with perfluorocarbons may protect the lung from acute pulmonary inflammation more effectively than CV or HFOV does.
Similar content being viewed by others
Main
Mechanical ventilation of the S-deficient lung may cause ALI in children and adults (1). Despite the widespread use of S, preferentially extremely premature infants are at high risk to develop chronic lung disease as result of the ALI (2, 3). Although the pathogenesis of chronic lung disease is very complex, pulmonary inflammation seems to play a major role in the development of this disease (4, 5). The severity of the ALI and the subsequent process of pulmonary inflammation can be modified by improved ventilation strategies.
In HFOV, small tidal volumes are oscillated around a relatively high, fixed MAP, which keeps the alveolar spaces of the lungs open. Large pressure or volume excursions are avoided, thereby minimizing alveolar collapse and reexpansion of the lungs. In several animal studies of respiratory distress syndrome, HFOV improved the oxygenation of the animals and reduced the inflammatory response caused by lung injury compared with CV (6–8). The results of different prospective human trials regarding pulmonary inflammation and the development of chronic lung disease, however, are contradictory (9–13).
Liquid ventilation with PFCs is an alternative technique that has been shown to improve gas exchange and lung function and minimizes histopathologic changes in animal models of S deficiency (14–16). PFCs, with their low surface tension with air and low interfacial tension with lung liquid, improve pulmonary compliance and prevent complete alveolar collapse. Thus, ventilation-perfusion matching is optimized, resulting in an improved oxygenation. Different in vitro studies demonstrated that PFCs reduce free radical release and attenuate oxidative damage to lung tissue (17, 18). Furthermore, PFCs protect lung epithelial cells from neutrophil-mediated injury and decrease cytokine production by human alveolar macrophages (19, 20).
The aim of this study was to compare the effect of PLV with other ventilation strategies with respect to the release of inflammatory cells and mediators from the lung in a prolonged animal model of S deficiency. To assess lung inflammation in vivo, the number of inflammatory cells in the BAL such as neutrophil granulocytes, lymphocytes, and macrophages as well as inflammatory mediators such as TNF-α, IL-6, and LTB4 were used as markers of the inflammatory response. We hypothesized that proinflammatory mediators are liberated in decreased amounts in PLV with PFC when compared with other ventilator strategies such as CV or HFOV.
METHODS
Animal preparation.
All procedures in this protocol were approved by the Tierschutzkommission, Bezirksregierung Köln, Germany. The experiments were performed according to the rules of the Deutsche Tierschutzgesetz (AZ 23.203.2-AC 40, 3/97) and to the National Institutes of Health guidelines for the use of laboratory animals.
During the 24-h study course, 30 pathogen-free newborn male piglets [1–3 d old; mean weight, 1.95 kg (range, 1.5–2.5 kg)] were anesthetized, initially with halothane in oxygen given by face mask. After insertion of an i.v. catheter in an auricular vein, i.v. anesthesia was begun with ketamine (2 mg/kg) and midazolam (0.2 mg/kg). The animals were paralyzed with vecuronium (0.2 mg/kg) and then intubated with an endotracheal tube (Vygon 4 or 4.5 mm with a surfactant side lumen). Artificial ventilation was delivered by a time-cycled, pressure-limited, continuous-flow ventilator (Stephan HF 300, Gackenbach, Germany). The animals were ventilated with a continuous flow of 6 L/min, a PIP of 16 cm H2O, a PEEP of 2 cm H2O, and a respirator rate of 30 cycles per minute. Proximal airway pressure was continuously monitored by a pressure transducer at the endotracheal tube connector. Catheters were placed in an internal carotid artery and external jugular vein to monitor arterial blood gases and intravascular pressures. For constant infusion Ringer's with 5% glucose solution (5 mL·kg−1·h−1) was provided. The piglets continuously received midazolam (1 mg·kg−1·h−1) and ketamine (2 mg·kg−1·h−1) for sedation and analgesia as well as vecuronium (0.6 mg·kg−1·h−1) for relaxation. The piglets were maintained supine with the head elevated 20° throughout the study, and the body temperature was maintained within 37.0–39.0°C.
