Abstract
Previous studies have shown the immunoregulatory functions IL-4 in type 1 diabetes mellitus. Therefore, the genes involved in the IL-4 regulatory pathway are candidates for diabetes susceptibility genes. Here we have evaluated IL4 and the alpha subunit of the IL-4 receptor (IL4R α) genes using the affected sibpair (ASP) and transmission/disequilibrium test (TDT). We analyzed 309 diabetic families from the United States and 87 families from various European countries. There was no evidence that either of these two genes are linked or associated with type 1 diabetes. Means by which IL-4 directed signals could indirectly alter diabetes susceptibility are proposed.
Similar content being viewed by others
Main
Type 1 diabetes is caused by cell mediated autoimmune destruction of the pancreatic Islets of Langerhans. Recently, the immunoregulatory function of interleukin-4 (IL-4) has been suggested as a determinant of disease amelioration in experimental animal models and in humans. The human IL4 gene has been mapped to 5q23–31 and the major component of its receptor, the IL4Rα gene has been mapped to 16p. Whereas neither of these loci falls within a defined diabetes susceptibility linkage interval, full genome screens may not be sensitive enough to detect their influence. Associations between diabetes and these genes have not, to our knowledge, been examined. We therefore examined whether the IL4 and IL4Rα genes are linked to or associated with diabetes susceptibility.
IL-4, produced by Th2 CD4+ T lymphocytes, NK T cells, γδ T lymphocytes, mast cells and basophils, exerts a wide variety of effects, both stimulatory and inhibitory, on immune function. It stimulates development of Th2 lymphocytes that produce IL-4, IL-5, IL-6, IL-10, and IL-13, whereas it suppresses interferon-γ and IL-2 producing Th1 cells. Immunoglobulin class switching to IgE and IgG4 is dependent on IL-4 and the cytokine enhances B lymphocyte proliferation, activation, and tissue adhesion. Accumulating evidence suggests that re-direction of a predominantly Th1 response toward one with more Th2 characteristics is associated with reduction of islet destruction, despite persistent islet-specific autoimmunity (1, 2). Expression of IL-4 in the β cells of transgenic non-obese diabetic (NOD) mice abrogated the development of diabetes (3). Therapy with IL-4 prevents the development of diabetes in the NOD mouse (4), and detection of IL-4 in islets at the onset of inflammation was predictive of nondestructive insulitis (5, 6). There have been reports of Th1 mediated inflammatory responses in and around β cells of the pancreas (7, 8) in NOD mice and in postmortem examination of the pancreas of humans with acute onset of diabetes (9–13). In humans, NKT cells, producing high levels of IL-4 were cloned less frequently from diabetic children than from their nondiabetic siblings (14). In addition, declining IgE responses to the diabetes-associated antigen, glutamic acid decarboxylase, have been associated with susceptibility to diabetes among siblings of affected individuals (15). The combined data support the hypothesis that IL-4 action provides some resistance to progression to diabetes in susceptible individuals.
Induction of IL-4 effects depends on the cytokine binding to its specific membrane receptor (reviewed in Ref. (16). After binding its ligand, IL-4Rα must also incorporate the γc chain into its complex to attain maximum activity. Signal transduction by the complex requires IL-4Rα phosphorylation by intracellular kinases (e.g. Jak-1, Jak-3). Subsequent binding of members of the insulin receptor substrate (IRS) family, Shc and Cbl adapters, and Stat-6 to phosphorylated residues on the IL-4 receptor complex, exerts influences on membranous and cytoplasmic signals as well directly as on gene transcription.
Several polymorphisms in the promoter region of the IL4 gene may lead to altered IL4 expression and possibly modify susceptibility to type 1 diabetes (17). A substitution of guanine for adenine at nucleotide 1902 in the α subunit of the IL-4Rα results in an amino acid change from glutamine to arginine in the cytoplasmic domain of the receptor (18). This gain of function point mutation has been shown to cause increased production of IgE (19). Association of this marker with asthma and other atopic diseases has been previously reported (20). Therefore, both the IL4 and IL4R α genes may be candidate genes for diabetes susceptibility. In this study, we have evaluated these two genes using sequencing, linkage, and association analyses in a large collection of diabetic families.
