Abstract
The allergy-preventing effect of breast-feeding remains controversial, possibly because of individual variations in the composition of the breast milk. The aim of this study was to investigate the concentrations of cytokines involved in allergic reactions and IgA antibody production in breast milk from allergic and nonallergic mothers. The cytokine concentrations were determined in colostrum and 1-mo milk samples from 24 mothers with, and 25 mothers without, atopic symptoms, using commercial ELISA kits. The immunosuppressive cytokine transforming growth factor-β was predominant and was detectable in all milk samples. IL-6 was detected in the majority of colostral and mature milk samples, whereas the other cytokines were less commonly detected. The concentrations of IL-6, IL-10, and transforming growth factor-β, which are all involved in IgA synthesis, correlated with each other and with total IgA concentrations in colostrum. The concentrations of IL-4 were higher in colostrum from allergic than nonallergic mothers, and similar trends were seen for IL-5 and IL-13. In conclusion, transforming growth factor-β and IL-6 were the predominant cytokines in human milk. The correlation between the concentrations of cytokines involved in IgA synthesis, i.e. IL-10, IL-6, and transforming growth factor-β, may explain the stimulatory effect on IgA production in breast-fed babies. Varying concentrations of IL-4, IL-5, and IL-13 may explain some of the controversy regarding the possible allergy-preventive effect of breast-feeding.
Similar content being viewed by others
Main
The immune system of a newborn infant is not fully developed, and susceptibility to bacterial and viral infections is enhanced during infancy and early childhood. During this same period, allergic sensitization to environmental allergens most commonly occurs (1). The immune system of the newborn infant is influenced by maternal immunity, both transplacentally (2) and by the breast milk (3). There is a close immunologic interaction between the mother and her baby during gestation and the period of breast-feeding, and the mother may provide her offspring with protective factors and immune-modifying components, as well as antigenic stimulation.
Human milk contains numerous components protecting the infant against infections, including such factors that provide specific immunity, e.g. antibodies and viable lymphocytes (4). It also contains nonspecific protective factors, such as the iron-chelating protein lactoferrin, lysozyme, oligosaccharides acting as receptor analogs inhibiting the binding of bacterial pathogens and their toxins, and lipids that may disrupt enveloped viruses (4). Components enhancing the maturation of the infant's immune system may also be present in human milk. Moreover, cytokines (5) and their receptors (6) and cytokine production stimulating factors (7) are present in breast milk.
The precise relationship between breast-feeding and infant allergy is poorly understood, and the results from different studies are controversial (8, 9). One explanation for this controversy may be that the immunoprotection conferred by human milk may vary from mother to mother.
Immune responses to allergens are characterized by a cross-regulation between competing Th1-like and Th2-like cell populations. Atopic allergy, however, is associated with a bias to production of type-2 cytokines (10), e.g. IL-4 and IL-5. IL-4 and IL-13, produced by Th0, Th1, and Th2 cell populations, stimulate IgE synthesis, and IL-5 enhances chemotaxis (11), prolonged survival (12), and degranulation of eosinophils (13). In contrast, IFN-γ from Th1 cells inhibits IgE synthesis (14). Other cytokines involved in the IgE synthesis include the stimulatory IL-6 (15) and the inhibitory IL-10 (16) and TGF-β (17). It has also been suggested that these cytokines are involved in IgA production. Consequently, the higher concentrations of food allergen-specific IgA seen in breast milk of nonatopic, compared with atopic, mothers [R. Casas, M.F. Böttcher, K. Duchén, B. Björkstén, unpublished experiments; (18)] could possibly be explained by low concentrations of these cytokines in atopic mothers.
The aim of this study was to compare the concentrations of TGF-β1, TGF-β2, IFN-γ, IL-4, IL-5, IL-6, IL-10, and IL-13 in human milk from allergic and nonallergic mothers, i.e. cytokines that are involved in allergic reactions and IgA antibody production.
MATERIAL AND METHODS
Subjects.