Acute lung injury.
After baseline measurements of hemodynamics (heart rate, mean arterial pressure, and central venous pressure) and arterial blood gases, respiratory failure was induced by repeated lung lavage with saline (21). Aliquot portions of 30 mL/kg warmed saline were instilled into the lungs via a side lumen of the endotracheal tube. The lavage was repeated at 10-min intervals, approximately 30 lavages were performed in each animal, and the amount of saline was approximately 1800 mL. The lavage procedure was performed at the following ventilator settings: PIP, 20 cm H2O; PEEP, 4 cm H2O; frequency, 30 cycles per minute; inspiratory time, 0.6 s; and Fio2 = 1.0. Pao2 values < 60 torr (8.0 kPa) had to be sustained on two consecutive measurements over 30 min while the animals were on the same ventilator settings. Additionally, chest radiographs had to show an increase in radiopacity.
Treatment protocol.
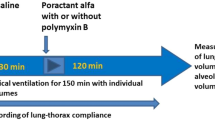
After induction of respiratory failure the animals were allocated to one of the five treatment groups:1) 24 h of CV;2) application of S followed by 24 h of CV (S+CV);3) S followed by 24 h of HFOV (S+HFOV);4) 1 h of PLV followed by 23 h of CV (PLV); and 5) 24 h of CV without previous induction of lung injury, serving as control group (controls).
In the PLV group preoxygenated and 38°C warmed PFC liquid (FC-77 perfluorocarbon liquid, 3M Company, Neuss, Germany) in an amount of 30 mL/kg was slowly infused via the side lumen of the endotracheal tube for 30 min. During this filling phase, blood gases were obtained every 10 min to adapt closely the ventilatory settings. The FC-77 application was then continued for a further 30 min with a dose of approximately 30 mL·kg−1·h−1. To ensure a complete filling of the lungs, the endotracheal tube meniscus was checked. After these 60 min the application of FC-77 was interrupted, and the PFC remained in the lungs. The animals of the PLV group were conventionally ventilated for 23 h until the end of the study. Piglets randomized to receive S treatment were given a single dose of S (100 mg/kg Alveofact, Boehringer Ingelheim, Ingelheim, Germany) via the side lumen of the endotracheal tube and they were ventilated for 24 h either by CV or HFOV. The S+HFOV group received high-frequency oscillation delivered by a piston pump generator (Stephan SHF 3000, Gackenbach, Germany). MAP and peak-to-peak pressure were monitored by a pressure transducer connected with the endotracheal tube. To achieve an optimal lung inflation, MAP was set initially 3–4 cm H2O higher than during CV. When Fio2 had been lowered to 0.4, MAP was allowed to be reduced. To ensure optimal lung volume a chest radiograph was obtained every 6 h. Oscillatory frequency was maintained at 15 Hz. The amplitude was altered as necessary to keep Paco2 between 35 (4.7 kPa) and 50 mm Hg (6.7 kPa).
Blood gases were kept within the following ranges: pH from 7.30 and 7.45, Paco2 from 35 (4.7 kPa) to 50 mm Hg (6.7 kPa), and Pao2 from 50 (6.7 kPa) to 80 mm Hg (10.7 kPa) (ABL 500, Radiometer, Copenhagen, Denmark). Arterial O2 saturation was continuously monitored using pulse oximetry (OxyShuttle, Critikon, Anaheim, CA, U.S.A.). Arterial blood gases were regularly obtained, and arterial blood gases as well as hemodynamic measurements (heart rate, mean arterial blood pressure, central venous pressure) were recorded at baseline CV, after induction of respiratory insufficiency and 30 min later, and at least at 1, 6, 12, 18, and 24 h after initiation of the specific ventilation strategy. To compare the gas exchange among the groups the OI was calculated as MAP (cm H2O) × Fio2 × 100 / Pao2 (mm Hg).
Inflammatory cells in tracheal aspirate.
