Abstract
We report a novel inborn error of metabolism identified in a child with an unusual neurodegenerative disease. The male patient was born at term and recovered well from a postnatal episode of metabolic decompensation and lactic acidosis. Psychomotor development in the first year of life was only moderately delayed. After 14 mo of age, there was progressive loss of mental and motor skills; at 2 years of age, he was severely retarded with marked restlessness, choreoathetoid movements, absence of directed hand movements, marked hypotonia and little reaction to external stimuli. Notable laboratory findings included marked elevations of urinary 2-methyl-3-hydroxybutyrate and tiglylglycine without elevation of 2-methylacetoacetate, mild elevations of lactate in CSF and blood, and a slightly abnormal acylcarnitine profile. These abnormalities became more apparent after isoleucine challenge. Enzyme studies showed absent activity of 2-methyl-3-hydroxybutyryl-CoA dehydrogenase (MHBD) in the mitochondrial oxidation of 2-methyl branched-chain fatty acids and isoleucine. Under dietary isoleucine restriction, neurologic symptoms stabilized over the next 7 months.
Similar content being viewed by others
Main
Most enzymes involved in the mitochondrial oxidation of straight-chain fatty acids have been identified, as well as the corresponding genetic diseases such as medium-chain acyl-CoA dehydrogenase deficiency. The metabolism of branched-chain fatty acids, however, is not as well characterized. Short 2-methyl branched-chain carboxylic acids arise from both the breakdown of 2-methyl long-chain fatty acids, such as pristanic acid, and isoleucine catabolism. The four enzymes involved in the mitochondrial beta-oxidation of these compounds have been established (Fig. 1). Recently, one patient with isolated 2-methylbutyryl-CoA dehydrogenase deficiency has been described(1). Otherwise, only patients with a genetic deficiency at the level of the 2-methyl branched-chain specific 3-ketothiolase, an enzyme that also has an important function in ketone body utilization, have been reported.
In this paper we report the identification of the first patient with a genetic deficiency of 2-methyl-3-hydroxybutyryl-CoA dehydrogenase (MHBD, EC 1.1.1.178)(2), an isolated defect in the mitochondrial oxidation of 2-methyl branched-chain fatty acids and isoleucine.
CASE REPORT
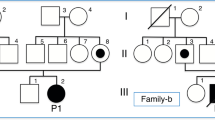
The affected boy is the first child of an unrelated German couple and was born at term. There was a family history of hemophilia A, which was diagnosed after birth. On the 2nd day of life, the boy developed tachydyspnea and metabolic acidosis with severe hypoglycemia (0.17 mmol/L), elevated lactate (11.6 mmol/L), mild hyperammonemia (210 μmol/L), and ketonuria. Seizure-like movements were observed but stopped without treatment. The child recovered under i.v. glucose infusion; no diagnosis was made. Urinary organic acid analysis at 2 1/2 months revealed marked excretion of tiglylglycine and 2-methyl-3-hydroxybutyrate, which was interpreted as diagnostic of 3-ketothiolase deficiency. The boy achieved head control at the age of 4 mo and sat with support at 8 mo. At the age of 13 mo, the boy moved by rolling from side to side, was able to sit by himself, and to stand when held by both hands. Expressive and receptive language as well as mental development were obviously retarded, emotional reactions were appropriate for his age. After 14 mo of age, coinciding with a vaccination, he started to show progressive loss of motor skills. He lost the ability to stand or sit and developed marked restlessness and choreoathetoid movements. Visual contact was lost, ophthalmologic investigations indicated nonpigmentary retinal degeneration verging on blindness, with normal nerve conduction latency. Acoustic evoked potentials were normal. During the next weeks the child developed epileptic seizures in the form of repeated head dropping and a modified hypsarrhythmia-pattern upon EEG. Treatment with vigabatrin reduced the frequency of seizures but the boy did not become seizure-free. An MRI scan of the brain revealed slight frontotemporal atrophy but no pathology of basal ganglia or significant white matter changes. At the age of 2 years, the boy was severely retarded with marked restlessness, choreoathetoid movements, absence of directed hand movements, marked hypotonia, and little reaction to external stimuli. In view of the clinical course, the diagnosis of 3-ketothiolase deficiency was reconsidered, and further metabolic investigations were conducted. All investigations were performed with informed consent.
