Abstract
The Fas-Fas ligand (FasL) pathway of apoptosis is abnormally activated in diseases associated with impaired immune tolerance or chronic inflammation. Pregnancy-related hypertension is a spectrum of disease that commonly causes significant morbidity in women and in their newborn infants, is associated with generalized inflammation, and may be causally related to impaired maternal-fetal tolerance. Our recent observation of enhanced trophoblast expression of FasL in one form of pregnancy-related hypertension led us to hypothesize that this group of disorders might be associated with abnormal activation of the Fas-FasL pathway. To test this hypothesis, we prospectively quantified soluble and leukocyte-associated Fas receptor and FasL in the maternal and umbilical cord blood (CB) sera of 20 gestations complicated by preeclampsia and of 18 normal control gestations, using ELISA and flow cytometric analyses. We determined higher soluble FasL levels in paired maternal and CB sera of hypertensive gestations compared with control gestations (p < 0.01); in contrast, soluble Fas levels were similar between groups. Surface expression of FasL was lower on maternal (p < 0.01) and CB (p < 0.05) neutrophils from affected gestations, whereas surface Fas expression was lower on maternal (p < 0.02), but not CB, neutrophils and lymphocytes. We conclude that expression of Fas and FasL in sera and on leukocytes is altered in gestations complicated by preeclampsia, and speculate that activation of the Fas-FasL pathway mediates associated pathologic processes in affected women and in their neonates.
Similar content being viewed by others
Main
Activation of the Fas-Fas Ligand pathway involves cellular interactions between the Fas receptor and FasL, and can result in apoptosis or in an inflammatory response (1). The Fas receptor (CD95, Apo-1, FasR), a type I integral membrane protein belonging to the tumor necrosis factor receptor family, is expressed on numerous cell types including hematopoietic cells, and its expression increases during inflammation (1). In contrast, expression of FasL (CD95L), a type II transmembrane molecule belonging to the tumor necrosis factor receptor superfamily, is limited to certain leukocytes and tissues with immune privilege (2). Fas-FasL interactions leading to clonal deletion of antigen-presenting cells have been implicated in the establishment of graft tolerance (3), and provide one explanation for the immune privilege status of certain tissues, including the placenta, cornea, and testis (2). In contrast, abnormal function of the Fas-FasL pathway is involved in the pathogenesis of a variety of disorders, including cytopenias, autoimmune diseases, graft-versus-host disease, and graft rejection (1, 3–6).
Mice with the gld mutation are deficient in FasL function and have smaller litters with decreased viability (7). Studies in these mice suggest that the Fas-FasL pathway contributes to preservation of the fetal allograft by preventing the trafficking of activated leukocytes between the mother and fetus during normal gestation, observations also supported by findings in humans (8–10). These studies suggest that interactions between FasL-positive placental trophoblasts and activated maternal lymphocytes that express Fas contribute to the induction of tolerance through a clonal deletion mechanism (8–11). Conversely, alternative mechanisms may be contributory to establishing maternal-fetal tolerance during pregnancy, as gld mice can reproduce (7), and clonotypic maternal T cells that remain after clonal deletion are unresponsive to fetal antigen challenge (9). In addition, trophoblasts themselves possess certain properties that could promote tolerance. These include a lack of MHC antigen expression (12), the presence of immunosuppressive substances such as transforming growth factor-β(13), and the expression of CD59, an inhibitor of the complement cascade (14).
Pregnancy-related hypertension encompasses a spectrum of disease that affects up to 10% of pregnancies and causes significant morbidity in women (15) and in their newborn infants (16, 17). Although numerous mechanisms have been proposed to explain the pathogenesis of pregnancy-related hypertension (18–21), its origin remains obscure. However, increasing evidence supports an immune-mediated pathogenesis for this disorder (22). Establishment of normal maternal-fetal tolerance appears to involve components of the Fas-FasL pathway (7–9), which also may mediate rejection of transplanted tissues (2, 3). Thus, it is reasonable to speculate that aberrant function of the Fas-FasL pathway might also be involved in a maternal rejection of the fetal allograft. The contribution of this pathway to the pathogenesis of pregnancy-related hypertension is further suggested by associated maternal and neonatal complications, including hepatic inflammation, endothelial injury, neutrophil activation, and neutropenia (17, 18, 20, 23), which can be mediated by the Fas-FasL pathway (1, 5, 6). In addition, we have recently reported enhanced expression of FasL on placental trophoblasts in PIH (24).