BAL samples were centrifuged at 800 rpm for 10 min. The supernatant was removed, and a thin film of the cells was mounted on a glass slide and stained with Maywald-Green-Giemsa. Finally, inflammatory cells in BAL were counted in five randomized fields (area, 10.000 μm2), and mean values were calculated for each investigated animal group.
Measurements of inflammatory mediators.
BAL was performed before induction of lung injury by repeated saline lavage and after the 24-h study period. Tracheal aspirate samples were collected using four aliquots of 1.0 mL of saline. Each aliquot was instilled directly down the endotracheal tube via the side lumen, followed by tracheal suction using a standard suction catheter. The catheter was then washed with 1 mL of saline. The specimens obtained were collected in a mucus trap and centrifuged at 3000 ×g for 10 min, and the supernatant was stored at −80°C for later analysis.
Concentrations of LTB4 were measured by RIA. The RIA was performed according to the supplier's instructions (Amersham, Braunschweig, Germany). LTB4 was extracted from the aspirate and separated from other lipids before the assay.
Concentrations of IL-6 and TNF-α were measured by porcine-specific ELISAs (Biozol, Hamburg, Germany), and the analysis was performed according to the supplier‘s instructions.
To compare ELF concentrations of different inflammatory mediators, a direct estimate was made using urea, according to the following formula: ELF volume (mL) = ([urea]BAL / [urea]Plasma) × VolBAL(22). The concentration, e.g. of IL-6 in ELF, was then calculated by the following equation: [IL-6] × VolBAL / ELF (mL) = [IL-6]ELF(22). The ELF concentration of all analyses was calculated (e.g. [IL-6]ELF), as were the ratios of LTB4 and TNF-α.
Histopathology.
Histopathologic analysis was performed on lung tissue obtained after the 24-h study period. Animals that had survived the 24-h study period were killed with an overdose of pentobarbital. Thereafter, the trachea and lungs were immediately removed and inflated with buffered 10% formalin at a pressure of 30 cc H2O for 30 min and finally put in a buffered 10% formalin bath for another 24 h.
Slides from the anterior upper and posterior lower lobes from each side were stained with hematoxylin and eosin and examined by a pathologist blinded with respect to the treatment groups. A four-point, semiquantitative severity-based scoring system was used, grading the pathologic findings as negative = 0, slight = 1, moderate = 2, and severe = 3. Four main characteristics based on 16 individual characteristics were evaluated: atelectasis, edema (based on septal edema, interstitial edema, lymphangiectasis, intraalveolar exudate), inflammation (based on alveolar neutrophil infiltration, interstitial neutrophil infiltration, interstitial lymphocyte infiltration, granulocyte sticking), and various (based on alveolar hemorrhage, hyaline membrane formation, congestive hyperemia, fibrin deposition, thrombocytic aggregation, desquamation of bronchial and bronchiolar epithelium). The results of each variable obtained from all animals in each investigated group were summarized. The sum of all 16 variables was then divided by the number of animals in each group, resulting in the total lung injury score.
Quantitative morphometric measurements were performed using a confocal laser scan microscope (CLSM; Zeiss, Jena, Germany) and an adjusted morphometry system (Quantimed 500, Leica, Wetzlar, Germany). The width of the alveolar wall was measured in randomly selected sampled fields. One hundred random fields in each lung section (anterior upper lobe and posterior lower lobe of both sides) were determined.
Statistical analysis.
Kruskal-Wallis test and the Mann-Whitney U test for intergroup comparisons were performed to evaluate statistical differences using Statistical Package for Social Sciences (SPSS, Chicago, IL, U.S.A.) software. Adjustment for multiple comparisons (Bonferroni) was performed. Intragroup differences were evaluated by the Wilcoxon rank test for dependent groups. Statistical significance was accepted at p < 0.05. Data are presented as mean and SD.
RESULTS
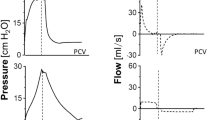
The treatment groups were not different with respect to age and weight. Gas exchange values and hemodynamics did not differ among the groups before lung injury. After saline lavage, all animals except the control group developed severe respiratory failure compared with baseline values (Fig. 1; p < 0.001). In the CV group three animals died because of respiratory failure, and in the PLV group one piglet died after 12 h owing to a pneumothorax. In the other groups none of the animals died before 24 h of ventilation.
