Abstract
Hereditary hemorrhagic telangiectasia (HHT) is a dominantly inherited vascular disorder that is heterogeneous in terms of age of onset and clinical manifestations. Endoglin is the gene mutated in HHT1, which is associated with a higher prevalence of pulmonary arteriovenous malformations than HHT2, where ALK-1 is the mutated gene. Endoglin is constitutively expressed on endothelial cells and inducible on peripheral blood activated monocytes so that protein levels can be measured by metabolic labeling and immunoprecipitation. We report the analysis of umbilical vein endothelial cells in 28 newborns from 24 families with a clinical diagnosis of HHT. Reduced levels of endoglin were observed in umbilical vein endothelial cells in 15/28 subjects and in activated monocytes of all clinically affected relatives tested, suggesting that these individuals had HHT1. No mutant protein was expressed at the cell surface in any of these cases, and a transient intracellular species was seen in samples of only two families, supporting a haploinsufficiency model. Quantitative multiplex PCR fragment analysis was established for the endoglin gene and revealed six mutations that were confirmed by automated DNA sequencing. An additional 10 mutations were identified in newborns by sequencing all exons. Of the 16 mutations, 10 were novel, three had been independently identified in related families, and three were previously known. Our data confirm that endoglin levels correlate with the presence or absence of mutation in HHT1 families, allowing the early identification of affected newborns that should be screened clinically to avoid serious complications of this disorder, such as cerebral arteriovenous malformations.
Similar content being viewed by others
Main
HHT is an autosomal dominant vascular disorder more common than previously thought, with an estimated frequency greater than 1:10 000 (1). HHT is heterogeneous between families as well as within a single family in terms of age of onset and severity of clinical manifestations. Although the first symptom of HHT in children is generally nosebleeds, several cases have been reported in which a much more severe manifestation of the disease such as CAVM or PAVM occurs in a child without prior warning (2–9). Clinical heterogeneity is in part due to genetics: the endoglin gene that maps to chromosome 9q33 is mutated in HHT1 (10), whereas the ALK-1 gene located on chromosome 12q is mutated in HHT2 (11–13). Several studies have suggested that the incidence of PAVM was higher in HHT1 than in HHT2 families (14–17). The fact that CAVM often cluster in families with a prevalence of PAVM suggests that children with HHT1 are more at risk of developing these complex vascular abnormalities from an early age. HHT2 is generally associated with a milder form of the disease, a later onset, and more cases of nonpenetrance (18).
Endoglin is constitutively expressed on all types of blood vessels, including capillaries, veins, and arteries (19, 20). It is a homodimeric transmembrane glycoprotein of Mr = 180 000 and is found at high levels at the surface of endothelial cells (19). It is recognized as an endothelial cell marker (CD105) although its expression is not restricted to that cell type (20). Endoglin is found at high levels on syncytiotrophoblasts throughout pregnancy and is also transiently expressed on extravillous trophoblasts during the first trimester of gestation (21, 22). ALK-1 is readily detected in highly vascularized tissues, being primarily expressed on endothelial cells (23, 24).
Endoglin is a component of the TGF-β1 receptor complex (25) and can modulate several responses to TGF-β1 in monocytes and in trophoblasts isolated from first trimester placenta (26, 27). More recently, endoglin was shown to bind TGF-β1 and -β3 through its association with TGF-β receptor II (28, 29). It can also bind activin, BMP-7, and BMP-2 by interacting with their respective ligand-binding receptors, suggesting that it acts as an accessory protein of the receptor complex for several growth factors of the TGF-β superfamily (28). ALK-1 is a type I receptor of this superfamily that associates with either TGF-β or activin type II receptors when cotransfected into COS-1 cells (23, 30). However, ALK-1 does not mediate signals for these ligands and, when activated, can trigger an intracellular Smad 1 pathway associated with signaling by BMP (31). Thus, both endoglin and ALK-1 are involved in the regulation of responses to ligands of the TGF-β superfamily and must play a crucial role in endothelial cell function.
The umbilical vein provides a unique source of HUVEC, which can be grown as primary cultures and tested for biochemical and functional properties. We reasoned that HUVEC from newborns with HHT1 could be tested for endoglin protein expression and predict affected individuals before mutation analysis. The analysis of peripheral blood samples is more difficult because endoglin is not present on lymphocytes or monocytes. However, adherence of monocytes to plastic for 16–24 h induces the expression of endoglin, albeit to levels 5–20 times lower than on HUVEC (32–34). This has permitted us to quantify endoglin levels on peripheral blood activated monocytes of HHT affected children and adults.
To date, 29 mutations have been reported for endoglin, most of which are unique to a particular family (10, 33, 35–38), rendering the process of mutation identification laborious. These mutations are located throughout the gene and include deletions and insertions, missense mutations, and point mutations that lead to premature stop codons (39). We previously reported for one newborn and four clinically affected individuals with known mutations that the level of endoglin at the surface of HUVEC and activated monocytes, respectively, was reduced to 50% (33). This led us to propose that haploinsufficiency was likely the underlying model for HHT1. The absence of transcripts reported for some mutations also supports the view that endoglin-mutated alleles are operating as null ones and are not affecting the normal alleles (36, 38).
In the present study, we report the analysis of 28 HUVEC from HHT families and demonstrate that quantifying the level of endoglin expressed on these cells and on activated monocytes from clinically affected relatives allows us to identify the newborns with HHT1. We also describe the conditions for efficient screening of endoglin mutations by QMPCR and automated DNA sequencing. We confirm the presence or absence of mutations in 19 newborns and identify 10 novel endoglin mutations.
METHODS
Families with HHT and their clinical evaluation.
Expectant parents from families with a clinical diagnosis of HHT who were willing to participate in the study of newborns provided informed consent for umbilical cord and placenta samples. Informed consent for blood samples was also obtained from the parents of the newborns and from all other participating individuals. All procedures were reviewed and approved by the Research Ethics Board of the Research Institute of the Hospital for Sick Children. All members of families with HHT are given a number and are referred to with the prefix H (for HHT).
A positive clinical diagnosis for HHT required any two of the following criteria: recurrent epistaxis, telangiectases elsewhere than in the nasal mucosa, evidence of autosomal inheritance, and visceral involvement such as pulmonary, cerebral or liver arteriovenous malformation (AVM). Presence of AVM in a family can only be revealed by adequate screening procedures, and an unknown status must be assumed when patients have not been screened. In the current study, a PAVM is considered present if a PaO2 is <92 mm Hg, with a positive chest radiograph and/or high-resolution computed tomogram of the chest. PAVM in these patients are confirmed by selective pulmonary angiography. A CAVM is considered present if magnetic resonance imaging (MRI) with and without gadolinium was positive for an enhancing malformation. For lesions >5 mm, cerebral angiography was performed to confirm size and angioarchitecture.
Cell culture.
Endothelial cells were derived from human umbilical veins from newborns of HHT families, obtained within 48 h of birth. HUVEC were prepared in parallel from umbilical cords obtained from normal local deliveries so that each HHT case was compared with a control HUVEC of equivalent passage. Cells were grown and maintained in culture, as previously described (19, 33). Proliferating HUVEC at subconfluence were used, as confluent monolayers down-regulate endoglin (40). In all experiments, equivalent cell densities and passage numbers were used with patient and matched controls. Liquid nitrogen stocks of all HUVEC were prepared at passages 1 or 2. Fresh cells between passages 2 and 5 were generally tested for endoglin expression. Frozen cells were also suitable for testing and were done in parallel with frozen control cells at related passages.
