Abstract
Low birth weight is associated with an increased risk of adult hypertension. To elucidate whether this association reflects altered vascular physiology already at birth, we studied acetylcholine-induced vasodilation. Forty newborn infants and their mothers were studied 3 d after delivery. Vasodilation in skin was induced by local application of acetylcholine and local heating to 44°C. Perfusion changes were measured with the laser Doppler technique. In response to acetylcholine, the mean skin perfusion increased by 240% in low birth weight infants compared with 650% in normal birth weight controls (p < 0.001). In contrast, mothers of low birth weight infants showed a mean increase in perfusion of 1100% after acetylcholine administration compared with 680% in mothers of control infants (p < 0.05). The perfusion increase at 44°C local skin temperature did not differ between the two groups of infants or between their mothers. Blood pressure was normal in all subjects. We conclude that low birth weight infants show signs of endothelial dysfunction at birth. Such findings may help us understand the link between low birth weight and adult hypertension.
Similar content being viewed by others
Main
The cardiovascular disorders related to aging are multifactorial in origin. Besides genetic and lifestyle factors, it has been suggested that adverse influences during fetal life may increase the risk of cardiovascular disease. Epidemiologic data have shown associations between low birth weight and an increased incidence of adult hypertension and coronary heart disease (1–3). There has been little verification of the proposed mechanisms or processes that could explain the fetal origins of cardiovascular disease (4). Studies in infants and children provide divergent information about the hypothesis that fetal malnutrition programs the development of abnormal vascular structure and physiology, which ultimately may cause hypertension in adults (5–8). Recent data have suggested a common genetic background for low birth weight, susceptibility for glucose intolerance, and cardiovascular disease in adults (9, 10).
The etiology of essential hypertension remains unknown. One of the theories proposed involves an imbalance between endothelium-derived vasoconstrictive and vasodilatory factors (11–13). The peripheral and coronary circulations of adults with essential hypertension have been shown to have decreased endothelium-dependent vasodilation in response to ACh stimulation (14–17). Experimental data indicate that this is also true of other parts of the vascular tree. In pregnant women with acute hypertension due to preeclampsia, the release of endothelial-derived NO is impaired in subcutaneous resistance arteries (18) and human umbilical vessels (19).
There have been no studies of endothelium-dependent vasodilation in human newborn infants. We hypothesized that low birth weight may be associated with altered vascular function already at birth. We compared ACh and heat-induced vasodilations in low and normal birth weight infants. A second aim was to characterize the vascular responses to ACh and heating in the two groups of mothers.
METHODS
Subjects.
We investigated 90 subjects, 40 newborn infants (19 boys) and their mothers as well as 10 healthy age-matched women with regular menstruation, without oral contraceptives, and with a history of pregnancy at least 2 y before the investigations (control women). Only term infants were studied (gestational age, 39 ± 1 wk). The gestational age of all infants had been determined by early routine ultrasound at a gestational age of 17–18 wk. Multiple pregnancies and infants with neonatal asphyxia, malformations, chromosomal disorders, or congenital infection were not included in the study. All neonates were nursed by their mothers in the maternity ward. All parents were white and born in Sweden. All women were healthy nonsmokers (both before and during pregnancy) who were not taking any medications or special diets. Mothers with hypertension (blood pressure >140/90 mm Hg), borderline hypertension (DBP >85 mm Hg), preeclampsia, or diabetes were excluded. Both parents of the infants were interviewed to obtain a possible family history of diabetes, myocardial infarction, stroke, and hypertension as well as hyperlipidemia among the first-degree relatives to the parents (Table 1).
On the basis of these criteria, we selected 20 newborn infants (nine boys) who were SGA (birth weight < −2 SD for newborn infants in Sweden). Their birth weights (2510 ± 270 g) were lower than those of the 20 control infants who were AGA (10 boys, birth weight 3608 ± 460 g, p < 0.001). There was no overlapping in birth weights between the two groups of infants. Birth lengths and head circumferences were significantly greater in the AGA group than the SGA group (p < 0.001, Table 1). No infant was microcephalic.