Gas exchange.
Within 1 h after S application or the initiation of liquid ventilation, the oxygenation improved significantly in the groups S+CV, S+HFOV, and PLV (p < 0.05), whereas the OI remained high in the CV group (Fig. 1). As half of the animals in the CV group died even before the end of the study, these results are not integrated in the statistical analysis. The oxygenation was better in the S-treated animals, either with S+CV or S+HFOV, when compared with the PLV group (p < 0.05). In the control group of healthy piglets gas exchange was without any problems throughout the 24-h period to maintain normoventilation, and the OI was significantly better at 1, 6, 12, and 24 h when compared with the treatment groups (p < 0.05).
Inflammatory cells in BAL.
The number of neutrophil granulocytes, lymphocytes, and macrophages in the different groups before the induction of ALI and after 24 h of specific ventilation are presented in Table 1. In contrast to the other groups, the amount of granulocytes did not increase during the 24-h course in the PLV group and tended to be as low as in the control group.
Inflammatory mediators.
Before lung lavage the levels of the different inflammatory mediators were low and similar in all groups. With the exception of the control group, after the 24-h course the release of IL-6 and LTB4 was increased independently of the mode of ventilation (p < 0.05). Only TNF-α was not elevated above baseline levels. IL-6 and LTB4 levels were significantly lower in the PLV group when compared with the other treatment groups (Fig. 2; PLV versus S+CV, p < 0.01; PLV versus S+HFOV, p < 0.05). The highest values for TNF-α and LTB4 were found in the CV group without prior S therapy. Because the analysis was from only three animals, these data are not integrated in the statistical analysis.
Inflammatory mediator concentrations in the BAL before ALI and after the 24-h ventilatory course. Results are presented as mean and SD. IL-6: PLV vs S+CV, p < 0.01; PLV vs S+HFOV, p < 0.05; PLV vs Controls, p < 0.05. LTB4: PLV vs S+CV, p < 0.01; PLV vs S+HFOV, p < 0.01; PLV vs Controls, NS. TNF-α: all intergroup comparisons without statistical significance.
Histology and morphometry.
The best histopathologic outcome was observed in the control group without previous lung injury (p < 0.05;Table 2). In all other groups, multiple indices of an ALI such as pulmonary edema and inflammation as well as atelectasis were noted without statistically significant differences among the groups. Representative microscopic photographs demonstrate the histologic patterns of the investigated groups (Fig. 3).
Representative histologic specimens indicating an almost unimpaired lung tissue in the control group without lung lavage (A), whereas CV with lung damage in the presented model demonstrates a picture of acute lung failure, with intraalveolar and interstitial edema, accumulation of inflammatory cells, and the formation of hyaline membranes comparable to states of acute lung failure in neonates (B). In contrast, CV+S (C), S+HFOV (D), and PLV (E) revealed a decreased level of lung alterations compared with CV (B), but again in all groups signs of edema and inflammation could be detected. However, the distribution pattern of these lesions was inhomogeneous in the PLV group (F) (all hematoxylin and eosin, ×400).
Morphometric analysis revealed a tendency of lower mean linear intercept in the lower lung lobes of the PLV group when compared with the other groups (Table 3). No obvious differences were found regarding the upper lung lobes.
DISCUSSION
This study compared the effect of different ventilation modes on the release of pulmonary inflammatory cells and proinflammatory mediators in BAL of newborn pigs. We showed that PLV reduces the inflammatory response from S-deficient lung when compared with CV (with and without prior S treatment) or with HFOV. These data are the first to demonstrate that antiinflammatory properties of PLV may persist even several hours after termination of PLV. They are consistent with previous findings that injured lungs treated with PLV have less evidence of inflammatory infiltrates and tissue damage when compared with gas-ventilated animals (14, 15, 23). The precise mechanism by which PLV attenuates lung injury is not yet fully understood. Several explanations are discussed.