Acid-citrate-dextran–treated whole venous blood (20 mL) of clinically affected HHT patients and control volunteers (family members or unrelated age-matched) were fractionated by 1 ×g sedimentation through 4.5% dextran T-500/0.9% NaCl, and mononuclear cells were recovered by Ficoll-Hypaque density gradient centrifugation (32, 33). The mononuclear cells were incubated at 37°C in a 100-mm plastic tissue culture-treated dish for at least 1 h. Nonadherent lymphocytes were removed for DNA preparation and the adherent monocytes were incubated for 16–20 h in RPMI plus FBS to induce optimal expression of endoglin (34).
Antibodies.
The MAb P3D1 and P4A4 to endoglin were provided by Dr. E.A. Wayner (Seattle, WA). MAb P3D1 recognizes an epitope located between the N-terminal residue E26 and G230 of the extracellular domain of endoglin, corresponding to exons 1–5. MAb P4A4 binds to an epitope in the Y277–G331 region of the extracellular domain, encoded by exons 6 and 7 (41) (Fig. 1).
Diagram of endoglin protein, cDNA, and DNA. The mature protein is illustrated, methionine 1 (M1) coded for by the ATG initiation codon designated as bp 1–3 of the cDNA. Cysteine residues (•) and of the four potential NH2-linked glycosylation sites (tridents) are illustrated. The epitopes recognized by MAb P3D1 and P4A4 are located within the regions E26–G230 and Y277–G331, respectively. The cDNA is aligned with the protein and reveals the relative position of the 15 exons. The genomic map of endoglin is shown with exons and introns relatively to scale. The mutations analyzed in this study are designated by family number and their respective position indicated.
Metabolic labeling and immunoprecipitation.
Equivalent numbers of patient and control HUVEC at subconfluence (80–90%), or in separate experiments of peripheral blood activated monocytes from patient and control, were metabolically labeled for the optimal time of 3.5 h with [35S]-methionine and solubilized in 1% Triton X-100 plus a cocktail of inhibitors and immunoprecipitated with saturating amounts of MAb (control nonimmune IgG, 2 μg; P3D1, 4 μg; P4A4, 1.6 μg) as described previously (33). Immune complexes were collected with BSA adsorbed gamma-bind G Sepharose (Pharmacia), washed with RIPA (0.05 M Tris-HCl, pH 7.4, 0.01 M NaCl, 1 mM EDTA, 0.1% SDS, 0.5% Triton X-100, 1% deoxycholate) and TNTE (0.05 M Tris-HCl, pH 7.4, 0.01 M NaCl, 0.1% Triton X-100, 1 mM EDTA) buffers, eluted by heating at >95°C for 2 min in nonreducing solution (60 mM Tris-HCl, pH 6.8, 2% SDS, 10% glycerol, 0.05% bromophenol blue) and subsequently reduced with 50 mM DTT where indicated. To quantitate endoglin expression and correct for differences in yield between samples and respective matched controls, incorporation into 10% TCA precipitable material (collected on glass-fiber filters) was measured in aliquots of total lysates. Equivalent cpm were fractionated by SDS-PAGE (4–12% gradient gels, Novex); gels were fixed, dried, and exposed to BioMax MS films in BioMax TransScreen LE cassettes. Radioactivity in the bands corresponding to the fully processed form of endoglin (E) and its metabolic intracellular precursor (P) was quantitated using a PhosphorImager and Image Quant software. The patient to control pixel value ratios of E and P were calculated for each immunoprecipitate, run under reduced and nonreduced conditions, and the mean ± SD was determined from at least four values. The most relevant parameter in terms of functional endoglin level is the ratio of E values, which corresponds to the level of fully processed glycoprotein expressed at the cell surface.
DNA isolation.
Genomic DNA was extracted from placenta, HUVEC, and blood lymphocytes by using DNAZOL or Puregene (Gentra Systems, Inc.). Purity and quality of the DNA and accurate estimation of the concentration are critical for QMPCR.
QMPCR fragment analysis.
All 15 exons of endoglin (Fig. 1) were amplified in five PCR reactions using one selected Cy 5.5 fluorescent conjugated primer for each exon. Reactions (25 μL) contained Taq polymerase, 5% DMSO, 250 μM of each dNTP (2′ deoxynucleoside 5′-triphosphate), 2–2.5 mM MgCl2, and optimized primer concentrations ranging from 80 to 800 nM. Quantitation was achieved by varying number of cycles, annealing T° and using 150 ng of genomic DNA. The amplification of a fragment (329 bp or 282 bp) derived from c4 gene on chromosome 15 was included as internal standard in each of the reactions. The multiplex PCR pools and fragment sizes (in bp) were as follows: reaction 1, exon 9b (149), exon 4 (283), c4 standard (329), exon 2 (363), exon 6 (389), and exon 11 (426); reaction 2, exon 12 (154), c4 standard (282), exon 10 (304), exon 1 (314), and exon 8 (373); reaction 3, exon 9a (222), exon 5 (238), exon 13 (255), and c4 standard (282); reaction 4, exon 14 (269), exon 7 (289), and c4 standard (329); reaction 5, exon 3 (251) and c4 standard (329).
Thermocycling was performed using DNAEngine (MJ Research) and a ramping time of 1°C/s. Initial denaturation is at 94°C for 2 min, followed by 18–22 cycles of denaturation at 94°C for 30 s, annealing at 51–55°C for 35 s, extension at 65°C for 150 s, and a final extension at 65°C for 4 min. QMPCR products were run on MicroGene Blaster sequencer [Visible Genetics, Inc. (VGI), Toronto, Ontario, Canada] at 1300 V at 54°C for 30–40 min. The data were analyzed using GeneObjects DNA analysis software (VGI). The ratio of the peak area for each endoglin exon was calculated relative to that of the c4 internal standard for each patient sample and compared with the normal two-copy control DNA sample.
Exon sequencing protocol.
The exons to be sequenced were first amplified with nonlabeled primers identical to those used in QMPCR and under standard conditions (1.5 mM MgCl2, 200 μM dNTP, 0.3 μM primer, 300 ng genomic DNA, and 2 U Taq polymerase in 25 μL). Annealing temperatures were determined experimentally. Thermocycling conditions were initial denaturation at 94°C for 2 min, denaturation for 33 cycles at 94°C for 30 s, annealing at 52–64°C for 30 s, extension at 70°C for 60 s, and a final extension at 70°C for 4 min. The PCR product was suitable for sequencing when it appeared as a single band with an intensity equivalent to 20–30 ng. Templates were sequenced using VGI sequencing buffer, 9.6 U of Thermo Sequenase (Amersham), 3 pmol of Cy 5.5 labeled primer (VGI), and termination mixes A,C,G,T (Amersham). Cycling conditions were identical to those used for template amplification. Products were run on a MicroGene Blaster sequencer at 1300 V at 54°C for 30–40 min. Sequences were automatically analyzed using the Gene Objects DNA analysis software (VGI).