Biochemical studies.
Specific biochemical findings are summarized in Table 1. Urinary organic acids by gas-chromatography mass-spectroscopy revealed constant, marked elevations of 3-hydroxy-2-methylbutyrate and tiglylglycine without elevation of 2-methylacetoacetate; plasma organic acids were normal. Urinary orotic acid, purines, and pyrimidines were normal. Lactate was repeatedly mildly elevated in blood and CSF. Normal plasma results were obtained for electrolytes; liver enzymes; amino acids; total, free and acyl-bound carnitine; very long-chain and long-chain fatty acids; phytanic and pristanic acids as well as bile acids. Tandem mass spectroscopy analysis of dried blood spots showed intermittent borderline elevations of C5:1-(tiglyl-)carnitine as well as C5-OH-(2-methyl-3-hydroxybutyryl-)carnitine. CSF neurotransmitter analysis revealed moderate elevations of the dopamine metabolite hydroxyvanillic acid (824 nmol/L, controls 429–729) and the serotonin metabolite 5-hydroxyindolacetic acid (330 nmol/L, controls 156–275). Normal values were obtained for CSF protein, glucose, amino acids, folate, and pterins.
An oral isoleucine challenge with 100 mg/kg body weight was conducted (Fig. 2). Plasma isoleucine (norm 28–95 μmol/L) rose to a concentration of 780 μmol/L within the first 30 min and was still elevated after 4 h (230 μmol/L). Blood lactate rose from 2.1 to 3.0 mmol/L in the first 30 min and later returned to borderline values. Urinary organic acids showed a marked increase in the excretion of 2-methyl-3-hydroxybutyrate and tiglylglycine in the sample collected 0–2 h after isoleucine challenge, which was further increased in the 3- to 8-h sample and decreased in the 9- to 14-h sample. Even following the challenge with isoleucine there was no elevation of 2-methylacetoacetate. There was mild excretion of 2-keto-3-methylvaleric acid particularly in the urine collected 3–8 h post-challenge. Plasma organic acid analysis showed traces of 3-hydroxy-2-methylbutyrate 4 h after isoleucine challenge (normally undetectable).
Plasma isoleucine (A) and urinary tiglylglycine and 2-methyl-3-hydroxybutyrate [MHB] concentrations (B) during isoleucine challenge test. Plasma samples were obtained before administration of isoleucine and after 30, 60, 90, 120, and 240 min. Urine was collected in separate fractions before and 0–2, 3–8, 9–14 h after administration of isoleucine.
Enzyme studies.
MHBD activity in fibroblasts was measured spectrophotometrically by following the increase in absorbance at 340 nm. The standard reaction medium contained the following components: 100 mM CHES-buffer pH 9.0; 0.1% (wt/vol) Triton X-100; 1 mM NAD; 4 U/mL crotonase; and 300 μg/mL fibroblast homogenate protein. Reactions were started by adding tiglyl-CoA at a concentration of 100 μmol/L. These analyses showed a virtually complete absence of MHBD activity, measured as 0.02 nmol/min·mg (controls 1.48 ± 0.12, n = 3). Activity measurements of other mitochondrial 3-hydroxyacyl-CoA dehydrogenases such as short-chain (SCHAD) and long-chain (LCHAD) 3-hydroxyacyl-CoA dehydrogenase as well as mitochondrial acetoacetyl-CoA lyase (3-ketothiolase) revealed normal values in the patient's fibroblasts.
Dietary treatment.
To reduce the production of pathologic metabolites, a special diet was introduced at the age of 2 y, with restriction of isoleucine to 350 mg/d and appropriate substitution of the other essential amino acids. Under this regimen the child showed no further deterioration of neurologic functions over the next 7 months. The restlessness, which had become very stressful for the parents, was markedly reduced and there was a decrease in the frequency of seizures.