The recruitment of collapsed alveoli by PLV with PFC results in more homogeneous alveolar inflation and a better preservation of the lung structure (24, 25). This may also explain why the proinflammatory mediator levels were lower in the HFOV group than in the CV group as HFOV by itself targets homogeneous alveolar recruitment. Conversely, ventilation strategies which permit inhomogeneous inflation result in pronounced atelectasis, require high inflation pressures with partial overdistension of the lung, and lead to progressive structural injury with pulmonary inflammation (1, 26).
As PFCs are immiscible with other substances and owing to their relatively high specific weight, inflammatory debris will be separated on the liquid column. Liquid ventilation with PFCs may thereby facilitate the removal of inflammatory debris (27).
Finally, there seems to be a direct protective inflammatory effect of PFCs in the alveolus. Smith et al. (17) and Steinhorn et al. (28) demonstrated that the oxidative damage is reduced during PLV with PFCs. Rotta and Steinhorn (30) and Colton et al. (29) observed a reduction in pulmonary neutrophil accumulation in animal experiments. Analogous to their results, we found a reduced amount of granulocytes in the tracheal aspirate fluid of our liquid-ventilated animals when compared with the other treatment groups. Rotta and Steinhorn (30) found a lower myeloperoxidase activity from lung extracts of PLV and HFOV animals than that of CV animals.
Furthermore, our results support recent in vitro observations suggesting PLV might decrease inflammatory cytokine production by human alveolar macrophages. Alveolar macrophages are the major source of proinflammatory cytokines involved in the pathogenesis of ALI (18, 30, 31). Tremblay et al. (32) showed that injurious ventilator strategies may increase inflammatory cytokines within the lung. There are preliminary results that the release of inflammatory mediators such as IL-1 and IL-6 during ongoing PLV is also reduced in humans (33). The present study demonstrates that even a short, 1-h period of PLV has sustained effect on the release of different proinflammatory mediators. This effect was obvious, although the ventilation variables and the histomorphometric outcome after 1 h of PLV were not better than the measurements under S+HFOV or S+CV. There is a discrepancy between the evident histopathologic signs of pulmonary inflammation after short-term PLV and the low levels of inflammatory mediators in the BAL. This may further support the thesis of direct antiinflammatory effects of PFCs, which may suppress the release of inflammatory mediators from granulocytes or macrophages (19). The mechanism by which this release of mediators from the inflammatory cells is altered is unknown, and the immunomodulatory properties of PFCs need further investigations.
One may speculate that a prolonged duration of PLV of more than 1 h will result in even less release of proinflammatory mediators as the gas exchange and particularly the histopathologic outcome is obviously better if PLV is performed for 24 h (34). However, we did not investigate the mediator levels after 24 h of PLV because we were concerned about a possible dilution of the inflammatory mediators caused by the remaining PFC liquid in the lung. In our study protocol with 1 h of PLV, most of the applied PFC volume, if not all, was evaporated during the following 23 h because of the high vapor pressure of FC-77 (85 mm Hg). To avoid the principal risk that the markers are differentially diluted by the BAL we estimated the volume of the ELF using urea as a marker of dilution, which has been shown to be an appropriate method in small-volume lavage (22, 35).
The pattern of TNF-α levels in BAL in our study was different from the results with LTB4 and IL-6. However, these findings are in accordance with previously published reports. Kawamae et al. (36) did not observe significant differences in tracheal fluid TNF-α concentrations comparing CV with PLV. Verbrugge et al. (37) could not detect elevated TNF-α levels as result of mechanical ventilation compared with those of spontaneously breathing controls, and Bagchi et al. (38) did not find elevated TNF-α concentrations in lung lavage of premature infants but did note increased IL-6 levels. Thus, TNF-α does not seem to be the ideal inflammatory factor to reflect the process of pulmonary inflammation. LB4 and IL-6, in contrast, may adequately reflect the inflammatory pulmonary process. LTB4 is involved in the pathogenesis of BPD in neonates as it is one of the most potent agents known for influencing neutrophil migration and adhesion to endothelial cell surfaces. LTB4 has been detected in several studies in BAL from infants with BPD (39, 40). IL-6, as a proinflammatory cytokine that is prominent in the early stages of the inflammatory process, has been shown to be increased in patients with BPD and adult respiratory distress syndrome (38, 41).