RESULTS
Quantitation of endoglin levels expressed on HUVEC of HHT andcontrol newborns.
HHT is a dominantly inherited disorder to the extent that each child has a 50% probability of carrying the disease. As only 29 mutations have now been reported for HHT1 and 18 for HHT2 [reviewed by (39)], the genotype of participating families is generally unknown. Our first step in the molecular identification of newborns with HHT1 is to quantify levels of endoglin on their HUVEC. The umbilical vein provides an excellent source of endothelial cells, expressing high levels of endoglin that can be quantified by metabolic labeling and immunoprecipitation. We report the analysis of a large number of HUVEC from families with a clinical diagnosis of HHT and confirm their HHT1 genotype.
Figure 2 illustrates the specificity of endoglin detection at the protein level. As HUVEC primary cultures gradually differentiate in vitro, early and equivalent passages of control and experimental cells were used in all experiments. Figure 2A illustrates that both MAb P3D1 and P4A4 specifically immunoprecipitate endoglin, whereas the control nonimmune IgG was completely negative. Endoglin was resolved as an intermediate precursor (P, 80 kD monomer; 140 kD homodimer) and a fully processed surface glycoprotein (E, 90 kD monomer; 160 kD homodimer) in patient H129 and control HUVEC. No mutant protein was detectable in H129 HUVEC, but fully processed endoglin E was seen at reduced levels relative to control, estimated at 45 ± 6% (Table 1).
Endoglin levels in HUVEC measured by metabolic labeling and immunoprecipitation. HUVEC of newborns from clinically diagnosed HHT families (H) and control (C) newborns were tested by metabolic labeling and immunoprecipitation. Samples were fractionated by SDS-PAGE (4–12% gradients) under nonreducing conditions (A, left panel, and B) or reducing conditions (B, right panel). (A) Endoglin was specifically immunoprecipitated as a precursor (P) and as a fully glycosylated surface glycoprotein (E) from H129 and C1 HUVEC with MAb P3D1 and P4A4 but not with nonimmune IgG. Half levels of normal E and no mutant protein were seen in H129, relative to control. (B) HUVEC derived from two independent segments of an umbilical cord (H136A and H136B) expressed reduced levels of endoglin relative to two independent controls (C2 and C3). Fraternal twins H219 and H220, also analyzed in the same experiment, showed reduced and normal levels, respectively. Data are shown for MAb P3D1.
To demonstrate that levels of endoglin on HUVEC could be measured reproducibly, two separate pieces of umbilical cord from the H136 newborn were processed independently. Figure 2B reveals that endothelial cells derived from both segments expressed indistinguishable levels of endoglin that were reduced (49 ± 10%) relative to two independent controls. HUVEC derived from fraternal twins H219 and H220 were also analyzed in the same experiment and showed reduced (37 ± 8%) and normal (91 ± 22%) levels, respectively, suggesting that only one twin was affected (Tables 1 and 2). A total of 65 umbilical cords from newborns of HHT families have been processed to date and an even higher number of control samples. In 50 experiments, HHT HUVEC were compared with two or three independent normal controls. With 20 of the HHT cases, experiments were repeated two to five times and gave similar results.
Analysis of endoglin expression in 24 families with HHT1.
The second step in the molecular analysis of newborns from HHT families is to determine the genotype of the clinically affected parent. This is achieved by measuring the level of endoglin expressed on peripheral blood monocytes, activated by adherence to plastic, and in vitro culture for 16–24 h. Levels of endoglin observed on activated monocytes of the clinically affected parent are compared with those of the spouse or of a normal age-matched adult control according to conditions optimized previously (33, 34).
Figure 3 illustrates the analysis of four families with HHT1. In families 96 and 97, H315 and H317 HUVEC expressed reduced levels of endoglin relative to the corresponding control HUVEC. Their respective clinically affected father (H314) and mother (H316) showed low endoglin levels relative to their spouse, suggesting an HHT1 genotype for the family and affected babies (Fig. 3 and Table 1). Two cases of normal newborns and their affected parents are also shown. In families 87 and 37, HUVEC from newborns H285 and H116 had normal levels of endoglin relative to control. Activated monocytes of the clinically affected mothers H284 and H115, respectively, showed reduced endoglin levels relative to their spouse and indicative of an HHT1 genotype for these two families (Fig. 3 and Table 2).
Analysis of endoglin expression in four HHT1 families. HUVEC of newborns from clinically diagnosed HHT families (H) and control (C) were immunoprecipitated with MAb P3D1 and fractionated under nonreduced conditions. Peripheral blood activated monocytes obtained from the clinically affected parent and nonaffected spouse (serving as control) were also analyzed similarly, as described in “Methods.” In families 96 and 97, H315 and H317 HUVEC express reduced levels of endoglin (E) relative to HUVEC controls run in the same experiment. Activated monocytes from clinically affected parents H314 and H316, respectively, showed reduced endoglin levels relative to their spouse. In families 87 and 37, H285 and H116 HUVEC express normal levels of endoglin relative to HUVEC controls, whereas activated monocytes of the clinically affected parents H284 and H115, respectively, showed reduced endoglin levels relative to their spouse.
The analysis of 28 newborn cases is summarized in Tables 1 and 2. These babies belong to 24 families of presumed HHT1 type as defined by clinically affected family members expressing reduced levels of endoglin, ranging from 14 to 67% of the levels measured on concurrently run normal samples. Fifteen cases of HUVEC clearly showed reduced levels of endoglin ranging from 26 to 61% (Table 1), whereas 13 showed normal levels ranging from 87 to 121% of control samples (Table 2). The analysis of samples from family 70 revealed that although the grandmother of the newborn was affected, as shown by clinical manifestations that included a PAVM and by an endoglin level of 39 ± 5%, the father who had an uncertain clinical diagnosis was likely not affected as his endoglin level was within the normal range (83 ± 10%).
Of the 24 families analyzed, only two showed a detectable mutated endoglin protein, namely families 9 and 85, as indicated in Table 3. In the case of family 9, a transient species missing the 47 amino acids encoded by exon 3 was detected only by metabolic labeling and not by surface labeling and Western blot analysis despite the presence of an intact transmembrane region (33). It was observed as an intracellular protein (130 kD dimer; 70 kD monomer) in HUVEC of H19 newborn and his affected father. In family 85, a missense mutation leads to a cysteine to arginine substitution at residue 53 and to expression of a transient species retained intracellularly and comigrating with the normal endoglin precursor (P; 80 kd monomer) in the affected H319 newborn (34). In all other cases presented in Tables 1 and 2, no metabolically labeled mutant protein was detectable in the endoglin immunoprecipitates from HUVEC or activated monocytes, suggesting that if expressed at all, these proteins were degraded inside the cells.
Analysis of endoglin mutations by QMPCR and confirmation by exonsequencing.