DISCUSSION
Our results provide conclusive evidence indicating that our patient is affected by a novel inborn error of branched-chain fatty acids and isoleucine metabolism at the level of the enzyme MHBD. It represents a yet unknown neurodegenerative disorder with clinical features that differ markedly from other organic acidurias. The disease can be easily detected through urinary organic acid analysis but in our case the diagnosis remained obscure for some time as the metabolite pattern was thought to be indicative of mitochondrial acetoacetyl-CoA lyase (3-ketothiolase) deficiency. It is important to note that the acylcarnitine profile in our patient was only slightly abnormal, and the significance of this finding was not recognized on several occasions. It is possible, nevertheless, that the disorder may be recognizable in neonatal screening by acylcarnitine analysis. Enzymatic confirmation is possible in fibroblasts (this study) and leukocytes (authors' unpublished observations).
The pathogenesis of neurodegeneration in our patient is unclear. The initial presentation with severe metabolic acidosis, highly elevated lactate, hyperammonemia and hypoglycemia at the 2nd day of life was suggestive of an organic aciduria and implies that under catabolic conditions, metabolites that accumulate in MHBD deficiency may interfere with mitochondrial energy metabolism. However, the subsequent clinical course was atypical as there were no further episodes of acute metabolic decompensation and instead the boy showed signs of progressive neurodegeneration in the 2nd year of life. He turned from a communicative infant who appeared mildly delayed in his motor development into a blind, agitated child with undirected choreoathetotic movements and little reaction to external stimuli. There was no clinical or neuroradiological evidence of demyelination, and the retinopathy and mild cortical atrophy are more likely to reflect diffuse neuronal damage.
It is unlikely that the boy's hemophilia has had any impact on his development and the clinical course of MHBD deficiency. The diagnosis was made immediately after birth and there were no major bleeds. Neither is there evidence of a genetic link between the two disorders. Molecular analysis of the factor VIII gene revealed a distal intron 22-inversion, which is well described as cause of hemophilia A in more than one third of patients(3).
Neurodegeneration as observed in our patient has not been reported in mitochondrial acetoacetyl-CoA lyase (3-ketothiolase) deficiency despite high levels of 2-methyl-3-hydroxybutyrate and tiglylglycine. The clinical features of that disorder are usually attributed to impaired ketolysis, which is not disturbed in MHBD deficiency. Patients with 3-ketothiolase deficiency typically suffer intermittent, severe ketoacidosis with vomiting and hematemesis, which may progress to coma and death. The majority of patients develop normally but others show variable psychomotor retardation that is usually considered to be a result of the acute decompensations. It is possible that in nervous tissue, 2-methyl-3-ketoacyl-CoA esters that accumulate in 3-ketothiolase deficiency are sufficiently metabolized by one of the other thiolases(4) and that the urinary metabolite pattern does not exactly reflect the metabolic situation in the brain. Interestingly, a neurodegenerative disease with a course somewhat similar to that observed in our patient has been described in cytosolic acetoacetyl-CoA thiolase deficiency(5, 6). One of the two patients reported developed normally in the first months of life but subsequently started to lose acquired motor skills and showed ataxic and choreatiform movements; blood lactate was consistently elevated. However, cytosolic acetoacetyl-CoA thiolase is required for sterol biosynthesis, and it has been suggested that the clinical features might be due to a disturbance in this pathway, which would not be expected to be affected in MHBD deficiency.
2-Methyl branched-chain fatty acids also derive from certain fatty acids such as pristanic acid that are shortened through peroxisomal beta-oxidation up to a chain-length of 11 C atoms (4,8-dimethyl nonanoyl-CoA) and transferred to the mitochondria for complete oxidation. The clinical features in our patient were reminiscent of the neurologic and ophthalmological manifestations observed in some generalized peroxisomal disorders, which prompted us to determine the plasma concentration of various fatty acids as well as bile acid intermediates known to be oxidized in peroxisomes. The analyses in our patient did not reveal any abnormalities, but nevertheless it remains possible that MHBD deficiency exerts a neurodegenerative effect through certain 2-methyl branched-chain fatty acids that might accumulate in nervous tissue.
It is noteworthy that the CSF concentrations of the main metabolites of the neurotransmitters dopamine and serotonine were elevated. This is in contrast to other children with metabolic encephalopathy who usually show decreased concentrations of these compounds due to a decreased number of active neurons or decreased neuronal activity.