We hypothesized that abnormal activation of the Fas-FasL pathway in pregnancy-related hypertension would result in increased amounts of the soluble forms of the Fas receptor or of FasL, as has been observed in other disease states linked with this pathway (4, 6, 25, 26). We further hypothesized that surface expression of Fas or FasL might also be elevated in maternal or CB leukocytes in this disorder, because inflammation has been associated with up-regulated expression of these proteins (27). To test these hypotheses, we measured Fas and FasL in the sera and on the surfaces of leukocytes of maternal blood and umbilical CB samples from pregnancies complicated by one form of pregnancy-related hypertension, preeclampsia, and in healthy normotensive control pregnancies, using ELISA and flow cytometric analysis.
METHODS
Study subjects.
The study population was made up of pregnant women with singleton gestations, after their admission to the Labor and Delivery unit at Shands Hospital-University of Florida. Subjects were enrolled consecutively from the period of August 9, 1999, through March 2, 2000. Peripheral venous blood samples were obtained from maternal subjects and from the umbilical cord of placentas immediately after delivery. The study was approved by the University of Florida Institutional Review Board for Human Studies, and informed consent was obtained from each subject.
The diagnosis and severity of one form of pregnancy-related hypertension, preeclampsia, was made by the attending obstetrician in pregnant women according to guidelines established by the American College of Obstetricians and Gynecologists (28). Preeclampsia was diagnosed if after several recordings systolic blood pressure was >140 mm Hg or a diastolic blood pressure was >90 mm Hg, with an onset after 20 wk of gestation, in the presence of proteinuria (≥0.3 g protein in a 24-h specimen, or ≥30 mg/dL in a random urine determination). Preeclampsia was considered to be severe if hypertension was associated with one or more of the following clinical manifestations: blood pressure >160–180 mm Hg systolic or >110 mm Hg diastolic; renal abnormalities (proteinuria >5 g/24 h, elevated serum creatinine, oliguria <500 mL/24 h); hematologic abnormalities (thrombocytopenia, microangiopathic hemolysis); hepatocellular dysfunction (elevated liver enzymes, right-upper quadrant pain); neurologic symptoms (headache, visual disturbances, seizures); pulmonary edema; or fetal abnormalities (intrauterine growth restriction, oligohydramnios). Exclusionary criteria included proven maternal or fetal infection, autoimmune disorders, and epilepsy. Control subjects comprised normotensive women with healthy pregnancies.
Determination of sFas and sFasL in maternal and CB sera.
Serum obtained from paired maternal and CB samples was separated into 0.5-mL aliquots and stored at −70°C until analysis. Duplicate samples were analyzed for their concentration of sFas or sFasL by ELISA (MBL, Nagoya, Japan), according to the manufacturer's instructions. Lower limits of detection were 31 pg/mL for sFas and 78 pg/mL for sFasL.
Detection of surface Fas and FasL on maternal and CB leukocytes.
After erythrocyte lysis of whole blood samples, cells were suspended in buffer (RPMI 1640, 2% FCS, 0.05% sodium azide) and stained for surface expression of Fas and FasL, as previously described (29). Briefly, to determine surface Fas expression, cell suspensions were stained with anti-CD95 MAb (IgG1, clone DX2, BD PharMingen, San Diego, CA, U.S.A.) conjugated to FITC, or a FITC-conjugated isotype control IgG antibody (Becton Dickinson, Mountainview, CA, U.S.A.). Cells were fixed with 2% paraformaldehyde (Sigma Chemical Co., St. Louis, MO, U.S.A.), then analyzed within 24 h of processing using a FACScan flow cytometer (Becton Dickinson). Neutrophil and lymphocyte populations were gated by using specific forward- and side-scatter characteristics, and results expressed as the mean fluorescence intensity of 10,000–20,000 gated events.
For detection of surface FasL, cells were first suspended in media (RPMI 1640) containing 2% FCS, 1 mg/mL BSA (both, Sigma Chemical Co.), and 250 μg/mL human immunoglobulin (Gammimune, Bayer Corporation, Elkhart, IN, U.S.A.) to block nonspecific binding. Cell suspensions were then stained with the primary MAb (rabbit anti-human CD95L, clone C20, or an isotype control IgG antibody, Santa Cruz Biochemicals, Santa Cruz, CA, U.S.A.), followed by staining with FITC-labeled goat-anti-rabbit antibody [F(ab)′2 fragments; Jackson Immunoresearch, West Grove, PA, U.S.A.]. Fixed cells were analyzed as described above.
Statistical analysis.
Data are presented as the mean ± SD unless otherwise indicated. Data comparisons were analyzed by one-way ANOVA (or the Kruskal-Wallis ANOVA on Ranks), the Mann-Whitney test, or by χ2 analysis as appropriate (30); regression analyses were performed using the Spearman rank order correlation (30). All data were analyzed using the PC program SigmaStat for Windows, Version 2.03 (SPSS, Inc., San Rafael, CA, U.S.A.); a p value < 0.05 was considered to indicate statistical significance.
RESULTS
Patient demographics.
