Abstract
This study was designed to test the hypotheses that furosemide directly causes relaxation in human fetal airway and that delivery of loop diuretics to either the adventitial or epithelial surface of newborn mouse airway results in equivalent relaxation. Isometric tension changes were measured in human fetal (11–16 wk) trachea and mainstem bronchus rings exposed to furosemide (300 μM) or saline after acetylcholine or leukotriene D4 constriction. Significant decreases in isometric tension to furosemide were demonstrated after constriction with acetylcholine or leukotriene D4. To examine the site of effect and mimic aerosolized and systemic administration, furosemide (3–300 μM) and bumetanide (0.3–30 μM) were applied separately to epithelial and adventitial surfaces of newborn mouse airways. No differences in airway diameter changes to epithelial or adventitial furosemide or bumetanide were observed, but a 10-fold difference in potency was found. In summary, human fetal airway relaxed to furosemide when constricted with either neurotransmitter or inflammatory mediator in vitro. Further, no differences in relaxation to equimolar epithelial and adventitial furosemide were observed in isolated newborn mouse airway. Taken together, this provides evidence that furosemide has a direct, nonepithelial-dependent effect on airway smooth muscle tone.
Similar content being viewed by others
Main
Systemically administered furosemide improves pulmonary mechanics and gas exchange in infants with chronic lung disease independent of its diuretic effects (1, 2). Studies demonstrating a reduction of bronchoconstrictive responses in pediatric (3) and adult asthmatics (4, 5) with aerosolized furosemide further support the notion that a nondiuretic effect may produce improvements in pulmonary function. Indeed, the in vitro airway relaxation to furosemide that is observed in animal models (6–8) suggests that there may be a direct effect on airway smooth muscle.
However, a bronchodilatory response to inhaled furosemide is not consistently observed in infants with chronic lung disease (9, 10). Although aerosolized administration of furosemide could minimize systemic effects while producing localized bronchodilation, it is not widely accepted that inhaled furosemide has therapeutic efficacy during acute bronchoconstriction. Taken together, it is presently unclear whether these inconsistent results are because of species differences or inadequate concentrations of drug that reach the airway with aerosolized treatment, or because furosemide in fact does not act via a mechanism of direct airway smooth muscle relaxation (11). Therefore, the potential relevance of previous in vitro animal findings requires validation by the study of human airway response (12), with the first objective to test the hypothesis that furosemide causes direct relaxation of human fetal airway.
In addition to demonstrating a direct relaxing effect on airway smooth muscle, further support for the bronchodilatory response to furosemide via aerosolization would require evidence that mechanisms can be activated from the luminal side of the airway. Traditional in vitro organ bath systems do not allow for the separation of drug delivery to either luminal or abluminal surfaces. To determine whether the action of furosemide on airway muscle responses could be induced by delivery specifically to the luminal surface, additional studies were designed to separate luminal and abluminal environments in whole airway segments from newborn mice. A cannulated, perfusion system with videomicrometry measurement (13) of airway diameter was used to mimic the delivery of drug to either surface in vitro, which may be relevant to in vivo situations of aerosolization compared with systemic administration. Thus, the second hypothesis tested was that adventitial and epithelial applications of loop diuretics produce similar relaxation in isolated newborn mouse airway. Newborn mouse tracheas were studied in this series because human fetal tracheal segments were too large for this system, and more distal segments were too short.
METHODS
This study was approved by the Animal Care and Use Committee, Tripler Army Medical Center, and the Human Use Committees at Tripler Army Medical Center, Kapiolani Medical Center for Women and Children, and the University of Hawaii. Procedures involving mice were performed in accordance with the National Institutes of Health policies, the Guide for the Care and Use of Laboratory Animals (National Institutes of Health Publication No. 85–23, revised 1985), and the Animal Welfare Act and Amendments. Tripler Army Medical Center is accredited by the American Association for Accreditation of Laboratory Animal Care International.
Human fetal airway isometric tension measurement.
Human fetal airway tissues (11–16 wk gestation) were obtained from Central Laboratory for Human Embryology, University of Washington, Seattle, WA, U.S.A. Informed consent was obtained for fetal tissue donation and use in the research of birth defects and other diseases. Fetuses with known congenital or chromosomal abnormalities were excluded. Samples were placed in cold Waymouth media supplemented with 10% fetal bovine serum, 0.25 μg/mL Fungizone, and 50 μg/mL gentamicin (Life Technologies, GIBCO, Gaithersburg, MD, U.S.A.), and express mailed on ice to arrive within 36 h postmortem.