The ratio between birth weight and birth length at the defined gestational age, given as SD scores (20), indicated leanness in 13/20 SGA infants. In the SGA group, the antenatal history showed impaired intrauterine growth in 12/20 fetuses as assessed by ultrasound fetometry and abnormal umbilical Doppler flow velocity in 4/12 growth-retarded fetuses. Regardless of the study protocol, an obstetrical decision to deliver by cesarean section was made among 11/20 in the SGA group. The AGA group was matched in respect to postnatal and gestational ages, gender, and mode of delivery (10/20 delivered by cesarean section).
Informed consent was obtained from the parents before each investigation, and the study was approved by the local Ethics Committee at Karolinska Hospital. The investigators were not blinded to the birth weights when undertaking the study.
Vascular studies.
The subjects were studied at a room temperature of 24 ± 1°C. All women refrained from eating and/or drinking coffee 2 h before the investigations. During the studies, they sat comfortably in chairs, resting their forearms and hands on armrests at heart level. The newborn infants were fed 30 to 60 min before each investigation, and vascular studies were performed when the infants were sleeping quietly in the prone position. The newborns and their mothers were studied 3 to 4 d after delivery. Control women were studied once. Heart rate and blood pressure (mean out of 3 repeated measures; Dinamap, USA) (21) were measured in all subjects. The body temperature and venous hematocrit were determined and found to be normal in all newborn subjects.
A LD instrument (Periflux 4001, wavelength 780 nm) and a micropharmacology system (iontophoresis) were used for noninvasive and continuous measurement of perfusion changes during vascular provocations in the skin (Perimed AB, Järfälla, Sweden). A drug delivery electrode was incorporated in the head of the LD probe. The probe temperature could be varied and was standardized to 32°C during drug tests.
To study endothelium-dependent vasodilation (22, 23), skin basal perfusion was recorded for at least 2 min, after which ACh 2% (acetylcholinum ophthalmicum, Dispersa AG, Hettlingen, Switzerland) dissolved in deionized water was transferred across the skin by iontophoresis (anodal current of 0.1 mA for 20 s). A dose-response curve was produced by repeating iontophoretic stimulation six times at 60-s intervals. Details of the methodology have been reported previously (24).
After the last iontophoretic stimulation and when skin perfusion had returned to the basal level, the probe temperature was increased to 44°C for 10–15 min. The peak perfusion value during local heating was measured as a reflection of maximal skin vasodilation.
The LD signal is proportional to the number and velocity of moving blood cells in illuminated superficial skin microvessels (25, 26). The LD output is semiquantitative and expressed in PU of output voltage (1 PU = 10 mV) in accordance with general consensus (European Laser Doppler Users Groups, London 1992). Because the output cannot easily be translated into absolute values of blood flow, the magnitude of the changes in skin perfusion after iontophoretic stimulation with ACh and after heating was calculated as the ratio between peak and mean baseline perfusions. The residual LD signal recorded during arterial occlusion is referred to as the zero reference in these calculations. Arterial occlusion was induced by inflating a pneumatic wrist cuff to a suprasystolic pressure for 1 min.
At our laboratory, the coefficient of variation has been found to be 18% for maximal perfusion changes after ACh stimulation, calculated in two sets of repeated measurements in seven healthy female volunteers with a time interval of 1 to 5 wk (24).
Statistical analyses.
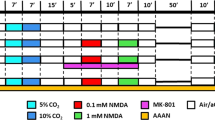
Values are given as mean ± SD (Text) or ± SEM (Figure 1). The dose-response curves created by repeated iontophoresis with ACh were characterized by calculating simple regression coefficients for relative changes in perfusion over time in each subject. The t test and ANOVA were used to compare group means. Stepwise regression analysis was used to test for relationships between perfusion and other background variables. Assessment of perfusion responses to iontophoresis with NaCl was made using ANOVA for repeated measures. A p < 0.05 was considered significant.
RESULTS
Blood pressure data.