From March 1996, pregnant women and their families were asked by the midwives at the maternity clinics in the Linköping area, county of Östergötland, Sweden, to participate in a prospective study. Forty-nine of these mothers were selected for the present study, on the basis of the availability of breast milk samples. The women received verbal and written information about the aim and design of the study. After having accepted participation, the atopic history, i.e. allergic rhinoconjunctivitis, bronchial asthma, or flexural, itchy dermatitis, was recorded by an experienced allergy research nurse for each mother during an initial interview. Except for allergy, none of the mothers had any autoimmune or other chronic disease. Twenty-four mothers had a history of atopic symptoms, whereas 25 did not. The mothers were then further divided into allergic (n = 19) and nonallergic (n = 20) groups on the basis of the symptoms and a positive or negative response to a screening test for IgE antibodies to a panel of inhalant allergens (Magic Lite SQ Allergy Screen, ALK, Hørsholm, Denmark).
Collection and processing of breast milk samples.
Colostrum was collected 3 - 4 d postpartum, and mature milk at 1, 2, and 3 mo. In this study, only the colostral and the 1-mo samples were used. The mothers collected the milk at home in sterile plastic tubes, using a manual breast-pump. The samples were immediately frozen at −20°C and later transported to the hospital and stored at −20°C until analysis, which was performed within 2 y.
After thawing, the breast milk fatty layer and the cellular elements were removed by two centrifugations. The first was performed at 680 ×g for 10 min at 4°C, after which the supernatants were removed and centrifuged at 10 000 ×g for 30 min at 4°C. Some of the resulting translucent whey was immediately used for measurement of IFN-γ, and the rest was stored in aliquots in plastic tubes at −20°C.
Cytokine assay.
The concentrations of IFN-γ, IL-4, IL-6, IL-10, and IL-13 in breast milk were analyzed using commercial ELISA kits (CLB Pelikine Compact human IFN-γ, IL-4, IL-6, IL-10, and IL-13, Research Diagnostics Inc., Flandern, NJ). The assays were performed according to the manufacturer's recommendation, continuously shaking the plate during the incubations. Before analyzing the samples for IFN-γ, the ELISA kit was tested with three different colostrum samples, kindly provided by Dr. Armond Goldman. These three samples were all from mothers who delivered their babies by cesarean section. The cutoff concentrations were 67 pg/mL for IFN-γ, 5.6 pg/mL for IL-4, 5.6 pg/mL for IL-6, 19 pg/mL for IL-10, and 3.2 pg/mL for IL-13. The concentrations of TGF-β1 and TGF-β2 were analyzed with commercial ELISA kits from R&D (R&D Systems Inc., Minneapolis, MN) according to the manufacturer's protocol. The cutoff concentrations were 125 and 250 pg/mL, respectively. The assay was performed after acid treatment to preactivate latent TGF-β, 10 μL of 1.2 N HCl per 100 μL of sample for 15 min at room temperature, followed by neutralization by adding 25 μL of 0.5 M HEPES/0.72 M NaOH per 100 μL of sample (19).
The concentrations of IL-5 were analyzed on high-binding, half-area Costar 3690 plates, coated with 50 μL/well of 0.25 μg/mL monoclonal rat anti-human IL-5 (clone no. TRFK5, Pharmingen, Becton-Dickinson, Stockholm, Sweden), diluted in carbonate buffer (pH = 9.2). The plates were incubated for 1 h at room temperature under continuous shaking and then at 4°C overnight. The following incubations were performed in the dark at room temperature with shaking for 1 h unless otherwise stated. After the incubations, the plates were washed four times in PBS, pH = 7.5, with 0.05% Tween. Free plastic spaces were blocked with 100 μL/well of a blocking solution (CLB). After incubation and washing, samples and standards, or for controls, buffer solution (CLB) only, were added to the plates at 50 μL/well. Recombinant human IL-5 (Pharmingen, Becton-Dickinson) diluted 2-fold in dilution buffer (range, 3.1–200 pg/mL) was used as a standard. The plates were incubated and washed, and 50 μL of the 1.0-μg/mL monoclonal biotinylated rat anti-human IL-5 (clone no. JES1–5A10, Pharmingen, Becton-Dickinson) was added. After incubation and washing, 50 μL of streptavidin-conjugated poly-horseradish peroxidase (in CLB) diluted 1/10 000 in dilution buffer was added to each well. After 30 min of incubation and the washing step, 50 μL/well of the substrate, tetramethylbenzidine (Sigma Chemical Co.-Aldrich, Stockholm, Sweden), was added to the wells. The substrate reaction was stopped after 30 min by adding 50 μL/well of 1.8 M sulfuric acid. The OD values of the samples and standards were measured at 450 nm, and the concentrations of IL-5 were determined by correlating the OD of the samples to the OD of the standard curve. All samples and standards were analyzed in duplicate, and the mean value was used. The OD values of the controls were subtracted from the OD of the standards and samples. Quantitative determinations could be performed at >6.2 pg/mL.