The maternal study population consisted of 20 women with preeclampsia and 18 healthy controls (Table 1). Maternal ages and the racial distribution of study subjects were similar between study groups, as was the proportion of primiparous women. Twelve women met diagnostic criteria for severe preeclampsia. Two of these women had chronic hypertension with superimposed preeclampsia. The duration of ruptured membranes and length of labor did not differ between groups as a whole. However, labor was shorter in women having severe preeclampsia (5 ± 8 h, p < 0.05 versus controls, mild preeclampsia), reflecting the need for emergent delivery because of worsening disease. Six of these women were delivered of their infants in the absence of labor, with intact membranes. More CS were performed for preeclampsia compared with controls, although this difference did not reach significance (p = 0.06, χ2). In the hypertensive group, eight of 12 women (67%) with severe preeclampsia were delivered of their infants by CS for worsening disease, whereas CS were performed in three patients with milder disease for failed progression of labor (mild versus severe preeclampsia, p = 0.36). Three women in the control group were delivered of their infants by CS: two for failed induction, and one for herpetic genital lesions.
The majority of preeclamptic women received magnesium sulfate therapy for their hypertension compared with only one patient in the control group given this treatment as tocolysis for premature labor. No differences were noted between antibiotic therapy between groups: three preeclamptic patients and seven control patients received prophylactic antibiotic therapy for a positive group B streptococcal screen or for unknown status (p = 0.14, χ2). Six women with severe preeclampsia and preterm gestations, but none with mild disease, received at least one dose of betamethasone or dexamethasone before delivery, whereas only one woman in the control group with preterm labor received this treatment.
Severe preeclampsia was associated with a lower mean gestational age (34 ± 3 wk;p < 0.01, ANOVA) versus controls (38 ± 2 wk) or milder disease (38 ± 1 wk). Overall the mean birth weights of delivered infants were not significantly lower in preeclamptic compared with control gestations. However, birth weights of neonates after severe preeclampsia were lower (2050 ± 812 g, p < 0.01, ANOVA) versus controls (3221 ± 492 g) or mild preeclampsia (3262 ± 635 g), and three of these neonates were small-for-gestational age. Neonatal neutrophil counts were not obtained prospectively in this study; however, neutrophil counts in the first 24 h of life in those tested were lower in the severe preeclampsia group (n = 11; 3490 ± 2993/μL) versus controls (n = 6; 7534 ± 2642/μL;p < 0.02, ANOVA); only one neonate, born at 27 wk gestation to a mother with severe preeclampsia, met criteria for neutropenia (640/μL) (31).
sFas and sFasL levels in maternal and CB sera.
Median concentrations of sFas in sera were similar between groups for both maternal samples (controls, 986 pg/mL; range, 550–1556 pg/mL;versus preeclampsia, 1152 pg/mL; 752–1980 pg/mL;p = 0.16 by Mann-Whitney) and CB samples (controls, 442 pg/mL; 300–1344 pg/mL;versus preeclampsia, 520 pg/mL; 365–1530 pg/mL;p = 0.10). For each group, maternal sFas values were higher than those in paired CB samples (p < 0.05). In contrast, sFasL serum concentrations were higher in preeclamptic gestations than in controls, and were generally concordant between paired maternal and CB samples (Fig. 1). A higher proportion of women from the control group (12 of 18) had serum FasL levels below the assay's limit of detection compared with four of 20 in the preeclampsia group (p < 0.02, χ2). In contrast, nine of 18 samples of CB sera from the control group had undetectably low FasL levels whereas all CB samples from preeclamptic gestations were measurable (p < 0.01). Median serum concentrations of sFasL in maternal and CB sera did not differ between those having mild preeclampsia (n = 8) and more severe disease (n = 12), respectively, maternal sera, 156 pg/mL; range, 78–296pg/mL;versus 160 pg/mL; range, 80–1324 pg/mL;p = 0.82; CB sera, 144 pg/mL; range, 78–387 pg/mL;versus 194 pg/mL; range, 78–424 pg/mL;p = 0.75. Regression analyses suggested that sFasL levels were independent of gestational age in both control (r = −0.46) and in preeclamptic (r = −0.34) subjects (p > 0.05).
sFasL levels in maternal and umbilical CB sera. Results represent individual sFasL concentrations (pg/mL) in paired samples of maternal (Mat) and CB sera from control gestations and gestations complicated by preeclampsia (PE). The solid horizontal lines represent mean values for each group;p < 0.02, controls versus PE (Mann Whitney). The shaded area represents the limit of sensitivity for the assay, and the proportion of values falling within this area varied for each group (discussed in “Results”).