We established the conditions for QMPCR fragment analysis for all exons of endoglin (Fig. 4). Primers were first selected that could amplify each exon as a single and clearly resolved PCR product on agarose gels. Exons in combination were then amplified using pairs of primers, each containing one selectively labeled with the Cy 5.5 fluorescent dye. These mixtures were fractionated on polyacrylamide gels by using the MicroGene Blaster sequencer and the size of each peak assessed relative to internal size standards. Optimization of the mixed QMPCR reactions was achieved by varying primer and MgCl2 concentrations and annealing temperatures. The presence of 5% DMSO was shown to stabilize the relative amplification of exons in various mixtures. A quantitative range of amplification was achieved by varying the number of cycles and testing different amounts of DNA. The area under the peak is calculated and estimated for each exon relative to the c4 internal control included in each PCR reaction and which represents an independently amplified gene. The resolution of all exons of endoglin was achieved using four mixed reactions, whereas exon 3 was amplified singly because the only primers available (36) were quite different from those of other exons (Fig. 4). These primers will be changed to accommodate coamplification of the promoter region now that the sequence is available (42, 43).
Amplification of genomic endoglin by QMPCR. Conditions were optimized to coamplify the 15 exons of the endoglin gene in five quantitative reactions, so that peak height corresponds to the DNA copy number. The c4 gene, derived from chromosome 15, is amplified in each reaction and serves as an internal control for quantitation; it is seen as a fragment of 282 bp in reactions 1, 4, and 5 or as a fragment of 329 bp in reactions 2 and 3. Exon numbers are indicated below the peaks. The fluorescent PCR products are size fractionated on a polyacrylamide gel using the VGI Microgene Blaster sequencer.
Six mutations were found by screening samples from 24 families by QMPCR, and examples are illustrated in Figures 5,6,and 7.
Identification of a 16-bp insertion in exon 7 of endoglin using QMPCR reaction 4. DNA from HUVEC and placenta of a newborn (H49) from HHT family 12 and from blood of clinically affected mother (H39), grandmother (H94), and control were analyzed by QMPCR. Reaction 4 revealed an additional peak of higher mobility (7′) for exon 7, whereas the peaks for exon 14 and internal standard c4 were unchanged in child and affected relatives. This peak corresponds to a PCR fragment with a 16-bp insertion.
Detection of two mutations in newborns of HHT families using QMPCR reaction 3. DNA from placenta of newborns and parents from HHT families 17 and 52 were analyzed by QMPCR. (A) An insertion of 4 bp in exon 5 was detected in H51 baby and H52 affected mother (fragment 5′) but not in control father H53. (B) Partial sequences of exon 5 (obtained with reverse primer) illustrate the GACA insertion at position 574. (C) A deletion of 1 bp in exon 9a was observed in newborn H152 and affected mother H151 (seen as doublet peak 9a′) but not in the nonaffected father H322. (D) Partial sequences of exon 9a (obtained with forward primer) show a G deletion at position 1186. (S = G or C;M = A or C;R =A or G;K = G or T;Y = C or T;W = A or T).
Absence of mutation in a newborn of HHT family 37 revealed by QMPCR reaction 2. DNA from newborn H116, affected mother H115, and control father H305 was analyzed by QMPCR. (A) A deletion of 2 bp was detected in exon 8 in affected mother (resolved as a double peak 8′) but was absent in newborn and father. (B) Partial sequences of exon 8 (obtained with forward primer) reveal a TG deletion at position 1089 in affected patient H115.
Family 12.
When samples from family 12 were subjected to QMPCR reaction 4, which amplifies exons 14 and 7, an additional peak estimated at 305 bp was seen migrating ahead of the normal exon 7 product of 289 bp (Fig. 5). This extra PCR fragment was observed in DNA prepared from HUVEC and placenta of the newborn and in blood samples of the clinically affected mother and grandmother, the latter having a PAVM. DNA from a nonaffected individual served as the normal control in the study (Fig. 5). These data suggested that the newborn was affected and carried a mutation consisting of a 16-bp insertion in exon 7, as did his mother and grandmother. Sequencing revealed a complex mutation, 3 bp within exon 7, at position 819 (Table 3). In fact, 8 bp were deleted and replaced by 24 bp, which represented a duplication of bp 834–857 of the normal sequence, with two introduced point mutations, G836C and G 840A. The net effect is a 16-bp insertion resulting in a frameshift at bp 820 and creating a stop downstream. The normal protein sequence terminates at threonine 273 and, if translated, would be followed by 64 aberrant amino acids before truncation. No other mutation was revealed by sequencing all exons of endoglin in the clinically affected patient H94.
Family 17.
The QMPCR reaction 3, which amplifies exon 9a, 5, and 13, revealed a novel mutation in exon 5 in the DNA samples of newborn H51 and his clinically affected mother H52 who had a PAVM embolized during pregnancy. The mutation yielded a doublet peak with an estimated 242-bp PCR fragment for the mutant allele and the normal PCR fragment of 238 bp. DNA of the father revealed a single peak at 238 bp with twice the intensity of that seen in the heterozygotes (Fig. 6A). Sequencing of exon 5 confirmed the presence of a GACA insertion (Fig. 6B). This mutation at position 574 of the endoglin cDNA causes a frameshift; the normal protein sequence terminates at threonine 193 and is followed by 139 unusual residues before truncation.
Family 52.
A mutation in exon 9a was also revealed in family 52 by QMPCR reaction 3. This family is severely affected with several members having PAVM and CAVM, including patient H151, the mother of newborn H152. DNA from both individuals showed a peak at the expected size of 222 bp but with a shoulder suggesting a 1-bp deletion (Fig. 6C). The control father showed a single sharp peak of 222 bp as expected for the normal PCR fragment amplified from exon 9a. Sequencing of this exon demonstrated a G deletion at bp 1186 (Fig. 6D). The normal protein is interrupted at aspartic acid 395 and is truncated after 24 aberrant residues (Table 3).
Family 37.
Newborn H116 from family 37 showed normal levels of HUVEC endoglin, whereas his clinically affected mother H115, who had a PAVM embolized during this pregnancy and a CAVM treated a few months later, had 33 ± 6% endoglin on her activated monocytes. Her DNA was subjected to QMPCR analysis. Reaction 2, which amplifies exons 12, 10, 1, and 8, revealed a doublet peak for the PCR product of exon 8, normally of 373 bp (Fig. 7A). Fractionation of DNA from the newborn and his father revealed the normal expected single peak profile for all exons. Sequencing of exon 8 confirmed the presence of a 2-bp deletion in DNA of the clinically affected mother and the absence of this mutation in the newborn (Fig. 7B). This TG deletion creates a frameshift at position 1089 of the cDNA that leads to interruption of the normal protein sequence at cysteine 363. An additional 30 amino acids would be translated before truncation (Table 3).
Family 66.
QMPCR reaction 2 also revealed a deletion of 11 bp in the PCR product of exon 12 in family 66. In this case, the newborn H217 and his mother were unaffected so that the respective exon profiles were normal in all mixtures. The clinically affected father had a CAVM and showed 47 ± 20% endoglin on his activated monocytes. Amplification of his DNA revealed two peaks for the PCR fragment of exon 12, corresponding to the mutant allele (143 bp) and the normal allele (154 bp), respectively (data not shown). Sequencing of this exon confirmed the 11-bp deletion that causes a frameshift at bp 1689. The normal sequence terminates at aspartic acid 562, followed by 11 residues before truncation (Table 3).