On receipt of tissue samples, intrathoracic tracheas or mainstem bronchi were identified, dissected clean of connective tissue, and placed in HEPES buffer (composition in mM: NaCl, 140; KCl, 4.5; d-glucose, 10; HEPES, 5; CaCl2·2H2O, 1.5; MgCl2·6H2O, 1). Airway segments were cut into rings of approximately 3 mm in length, with care taken not to damage the epithelial surface. Cartilage was left intact on the preparation, as removal of cartilage has been shown to reduce muscle reactivity (14). Rings were mounted on two fine stainless steel wires passed through the lumen. One wire was anchored to a stationary rod and the other to a gold chain suspended from a Grass FT.03 (Grass Instruments, Quincy, MA, U.S.A.) force-displacement transducer connected to a Gould recorder (Gould Instrument Systems, Cleveland, OH, U.S.A.) for measurement of isometric force (15). Airway rings were suspended in an organ bath at 37°C, bathed with 25 mL of HEPES buffer aerated with 100% O2.
After equilibration for 1 h, with solution exchanged every 15 min, each ring segment was stretched to the optimal point on its length-tension curve as determined by maximal tension developed to an EC50–75 of acetylcholine chloride (Sigma Chemical Co, St. Louis, MO, U.S.A.). Once this optimal resting tension was determined, the EC50 for acetylcholine was determined for each tissue. The rings were constricted with the EC50 concentration of acetylcholine, then 300 μM furosemide (American Regent Laboratories, Inc, Shirley, NY, U.S.A.) or an equal volume of saline control was added. In a separate set of experiments, rings were constricted with EC50 for LTD4 (BIOMOL Research Laboratories, Plymouth Meeting, PA, U.S.A.), followed by addition of 300 μM furosemide or saline control. The tissues were dried at 59°C for 5 d, then weighed. Concentration-response curves were not performed on the fetal tissues owing to the duration required for transport of airways together with the length of time required for each response. Methacholine responsiveness of human airways has been shown to remain intact up to 55 h after resection (16); however, at approximately 40 h after resection, we found loss of active tension with time after acetylcholine constriction.
Localization of response in newborn mouse airway.
To localize the effects of loop diuretics in the airway, adventitial and epithelial applications of loop diuretics were examined separately. Because of size limitations of the perfusion apparatus and the availability of airways, newborn mouse tracheas were used for this series of experiments. One- to five-d-old C57BL/6J mice (Jackson Laboratories, Bar Harbor, ME, U.S.A.) were killed with 1 g/kg sodium pentobarbital (Wyeth, Philadelphia, PA, U.S.A.). Tracheas (200–400 μm diameter) were isolated and cleaned free of connective tissue. Tracheal segments (2–3 mm in length) were mounted onto glass cannulas. The cannulas were set in a Plexiglas chamber (Living Systems, Burlington, VT, U.S.A.) that allows for separation of luminal (epithelial) and abluminal (adventitial) environments (13). Tissues were equilibrated in continuously exchanged HEPES buffer, pH 7.4, at 37°C, aerated with 100% O2. There was also constant flow of oxygenated HEPES buffer through the tracheal lumen. Proximal perfusion pressure was maintained at 5–8 mm Hg and flow rate was maintained at 12 mL/h. Airway diameter changes were measured by videomicrometry (Living Systems). The lack of response to luminally applied acetylcholine confirmed the separation of the epithelial and adventitial environments.
Tracheas were constricted with abluminal acetylcholine EC50–75, then exposed to cumulative doses of furosemide (3–300 μM) or bumetanide (0.3–30 μM; Hoffman-La Roche, Inc, Nutley, NJ, U.S.A.) applied to either the luminal or abluminal surfaces. A 30 μM concentration of furosemide approximates the plasma concentration expected in a newborn after i.v. administration of 1 mg/kg furosemide (17, 18).
Data analysis.