Steroid treatment was not associated with a difference in sFasL levels in gestations affected by severe preeclampsia: maternal sFasL, no steroids, 422 ± 601 pg/mL versus with steroids, 274 ± 249 pg/mL, p = 0.59; CB sFasL, no steroids, 157 ± 129 pg/mL versus with steroids, 257 ± 153 pg/mL, p = 0.33. The presence or absence of labor, respectively, did not appear to affect sFasL levels in gestations affected by severe preeclampsia: maternal sFasL, 289 ± 311 pg/mL versus 363 ± 478 pg/mL, p = 0.91; CB sFasL, 205 ± 150 pg/mL versus 221 versus 140 pg/mL, p = 0.86.
Surface expression of Fas and FasL in maternal and CB leukocytes.
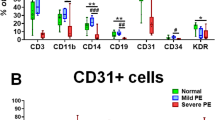
Surface expression of the Fas receptor and FasL was determined on gated neutrophil and lymphocyte populations in maternal and CB samples from eight control and 11 preeclamptic gestations. Maternal neutrophils and lymphocytes from affected gestations had less surface Fas expression compared with controls (Fig. 2A). In a similar manner, surface expression of FasL was lower on both maternal and CB neutrophils from preeclamptic gestations than from controls, although surface FasL expression on maternal or CB lymphocytes was not different between groups (Fig. 2B).
Surface Fas and FasL expression on maternal (Mat) and CB leukocytes. Results represent the mean fluorescence intensity (MFI) of surface Fas receptor (A) and of surface FasL (B) on Mat and CB neutrophils (PMN) and lymphocytes (Lymph) from control (□) and hypertensive gestations (▪). *p < 0.02, **p < 0.05, preeclampsia versus controls (ANOVA).
DISCUSSION
We observed elevated sFasL concentrations in the maternal and CB sera of gestations complicated by preeclampsia, although the source(s) of this protein remains unclear. The fetal trophoblast is one likely candidate, suggested by our recent observation that trophoblasts in PIH have enhanced FasL expression (24). FasL is an integral membrane protein that can be cleaved into its soluble form by the MMP matrilysin (32), which is overexpressed by trophoblasts in preeclamptic placentas (33). Continuous exposure of the fetal trophoblast to maternal blood would allow FasL, cleaved from the trophoblast into soluble form, access to both the maternal and fetal circulations, and is consistent with the similar maternal and CB concentrations of sFasL that we showed in the present study. A second source of the elevated levels of sFasL might be membrane-associated FasL released from the surfaces of activated neutrophils (34). This possibility is supported both by the lower neutrophil surface expression of FasL in preeclamptic gestations, and by the observation that preeclampsia is associated with neutrophil activation (20, 23). A third possible explanation is that increased levels of inflammatory cytokines in preeclampsia, such as TNF-α(35), might down-regulate FasL expressed on endothelial cells (1), also activated in preeclampsia (36). However, whether this down-regulation is caused by cleavage of the membrane-bound form of FasL is not clear (1). Alternatively, elevated levels of TNF-α could potentially affect sFasL levels indirectly by inducing MMP production (37) and subsequent cleavage of membrane-bound FasL (32).
Several therapeutic or physiologic factors might have potentially influenced the expression of Fas-related proteins in our study subjects. For example, magnesium sulfate therapy was disproportionately represented in the preeclampsia group, although such therapy has not been reported to have a direct effect on leukocytes or the Fas-FasL pathway. However, it may have general antiinflammatory effects, including decreased expression of MMP (38). A number of preeclamptic subjects with preterm gestations also received antenatal steroids, which can induce expression of Fas-related proteins (39, 40). However, we found no differences in serum sFasL concentrations between treated and untreated women with severe preeclampsia, making it less likely that exogenous steroids influenced our results. Although physiologic factors, such as prolonged labor or duration of ruptured membranes, are associated with cytokine release (41), which could potentially affect Fas expression, we found no overall differences between groups with respect to these measurements. Indeed, many of the women with severe preeclampsia were delivered of their infants in the absence of labor, with intact membranes. Gestational age differences might also have contributed to variances in sFasL levels between groups. This question is difficult to resolve, however, because premature delivery is an abnormal event, and sampling of normal human fetuses to determine age-specific values is not feasible. Additionally, it is possible that our assay may have underestimated the amount of bioactive FasL in the sera by not detecting the intact form of FasL, which can be found in soluble form in association with microvesicles (42).
The clinical relevance of elevated sFasL levels in the maternal and CB circulation during preeclampsia is suggested by studies of other disorders. sFasL and a membrane-bound form associated with microvesicles are bioactive (25, 42, 43) and can mediate a variety of pathologic conditions including cytopenias, hepatic inflammation, autoimmune disorders, and rejection syndromes (1, 3–6, 44). In addition, although sFasL can inhibit the cytoxicity of membrane-bound FasL (45), it is itself chemotactic for neutrophils (46) and could promote the neutrophilic infiltration observed in preeclamptic placentas (20, 23). Because tissue expression of FasL is also associated with neutrophil-mediated injury and apoptosis (47, 48), it is conceivable that a high expression of FasL on trophoblasts (24) in the presence of elevated levels of sFasL might potentially exacerbate a similar process in preeclampsia.