Blood pressure (Table 2) was within normal limits in all subjects, and it was similar in the two groups of infants. There were no gender differences. The systolic but not DBP was higher in mothers of SGA infants than in mothers of AGA infants and in control women (p < 0.05). Both groups of newly delivered women had higher heart rates than healthy control women. Subjects with a positive family history of cardiovascular disease had a similar blood pressure compared with those without such a history.
Basal perfusion data.
At a standardized probe temperature (32°C), we found large interindividual variations in basal skin perfusion values, ranging from 2 to 38 PU (Table 3). The only significant group differences in basal skin perfusion values were found for the mothers of AGA infants, who had higher basal skin perfusion rates (11 ± 5.9 PU, p < 0.05) than those from other groups (control women 5.3 ± 2.8, mothers of SGA infants 6.5 ± 5.1, AGA infants 6.2 ± 3.8, and SGA infants 8.8 ± 7.8 PU, Table 3).
NaCl iontophoresis.
To exclude any vascular response from the current alone, the skin perfusion was measured in control women (n = 10) and in an additional group of newborn infants and their mothers (n = 10 pairs) after repeated iontophoretic application of isotonic NaCl. No change in skin perfusion was detected (p = 0.91, 0.70, and 0.97 in the respective group).
ACh-induced vasodilation.
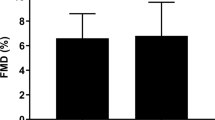
Starting from similar basal perfusion values as AGA infants, the SGA infants showed a significantly lower (p < 0.001) increase in perfusion in response to ACh. The relative peak perfusion was 240 ± 125% in SGA infants compared with 650 ± 250% in infants of normal weight (basal perfusion = 100%, Fig. 1). Within groups, there were no correlations between vasodilation and birth weight, gestational age, or gender. Subdividing the SGA group, lean SGA infants (n = 13) had a lower perfusion increase (189 ± 40%) compared with the symmetrically small SGA infants (338 ± 170%, p < 0.01). Infants with a positive family history of cardiovascular disease among second-degree relatives (13/40) had a similar perfusion increase compared with those without such a history (p = 0.84).
Mothers of SGA infants had a higher peak/baseline perfusion ratio in response to ACh (1100 ± 785%) compared with mothers with AGA infants (685 ± 337%, p < 0.05, Fig. 1). This finding may be attributed to higher basal skin perfusion values in mothers of AGA infants (11 ± 5.9 PU) compared with mothers of SGA infants (6.5 ± 5.1 PU), whereas the peak perfusion values did not differ significantly between the two groups (Table 3 and Fig. 1).
The relative peak perfusion in healthy control women exceeded that in both groups of newly delivered women and was 1860 ± 780% (p < 0.05, Fig. 1). Mothers with a positive family history of cardiovascular disease showed a tendency toward a higher relative peak perfusion increase (p = 0.14). After the difference in family history had been accounted for using multiple regression, the difference in the relative perfusion increase still existed between mothers in the SGA and the AGA group (p < 0.05).
Mothers and infants in the AGA group showed similar vascular responses to ACh (Fig. 1). The degree of relative increases in peak perfusion from the AGA infants correlated to those of their mothers (r = 0.57, p < 0.01). Mothers and infants in the SGA group showed deviating vascular responses to ACh (p < 0.001), and their perfusion responses showed no correlation.
Variations in vascular response to ACh showed no correlation to variations in blood pressure, heart rate, or hematocrit in newborn infants. In mothers of SGA infants, a correlation between DBP and relative perfusion change was found (r = 0.49, p = 0.03).
There was a significant relation between the basal perfusion value and percentage peak perfusion increase in AGA infants (r = −0.73, slope = −64, p < 0.001) and in control women (r = −0.77, slope = −230, p < 0.01). There was no significant association between basal perfusion values and relative peak perfusion increase in the other groups.