Family 92.
The QMPCR reaction 1 identified a mutation in exon 11 in family 92 in which PAVM or CAVM have been observed in several individuals. Exon 11 yields a relatively large PCR product (426 bp) so that the 2-bp deletion gave a poorly resolved but discernible doublet for the affected newborn H304 and his clinically affected mother H303 relative to the control father (data not shown). The GC deletion at position 1553 confirmed that both child and mother were affected. This mutation creates a frameshift so that the normal protein ends with valine 517 and is followed by eight aberrant residues (Table 3). This mutation has been previously reported in a family seemingly unrelated to family 92 (10). However, these families are not too distant geographically and may have arisen from a common ancestor.
Identification of additional mutations in endoglin by sequencing ofall exons.
Families in which clinically affected individuals and/or newborns showed reduced levels of endoglin in their peripheral blood activated monocytes and HUVEC, respectively, and for which no mutation could be found by QMPCR screening were subjected to exon sequencing. Five new mutations were revealed as well as two previously identified in independent studies (Table 3). Newborns from two families with known mutations were also studied.
Family 70.
Newborn H246 showed normal HUVEC endoglin levels. The grandmother H243, who had a PAVM, expressed 45 ± 7% endoglin on her activated monocytes, whereas her son had an unknown HHT status and 83 ± 10% endoglin. Analysis of H243 DNA revealed a nonsense mutation, a C277 to T substitution that leads to a stop codon and a protein truncated at arginine 93. This mutation was not found in the newborn or his father, confirming that they were unaffected.
Family 3.
Newborn H6 is from a family with a recurrent history of CAVM and PAVM, his own mother having a PAVM. The levels of endoglin in H6 HUVEC in culture were normal, whereas those on activated monocytes of an affected uncle and grandfather were reduced. Sequencing of DNA from these affected adults revealed an acceptor splice site mutation in the 3′ end of intron VI, an (a to t) intronic substitution at position −2 (relative to exon 7). This mutation could cause skipping of exon 6, leading to a frameshift and truncation of the protein. The H6 DNA did not show such a mutation, indicating that this newborn did not have HHT1.
Family 96.
Newborn H315 showed reduced endoglin as did his father who is severely affected, having both PAVM and CAVM. The DNA samples from child and father showed a donor splice site mutation at the 5′ end of intron IXb, an intronic substitution (t to a) at position +2 relative to exon 9b. This mutation could lead to skipping of exon 9b or to an unstable mRNA. As exon 9b is in frame and no mutant protein was detected by metabolic labeling, the latter possibility is more likely.
Family 18.
Newborn H56 and his mother H55 showed low levels of endoglin and were from a family with a high incidence of PAVM and CAVM. Sequencing of exon 10 in newborn and mother revealed a complex mutation that deletes AGA and inserts GT at position 1414, leading to termination of the normal sequence at glutamic acid 471, followed by 18 aberrant amino acids. Mutation in this family has been independently identified by W.W. Chan and R.P. Lifton (unpublished data).
Family 44.
Newborn H129 expressed low endoglin levels as did his father who had several small PAVM and CAVM (Table 1). When the DNA samples were sequenced, a 1-bp insertion (A) at position 1470 in exon 11 caused a frameshift that led to a protein with a normal sequence terminating at leucine 490 followed by 9 abnormal amino acids. This mutation was absent from the mother's sample and confirmed that both child and father were affected.
Family 74.
Newborn H259 had 56% endoglin on his HUVEC and the corresponding DNA was sequenced. A blood sample from the severally affected mother (diffuse PAVM) could not be obtained. A substitution (T to C) in the ATG initiation codon was found while sequencing exon 1. Such a mutation, which is considered a classical null allele as no protein can be translated, had been reported previously (38). We established that newborn H259 was in fact related to this independently described family, thus allowing us to confirm that the child had the same mutation as his affected relatives.
Family 8.
Three newborns from this family with a high frequency of PAVM and CAVM were involved in the current study. Newborn H136 and his mother H135 had low levels of endoglin. Newborns H18 and H232 had normal levels of endoglin, whereas their father and sister had low levels (Table 1). Sequencing of DNA from several affected members of this family confirmed a disease-associated mutation in exon 5. A nonsense mutation created by a C587T substitution converts codon 196 into a stop codon. The mutation was present in newborn H136 but absent from newborns H18 and H232. Such a mutation had been reported previously (35), and we were able to confirm that the newborns were related to the previously studied individuals.
Other families.
The mutation from family 21 was reported previously (35) as a 1-bp insertion (A) at position 1112 in exon 8 giving rise to a frameshift and a normal sequence terminating at leucine 370 plus 31 amino acids before truncation. We had also previously reported that patient H65 had low endoglin on his activated monocytes (33). We now report that his child H344 has reduced endoglin on his HUVEC and also carries the disease-related mutation. A missense mutation in exon 2 has been reported for family 85 (38). We now demonstrate that two newborn second cousins from this family are respectively affected (H319) and nonaffected (H321). Both of their mothers were shown to carry the mutation. A T157C substitution leads to cysteine 53 to arginine conversion.
Four mutations were unresolved after QMPCR and sequencing of all exons, those of families 20, 26, 67, and 75. These mutations are likely located outside of the coding region such as in the promoter region or in the 3′ end of the gene. In the case of families 45, 86, 87, and 97, no mutations were observed by QMPCR and exons are currently being subjected to sequencing.
Polymorphisms in endoglin.
Whereas all exons of endoglin were sequenced for members of 20 families, some previously reported polymorphisms (36) were observed. Two silent nucleotide variations were seen: a G207A substitution in exon 2 and a C1029T substitution in exon 8 that do not alter the leucine and threonine codons, respectively. Both polymorphisms were observed in two independent families.
DISCUSSION
It is important to identify children with HHT and particularly those of HHT1 type as they are more at risk of developing complex vascular abnormalities such as PAVM and CAVM at an early age. Our preliminary studies of one HUVEC and four blood samples had showed that HHT1 was associated with reduced levels of endoglin (33). This suggested that measuring the level of endoglin expressed on endothelial cells isolated from the umbilical vein should allow us to quickly identify newborns with HHT1. In the current study, we report the analysis of 28 newborns from 24 families with a clinical diagnosis of HHT. Fifteen of the HUVEC samples showed reduced levels of endoglin ranging from 26 to 61% of control, corresponding to expression of only the normal allele and indicating that these newborns were affected. The other 13 HUVEC had normal levels of endoglin ranging from 87 to 121% and were thus nonaffected. All of these 24 families were of HHT1 genotype as suggested by the analysis of peripheral blood activated monocytes of clinically affected members, which showed reduced levels of endoglin ranging from 16 to 67% of nonaffected controls. Mutations have now been confirmed in 16 of these families.
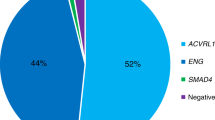
To date, we have analyzed samples from 61 newborns from HHT families by using both umbilical cord and placenta, so that if cultures of endothelial cells cannot be established, the status of the baby can be determined using placental DNA. By a combination of protein and mutation analysis, 41 of these newborns were shown to belong to HHT1 families, 21 being affected and 20 being normal. When samples from both newborns and clinically affected relatives have normal levels of endoglin, we assume an HHT2 genotype for the family and proceed to ALK-1 mutation analysis. We have observed 14 such cases and confirmed the presence or absence of an ALK-1 mutation in seven of the newborns (Abdalla et al., manuscript in preparation). The other cases with normal endoglin levels are from families of currently unknown genotype.