To evaluate the influence of breast milk components on the measured cytokine concentrations, known amounts of recombinant cytokines were added to a milk sample and then analyzed. In addition to the endogenous cytokine, 93–98% (means of two determinations) of the exogenous cytokine was detected for IL-4, IL-6, IL-10, IFN-γ, TGF-β1, and TGF-β2, although the recovery was lower for IL-13 (87%) and IL-5, for which it varied between 24 and 97% among four different samples.
Total IgA.
sIgA concentrations in the breast milk were analyzed on high-binding Costar 3590 plates. The plates were coated with 200 μL/well of polyclonal rabbit anti-human SC antibody (DakoPatts, Stockholm, Sweden), diluted 1/500 in PBS with 0.5% HSA (Chemicon, Stockholm, Sweden). The plates were incubated for 2 h in a moist chamber at 37°C and after that for at least 3 h at 4°C. After washing, the plates were blocked with 200 μL/well of PBS with 2% HSA. The plates were incubated in a moist chamber at 37°C for 2 h and then overnight at 4°C. The following incubations took place in a moist chamber at 37°C for 1 h unless otherwise stated. After washing, 100 μL of each standard and samples, diluted 1/8 000–1/32 000 in PHT, or, for controls, PHT only, were added to the wells in duplicate. Human IgA (Sigma), diluted 2-fold (range, 16–1000 ng/mL) in PHT, was used as a standard. The plates were washed and incubated with 100 μL/well of monoclonal mouse anti-human IgA antibody (clone 2D7, Bio-Zac AB, Järfälla, Sweden), diluted 1/2000 in PHT. After washing, the plates were incubated with 100 μL/well of alkaline phosphatase–conjugated rabbit anti-mouse antibody (Sigma), diluted 1/5000 in PHT. For detection, a conventional substrate system, FAST™ pNPP in tablet form (Sigma), was used. All washes were performed four times in PBS with 0.05% Tween.
After washing, 200 μL/well of FAST pNPP was added and allowed to react with the bound phosphatase at room temperature in the dark. The reaction was stopped after 30 min by adding 50 μL/well of 3 M sodium hydroxide. The OD was read at 405 nm. The OD values of the controls were subtracted from the values of the standard and the samples.
Collection and processing of serum samples.
Venous blood samples were drawn from the mothers at the maternity ward within 4 d after delivery. The blood was allowed to clot and then centrifuged. The serum samples were capped and stored at −20°C. The IgE concentrations were analyzed with Magic Lite Total IgE Extended Range Immunoassay system (ALK, Hørsholm, Denmark), as recommended by the manufacturer. IL-4, IL-5, IL-6, IL-10, IL-13, and IFN-γ were analyzed with the same assays as used for the breast milk samples. TGF-β was not analyzed inasmuch as it has been suggested that the major part of TGF-β detected in serum is released from platelets during the clotting process (20).
Statistics.
Because the concentrations of cytokines and antibodies were not normally distributed, paired analyses were performed with Wilcoxon signed rank test and unpaired analyses with Mann-Whitney U test, and correlations were analyzed with Spearman rank order correlation coefficient test. A probability level of <0.05 was considered to be statistically significant. Calculations were performed using the statistical package StatView 4.5 for Macintosh (Abacus Concepts Inc, Berkeley, CA).
Those samples that had concentrations below the cutoff were assigned a value corresponding to half the cutoff value.
Ethics.
The study was approved by the Regional Ethics Committee for Human Research at the University Hospital of Linköping.
Results
Cytokine concentrations in breast milk.