The basal perfusion correlated to the absolute peak perfusion value in SGA infants (r = 0.89, slope = 1.6, p < 0.001) and in mothers to SGA infants (r = 0.53, slope = 3.9, p < 0.05). There was no significant association between basal perfusion and absolute peak perfusion values in the other groups.
Maximal vasodilation at 44°C.
Setting the probe temperature to 44°C resulted in a marked increase in perfusion that peaked at absolute perfusion values that did not differ from those after ACh stimulation in healthy control women and in AGA infants (Table 3). In mothers of SGA and AGA infants and in SGA infants, the peak perfusion values at 44°C were higher than the peak perfusion values after ACh (p < 0.01, Table 3).
Comparing absolute and relative perfusion responses at 44°C, we found no significant difference in perfusion changes between SGA (430 ± 190%) and AGA infants (570 ± 310%).
The relative perfusion increases at 44°C in mothers of AGA infants (1040 ± 520%) were lower than the corresponding values in mothers of SGA infants (1620 ± 650%, p < 0.05) and in healthy control women (1940 ± 810%, p < 0.01). The absolute peak perfusion value did not differ between the three groups of women (Table 3). Subjects with a positive family history of cardiovascular disorder showed similar perfusion responses to local heating as found in those without such history.
In SGA mothers, a correlation was found between the DBP and the maximal hyperemic response (r = 0.64, p < 0.01). No other associations were found between the vascular response to 44°C and the other variables studied.
DISCUSSION
The major finding in this study was a significant impairment of the vascular responses to ACh in newborn infants who were SGA. The reduced responsiveness to ACh suggests an abnormal function on the part of the vascular tree that was under study. Our data probably reflect the perfusion in the subpapillary vascular bed from which the major part of the LD signal has been thought to originate (27). These subpapillary resistance vessels participate in specific functions required by the organism as a whole, such as regulation of systemic blood pressure and body temperature. The loss of normal ACh-induced relaxation in cutaneous blood vessels of newborn infants with low birth weight may indicate disturbed blood pressure regulation even at birth. Although limited by a small and incomplete number of infants (n = 10, 5 SGA infants), a pilot follow-up at 3 mo of age indicates that the vascular dysfunction associated with low birth weight may not only be a transient problem confined to the immediate neonatal period (our unpublished observation). Our assumptions are supported by the finding of reduced flow-mediated endothelium-dependent vasodilation in the brachial artery of schoolchildren with low birth weight (8).
Vasodilation elicited by ACh is endothelium dependent; when the endothelium is damaged or removed, the vasodilatory effect of ACh is lost (22, 28). Previous studies of vascular responses in human skin have suggested that endothelial release of NO, endothelium-derived hyperpolarizing factor, or prostanoids are mediators of ACh-induced vasodilation in healthy subjects (23, 29, 30). Our finding that low birth weight newborn infants had little if any vascular response to ACh may, therefore, reflect a cutaneous endothelial dysfunction involving the NO, endothelium-derived hyperpolarizing factor, or prostanoid systems.
Our interpretations are based on the assumption that the two groups of infants received the same dose of ACh. Variations in skin thickness and skin resistance may affect the ACh dose. The finding of thinner skin in low birth weight neonates (31) suggests a higher transdermal delivery of ACh in SGA compared with AGA infants. The lower perfusion response to ACh in SGA infants is, therefore, unlikely an effect of lower ACh dose. A higher local vascular uptake and clearance of the drug in SGA infants is also unlikely because the basal perfusion values were similar in the two groups and, at least among SGA subjects, the perfusion response to ACh increased in relation to a higher basal perfusion level. Hypothetically, differences in local drug metabolism may exist. The most reassuring evidence that the differences in vascular responses to ACh are real is the dose-response curves themselves.
The physiologic vasodilation at 44°C suggests that the vascular smooth muscle was not refractory to relaxation in infants who were SGA. Selective vascular smooth muscle responsiveness to NO could have been pharmacologically tested by the introduction of an exogenous NO donor such as nitroprusside into the skin. However, we chose to refrain from such testing, because iontophoresis of nitroprusside requires a more powerful cathodal current, which has been reported to induce vascular responses due to the current itself (23, 32).