Quantifying the level of endoglin is a rapid and useful way to screen potential HHT1 patients before mutation identification. The targeted population for diagnostic purposes includes families with an established or suspected clinical diagnosis of HHT. The endoglin protein test is particularly suited to the analysis of HUVEC, as these cells constitutively express high levels of endoglin and the established primary cultures can be retested several times. There is also no overlap between the affected range (26–64%) and the nonaffected one (83–128%) for all HUVEC analyzed to date. The test is definitely faster than mutation analysis once methods for culturing HUVEC, metabolic labeling, and immunoprecipitation have been established. Results are generally available 2–3 wk after birth of the newborn. The protein measurements are currently more sensitive than genomic DNA analysis as only 16 mutations were found after QMPCR fragment analysis and sequencing of all exons in 20 families with reduced levels of endoglin. In those 16 families, there was complete correlation between presence or absence of a mutation and reduced or normal levels of endoglin. However, a larger number of HUVEC must be processed to establish the validity of this diagnostic method.
The analysis of peripheral blood samples is more difficult than that of HUVEC as activated monocytes generated by adherence of mononuclear cells to plastic for 16–24 h are the only readily available cells in children and adults that express endoglin (32–34). Activated monocytes also express 5–20 times less endoglin than HUVEC, and the levels could be modulated by hormones and/or growth factors such as TGF-β itself (26). Nevertheless, we have observed reduced levels of endoglin (<70%) in affected members from 67/100 families tested. An HHT1 genotype has been ascribed to 27 of these families by endoglin mutation analysis. Among the families with normal levels of endoglin (>80%), seven have been confirmed to be of HHT2 type as revealed by ALK-1 mutations. Five percent of individuals tested fell between 70 and 80%, rendering prediction of their genotype impossible from endoglin level. Assuming that the standard of reference is mutation identification, a much larger number of samples must be analyzed to establish the true sensitivity and specificity of a protein diagnostic test for both newborns, children, and adults.
Individuals from HHT families are prescreened by protein analysis. DNA samples from those with low endoglin levels are targeted to HHT1 mutation analysis, whereas those with normal endoglin levels are first analyzed for an HHT2 mutation. We cannot rule out the possibility that mutations in key functional residues of endoglin may lead to a nonfunctional protein that could still be expressed at the cell surface. Members of these families would then express normal levels of endoglin and would not be identified as having HHT1 by the protein test, thus decreasing its sensitivity. Consequently, to determine the frequency of such mutations, DNA from affected individuals with normal levels of endoglin will be sequenced for endoglin if an ALK-1 mutation is not found. As every HHT family appears to have a different mutation, our stratified approach is designed to accelerate the laborious process of mutation identification.
No mutant endoglin proteins were detected in HUVEC and activated monocytes from 22/24 families with HHT1 presented in this study. The only two mutant proteins detected were expressed as transient intracellular species (Table 3) (33, 34). In fact, mutant proteins are not expressed at the cell surface in a total of 67 families analyzed to date, and only very few are even expressed intracellularly, supporting a haploinsufficiency model for HHT1. This implies that reduction in the level of surface endoglin rather than interference by a mutated protein is the underlying cause of this disorder.
To establish a correlation between the presence of an endoglin mutation and reduced levels of the protein, we set up QMPCR fragment analysis (Fig. 4). Six mutations were identified in the initial QMPCR screen of 24 families, most of which were deletions and insertions ranging from 1 to 16 bp in size (Table 3). When an exon is small, such as exon 9a, a 1-bp deletion can be observed; however, a 1-bp insertion in the large exon 11 was not detected (Table 3). The endoglin QMPCR was optimized so that it can also distinguish copy number and identify intronic mutations that lead to duplication or deletion of one or several exons (44). The advantage of detecting a mutation by QMPCR (45) is that only one exon rather than 15 needs to be sequenced. So despite the fact that only 25% of endoglin mutations may be found by this technique, it is still timesaving and useful when screening large numbers of samples. We report 10 novel mutations that include four deletions, three insertions, two splice mutations, and one nonsense mutation (Fig. 1 and Table 3). These are distributed throughout the gene and include an 11-bp deletion in exon 12 for which no mutation had been described previously (39). The complex and lengthy task of identifying each mutation despite the use of a technology optimized for such a purpose leads us to suggest that a simpler diagnosis for HHT1, based on assessing endoglin protein levels in affected or suspected HHT families, will be developed in the next few years. It is, however, necessary to confirm that the correlation between reduced levels of endoglin and the presence of a mutation is true in most if not all HHT1 families.
The prevalence of PAVM in the families enrolled in the present study is remarkably high with 21/24 having experienced these complications. CAVM were also reported in 11 of the families. Several studies have suggested that PAVM are more frequent in HHT1 than HHT2 families (14–17) and that CAVM are often observed in the same families. It is currently estimated that 20% of patients with HHT have PAVM, whereas cerebral involvement is generally underdiagnosed and believed to affect 5–10% of HHT patients. Although the prevalence of these AVM would definitely be higher if considering only HHT1 families, it must be noted that parents enrolled in our study were often themselves or their relatives were treated for PAVM and CAVM. However, newborns from these families are the ones most at risk of developing these complex vascular abnormalities from an early age. HHT2 is associated with a milder form of the disease, a later onset, and more cases of nonpenetrance (18); thus, children from these families would have a lesser risk of developing severe complications.
After a molecular diagnosis for HHT has been established in a newborn, clinical screening for CAVM/PAVM should be considered. Although there is lack of consensus among clinicians as to whether newborns should be screened, we strongly recommend unenhanced brain MRI of infants with HHT1, particularly those from families with a history of CAVM or unexplained cerebral hemorrhage. Children from several families included in the current study have died or were permanently disabled from intracerebral hemorrhage associated with CAVM. The discovery of a CAVM in an infant would lead to close follow up to monitor its growth and to treat if the CAVM were large (46). Screening for PAVM in infants is less problematic. Recently, Faughnan et al. (manuscript in preparation) reviewed 28 cases of children with PAVM and found that among children <12 y old, only those who were cyanotic and had large PAVM or diffuse involvement sustained a stroke or brain abscess. On the basis of these data, we advocate monitoring by pulse oximetry up to age 12 and further investigation and treatment for younger children who are cyanotic or experiencing growth failure. A molecular diagnosis for HHT1 will thus allow us to identify newborns and children with the disease and particularly those that should be monitored clinically and screened by brain MRI to avoid the serious complications of this disorder.