The median values and ranges of the analyzed cytokines are presented in Table 1. High concentrations of TGF-β1 and TGF-β2 were detected in all, and IL-6 in most samples, whereas IL-4, IL-10, and IL-13 were less commonly detected and IL-5 and IFN-γ were detected in <10% of the colostrum and 1-mo mature milk. Two of the three samples used for testing the IFN-γ ELISA had high concentrations of IFN-γ, and the third sample was just below the cutoff.
There were strong correlations between the concentrations in colostrum and mature milk for IL-4 (ρ = 0.78;p < 0.001), IL-6 (ρ = 0.60;p < 0.001), and IL-13 (ρ = 0.80;p < 0.001). The correlations were weaker for IL-10 (ρ = 0.43;p < 0.01), TGF-β1 (ρ = 0.36;p < 0.05), and TGF-β2 (ρ = 0.32;p < 0.05). No correlation analyses were performed for IL-5 and IFN-γ, as only few samples were positive for these cytokines.
The concentrations of IL-6 (p < 0.001), IL-13 (p < 0.05), TGF-β1 (p < 0.05), and TGF-β2 (p < 0.001) were significantly higher in colostrum compared with mature milk, whereas the concentrations of IL-4, IL-5, IL-10, and IFN-γ were similar in colostrum and mature milk.
The allergic, compared with the nonallergic, mothers had significantly higher concentrations of IL-4 in colostrum but not in mature milk (Fig. 1). A similar trend was seen for IL-13 (p = 0.11) and IL-5 (p = 0.13) in colostrum. The differences were not affected by pollen season. Thus, seven allergic and six nonallergic mothers collected their breast milk during the grass and tree pollen season. Of the nine mothers with allergic rhinoconjunctivitis to grass or birch pollen, four collected their colostrum within and five, outside the pollen season. The number of positive samples for IL-4 and the IL-4 concentrations were similar in the two groups.
Concentrations of IL-4 in colostrum from allergic and nonallergic mothers. The mothers were considered to be allergic if they had a history of allergic symptoms and a positive allergy screen, and nonallergic if they had no allergic symptoms and a negative allergy screen. Detection concentration was 5.6 pg/mL. The 50th, 75th, and 90th percentiles are indicated for column 1 and the 50th and 90th percentiles for column 2, as well as outliers.
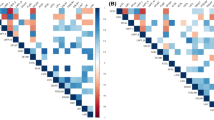
The concentrations of IL-4, IL-5, IL-10, and IL-13 correlated with each other (Table 2). The IL-6 concentrations correlated with the concentrations of TGF-β1, TGF-β2, and IL-10. The concentrations of IL-10 also tended to correlate with TGF-β1, and a moderate correlation was seen between TGF-β1 and TGF-β2 (Table 2).
Similar to colostrum, the concentrations of IL-4 and IL-13 in mature milk correlated strongly (ρ = 0.88;p < 0.001), and IL-6 correlated with TGF-β1 (ρ = 0.52;p < 0.001) and TGF-β2 (ρ = 0.32;p < 0.05). The correlation between the concentrations of IL-10 and IL-13 at 1 mo was even more pronounced (ρ = 0.54;p < 0.001) than in colostrum. There was also a correlation between IL-4 and IL-6 (ρ = 0.53;p < 0.001) in mature milk, but not in colostrum.
The median concentration of serum IgE was 44.3 μg/mL (range, 0.4–870 μg/mL), and the concentrations were higher in allergic than in nonallergic mothers (p < 0.001). None of the cytokines in breast milk correlated to IgE concentrations in serum (data not shown).
Correlations between cytokine and IgA concentrations.
The median IgA concentration in colostrum was 631 g/L (range, 152-3519 g/L) and in mature milk, 323 g/L (range, 16–738 g/L). Total IgA concentrations in colostrum correlated with IL-6 (ρ = 0.30;p < 0.05) and IL-10 (ρ = 0.40;p < 0.01) in colostrum. A similar trend was seen for the IgA and IL-6 concentrations in mature milk (ρ = 0.23;p = 0.13). Furthermore, samples with total IgA concentrations above the median in colostrum had higher concentrations of IL-6 and IL-10 (Fig. 2) than samples with lower IgA concentrations. A similar trend was seen for IgA and IL-6 in mature milk (p = 0.10).
Correlations between cytokine concentrations in breast milk andserum.