In conclusion, even a short-term period of PLV with FC-77 followed by 23 h of CV led to a significantly decreased release of proinflammatory mediators when compared with CV or HFOV. The antiinflammatory properties of PFCs may play a major role in the prevention of ventilator-induced pulmonary inflammation.
Abbreviations
- ALI:
-
acute lung injury
- BAL:
-
bronchoalveolar lavage
- BPD:
-
bronchopulmonary dysplasia
- CV:
-
conventional ventilation
- ELF:
-
epithelial lining fluid
- Fio2:
-
fraction of inspired oxygen
- HFOV:
-
high-frequency oscillatory ventilation
- LTB4:
-
leukotriene B4
- MAP:
-
mean airway pressure
- OI:
-
oxygenation index
- Paco2:
-
partial pressure of arterial carbon dioxide
- Pao2:
-
partial pressure of arterial oxygen
- PEEP:
-
positive end-expiratory pressure
- PFC:
-
perfluorocarbon
- PIP:
-
peak inflation pressure
- PLV:
-
partial liquid ventilation
- S:
-
surfactant
- TNF-α:
-
tumor necrosis factor-α
References
Dreyfuss D, Saumon G 1998 Ventilator-induced lung injury: lessons from experimental studies. Am J Respir Crit Care Med 157: 294–323
Parker RA, Lindstrom DP, Cotton RB 1992 Improved survival accounts for most, but not all, of the increase in bronchopulmonary dysplasia. Pediatrics 90: 663–668
Jobe AH 1993 Pulmonary surfactant therapy. N Engl J Med 329: 1602–1607
Groneck P, Speer CP 1995 Inflammatory mediators and bronchopulmonary dysplasia. Arch Dis Child 73: F1–F3
Pierce MR, Bancalari E 1995 The role of inflammation in the pathogenesis of bronchopulmonary dysplasia. Pediatr Pulmonol 19: 371–378
De Lemos R, Coalson J, de Lemos J, King R, Clark R, Gerstmann D 1987 Ventilatory management of infant baboons with hyaline membrane disease: the use of high frequency ventilation. Pediatr Res 21: 594–602
Hamilton P, Onayemi A, Smyth J, Gillan J, Cutz E, Froese A, Bryan A 1983 Comparison of conventional and high-frequency ventilation: oxygenation and lung pathology. J Appl Physiol 55: 131–138
Thompson WK, Marchak BE, Froese AB, Bryan C 1982 High frequency oscillation compared with standard ventilation in pulmonary injury model. J Appl Physiol 52: 543–548
Clark RH, Gerstmann DR, Null DM, de Lemos RA 1992 Prospective randomized comparison of high-frequency oscillatory and conventional ventilation in respiratory distress syndrome. Pediatrics 89: 5–12
Gerstmann D, Minton S, Stoddard R, Meredith K, Monaco F, Bertrand O, Battisti J, Langhendries J, Francois A, Clark R 1996 The Provo multicenter early high-frequency oscillatory ventilation trial: improved pulmonary and clinical outcome in respiratory distress syndrome. Pediatrics 98: 1044–1057
HIFI Study Group 1989 High-frequency oscillatory ventilation compared with conventional mechanical ventilation in the treatment of respiratory failure in preterm infants. N Engl J Med 320: 88–93
HiFO Study Group 1993 Randomized study of high-frequency oscillatory ventilation in infants with severe respiratory distress syndrome. J Pediatr 122: 609–619
Thome U, Götze-Speer B, Speer CP, Pohlandt F 1998 Comparison of pulmonary inflammatory mediators in preterm infants treated with intermittent positive pressure ventilation or high frequency oscillatory ventilation. Pediatr Res 44: 330–337
Merz U, Kellinghaus M, Häusler M, Rose E, Hörnchen H, Klosterhalfen B 2000 Effects of prolonged partial liquid ventilation, high frequency ventilation and conventional ventilation on gas exchange and lung pathology in newborn surfactant-depleted piglets. Shock 13: 472–477