Statistics were performed using the Sigmastat statistical package (Jandel Scientific, San Rafael, CA, U.S.A.). Relaxation is expressed as a percent decrease in isometric tension for the human fetal airway, relative to the prior constriction to acetylcholine or to LTD4. Human fetal airway responses to furosemide were compared with controls by unpaired t test. Relaxation in the mouse airway is expressed as a percent increase in airway diameter, relative to the prior constriction to acetylcholine. Luminal responses were compared with abluminal responses after furosemide and bumetanide applications using two-way ANOVA for repeated measures. Normality was determined by the Kolmogorov-Smirnov test. Results are expressed as mean ±SEM.
RESULTS
Human fetal airway.
Human fetal airway rings relaxed in response to furosemide. Airway rings constricted with the neurotransmitter, acetylcholine (Fig. 1A), showed significant decreases in isometric tension in response to a single 300 μM dose of furosemide (n = 9) compared with saline controls (n = 6;p < 0.05). Airway rings constricted with an inflammatory mediator, LTD4 (Fig. 1B), also demonstrated significant decreases in isometric tension in response to furosemide (n = 6) compared with controls (n = 6;p < 0.05).
Human fetal airway relaxation in vitro to furosemide (300 μM) after constriction with acetylcholine (A) and with LTD4 (B). A, acetylcholine-constricted airways also showed a significant decrease in isometric tension in response to furosemide (n = 9) compared with saline controls (n = 6). B, airways constricted with LTD4 showed a significant decrease in isometric tension to furosemide (n = 6) compared with saline controls (n = 6). *p < 0.05.
Newborn mouse airway.
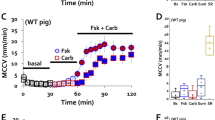
Figure 2 shows a representative tracing of changes in diameter in response to acetylcholine and furosemide. No localization of loop diuretic relaxation was observed. There were no differences in airway diameter changes to epithelial (luminal) and adventitial (abluminal) applications of furosemide and bumetanide in isolated newborn mouse airways. The increases in airway diameter were similar when responses to cumulative luminal (n = 4) and abluminal (n = 7) applications of furosemide were compared (Fig. 3A). Cumulative luminal (n = 3) and abluminal (n = 4) applications of bumetanide also resulted in similar increases in airway diameter (Fig. 3B). There were no differences in maximal airway diameter changes or potency between luminal and abluminal diuretic exposure. Maximal changes in airway diameter to furosemide and bumetanide were comparable, but a 10-fold difference in potency was observed.
Airway diameter changes in newborn mouse tracheal segments constricted with acetylcholine. A, luminal (n = 4) and abluminal (n = 7) applications of furosemide (3–300 μM) resulted in similar increases in airway diameter (p > 0.05). B, bumetanide (0.3–30 μM) also produced similar changes in airway diameter to luminal (n = 3) and abluminal (n = 4) applications (p > 0.05).
DISCUSSION
Furosemide produced relaxation in human fetal airway after constriction by the neurotransmitter, acetylcholine, as well as by the inflammatory mediator, LTD4. Elevated levels of LTD4, one of the most potent inflammatory bronchoconstrictors (19), have been demonstrated in infants with acute (20) and chronic lung disease (21). The fact that furosemide can produce relaxation in airways with increased reactivity caused by inflammatory processes suggests that it may be efficacious in the management of infants with chronic inflammatory lung disease (22). Thus, these data indicate that furosemide is capable of directly relaxing human airway segments.
When furosemide was administered separately to the adventitial and epithelial surfaces of newborn mouse airway segments, relaxation responses were similar for the same cumulative concentrations. This observation is important because it is known that responses of airway segments to different stimuli depend on the surface exposed to the stimulating agent (23). For example, there is a 29-fold increased sensitivity of airway narrowing to adventitial versus luminal applications of acetylcholine (24).
In addition to the ability to partition the luminal and abluminal environments, the cannulated perfusion system allows for assessment of relaxation by measurement of airway diameter by videomicrometry (13) rather than changes in isometric tension. When airway diameter changes are examined, airway tone alterations are independent of the degree of stretch or load on the tissue before the start of the experimental conditions (25). In addition, this videomicrometry system permits the study of much smaller tissues with smaller amounts of agonists (26), allowing for the examination of airway diameter changes in the conduit airways of newborn mice. The observation of airway dilation to adventitial and luminal delivery of furosemide indicates that airway relaxation measured by isometric tension can correlate with changes in airway diameter.