Using our protocol, unspecific neurogenic vasodilation in response to the current used for iontophoretic stimulation is unlikely, because we found no perfusion change during repeated iontophoresis with NaCl. Anodal iontophoresis must be used for longer periods with higher current strength and more concentrated ACh solutions to elicit axon reflexes (33).
As the sampling volume cannot be exactly defined and as it may vary between individuals, the LD method does not permit true quantitations of skin blood flow. The output is directly proportional to the number of moving blood cells and their velocity within the illuminated skin volume. Although blood cell velocity may change differently from blood flow, the LD signal has been found to correspond to tissue blood flow determined by other methods (25, 26). The continuous output makes the LD method particularly useful for studying rapid skin perfusion changes, such as those induced by iontophoretically applied drugs or heating.
During pregnancy, the maternal uteroplacental circulation switches from a high-resistance low-flow system to a low-resistance high-flow vascular bed to meet the needs of the growing fetus. The vascular endothelium is involved in these changes, also facilitating lowered vascular resistance in the peripheral circulation (34, 35). This could be the explanation for our finding of doubled basal perfusion values in mothers of AGA infants compared with control women. In contrast, basal perfusion values of the mothers of SGA infants were similar to those of control women. The differences in basal perfusion data among the three groups of women are important to think of when the results are interpreted. After administration of ACh, the higher relative perfusion increase in mothers of SGA infants compared with mothers of AGA infants may not reflect larger ACh-induced vasodilation. Considering the absolute perfusion values before and after ACh stimulation, the opposite may in fact be true, i.e. that the mothers of SGA infants had a blunted endothelial function similar to their infants.
Under physiologic conditions, the vascular function of both the pregnant woman and her fetus may have been influenced by one or several common factors, e.g. circulating hormones. Estrogen levels increase during normal pregnancy, and these hormones show free transplacental passage and are partly synthesized in the placenta. Estrogens have protective cardiovascular properties in women of reproductive age and enhance basal vascular relaxation and blood flow in the forearm (35, 36). In intrauterine growth retardation (IUGR), the placental-fetal unit functions poorly and estrogen levels in both maternal and fetal circulations are decreased (37).
Low birth weight is not the same as IUGR, and its definition may vary between different studies. We have used the statistical term SGA (birth weight < −2 SD corrected for gestational age) to discriminate infants in an otherwise comparable and well-defined population sample. Estimates among SGA infants in North America have shown that approximately 50% were IUGR, whereas the remaining subjects could only be characterized as small (38). These proportions also seem to be fairly the same in our sample, as judged from the number of lean SGA neonates (13/20). This probably contributed to our finding of overlapping vascular responses in small and appropriately sized infants.
This study gives no clear evidence of either intrauterine programming of the vascular tree in response to fetal malnutrition or genetic preselection. Although lean SGA infants showed the lowest vascular responses, a common genetic background cannot be excluded (9, 10). The mothers of infants who were SGA had slightly higher blood pressures than the control mothers.
What this study does give, however, is a clue to a better understanding of the previously reported association between low birth weight and increased risk of developing hypertension in adult life. This clue is that the vascular endothelium, which is involved in the pathogenetic process of hypertension, responds poorly to ACh in low birth weight infants. Further studies should be done to find the cause of this endothelial dysfunction and to determine whether it can be detected early among pregnant women and in the fetus and to pursue its development during childhood.
Abbreviations
- AGA:
-
appropriate for gestational age
- SGA:
-
small for gestational age
- ACh:
-
acetylcholine
- LD:
-
laser Doppler
- PU:
-
perfusion units
- NO:
-
nitric oxide
- DBP:
-
diastolic blood pressure
References
Barker D, Osmond C, Golding J, Kuh D, Wadsworth M 1989 Growth in utero, blood pressure in childhood and adult life, and mortality from cardiovascular disease. BMJ 298: 564–567.
Gennser G, Rymark P, Isberg P 1988 Low birth weight and risk of high blood pressure in adulthood. BMJ 296: 1498–1500.