Smith KM, Mrozek JD, Simonton SC, Bing DR, Meyers PA, Connett JE, Mammel MC 1997 Prolonged partial liquid ventilation using conventional and high-frequency ventilatory techniques: gas exchange and lung pathology in an animal model of respiratory distress syndrome. Crit Care Med 25: 1888–1897
Hummler HD, Thome U, Schulze A, Schnabel R, Pohlandt F, Franz AR 2001 Spontaneous breathing during partial liquid ventilation in animals with meconium aspiration. Pediatr Res 49: 572–580
Smith TM, Steinhorn DM, Thusus K, Fuhrman BP, Dandona P 1995 A liquid perfluorochemical decreases the in vitro production of reactive oxygen species by alveolar macrophages. Crit Care Med 23: 1533–1539
Steinhorn DM, Papo MC, Fuhrman BP 1996 Oxidative damage is reduced during partial liquid ventilation with Perflubron. Crit Care Med 24: A148( abstr)
Thomassen MJ, Buhrow LT, Wiedemann HP 1997 Perflubron decreases inflammatory cytokine production by human alveolar macrophages. Crit Care Med 25: 2045–2047
Varani J, Hirschl RB, Dame M, Johnson K 1996 Perfluorocarbon protects lung epithelial cells from neutrophil-mediated injury in an in vitro model of liquid ventilation therapy. Shock 6: 339–344
Lachmann B, Robertson B, Vogel J 1980 In vivo lung lavage as an experimental model of the respiratory distress syndrome. Acta Anaesth Scand 24: 231–236
Rennard SI, Basset G, Lecossier D, O'Donnell KM, Pinkston P, Martin PG, Crystal RG 1986 Estimation of volume of epithelial lining fluid recovered by lavage using urea as marker of dilution. J Appl Physiol 60: 532–538
Quintel M, Heine M, Hirschl RB, Tillmanns R, Wessendorf V 1998 Effects of partial liquid ventilation on lung injury in a model of acute respiratory failure: a histologic and morphometric analysis. Crit Care Med 26: 833–843
McCulloch PR, Forkert PG, Froese AB 1988 Lung volume maintenance prevents injury during high-frequency oscillatory ventilation in surfactant-deficient rabbits. Am Rev Respir Dis 137: 1185–1192
Meredith KS, de Lemos RA, Coalson JJ, King RJ, Gerstmann DR, Kumar R, Kuehl TJ, Winter DC, Taylor A, Clark RH 1989 Role of lung injury in the pathogenesis of hyaline membrane disease in premature baboons. J Appl Physiol 66: 2150–2158
Sandhar BK, Nibblett DJ, Argiras EP, Dunnill MS, Sykes MK 1988 Effects of positive end-expiratory pressure on hyaline membrane formation in a rabbit model of the neonatal respiratory distress syndrome. Intensive Care Med 14: 538–546
Gauger PG, Pranikoff T, Schreiner RJ, Moler FW, Hirschl B 1996 Initial experience with partial liquid ventilation in pediatric patients with the acute respiratory distress syndrome. Crit Care Med 24: 16–22
Steinhorn DM, Papo MC, Rotta AT, Aljada A, Fuhrman BP, Dandona P 1999 Liquid ventilation attenuates pulmonary oxidative damage. J Crit Care 14: 20–28
Colton DM, Till GO, Johnson KJ, Gater JJ, Hirschl RB 1999 Partial liquid ventilation decreases albumin leak in the setting of acute lung injury. J Crit Care 13: 136–139
Rotta AT, Steinhorn DM 1998 Partial liquid ventilation reduces pulmonary neutrophil accumulation in an experimental model of systemic endotoxemia and acute lung injury. Crit Care Med 26: 1707–1715
Kelly J 1990 Cytokines of the lung. Am Rev Respir Dis 141: 388–401
Tremblay L, Valenza F, Ribeiro SP, Li J, Slutsky AS 1997 Injurious ventilatory strategies increase cytokines and c-fos m-RNA expression in an isolated rat lung model. J Clin Invest 99: 944–952