MHBD deficiency in our patient was originally misdiagnosed as 3-ketothiolase deficiency, and it is possible that this may have occurred in other patients. Indeed, a group of four children with variable clinical features and the same urinary organic acid profile as our patient has been reported(7, 8). The urinary concentrations of 2-methyl-3-hydroxybutyrate and tiglylglycine in these patients strongly increased after isoleucine loading while 2-methylacetoacetate remained undetectable. 3-Ketothiolase activity was normal, but MHBD deficiency was not considered.
In conclusion, we have reported a patient with progressive neurodegeneration caused by a novel defect in the metabolism of short branched-chain fatty acid oxidation and isoleucine metabolism. The patient's condition improved under dietary isoleucine reduction. It remains to be seen whether treatment may prevent neurodegeneration in other patients with this disease, which may be recognized through urinary organic acid analysis or possibly neonatal screening by tandem mass spectroscopy.
Abbreviations
- MHBD,:
-
2-methyl-3-hydroxybutyryl-CoA dehydrogenase
References
Gibson KM, Burlingame G, Hogema B, Jakobs C, Schutgens RBH, Millington D, Roe CR, Roe DS, Sweetman L, Steiner RD, Linck L, Pohowalla P, Sacks M, Kiss D, Rinaldo P, Vockley J 2000 2-Methlybutyryl-Coenzyme A dehydrogenase deficiency: a new inborn error of L-isoleucine metabolism. Pediatr Res 47: 830–833.
Luo MJ, Mao LF, Schulz H 1995 Short-chain 3-hydroxy-2-methylacyl-CoA dehydrogenase from rat liver: purification and characterisation of a novel enzyme of isoleucine metabolism. Arch Biochem Biophys 321: 214–220.
Lakich D, Kazazian HH, Antonarakis SE, Gitschier J 1993 Inversions disrupting the factor VIII gene are a common cause of severe haemophilia A. Nat Genet 5: 236–241.
Middleton B, Bartlett K 1983 The synthesis and characterisation of 2-methylacetoacetyl coenzyme A and its use in the identification of the site of the defect in 2-methylaceto-acetic and 2-methyl-3-hydroxybutyric aciduria. Clin Chim Acta 128: 291–305.
De Groot CJ, Haan GL, Hulstaert CE, Hoomes FA 1977 A patient with severe neurologic symptoms and acetoacetyl-CoA thiolase deficiency. Pediatr Res 11: 1112–1116.
Bennett MJ, Hosking GP, Smith MF, Gray RG, Middleton B 1984 Biochemical investigations on a patient with a defect in cytosolic acetoacetyl-CoA thiolase, associated with mental retardation. J Inherit Metab Dis 7: 125–128.
Iden P, Middleton B, Robinson BH, Sherwood WG, Gibson KM, Sweetman L, Sowik O 1990 3-Oxothiolase activities and [14C]-2-methylbutanoic acid incorporation in cultured fibroblasts from 13 cases of suspected 3-oxothiolase deficiency. Pediatr Res 28: 518–522.
Aramaki S, Lehotay D, Sweetman L, Nyhan WL, Winter SC, Middleton B 1991 Urinary excretion of 2-methylacetoacetate, 2-methyl-3-hydroxybutyrate and tiglylglycine after isoleucine loading in the diagnosis of 2-methylacetoacetyl-CoA thiolase deficiency. J Inherit Metab Dis 14: 63–74.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Zschocke, J., Ruiter, J., Brand, J. et al. Progressive Infantile Neurodegeneration Caused by 2-Methyl-3-Hydroxybutyryl-CoA Dehydrogenase Deficiency: A Novel Inborn Error of Branched-Chain Fatty Acid and Isoleucine Metabolism. Pediatr Res 48, 852–855 (2000). https://doi.org/10.1203/00006450-200012000-00025
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/00006450-200012000-00025
This article is cited by
-
Lost in promiscuity? An evolutionary and biochemical evaluation of HSD10 function in cardiolipin metabolism
Cellular and Molecular Life Sciences (2022)
-
Recent advances in understanding beta-ketothiolase (mitochondrial acetoacetyl-CoA thiolase, T2) deficiency
Journal of Human Genetics (2019)
-
Divergent Expression Patterns of Drp1 and HSD10 in the Nigro-Striatum of Two Mice Strains Based on their MPTP Susceptibility
Neurotoxicity Research (2019)
-
Enzymes involved in branched-chain amino acid metabolism in humans
Amino Acids (2017)