Cytotoxicity associated with sFasL might also contribute to the cytopenias observed both in preeclamptic women and in their neonates. Patients with lymphocytic leukemia were shown to have elevated serum levels of sFasL that correlated with the presence of neutropenia (6). This observation may have relevance to the frequent neutropenia in premature neonates delivered to hypertensive women (16, 17), as we previously observed that CB sera from these gestations inhibit neutrophil production in vitro(49) and sFasL can inhibit hematopoiesis (50). Although neutrophil counts, when tested, were generally lower in neonates born to preeclamptic women, we did not attempt a correlation with sFasL levels as these counts were not prospectively determined.
Hsu et al.(51) recently reported elevated sFas levels in the sera of women with severe preeclampsia or the HELLP syndrome. In the present study, we observed a tendency for sFas levels to be higher in maternal and CB sera from preeclamptic gestations, although these differences did not reach statistical significance. It is possible that variations in the results of these two studies reflect differences in the severity of maternal disease or gestational age, as only a portion of women in our study had severe preeclampsia, and few gestations were extremely premature. In addition, although not reported, it is possible that interactions of sFas with sFasL, or its microvesicle-associated form (28), might have interfered with detection by our assay system.
We hypothesized that Fas expression would be elevated in leukocytes from preeclamptic gestations, on the basis of reports of increased lymphocyte Fas expression in disorders associated with abnormalities of the Fas-FasL pathway (52). Thus, decreased Fas expression in maternal leukocytes from affected gestations was an unexpected finding. Enhanced Fas expression on lymphocytes has been observed in response to stimulation with cytokines (53). Thus, we anticipated that leukocyte activation after exposure to the elevated levels of TNF-α associated with preeclampsia (35) would have increased, not decreased, Fas expression. Although decreased Fas expression might have been related to increased release of the soluble protein, our observation of similar sFas levels in affected and normal control gestations does not support this possibility. An alternative explanation for low Fas expression might be that lymphocytes from women predisposed to develop preeclampsia have intrinsically low Fas expression, which if associated with a resistance to apoptosis might allow their evasion of normal immune mechanisms. A defect in the expected clonal deletion of maternal antigen-presenting cells (8, 9) could potentially be an inciting factor for the development of pregnancy-related hypertension by allowing the unwanted trafficking of maternal cells (7). This possibility is supported by observations in Fas-deficient lpr mice, in which a parallel mechanism contributes to their development of autoimmune phenomena (54) and graft-versus-host disease (55).
The mechanism underlying the lower surface FasL expression on maternal and CB neutrophils in preeclamptic gestations is also not clear. One explanation may be that low surface expression resulted from cleavage of membrane-bound FasL from activated neutrophils (34), as suggested by high serum levels in those subjects. It is unlikely that elevated TNF-α levels (35) might have accounted for this observation, since TNF-α does not appear to affect neutrophil expression of either Fas or FasL (56). However, it is possible that cleavage of membrane-bound FasL by MMP (32) might have resulted in lower FasL expression on leukocytes and secondarily elevated sFasL levels in sera. In addition, although we attempted to process all samples in a timely manner, delayed processing can activate neutrophils and result in increased surface expression of FasL and release of sFasL (27). However, such activation might have also been expected to increase Fas expression on the same neutrophils (27), in contrast to the lower surface levels we observed, making this explanation less likely. Conversely, the observation that defective FasL function in gld mice is associated with reproductive abnormalities, including small litter size and placental inflammation (7), induces speculation regarding the relationship between an intrinsic defect of FasL expression or function and the pathogenesis of pregnancy-related hypertension. Human placentas of preeclamptic gestations also exhibit neutrophilic infiltrates (7), a reflection of the abnormal inflammatory response observed in this disorder (20, 23). Although the underlying mechanism remains to be defined, such inflammation might be associated with deficient FasL function, because antigen-presenting cells of gld mice promote chronic inflammatory disease, a result of defective elimination of activated T cells (57).
The results of the present studies complement our previous findings of enhanced expression of Fas-associated proteins in PIH (24), and suggest a contribution of the Fas-FasL pathway to the pathogenesis of this group of disorders, or to the associated maternal and neonatal complications. However, whether the underlying mechanism(s) involves impaired maternal-fetal immunity, reflects exacerbated inflammation, or is associated with an alternative process is not clear. Investigations that further define the regulation of Fas-FasL interactions, as well as longitudinal clinical studies, will be important to understanding a role of the Fas-FasL pathway in both normal and pathologic gestations.