METHODS
Subjects
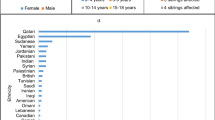
The study subjects include 309 diabetic families from the United States (53 from southeastern USA and 256 from the human biologic data interchange) and 87 families from European countries (46 from continental Italy, 25 families from France and 16 from Spain). The 10 patients used in sequencing analyses were randomly selected from 10 of our diabetic families (6 from the United States, 2 from Italy, and 2 from France). The 5 sequenced controls were selected from our normal control samples (Caucasians from Florida). The study was approved by the Institutional Review Board of the University of Florida and informed consent was obtained from all subjects.
Protocols
A CA repeat polymorphism in intron 2 of the IL4 gene was genotyped using the primers IL4–3 (5′-CGTCCACCTCGGCCTCTC-3′) and IL4–4 (5′-CGGTTGGATGGACTTGGAG-3′). The marker was genotyped using a procedure described previously (21).
We sequenced a 370 bp fragment (from −315 to 55) containing the promoter region of IL4 after amplification with the primers IL4–1 (5′TATTACTCTATCTTTCCCCAGG3′) and IL4–2 (5′TTGCAGTGACAATGTGAGGCA3′). PCR product (50 μL) was electrophoresed on a 2.0–2.5% agarose gel. An aliquot of the purified products (30 ng) was then directly used for cycle sequencing using the ABI Prism BigDye terminator (Applied Biosystems) according to manufacturer's instructions.
A substitution of guanine for adenine at nucleotide 1902 in IL4R α was genotyped for all diabetic families using a polymerase chain reaction (PCR)/restriction enzyme digest method (22, 23). PCR amplifications were performed using the primers IL4Rα-1 (5′-CCCCCACCAGTGGCTACC-3′) and IL4Rα-2 (5′-AGAGAAATGTGGGTTTGGGC-3′) with 20 ng of genomic DNA in 12 μL reaction volume containing 50 mM KCL, 10 mM Tris-Cl, pH 8.3, 1.5 mM MgCl2; 60 μM of each dNTP. Samples were subjected to 35 cycles of 30s at 94°C for denaturing, 30 s at 60°C and 30 s at 72°C for extension with a preliminary 2 min at 94°C for denaturation and a final annealing period of 2 min at 72°C. The IL4Rα-1 primer was designed to create a Msp I restriction site in the PCR products from the 1902-G allele but not in the 1902-A allele. Digestion was performed overnight in a 37°C water bath using 20 units of enzyme per 12 μL PCR product (final volume of 32 μL). Digestion of the 161 bp PCR product resulted in a 143 bp fragment for the 1902-G allele and uncleaved 161 bp for the 1902-A allele. The fragments were separated by electrophoresis on a 3.5% agarose gel.
Data analysis
The affected sibpair (ASP) method was used to evaluate linkage evidence. This method compares the observed gene sharing by affected sibpairs with the randomly expected 50%. The maximum lod scores (MLS) were calculated according to Risch (24) using the following equation: T = N1[log10(N1/0.5N)] + N0[log10(N0/0.5N)], where N1 and N0 are the numbers of ASPs sharing 1 and 0 alleles, respectively, and N is the total number of informative meioses (N0 + N1). The transmission/disequilibrium test (TDT) (25) was used to evaluate linkage/association within ASP families. In a conventional TDT, the transmission of individual alleles is compared with the expected 50% transmission from heterozygous parents to affected children using a χ2 test of equal expectation.
RESULTS
Two experimental approaches, sequencing of the promoter region and linkage/association analysis, were used to assess the potential role of the IL4 gene, which is located in a cluster of cytokine genes on chromosome 5q23–31. We have sequenced the promoter region of this gene for 10 diabetic subjects and 5 controls. No sequence variation was found in the subjects or controls. To further evaluate the IL4 gene, we analyzed a CA repeat polymorphism in intron 2 of the IL4 gene. Affected sibpair analysis of the data did not reveal any evidence for linkage (Table 1). We then performed TDT tests for the three most frequent alleles (alleles 2, 3, and 12). No significant transmission deviation from the 50% expectation was detected in our data set (Table 1). These results suggest that IL4 is not a diabetes susceptibility gene.