Abbreviations
- HHT:
-
hereditary hemorrhagic telangiectasia
- HHT1:
-
hereditary hemorrhagic telangiectasia type 1
- HHT2:
-
hereditary hemorrhagic telangiectasia type 2
- HUVEC:
-
human umbilical vein endothelial cells
- QMPCR:
-
quantitative multiplex polymerase chain reaction
- PAVM:
-
pulmonary arteriovenous malformation
- CAVM:
-
cerebral arteriovenous malformation
- TGF-β:
-
transforming growth factor β
- ALK-1:
-
activin-like kinase
- BMP:
-
bone morphogenetic proteins
References
Guttmacher AE, Marchuk DA, White RIJ 1995 Hereditary hemorrhagic telangiectasia. N Engl J Med 333: 918–924.
Hoffman HJ, Mohr G, Kusunoki T 1976 Multiple arteriovenous malformations of spinal cord and brain in a child. Childs Brain 2: 317–324.
Roy C, Noseda G, Arzimanoglou A, Harpey JP, Binet MH, Vaur C, Caille B 1990 Maladie de Rendu-Osler révélée par la rupture d'un anévrisme artériel cérébral chez un nourrisson. Arch Fr Pediatr 47: 741–742.
Belzic I, Yaseen H, Voirin J, Bonte JB, Laloum D 1992 Malformations artério-veineuses cérébrales dans une probable forme familiale de Rendu-Osler. Ann Pediatr 39: 301–304.
John PR 1992 Early childhood presentation of neurovascular disease in hereditary haemorrhagic telangiectasia. Pediatr Radiol 22: 140–141.
Kadoya C, Momota Y, Ikegami Y, Urasaki E, Wada SI, Yokota A 1993 Central nervous system malformations with hereditary hemorrhagic telangiectasia: report of a family with three cases. Surg Neurol 42: 234–239.
Kikuchi K, Kowada M, Sasajima H 1994 Vascular malformations of the brain in hereditary hemorrhagic telangiectasia (Rendu-Osler-Weber disease). Surg Neurol 41: 374–380.
Allen SW, Whitfield JM, Clarke DR, Sujansky E, Wiggins JW 1993 Pulmonary arteriovenous malformations in the newborn: a familial case. Pediatr Cardiol 14: 58–61.
Ribet M, Denibal F 1991 Malformations artério-veineuses pulmonaires. Chirurgie 117: 533–541.
McAllister KA, Grogg KM, Johnson DW, Gallione CJ, Baldwin MA, Jackson CE, Helmbold EA, Markel DS, McKinnon WC, Murrell J, McCormick MK, Pericak-Vance MA, Heutink P, Oostra BA, Haitjema T, Westerman CJJ, Porteus ME, Guttmacher AE, Letarte M, Marchuk DA 1994 Endoglin, a TGF-β binding protein of endothelial cells is the gene for hereditary haemorrhagic telangiectasia type 1. Nat Genet 8: 345–351.
Vincent P, Plauchu H, Hazan J, Fauré S, Weissenbach J, Godet J 1995 A third locus for hereditary haemorrhagic telangectasia maps to chromosome 12q. Hum Mol Genet 4: 945–949.
Johnson DW, Berg JN, Gallione CJ, McAllister KA, Warner JP, Helmbold EA, Markel DS, Jackson CE, Porteus MEM, Marchuk DA 1995 A second locus for hereditary hemorrhagic telangiectasia maps to chromosome 12. Genet Res 5: 21–28.
Berg JN, Gallione CJ, Stenzel TT, Johnson DW, Allen WP, Schwartz CE, Jackson CE, Porteous MEM, Marchuk DA 1997 The activin receptor-like kinase 1 gene: genetic structure and mutations in hereditary hemorrhagic telangiectasia type 2. Am J Hum Genet 6: 60–67.
Heutink P, Haitjema T, Breedveld GJ, Janssen B, Sandkuijl LA, Bontekoe CJM, Westerman CJJ, Oostra BA 1994 Linkage of hereditary haemorrhagic telangiectasia to chromosome 9q34 and evidence for locus heterogeneity. J Med Genet 31: 933–936.
McAllister KA, Lennon F, Bowles-Biesecker B, McKinnon WC, Helmbold EA, Markel DS, Jackson CE, Guttmacher AE, Pericak-Vance MA, Marchuk DA 1994 Genetic heterogeneity in hereditary haemorrhagic telangiectasia: possible correlation with clinical phenotype. J Med Genet 31: 927–932.
Porteous MEM, Curtis A, Williams O, Marchuk D, Bhattacharya SS, Burn J 1994 Genetic heterogeneity in hereditary haemorrhagic telangiectasia. J Med Genet 31: 925–926.
Berg JN, Guttmacher AE, Marchuk DA, Porteous MEM 1996 Clinical heterogeneity in hereditary haemorrhagic telangiectasia: are pulmonary arteriovenous malformations more common in families linked to endoglin?. J Med Genet 33: 256–257.
Johnson DW, Berg JN, Baldwin MA, Gallione CJ, Marondel I, Yoon SJ, Stenzel TT, Speer M, Pericak-Vance MA, Diamond A, Guttmacher AE, Jackson CE, Attisano L, Kucherlapati R, Porteus MEM, Marchuk DA 1996 Mutations in the activin receptor-like kinase 1 gene in hereditary hemorrhagic telangiectasia type 2. Nature Genet 13: 189–195.
Gougos A, Letarte M 1988 Identification of a human endothelial cell antigen with monoclonal antibody 44G4 produced against a pre-B leukemic cell line. J Immunol 141: 1925–1933.
Letarte M, Greaves A, Vera S 1995 CD105 (endoglin) cluster report. In: Schlossman SF, Boumsell L, Gilks W, Harlan J, Kishimoto T, Morimoto C, Ritz J, Shaw S, Silverstein R, Springer T, Tedder T, Todd R (eds) Leukocyte Typing V. White Cell Differentiation Antigens. Oxford University Press, Oxford, 1756–1759.
Gougos A, St Jacques S, Greaves A, O'Connell PJ, d'Apice AJF, Buhring HJ, Bernabeu C, van Mourik JA, Letarte M 1992 Identification of distinct epitopes of endoglin, an RGD-containing glycoprotein of endothelial cells, leukemic cells, and syncytiotrophoblasts. Int Immunol 4: 83–92.
St-Jacques S, Forte M, Lye SJ, Letarte M 1994 Localization of endoglin, a transforming growth factor-β binding protein, and of CD44 and integrins in placenta during the first trimester of pregnancy. Biol Reprod 51: 405–413.
Attisano L, Carcamo J, Ventura F, Weis FMB, Massagué J, Wrana JL 1993 Identification of human activin and TGF beta type I receptors that form heteromeric kinase complexes with type II receptors. Cell 75: 671–680.
Pachenko MP, Williams MC, Brody JS, Qiang Y 1996 Type I receptor serine-threonine kinase preferentially expressed in pulmonary blood vessels. Am J Physiol 270: L547–L558
Cheifetz S, Bellon T, Calés C, Vera S, Bernabeu C, Massagué J, Letarte M 1992 Endoglin is a component of the transforming growth factor-β receptor system in human endothelial cells. J Biol Chem 267: 19027–19030.
Lastres P, Letamendia A, Zhang H, Rius C, Almendro N, Lopez LA, Langa C, Fabra A, Letarte M, Bernabeu C 1996 Endoglin modulates cellular responses to TGF-β1. J Cell Biol 133: 1109–1121.