Fifteen, 33, 18, and 12 of 48 mothers had detectable serum concentrations of IL-4, IL-5, IL-6, and IL-13, respectively, whereas IL-10 and IFN-γ were only detected in one mother each. The serum concentrations of IL-4 and IL-13, but not the other cytokines, correlated weakly (ρ = 0.3–0.4;p < 0.05) with the concentrations in breast milk. The correlations were weak, however. The concentrations of IL-6 (p < 0.001) and IL-13 (p < 0.05) were higher in breast milk than in serum, whereas the concentrations of IL-5 were higher in serum (p < 0.001) and the concentrations of IL-4 were similar in the two fluids.
DISCUSSION
The observations may partly explain the anti-inflammatory properties of breast milk (4). All samples in our study were positive for TGF-β1 and TGF-β2, and almost all contained IL-6. Animal studies showing that TGF-β knockout mice die of a widespread inflammatory disease after weaning (21) suggest that TGF-β is an important anti-inflammatory substance in breast milk. We showed TGF-β to be present in a latent form that only exhibits physiologic action after acid activation. It is likely that such activation occurs in the baby when the milk is exposed to a low pH in the stomach. The presence of large quantities of this cytokine may explain why breast-fed babies have a reduced incidence of conditions with an autoregulated or dysregulated immunity, such as Crohn's disease (22) and insulin-dependent diabetes mellitus (23). Furthermore, TGF-β has also been proposed to down-regulate IgE synthesis (17). Varying concentrations of this cytokine in breast milk from different mothers may partly explain the controversy regarding the protective role of breast-feeding against allergy (24).
Similarly, IL-6 has recently been suggested to have anti-inflammatory and immunosuppressive properties (25). Also, IL-6 (26) and TGF-β, together with IL-10 (27), may have an indirect anti-inflammatory effect through stimulation of IgA synthesis. Antigen-specific IgA mediates exclusion of antigens, capable of provoking immune inflammatory responses. The concentrations of IgA correlated with IL-6 and IL-10 concentrations in breast milk. This is in agreement with an earlier study showing a relationship between high serum concentrations of IL-6 and elevated concentrations of IgA1 and IgA2 (28). This may shed some light on the contradictory studies reporting the enhanced effect of breast-feeding on IgA production in children (29, 30).
IL-10 was detected only in 12 and 6% of the colostrum and mature milk samples. This is in contrast with the results from another study (31), in which high concentrations of IL-10 were found in most colostrum samples. In that study, high concentrations of IL-10 were detected in samples collected during the first 24 h, although the concentrations were lower in milk collected later. The colostrum samples in our study were collected 3–4 d postpartum, which may explain the low concentrations of IL-10.
The low concentrations of IFN-γ are in agreement with some (32, 33), but not all, previous studies (34–36). In one of the latter studies (35) IFN-γ was only detected in unfractionated breast milk from mothers who delivered their babies by cesarean section. None of the mothers in our study delivered their babies by cesarean section. We did, however, detect IFN-γ in two of three reference samples that were obtained from mothers who delivered by cesarean section. The mode of delivery is unknown for the mothers in the two other studies in which IFN-γ was detected (34, 36).
The concentrations of IL-4 in breast milk were low, and only a few samples were positive, confirming the results from earlier studies (33, 36). Similar results were seen for IL-5 and IL-13. The allergic mothers had higher colostrum concentrations of IL-4 than the nonallergic mothers. A similar trend was seen in a recent study (33). The allergic status of the mothers in that study (33) was not as strictly defined as in our study, which may explain why the difference in that study was not statistically significant. The concentrations of IL-5 and IL-13 also tended to be higher in colostrum from allergic mothers. This may explain why breast milk cell supernatants from atopic, but not from nonatopic, mothers stimulate IgE production by cord blood lymphocytes (37). These findings may be relevant in the controversy regarding the protective effect of breast-feeding against atopic sensitization in the children.
Except for the weak relationship between the concentrations of IL-4 and IL-13, there were no correlations between serum and breast milk concentrations for the different cytokines. The higher concentrations of IL-13 and IL-6 in breast milk compared with serum suggest that these cytokines are locally produced.