To assess the potential role of the α subunit of IL-4 receptor in type 1 diabetes, the 1902-A/G mutation was genotyped for all diabetic families. As shown in Table 1, there was no significant deviation of allele sharing of the IL4Rα gene by affected sibpairs. We then tested the transmission of the two alleles to affected siblings from heterozygous parents and no significant deviation of transmission was detected, suggesting IL4Rα is probably not a type 1 diabetes susceptibility gene.
DISCUSSION
Type 1 diabetes is a polygenic and multifactorial disease and a large number of susceptibility genes may contribute to the genetic predisposition to the disease (26, 27). However, only IDDM1 (the HLA genes) and IDDM2 (the insulin gene) have been definitively identified. These genes were indeed identified through linkage and association analyses of candidate genes. In this study, we used linkage and association analyses to evaluate two candidate genes:IL4 and IL4Rα. A polymorphism in the promoter region of IL4 (C to T change at −590) is associated with significant increases in the mean total IgE level and allergic responses (28, 29). Therefore, polymorphisms in IL4 may also be a contributing factor in Type 1 diabetes. To test this hypothesis, we attempted to identify polymorphisms with potential functional significance by sequencing the promoter region so that they can be used in linkage and association studies. Unfortunately, we were not able to identify any polymorphisms in 10 diabetic patients and 5 normal controls. Since a total of 40 chromosomes (20 individuals) were sequenced, any polymorphisms, if they exist, must have very low frequencies (probably less than 5%). From these sequencing analyses, we believe that the IL4 promoter region is unlikely a major genetic factor in Type 1 diabetes, even though variations in the region may be related to Type 1 diabetes in a very small number of patients. Since no polymorphism was identified by sequencing analyses, we used a CA repeat within intron 2 of IL4 as a genetic marker to test linkage and association between IL4 and the disease. If a diabetes-related mutation is in linkage disequilibrium with the CA repeat, analyses of the marker should reveal significant association. Since no association was detected with 396 multiplex families, our data provided solid evidence that IL4 is unlikely IDDM susceptibility genes, consistent with all previous reports that identified no type 1 diabetes genes on chromosome 5q. Our studies cannot firmly exclude a possible association between diabetes and potential IL4 polymorphisms that are not in linkage disequilibrium with the CA repeat in intron 2, but this circumstance is unlikely.
IL4Rα was also a good candidate gene for type 1 diabetes, because it mediates IL-4 activity. A substitution of guanine for adenine at nucleotide 1902 in IL4Rα is associated with atopy (19). This substitution results in an amino acid change from glutamine to arginine (Q576R) in the cytoplasmic domain of the receptor. It has been shown that the signaling function of the R576 allele is greater than that of the wild-type allele (Q576). Our studies can exclude all polymorphisms in linkage disequilibrium with the Q/R576 mutation as type 1 diabetes factor. Definitive exclusion of IL4Rα as a candidate gene would require an exhaustive search for other polymorphisms that are not in linkage disequilibrium with the Q/R576 mutation.
Modulation of autoimmunity by IL-4 may occur indirectly through other genetic mutations. Expression of IL4 may, for instance, be altered by other cytokines, such as interferon-γ or IL-12. The production of IL-4 is itself dependent on the generation of IL-4 mediated signals. Therefore, defects in the receptor complex assembly or intracellular signaling pathways at points distal to the IL-4Rα subunit itself may account for alterations of susceptibility to type 1 diabetes.