Abbreviations
- CB:
-
umbilical cord blood
- CS:
-
cesarean section
- FasL:
-
Fas ligand
- MMP:
-
matrix metalloproteinase
- PIH:
-
pregnancy-induced hypertension
- sFas:
-
soluble Fas
- sFasL:
-
soluble Fas ligand
- SGA:
-
small-for-gestational age
- TNF-α:
-
tumor necrosis factor-α
References
Nagata S 1999 Fas ligand-induced apoptosis. Annu Rev Genet 33: 29–55
Griffith TS, Brunner T, Fletcher SM, Green DR, Ferguson TA 1995 Fas ligand-induced apoptosis as a mechanism of immune privilege. Science 270: 1189–1192
Kabelitz D 1998 Apoptosis, graft rejection, and transplantation tolerance. Transplantation 65: 869–875
Haneline LS, Broxmeyer HE, Cooper S, Hangoc G, Carreau M, Buchwald M, Clapp DW 1998 Multiple inhibitory cytokines induce deregulated progenitor growth and apoptosis in hematopoietic cells from Fac−/− mice. Blood 91: 4092–4098
Waring P, Mullbacher A 1999 Cell death induced by the Fas/Fas ligand pathway and its role in pathology. Immunol Cell Biol 77: 312–317
Liu JH, Wei S, Lamy T, Epling-Burnette PK, Starkebaum G, Djeu JY, Loughran TP 2000 Chronic neutropenia mediated by fas ligand. Blood 95: 3219–3222
Hunt JS, Vassmer D, Ferguson TA, Miller L 1997 Fas ligand is positioned in mouse uterus and placenta to prevent trafficking of activated leukocytes between the mother and the conceptus. J Immunol 158: 4122–4128
Uckan D, Steele A, Cherry Wang BY, Chamizo W, Koutsonikolis A, Gilbert-Barness E, Good RA 1997 Trophoblasts express Fas ligand: a proposed mechanism for immune privilege in placenta and maternal invasion. Mol Hum Reprod 3: 655–662
Jiang SP, Vacchio MS 1998 Multiple mechanisms of peripheral T cell tolerance to the fetal “allograft.”. J Immunol 160: 3086–3090
Kauma SW, Huff TF, Hayes N, Nilkaeo A 1999 Placental Fas ligand expression is a mechanism for maternal immune tolerance to the fetus. J Clin Endocrinol Metab 84: 2188–2194
Guller S, LaChapelle L 1999 The role of placental Fas ligand in maintaining immune privilege at maternal-fetal interfaces. Semin Reprod Endocrinol 17: 39–44
Bulmer JN 1992 Immune aspects of pathology of the placental bed contributing to pregnancy pathology. Baillieres Clin Obstet Gynaecol 6: 461–488
Kauma S, Matt D, Strom S, Eierman D, Turner T 1990 Interleukin-1 beta, human leukocyte antigen HLA-DR alpha, and transforming growth factor-beta expression in endometrium, placenta, and placental membranes. Am J Obstet Gynecol 163: 1430–1437
Tedesco F, Narchi G, Radillo O, Meri S, Ferrone S, Betterle C 1993 Susceptibility of human trophoblast to killing by human complement and the role of the complement regulatory proteins. J Immunol 151: 1562–1570
Perloff D 1998 Hypertension and pregnancy-related hypertension. Cardiol Clin 16: 79–101
Brazy JE, Grimm JK, Little VA 1982 Neonatal manifestations of severe maternal hypertension occurring before the thirty-sixth week of pregnancy. J Pediatr 100: 265–271
Koenig JM, Christensen RD 1989 Incidence, neutrophil kinetics, and natural history of neonatal neutropenia associated with maternal hypertension. N Engl J Med 321: 557–562
Taylor RN, de Groot CJ, Cho YK, Lim KH 1998 Circulating factors as markers and mediators of endothelial cell dysfunction in preeclampsia. Semin Reprod Endocrinol 16: 17–31
Walsh SW 1998 Maternal-placental interactions of oxidative stress and antioxidants in preeclampsia. Semin Reprod Endocrinol 16: 93–104
Redman CW, Sacks GP, Sargent IL 1999 Preeclampsia: an excessive maternal inflammatory response to pregnancy. Am J Obstet Gynecol 180: 499–506
Esplin MS, Fausett MB, Fraser A, Kerber R, Mineau G, Carrillo J, Varner MW 2001 Paternal and maternal components of the predisposition to preeclampsia. N Engl J Med 344: 867–872
Taylor RN 1997 Review: immunobiology of preeclampsia. Am J Reprod Immunol 37: 79–86
Clark P, Boswell F, Greer IA 1998 The neutrophil and preeclampsia. Semin Reprod Endocrinol 16: 57–64
Koenig JM, Chegini N 2000 Enhanced expression of Fas-associated proteins in decidual and trophoblastic tissue in pregnancy-induced hypertension. Am J Reprod Immunol 44: 347–349