Caniggia I, Taylor CV, Ritchie JWK, Lye SJ, Letarte M 1997 Endoglin regulates trophoblast differentiation along the invasive pathway in human placental villous explants. Endocrinology 138: 4977–4988.
Pece Barbara N, Wrana J, Letarte M 1999 Endoglin is an accessory protein that interacts with the signaling receptor complex of multiple members of the transforming growth factor-β superfamily. J Biol Chem 274: 584–594.
Letamendia A, Lastres P, Botella LM, Raab U, Langa C, Velasco B, Attisano L, Bernabeu C 1998 Role of endoglin in cellular responses to transforming growth factor-beta. J Biol Chem 273: 33011–33019.
ten Dijke P, Yamashita H, Ichijo H, Franzen P, Laiho M, Miyazono K, Heldin CH 1994 Characterization of the type I receptors for transforming growth factor β receptor-like and activin. Science 264: 101–104.
Macias-Silva M, Hoodless PA, Tang SJ, Buchwald M, Wrana JL 1998 Specific activation of Smad1 signaling pathways by the BMP7 type I receptor, ALK2. J Biol Chem 273: 25628–25636.
Lastres P, Bellon T, Cabanas C, Sanchez-Madrid F, Acevedo A, Gougos A, Letarte M, Bernabeu C 1992 Regulated expression on human macrophages of endoglin, an RGD containing surface antigen. Eur J Immunol 22: 393–397.
Pece N, Vera S, Cymerman U, White RIJ, Wrana JL, Letarte M 1997 Mutant endoglin in hereditary hemorrhagic telangiectasia type I is transiently expressed intracellularly and is not a dominant negative. J Clin Invest 100: 2568–2579.
Pece N, Cymerman U, Vera S, Marchuk D, Letarte M 1999 Expression analysis of four endoglin missense mutations suggests haploinsufficiency is the predominant mechanism for hereditary hemorrhagic telangiectasia type 1. Hum Mol Genet 8: 2171–2181.
McAllister KA, Baldwin MA, Thukkani AK, Gallione CJ, Berg JN, Porteus ME, Guttmacher AE, Marchuk DA 1995 Six novel mutations in the endoglin gene in hereditary hemorrhagic telangiectasia type 1 suggest a dominant-negative effect of receptor function. Hum Mol Genet 4: 1983–1985.
Shovlin CL, Hughes JMB, Scott J, Seidman CE, Seidman JG 1997 Characterization of endoglin and identification of novel mutations in hereditary hemorrhagic telangiectasia. Am J Hum Genet 61: 68–79.
Yamaguchi H, Azuma H, Shigekiyo T, Inoue H 1997 A novel missense mutation in the endoglin gene in hereditary hemorrhagic telangiectasia. Thromb Haemost 77: 243–247.
Gallione CJ, Klaus DJ, Yeh EY, Stenzel TT, Xue Y, Anthony KB, McAllister KA, Baldwin MA, Berg JN, Lux A, Smith JD, Vary CPH, Craighen WJ, Westermann CJJ, Warner ML, Miller YE, Jackson CE, Guttmacher AE, Marchuk DA 1998 Mutation and expression analysis of the endoglin gene in hereditary hemorrhagic telangiectasia reveals null alleles. Hum Mutat 11: 286–294.
Shovlin C, Letarte M 1999 Hereditary hemorrhagic telangiectasia and pulmonary arteriovenous malformations: issues in clinical management and review of pathogenic mechanisms. Thorax 54: 714–729.
Burrows FJ, Derbyshire EJ, Tazzari PL, Amlot P, Gazdar AF, King SW, Letarte M, Vitetta ES, Thorpe PE 1995 Up-regulation of endoglin on vascular endothelial cells in human solid tumors: implications for diagnosis and therapy. Clin Cancer Res 1: 1623–1634.
Pichuantes S, Vera S, Bourdeau A, Pece N, Kumar S, Wayner EA, Letarte M 1997 Mapping epitopes to distinct regions of the extracellular domain of endoglin using bacterially expressed recombinant fragments. Tissue Antigens 50: 265–276.
Rius C, Smith JD, Almendro N, Langa C, Botella LM, Marchuk DA, Vary CPH, Bernabeu C 1998 Cloning of the promoter region of human endoglin, the target gene for hereditary hemorrhagic telangiectasia type 1. Blood 92: 4677–4690.
Graulich W, Nettlebeck DM, Fischer D, Kissel T, Muller R 1999 Cell type specificity of the human endoglin promoter. Gene 227: 55–62.
Bourdeau A, Cymerman U, Paquet M-E, Meschino W, McKinnon WC, Guttmacher AE, Becker L, Le Tarte M 2000 Endoglin expression is reduced in normal vessels but still detectable in arteriovenous malformations of patients with Hereditary Hemorrhagic Telangiectasia Type 1. Am J Pathol 156: in press.
Ioannou P, Christopoulos G, Panayides K, Kleanthous M, Middleton L 1992 Detection of Duchenne and Becker muscular dystrophy carriers by quantitative multiplex polymerase chain reaction analysis. Neurology 42: 1783–1790.
Fullbright RK, Chaloupka JC, Putman CM, Sze GK, Merriam MM, Lee GK, Fayad PB, Awad IA, White RIJ 1998 MR of hereditary hemorrhagic telangiectasia: prevalence and spectrum of cerebrovascular malformations. AJNR 19: 477–484.
Acknowledgements
The authors thank Dr. Robert Shipman, May Hui, Liping Han, and Diane Rushlow for their invaluable help in the development of the mutation analysis strategy. We also thank Marie-Eve Paquet and Shahnaz Al Rashid for their assistance in sample preparation. We are most grateful to the patients who participated in our study and to the HHT Foundation International, Inc., for their assistance. M. Letarte is a Terry Fox Research Scientist of the National Cancer Institute of Canada.
Author information
Authors and Affiliations
Additional information
Supported by grant No. NA3434 from the Heart and Stroke Foundation of Ontario, by a grant from the Medical Research Council of Canada, and by Visible Genetics, Inc. R.I. White is supported in part by the Josephine Lawrence Hopkins Foundation.
Rights and permissions
About this article
Cite this article
Cymerman, U., Vera, S., Pece-Barbara, N. et al. Identification of Hereditary Hemorrhagic Telangiectasia Type 1 in Newborns by Protein Expression and Mutation Analysis of Endoglin. Pediatr Res 47, 24 (2000). https://doi.org/10.1203/00006450-200001000-00008
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/00006450-200001000-00008
This article is cited by
-
Endothelial signaling and the molecular basis of arteriovenous malformation
Cellular and Molecular Life Sciences (2014)
-
Specific cancer rates may differ in patients with hereditary haemorrhagic telangiectasia compared to controls
Orphanet Journal of Rare Diseases (2013)
-
A long diagnostic delay in patients with Hereditary Haemorrhagic Telangiectasia: a questionnaire-based retrospective study
Orphanet Journal of Rare Diseases (2012)
-
Mutation study of Spanish patients with Hereditary Hemorrhagic Telangiectasia
BMC Medical Genetics (2008)
-
Analysis of ENG and ACVRL1 genes in 137 HHT Italian families identifies 76 different mutations (24 novel). Comparison with other European studies
Journal of Human Genetics (2007)