Law C, de Swiet M, Osmond C, Fayers P, Barker D, Cruddas A, Fall C 1993 Initiation of hypertension in utero and its amplification throughout life. BMJ 306: 24–27.
Elford J, Whincup P, Shaper A 1991 Early life experience and adult cardiovascular disease: longitudinal and case-control studies. Int J Epidemiol 20: 833–844.
Whincup P, Cook D, Papacosta O, Walker M 1995 Birth weight and blood pressure: cross-sectional and longitudinal relations in childhood. BMJ 311: 773–776.
Ley D, Stale H, Marsal K 1997 Aortic vessel wall characteristics and blood pressure in children with intrauterine growth retardation and abnormal foetal aortic blood flow. Acta Paediatr 86: 299–305.
Himmelmann A, Svensson A, Hansson L 1994 Relation of maternal blood pressure during pregnancy to birth weight and blood pressure in children. J Intern Med 235: 347–352.
Leeson C, Whincup P, Cook D, Donald A, Papacosta O, Lucas A, Deanfield J 1997 Flow-mediated dilation in 9- to 11-year-old children. Circulation 96: 2233–2238.
Hattersley A, Beards F, Ballantyne E, Appleton M, Harvey R, Ellard S 1998 Mutations in the glucokinase gene of the fetus result in reduced birth weight. Nat Genet 19: 268–270.
Hattersley A, Tooke J 1999 The fetal insulin hypothesis: an alternative explanation of the association of low birth weight with diabetes and vascular disease. Lancet 353: 1789–1792.
Gibbons G 1997 Endothelial function as a determinant of vascular function and structure: a new therapeutic target. Am J Cardiol 79: 3–8.
Taddei S, Virdis A, Mattei P, Ghiadoni L, Sudano I, Salvetti A 1996 Defective l -arginine-nitric oxide pathways in offspring of essential hypertensive patients. Circulation 94: 1298–1303.
Cardillo C, Kilcyone C, Arshed R, Quyyumi A, Cannon R III, Panza J 1998 Selective defect in nitric oxide synthesis may explain the impaired endothelium-dependent vasodilation in patients with essential hypertension. Circulation 97: 851–856.
Linder L, Kiowski W, Bühler F, Lüscher T 1990 Indirect evidence for release of endothelium-derived relaxing factor in human forearm circulation in vivo. Circulation 81: 1762–1767.
Egashira K, Suzuki S, Hirooka Y, Kai H, Sugimachi M, Imaizumi T, Takeshita A 1995 Impaired endothelium-dependent vasodilation of large epicardial and resistance coronary arteries in patients with essential hypertension. Hypertension 25: 201–206.
Taddei S, Virdis A, Mattei P, Arzilli F, Salvetti A 1992 Endothelium-dependent forearm vasodilation is reduced in normotensive subjects with familial history of hypertension. J Cardiovasc Pharmacol 20: 193–195.
Ghiadoni L, Taddei S, Virdis A, Sudano I, Di Legge V, Meola M, Di Venanzio L, Salvetti A 1998 Endothelial function and common carotid artery wall thickening in patients with essential hypertension. Hypertension 32: 25–32.
McCarthy A, Woolfson R, Raju S, Poston L 1993 Abnormal endothelial cell function of resistance arteries from women with preeclampsia. Am J Obstet Gynecol 168: 1323–1330.
Pinto A, Sorrentino R, Sorrentino P, Guerritore T, Miranda L, Biondi A, Martinelli P 1991 Endothelial-derived relaxing factor released by endothelial cells of human umbilical vessels and its impairment in pregnancy-induced hypertension. Am J Obstet Gynecol 164: 507–513.
Niklasson A, Karlberg P 1993 Weight-for-length model in newborn Swedish infants. Acta Paediatr 82: 333–339.
Thoresen M, Cowan F 1992 Dinamap blood pressure measurements in the newborn: how many–what effects?. Acta Paediatr 81: 272–273.