Croce MA, Fabian TC, Patton JH Jr, Melton SM, Moore M, Trenthem LL 1998 Partial liquid ventilation decreases the inflammatory response in the alveolar environment of trauma patients. J Trauma 45: 273–80
Merz U, Klosterhalfen B, Kellinghaus M, Peschgens T, Pluschke S, Hoernchen H 2001 Effects of single and multiple doses of perfluorocarbon in comparison with continuous partial liquid ventilation on gas exchange and lung pathology in newborn surfactant-depleted pigs. Crit Care Med 29: 645–651
Dargaville PA, South M, Vervaart P, McDougall PN 1999 Validity of markers of dilution in small volume lung lavage. Am J Respir Crit Care Med 160: 778–784
Kawamae K, Pristine G, Chiumello D, Tremblay LN, Slutsky AS 2000 Partial liquid ventilation decreases serum tumor necrosis factor-alpha concentrations in a rat acid aspiration lung injury model. Crit Care Med 28: 479–483
Verbrugge SJ, Uhlig S, Neggers SJ, Martin C, Held HD, Haitsma JJ, Lachmann B 1999 Different ventilation strategies affect lung function but do not increase tumor necrosis factor-alpha and prostacyclin production in lavaged rat lungs in vivo. Anesthesiology 91: 1834–1843
Bagchi A, Viscardi RM, Taciak V, Ensor JE, McCrea KA, Hasday JD 1994 Increased activity of interleukin-6 but not tumor necrosis factor-alpha in lung lavage of premature infants is associated with the development of bronchopulmonary dysplasia. Pediatr Res 36: 244–252
Groneck P, Goetze-Speer B, Oppermann M, Eiffert H, Speer CP 1994 Association of pulmonary inflammation and increased microvascular permeability during the development of bronchopulmonary dysplasia: a sequential analysis of inflammatory mediators in respiratory fluids of high-risk preterm neonates. Pediatrics 93: 712–718
Wang JY, Yeh TF, Lin Yj, Chen WY, Lin CH 1997 Early postnatal dexamethasone therapy may lessen lung inflammation in premature infants with respiratory distress syndrome on mechanical ventilation. Pediatr Pulmonol 23: 193–197
Kotecha S, Wilson L, Wangoo A, Silverman M, Shaw RJ 1996 Increase in interleukin (IL)-1β and IL-6 in bronchoalveolar lavage fluid obtained from infants with chronic lung disease of prematurity. Pediatr Res 40: 250–256
Acknowledgements
The authors thank Prof. Dr. Kirckpatrick (Institute of Pathology, University of Mainz, Germany) for the RIA and Leon Muys for his excellent technical assistance.
Author information
Authors and Affiliations
Corresponding author
Additional information
Financial support from START, Medical Faculty of the Aachen University of Technology, Germany (grant no. 5796/II).
Rights and permissions
About this article
Cite this article
Merz, U., Klosterhalfen, B., Häusler, M. et al. Partial Liquid Ventilation Reduces Release of Leukotriene B4 and Interleukin-6 in Bronchoalveolar Lavage in Surfactant-Depleted Newborn Pigs. Pediatr Res 51, 183–189 (2002). https://doi.org/10.1203/00006450-200202000-00010
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/00006450-200202000-00010
This article is cited by
-
Hypothermic total liquid ventilation after experimental aspiration-associated acute respiratory distress syndrome
Annals of Intensive Care (2018)
-
High-frequency oscillatory ventilation combined with partial liquid ventilation in experimental lung injury: effects on lung cell apoptosis
Wiener klinische Wochenschrift (2015)
-
High-frequency Partial Liquid Ventilation in Two Infants
Journal of Perinatology (2004)