Tanaka M, Suda T, Haze K, Nakamura N, Sato K, Kimura F, Motoyoshi K, Mizuki M, Tagawa S, Ohga S, Hatake K, Drummond AH, Nagata S 1996 Fas ligand in human serum. Nat Med 2: 317–322
Kanda Y, Tanaka Y, Shirakawa K, Yatomi T, Nakamura N, Kami M, Saito T, Izutsu K, Asai T, Yuji K, Ogawa S, Honda H, Mitani K, Chiba S, Yazaki Y, Hirai H 1998 Increased soluble Fas-ligand in sera of bone marrow transplant recipients with acute graft-versus-host disease. Bone Marrow Transplant 22: 751–754
Mincheff M, Loukinov D, Zoubak S, Hammett M, Meryman H 1998 Fas and Fas ligand expression on human peripheral blood leukocytes. Vox Sang 74: 113–121
[No author] 1996 ACOG technical bulletin. Hypertension in pregnancy. Number 219-January 1996. Committee on Technical Bulletins of the American College of Obstetricians and Gynecologists. Int J Gynaecol Obstet 53: 175–183
Allgaier B, Shi M, Luo D, Koenig JM 1998 Spontaneous and Fas-mediated apoptosis are diminished in umbilical cord blood neutrophils compared with adult neutrophils. J Leukoc Biol 64: 331–336
Glantz SA 2001 Primer of Biostatistics, 3rd Ed. McGraw-Hill, New York, pp 95–104; 250–268
Mouzinho A, Rosenfeld CR, Sanchez PJ, Risser R 1994 Revised reference ranges for circulating neutrophils in very-low-birth-weight neonates. Pediatrics 94: 76–82
Powell WC, Fingleton B, Wilson CL, Boothby M, Matrisian LM 1999 The metalloproteinase matrilysin proteolytically generates active soluble fas ligand and potentiates epithelial cell apoptosis. Curr Biol 9: 1441–1447
Vettraino IM, Roby J, Tolley T, Parks WC 1996 Collagenase-I, stromelysin-I, and matrilysin are expressed within the placenta during multiple stages of human pregnancy. Placenta 17: 557–563
Liles WC, Kiener PA, Ledbetter JA, Aruffo A, Klebanoff SJ 1996 Differential expression of Fas (CD95) and Fas ligand on normal human phagocytes: implications for the regulation of apoptosis in neutrophils. J Exp Med 184: 429–440
Williams MA, Farrand A, Mittendorf R, Sorensen TK, Zingheim RW, O'Reilly GC, King IB, Zebelman AM, Luthy DA 1999 Maternal second trimester serum tumor necrosis factor-alpha-soluble receptor p55 (sTNFp55) and subsequent risk of preeclampsia. Am J Epidemiol 149: 323–329
Roberts JM, Taylor RN, Goldfien A 1991 Clinical and biochemical evidence of endothelial cell dysfunction in the pregnancy syndrome preeclampsia. Am J Hypertens 4: 700–708
Ohta S, Imai K, Yamashita K, Matsumoto T, Azumano I, Okada Y 1998 Expression of matrix metalloproteinase 7 (matrilysin) in human osteoarthritic cartilage. Lab Invest 78: 79–87
Shibata M, Ueshima K, Harada M, Nakamura M, Hiramori K, Endo S, Sato N, Mukaida H, Suzuki T, Suzuki T, Inada K 1999 Effect of magnesium sulfate pretreatment and significance of matrix metalloproteinase-1 and interleukin-6 levels in coronary reperfusion therapy for patients with acute myocardial infarction. Angiology 50: 573–582
Sfikakis PP, Souliotis VL, Akbar AN, Katsilambros N, Hoffbrand VA, Panayiotidis P 1996 Regulation of bcl-2 and fas expression in primary activation of human peripheral lymphocytes is not sensitive to dexamethasone or cyclosporin-A. Hum Immunol 50: 121–126
Montani MS, Tuosto L, Giliberti R, Stefanini L, Cundari E, Piccolella E 1999 Dexamethasone induces apoptosis in human T cell clones expressing low levels of Bcl-2. Cell Death Differ 6: 79–86
Steinborn A, Niederhut A, Solbach C, Hildenbrand R, Sohn C, Kaufmann M 1999 Cytokine release from placental endothelial cells, a process associated with preterm labour in the absence of intrauterine infection. Cytokine 11: 66–73
Martinez-Lorenzo MJ, Anel A, Gamen S, Monle Lasierra P, Larrad L, Pineiro A, Alava MA, Naval J 1999 Activated human T cells release bioactive Fas ligand and APO2 ligand in microvesicles. J Immunol 163: 1274–1281
Martinez-Lorenzo MJ, Alava MA, Anel A, Pineiro A, Naval J 1996 Release of preformed Fas ligand in soluble form is the major factor for activation-induced death of Jurkat T cells. Immunology 89: 511–517
Pinkoski MJ, Brunner T, Green DR, Lin T 2000 Fas and Fas ligand in gut and liver. Am J Physiol 278: G354–G366