Abbreviations
- IL-4:
-
interleukin 4
- IL4:
-
gene encoding IL-4
- IL-4Rα:
-
alpha subunit of interleukin 4 receptor
- IL4R α:
-
gene encoding the α subunit of the interleukin 4 receptor
- NOD:
-
non-obese diabetic
- MLS:
-
maximum lod score
- ASP:
-
affected sibpair
- TDT:
-
transmission/disequilibrium test
References
Tisch R, Wang B, Serreze DV 1999 Induction of glutamic acid decarboxylase 65-specific Th2 cells and suppression of autoimmune diabetes at stages of disease is epitope dependent. J Immunol 163: 1178–1187
Maron R, Melican NS, Weiner HL 1999 Regulatory Th2-type cell lines against insulin and GAD peptides derived from orally- and nasally-treated NOD mice suppress diabetes. J Autoimmun 12: 251–258
Gallichan WS, Balasa B, Davies JD, Sarvetnick N 1999 Pancreatic IL-4 expression results in islet-reactive Th2 cells that inhibit diabetogenic lymphocytes in the nonobese diabetic mouse. J Immunol 163: 1696–1703
Rapoport MJ, Jaramillo A, Zipris D, Lazarus AH, Serreze DV, Leiter EH, Cyopick P, Danska JS, Delovitch TL 1993 Interleukin 4 reverses T cell proliferative unresponsiveness and prevents the onset of diabetes in nonobese diabetic mice. J Exp Med 178: 87–99
Mueller R, Krahl T, Sarvetnick N 1996 Pancreatic expression of interleukin-4 abrogates insulitis and autoimmune diabetes in nonobese diabetic (NOD) mice. J Exp Med 184: 1093–1099
Fox CJ, Danska JS 1997 IL-4 expression at the onset of islet inflammation predicts nondestructive insulitis in nonobese diabetic mice. J Immunol 158: 2414–2424
Campbell IL, Kay TW, Oxbrow L, Harrison LC 1991 Essential role for interferon-gamma and interleukin-6 in autoimmune insulin-dependent diabetes in NOD/Wehi mice. J Clin Invest 87: 739–742
Debray-Sachs M, Carnaud C, Boitard C, Cohen H, Gresser I, Bedossa P, Bach JF 1991 Prevention of diabetes in NOD mice treated with antibody to murine IFN gamma. J Autoimmun 4: 237–248
Bottazzo GF, Dean BM, McNally JM, MacKay EH, Swift PG, Gamble DR 1985 In situ characterization of autoimmune phenomena and expression of HLA molecules in the pancreas in diabetic insulitis. N Engl J Med 313: 353–360
Hanninen A, Jalkanen S, Salmi M, Toikkanen S, Nikolakaros G, Simell O 1992 Macrophages, T cell receptor usage, and endothelial cell activation in the pancreas at the onset of insulin-dependent diabetes mellitus. J Clin Invest 90: 1901–1910
Somoza N, Vargas F, Roura-Mir C, Vives-Pi M, Fernandez-Figueras MT, Ariza A, Gomis R, Bragado R, Marti M, Jaraquemada D, Pujol-Borrell R 1994 Pancreas in recent onset insulin-dependent diabetes mellitus. Changes in HLA, adhesion molecules and autoantigens, restricted T cell receptor V beta usage, and cytokine profile. J Immunol 153: 1360–1377
Itoh N, Hanafusa T, Miyazaki A, Miyagawa J, Yamagata K, Yamamoto K, Waguri M, Imagawa A, Tamura S, Inada M, Kawata S, Tarui S, Kono N, Matsuzawa Y 1993 Mononuclear cell infiltration and its relation to the expression of major histocompatibility complex antigens and adhesion molecules in pancreas biopsy specimens from newly diagnosed insulin-dependent diabetes mellitus patients. J Clin Invest 92: 2313–2322
Huang X, Yuang J, Goddard A, Foulis A, James RF, Lernmark A, Pujol-Borrell R, Rabinovitch A, Somoza N, Stewart TA 1995 Interferon expression in the pancreases of patients with type I diabetes. Diabetes 44: 658–664
Wilson SB, Kent SC, Patton KT, Orban T, Jackson RA, Exley M, Porcelli S, Schatz DA, Atkinson MA, Balk SP, Strominger JL, Hafler DA 1998 Extreme Th1 bias of invariant Valpha24JalphaQ T cells in type 1 diabetes. Nature 391: 177–81
Petersen JS, Kulmala P, Clausen JT, Knip M, Dyrberg T 1999 Progression to type 1 diabetes is associated with a change in the immunoglobulin isotype profile of autoantibodies to glutamic acid decarboxylase (GAD65). Clin Immunol 90: 276–281