Furchgott R, Zawadzki J 1980 The obligatory role of endothelial cells in the relaxation of arterial smooth muscle by acetylcholine. Nature 288: 373–376.
Morris S, Shore A 1996 Skin blood flow responses to the iontophoresis of acetylcholine and sodium nitroprusside in man: possible mechanisms. J Physiol 496: 531–542.
Hu J, Norman M, Wallensteen M, Gennser G 1998 Increased large arterial stiffness and impaired acetylcholine-induced skin vasodilatation in women with previous gestational diabetes mellitus. Br J Obstet Gynaecol 105: 1279–1287.
Nilsson G, Tenland T, Öberg P 1980 Evaluation of a laser Doppler flowmeter for measurement of tissue blood flow. IEEE Trans Biomed Eng 27: 597–604.
Smits G, Roman R, Lombard J 1986 Evaluation of laser Doppler flowmetry as a measure of tissue blood flow. J Appl Physiol 61: 666–672.
Fagrell B 1994 Problems using laser Doppler on the skin in clinical practice. In: Belcaro G, Hoffmann U, Bollinger A, Nicolaides A (eds) Laser Doppler. Med-Orion Publishing Company, London, 50–52.
Furchgott R, Vanhoutte P 1989 Endothelium-derived relaxing and contracting factors. FASEB J 3: 2007–2018.
Warren J 1994 Nitric oxide and human skin blood flow responses to acetylcholine and ultraviolet light. FASEB J 8: 247–251.
Noon J, Walker B, Hand M, Webb D 1998 Studies with iontophoretic administration of drugs to human dermal vessels in vivo : cholinergic vasodilation is mediated by dilator prostanoids rather than nitric oxide. Br J Clin Pharmacol 45: 545–550.
Reinholdt Petersen J, Petersen S, Serup J 1995 High-frequency ultrasound measurement of dermis and subcutaneous fat in the newborn infant. Skin Res Technol 1: 86–89.
Morris S, Shore A, Tooke J 1995 Responses of the skin microcirculation to acetylcholine and sodium nitroprusside in patients with NIDDM. Diabetologia 38: 1337–1344.
Parkhouse N, Le Quesne P 1988 Quantitative objective assessment of peripheral nociceptive C fibre function. J Neurol Neurosurg Psychiatry 51: 28–34.
Williams D, Vallance P, Neild G, Spencer J, Imms F 1997 Nitric oxide-mediated vasodilation in human pregnancy. Am J Physiol 272: H748–H752.
Morris N, Eaton B, Dekker G 1996 Nitric oxide, the endothelium, pregnancy and pre-eclampsia. Br J Obstet Gynaecol 103: 4–15.
Sudhir K, Jennings G, Funder J, Komesaroff P 1996 Estrogen enhances basal nitric oxide release in the forearm vasculature in perimenopausal women. Hypertension 28: 330–334.
Reynolds J, Barnhart B, Carlson C 1986 Feto-placental steroid metabolism in growth retarded human fetuses. Pediatr Res 20: 166–168.
Metcoff J 1994 Clinical assessment of nutritional status at birth. Pediatr Clin North Am 41: 875–891.
Author information
Authors and Affiliations
Additional information
Supported by grants from the Samariten Foundation, General Maternity Hospital Foundation, and the Karolinska Institute's research foundations in Stockholm, Sweden.
Rights and permissions
About this article
Cite this article
Martin, H., Gazelius, B. & Norman, M. Impaired Acetylcholine-Induced Vascular Relaxation in Low Birth Weight Infants: Implications for Adult Hypertension?. Pediatr Res 47, 457–462 (2000). https://doi.org/10.1203/00006450-200004000-00008
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/00006450-200004000-00008
This article is cited by
-
Maternal undernutrition and cardiometabolic disease: a latin american perspective
BMC Medicine (2015)
-
Fetale und perinatale Programmierung der Nierenfunktion
Gynäkologische Endokrinologie (2014)
-
Fetal programming of renal function
Pediatric Nephrology (2012)