Tanaka M, Itai T, Adachi M, Nagata S 1998 Downregulation of Fas ligand by shedding. Nat Med 4: 31–36
Ottonello L, Tortolina G, Amelotti M, Dallegri F 1999 Soluble Fas ligand is chemotactic for human neutrophilic polymorphonuclear leukocytes. J Immunol 162: 3601–3606
Kang SM, Schneider DB, Lin Z, Hanahan D, Dichek DA, Stock PG, Baekkeskov S 1997 Fas ligand expression in islets of Langerhans does not confer immune privilege and instead targets them for rapid destruction. Nat Med 3: 738–743
Takeuchi T, Ueki T, Nishimatsu H, Kajiwara T, Ishida T, Jishage K, Ueda O, Suzuki H, Li B, Moriyama N, Kitamura T 1999 Accelerated rejection of Fas ligand-expressing heart grafts. J Immunol 162: 518–522
Koenig JM, Christensen RD 1991 The mechanism responsible for diminished neutrophil production in neonates delivered of women with pregnancy-induced hypertension. Am J Obstet Gynecol 165: 467–473
De Maria R, Testa U, Luchetti L, Zeuner A, Stassi G, Pelosi E, Riccioni R, Felli N, Samoggia P, Peschle C 1999 Apoptotic role of Fas/Fas ligand system in the regulation of erythropoiesis. Blood 93: 796–803
Hsu CD, Harirah H, Basherra H, Mor G 2001 Serum soluble Fas levels in preeclampsia. Obstet Gynecol 97: 530–532
Berridge MJ 1997 Lymphocyte activation in health and disease. Crit Rev Immunol 17: 155–178
Kawakami A, Eguchi K, Matsuoka N, Tsuboi M, Koji T, Urayama S, Nakashima T, Kawabe Y, Nagataki S 1998 Expression and function of Fas and Fas ligand on peripheral blood lymphocytes in normal subjects. J Lab Clin Med 132: 404–413
Singer GG, Carrera AC, Marshak-Rothstein A, Martinez C, Abbas AK 1994 Apoptosis, Fas and systemic autoimmunity: the MRL-lpr/lpr model. Curr Opin Immunol 6: 913–920
van den Brink MR, Moore E, Horndasch KJ, Crawford JM, Hoffman J, Murphy GF, Burakoff SJ 2000 Fas-deficient lpr mice are more susceptible to graft-versus-host disease. J Immunol 164: 469–480
Salamone G, Giordano M, Trevani AS, Gamberale R, Vermeulen M, Schettinni J, Geffner JR 2001 Promotion of neutrophil apoptosis by TNF-alpha. J Immunol 166: 3476–3483
Zhang HG, Fleck M, Kern ER, Liu D, Wang Y, Hsu HC, Yang P, Wang Z, Curiel DT, Zhou T, Mountz JD 2000 Antigen presenting cells expressing Fas ligand down-modulate chronic inflammatory disease in Fas ligand-deficient mice. J Clin Invest 105: 813–821
Acknowledgements
The authors thank the Labor and Delivery nurses and physicians at Shands-University of Florida for their help in identifying study subjects and in collecting maternal and CB samples. We also thank Drs. Nasser Chegini and Cynthia Edstrom for their helpful comments and review of this manuscript.
Author information
Authors and Affiliations
Corresponding author
Additional information
Supported partly from funds provided by The Children's Miracle Network Telethon, STOP! Children's Cancer, Inc., and the Howard Hughes Medical Institute Research Resources Program.
Presented in part at the annual meeting of the Society for Pediatric Research, Boston, MA, U.S.A., May 14, 2000.
Rights and permissions
About this article
Cite this article
Kuntz, T., Christensen, R., Stegner, J. et al. Fas and Fas Ligand Expression in Maternal Blood and in Umbilical Cord Blood in Preeclampsia. Pediatr Res 50, 743–749 (2001). https://doi.org/10.1203/00006450-200112000-00019
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/00006450-200112000-00019
This article is cited by
-
Hematological profiles of newborns of mothers with hypertensive disorders of pregnancy delivered at the University of Gondar comprehensive specialized hospital: a comparative cross-sectional study
BMC Pediatrics (2024)
-
The CD95/CD95L pathway is involved in phagocytosis-induced cell death of monocytes and may account for sustained inflammation in neonates
Pediatric Research (2013)
-
Blood parameters changes in cord blood of newborns of hypertensive mothers
European Journal of Pediatrics (2013)
-
Dysfunction of innate immunity and associated pathology in neonates
The Indian Journal of Pediatrics (2007)