Nelms K, Keegan AD, Zamorano J, Ryan JJ, Paul WE 1999 The IL-4 receptor: signaling mechanisms and biological functions. Annu Rev Immunol 17: 701–738
Song Z, Casolaro V, Chen R, Georas SN, Monos D, Ono SJ 1996 Polymorphic nucleotides within the human IL-4 promoter that mediate overexpression of the gene. J Immunol 156: 424–429
Hershey GK, Friedrich MF, Esswein LA, Thomas ML, Chatila TA 1997 The association of atopy with a gain-of-function mutation in the alpha subunit of the interleukin-4 receptor [see comments]. N Engl J Med 337: 1720–1725
Mitsuyasu H, Izuhara K, Mao XQ, Gao PS, Arinobu Y, Enomoto T, Kawai M, Sasaki S, Dake Y, Hamasaki N, Shirakawa T, Hopkin JM 1998 Ile50Val variant of IL4R alpha upregulates IgE synthesis and associates with atopic asthma [letter]. Nat Genet 19: 119–120
Deichmann KA, Heinzmann A, Forster J, Dischinger S, Mehl C, Brueggenolte E, Hildebrandt F, Moseler M, Kuehr J 1998 Linkage and allelic association of atopy and markers flanking the IL4- receptor gene. Clin Exp Allergy 28: 151–155
Luo DF, Buzzetti R, Rotter JI, Maclaren NK, Raffel LJ, Nistico L, Giovannini C, Pozzilli P, Thomson G, She JX 1996 Confirmation of three susceptibility genes to insulin-dependent diabetes mellitus: IDDM4, IDDM5 and IDDM8. Hum Mol Genet 5: 693–698
Deng GY, Muir A, Maclaren NK, She JX 1995 Association of LMP2 and LMP7 genes within the major histocompatibility complex with insulin-dependent diabetes mellitus: population and family studies. Am J Hum Genet 56: 528–534
Marron MP, Raffel LJ, Garchon HJ, Jacob CO, Serrano-Rios M, Martinez Larrad MT, Teng WP, Park Y, Zhang ZX, Goldstein DR, Tao YW, Beaurain G, Bach JF, Huang HS, Luo DF, Zeidler A, Rotter JI, Yang MC, Modilevsky T, Maclaren NK, She JX 1997 Insulin-dependent diabetes mellitus (IDDM) is associated with CTLA4 polymorphisms in multiple ethnic groups. Hum Mol Genet 6: 1275–1282
Risch N 1990 Linkage strategies for genetically complex traits. Am J Hum Genet 46: 229–241
Spielman RS, Mcginnis RE, Ewens WJ 1993 Transmission test for linkage disequilibrium: The insulin gene region and insulin-dependent diabetes mellitus (IDDM). Am J Hum Genet 52: 506–512
Becker KG 1999 Comparative genetics of type 1 diabetes and autoimmune disease. Diabetes 48: 1353–1358
She JX, Marron MP 1998 Genetic Susceptibility factors in type 1 diabetes: linkage, disequilibrium and functional analyses. Curr Opin Immunol 10: 682–689
Burchard EG, Silverman EK, Rosenwasser LJ, Borish L, Yandava C, Pillari A, Weiss ST, Hasday J, Lilly CM, Ford JG, Drazen JM 1999 Association between a sequence variant in the IL-4 gene promotor and FEV(1) in asthma. Am J Respir Crit Care Med 160: 919–922
Rosenwasser LJ, Borish L 1998 Promotor polymorphisms predisposing to the development of asthma and atopy. Clin Exp Allergy 28: 13–15
Acknowledgements
The authors thank Drs. Paolo Pozzilli, Henri-Jean Garchon, Manuel Serrano-Rios, Maria T. Martinez Larrad, and Jean-Francois Bach for providing DNA samples and Dr. Mark Yang and James Yang for data analyses.
Author information
Authors and Affiliations
Additional information
This work was supported by grants RO1 DK 50220, RO1 DK 53105, and PO1 AI 42288 from the National Institutes of Health.
Rights and permissions
About this article
Cite this article
Reimsnider, S., Eckenrode, S., Marron, M. et al. IL4 and IL4R α Genes Are Not Linked or Associated with Type 1 Diabetes. Pediatr Res 47, 246 (2000). https://doi.org/10.1203/00006450-200002000-00016
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/00006450-200002000-00016
This article is cited by
-
Association analysis of SNPs in the IL4R locus with type I diabetes
Genes & Immunity (2009)
-
Lack of association of type 1 diabetes with the IL4R gene
Diabetologia (2006)
-
Testing the possible negative association of type 1 diabetes and atopic disease by analysis of the interleukin 4 receptor gene
Genes & Immunity (2003)