The exact mechanism by which furosemide produces airway relaxation is not completely understood. Although the most widely held notion is that its action is likely owing to its inhibitory effect on the Na-K-2Cl cotransporter, in a study using rat tracheal venules and arterioles, Corboz and coworkers (11) concluded that furosemide attenuates bronchoconstriction through a decrease in intra-airway thermal gradient because of vasodilation.
In the kidney, where it is established that loop diuretic action is mediated by the inhibition of the Na-K-2Cl cotransporter, there is a 10- to 30-fold difference in inhibitory potency between furosemide and bumetanide (27, 28). Although the present study was not designed to specifically address mechanism of airway relaxation of furosemide, the 10-fold difference in airway relaxation potency between furosemide and bumetanide suggests that airway relaxation may also be mediated, in part, by inhibition of the cotransporter. In addition, functional data exist for the presence of the Na-K-2Cl cotransporter in the airway (7, 27, 29), and there is evidence that inhibition of the Na-K-2Cl cotransporter may play a partial role in airway relaxation (29). In summary, the relaxation of isolated human fetal airway in vitro, coupled with equivalent relaxation to equal concentrations of adventitial and epithelial delivery of loop diuretics observed in newborn mouse airways, provides additional evidence that there is a direct, nonepithelial-dependent effect of furosemide on airway smooth muscle tone. We speculate that the Na-K-2Cl cotransporter is present in the human airway smooth muscle cell and plays at least a partial role in regulating airway tone.
Abbreviations
- LTD4:
-
leukotriene D4
- EC50:
-
effective concentration to produce 50% of maximal response
References
Kao LC, Warburton D, Sargent CW, Platzker ACG, Keens TG 1983 Furosemide acutely decreases airways resistance in chronic bronchopulmonary dysplasia. J Pediatr 103: 624–629
Najak ZD, Harris EM, Lazzara A Jr, Pritt AW 1983 Pulmonary effect of furosemide in preterm infants with lung disease. J Pediatr 102: 758–763
Chinn T, Franchi L, Nussbaum E 1994 Reversal of bronchial obstruction in children with mild stable asthma by aerosolized furosemide. Pediatr Pulmonol 18: 93–98
Bianco S, Vaghi A, Robuschi M, Pasargiklian M 1988 Prevention of exercise induced bronchoconstriction by inhaled furosemide. Lancet 2: 252–255
Nichol GM, Alton EWFW, Nix A, Geddes DM, Chung KF, Barnes PJ 1990 Effect of inhaled furosemide on metabisulfite- and methacholine-induced bronchoconstriction and nasal potential difference in asthmatic subjects. Am Rev Respir Dis 142: 576–580
Stevens EL, Uyehara CFT, Southgate WM, Nakamura KT 1992 Furosemide differentially relaxes airway and vascular smooth muscle in fetal, newborn, and adult guinea pigs. Am Rev Respir Dis 146: 1192–1197
Iwamoto LM, Wilson VL, Lavallee SL, Fujiwara N, Ayau EL, Nakamura KT 1996 Tachyphylaxis to furosemide in isolated airways of guinea pigs. Life Sci 59: 1015–1024
Almirall JJ, Dolman CS, Eidelman DH 1997 Furosemide-induced bronchodilation in the rat bronchus: evidence of a role for prostaglandins. Lung 175: 155–163
Rastogi A, Luayon M, Ajayi OA, Pildes RS 1994 Nebulized furosemide therapy in infants with BPD. J Pediatr 125: 976–979
Kugelman A, Durand M, Garg M 1997 Pulmonary effect of inhaled furosemide in ventilated infants with severe bronchopulmonary dysplasia. Pediatrics 99: 71–75
Corboz MR, Ballard ST, Inglis SK, Taylor AE 1997 Dilatory effect of furosemide on rat tracheal arterioles and venules. Am J Respir Crit Care Med 156: 478–483
Christ MJ, Iwamoto LM, de Silva A, Lavallee SL, Nakamura KT 1998 Amiloride-induced contraction of isolated guinea pig, mouse, and human fetal airways. Am J Physiol 274: R209–R213
Halpern W, Kelley M 1991 In vitro methodology for resistance arteries. Blood Vessels 28: 245–251
Raeburn D, Hay DWP, Farmer SG, Fedan JS 1987 Influence of cartilage on reactivity and on the effectiveness of verapamil in guinea pig isolated airway smooth muscle. J Pharmacol Exp Ther 242: 450–454
Van Neuten JM 1980 Comparison of isotonic and isometric measurements in isolated arterial tissues. In: Bevan JA, Godfraind T, Maxwell RA, Vanhoutte PM (eds) Vascular Neuroeffector Mechanisms. Raven Press, New York, pp 37–39
de Jongste JC, Van Strik R, Bonta IL, Kerrebijn KF 1985 Measurement of human small airway smooth muscle function in vitro with the bronchiolar strip preparation. J Pharmacol Methods 14: 111–118
Aranda JV, Perez J, Sitar DS, Collinge J, Portuguez-Malavasi A, Duffy B, Dupont C 1978 Pharmacokinetic disposition and protein binding of furosemide in newborn infants. J Pediatr 93: 507–511
Roberts RJ 1984 Drug Therapy in Infants: Pharmacological Principles and Clinical Experience. WB Saunders, Philadelphia, pp 226–249
Drazen JM, Gaston B, Shore SA 1995 Chemical regulation of pulmonary airway tone. Annu Rev Physiol 57: 151–170
Stenmark KR, James SL, Voelkel NF, Toews WH, Reeves JT, Murphy RC 1983 Leukotriene C4 and D4 in neonates with hypoxemia and pulmonary hypertension. N Engl J Med 309: 77–80
Mirro R, Armstead W, Leffler C 1990 Increased airway leukotriene levels in infants with severe bronchopulmonary dysplasia. Am J Dis Child 144: 160–161
Jobe AH, Ikegami M 1998 Mechanisms initiating lung injury in the preterm. Early Hum Dev 53: 81–94
Iriarte CF, Pascual R, Villanueva MM, Roman M, Cortijo J, Morcillo EJ 1990 Role of epithelium in agonist-induced contractile responses of guinea-pig trachealis: influence of the surface through which drug enters the tissue. Br J Pharmacol 101: 257–262
Sparrow MP, Mitchell HW 1991 Modulation by the epithelium of the extent of bronchial narrowing produced by substances perfused through the lumen. Br J Pharmacol 103: 1160–1164
Sparrow MP, McFawn PK, Omari TI, Mitchell HW 1992 Activation of smooth muscle in the airway wall, force production, and airway narrowing. Can J Physiol Pharmacol 70: 607–614
Galens S, Munoz NM, Rabe KF, Herrnreiter A, Mayer D, Morton B, McAllister K, Leff AR 1995 Assessment of agonist- and cell-mediated responses in airway microsections by computerized videomicrometry. Am J Physiol 268: L519–L525
Rhoden KJ, Douglas JS 1995 Evidence of Na-K-Cl cotransport in airway smooth muscle. Am J Physiol 268: L551–L557
Owen NE, Prastein ML 1985 Na/K/Cl cotransport in cultured human fibroblasts. J Biol Chem 260: 1445–1451
Lavallee SL, Iwamoto LM, Claybaugh JR, Dressel MVC, Sato AK, Nakamura KT 1997 Furosemide-induced airway relaxation in guinea pigs: Relation to Na-K-2Cl cotransporter function. Am J Physiol 273: L211–L216
Acknowledgements
The authors thank Drs. David Easa and John Claybaugh for their advcice and Naomi Fujiwara and Asoka DeSilva for their technical support. Human tissue used for this research was obtained from the Central Laboratory for Human Embryology, University of Washington, supported by National Institutes of Health Grant HD 00836 to Dr. Alan Fantel.
Author information
Authors and Affiliations
Corresponding author
Additional information
The opinions or assertions contained herein are the private views of the authors and are not to be considered as official or as reflecting the views of the Department of the Army or the Department of Defense.
Supported by Kapi'olani Health Research Institute, the US Army Health Service Command, a Leahi Fund Grant of the Hawai'i Community Foundation, and Research Centers in Minority Institutions awards, U54 RR14607 and P20 RR11091, from the National Center for Research Resources, NIH.
Rights and permissions
About this article
Cite this article
Iwamoto, L., Gries, D. & Nakamura, K. Loop Diuretics and In Vitro Relaxation of Human Fetal and Newborn Mouse Airways. Pediatr Res 50, 273–276 (2001). https://doi.org/10.1203/00006450-200108000-00018
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/00006450-200108000-00018
This article is cited by
-
Expression of Na+-K+-2Cl− Cotransporter 1 Is Epigenetically Regulated During Postnatal Development of Hypertension
American Journal of Hypertension (2011)