Low cytokine production in neonates (38) may in part be compensated by cytokines in the human milk. Some of the cytokines are bound to other proteins, e.g. to their receptors (31, 39), and are thereby protected from digestion. Furthermore, human milk contains antiproteases interfering with proteolysis, and the digestive capacity is not fully developed in the newborn (5).
The presence of TGF-β and IL-6 in human milk and the relationship between concentrations of cytokines involved in IgA synthesis, IL-10, IL-6, and TGF-β, may explain the enhanced IgA production in breast-fed, compared with formula-fed, babies. The higher concentrations of IL-4 in colostrum from allergic mothers and the similar trends for IL-5, IL-13, and IL-10 may in part explain the controversial results reported on the protective effect of breast-feeding against atopic sensitization in children.
Abbreviations
- Th:
-
T-helper
- TGF-β:
-
transforming growth factor-β
- IFN-γ:
-
interferon-γ
- sIg:
-
secretory immunoglobulin
- SC:
-
secretory component
- HSA:
-
human serum albumin
- PHT:
-
PBS with 0.05% Tween and 0.5% HSA
- pNPP:
-
p-nitrophenyl phosphate
References
Hattevig G, Kjellman B, Björkstén B 1993 Appearance of IgE antibodies to ingested and inhaled allergens during the first 12 years of life in atopic and non-atopic children. Pediatr Allergy Immunol 4: 182–186.
Billington WD 1992 The normal fetomaternal immune relationship. Clin Obstet Gynecol 6: 417–438.
Orlando S 1995 The immunologic significance of breast milk. J Obstet Gynecol Neonatal Nurs 24: 678–683.
Goldman AS 1993 The immune system of human milk: antimicrobial, antiinflammatory and immunomodulating properties. Pediatr Infect Dis J 12: 664–671.
Goldman AS, Chheda S, Garofalo R, Schmalstieg FC 1996 Cytokines in human milk: properties and potential effects upon the mammary gland and the neonate. J Mammary Gland Biol Neoplasia 1: 251–258.
Buescher ES, Malinowska I 1996 Soluble receptors and cytokine antagonists in human milk. Pediatr Res 40: 839–844.
Bessler H, Straussberg R, Hart J, Notti I, Sirota L 1996 Human colostrum stimulates cytokine production. Biol Neonate 69: 376–382.
Saarinen UM, Kajoraari M 1995 Breastfeeding as prophylaxis against atopic disease: prospective follow-up study until 17 years old. Lancet 346: 1065–1069.
van Asperen PP, Kemp AS, Mellis CM 1984 Relationship of the diet in the development of atopy in infancy. Clin Allergy 14: 525–532.
Romagnani S 1994 Lymphokine production by human T cells in disease states. Annu Rev Immunol 12: 227–257.
Venge J, Lampinen M, Håkansson L, Rak S, Venge P 1996 Identification of IL-5 and RANTES as a major eosinophil chemoattractants in the asthmatic lung. J Allergy Clin Immunol 97: 1110–1115.
Yamaguchi Y, Suda T, Ohta S, Tominaga K, Miura Y, Kasahara T 1991 Analysis of the survival of mature human eosinophils: interleukin-5 prevents apoptosis in mature human eosinophils. Blood 78: 2542–2547.
Horie S, Gleich GJ, Kita H 1996 Cytokines directly induce degranulation and superoxide production from human eosinophils. J Allergy Clin Immunol 98: 371–381.
Pène JF, Rousset F, Brière F, Chrétien I, Bonnefoy J-Y, Spits H, Yokota T, Aral K-I, Bancherau J, de Vries JE 1988 IgE production by normal human lymphocytes is induced by interleukin 4 and suppressed by interferons γ and α and prostaglandin E2 . Proc Natl Acad Sci U S A 85: 6880–6884.
Vercelli D, Jabara HH, Arai K-I, Yokota T, Geha RS 1989 Endogenous interleukin 6 plays an obligatory role in interleukin 4-dependent human IgE synthesis. Eur J Immunol 19: 1419–1424.
Punnonen J, de Waal Malefyt R, van Vlasselaer P, Gauchat J-F, de Vriers JE 1993 IL-10 and viral IL-10 prevent induced IgE synthesis by inhibiting the accessory cell function of monocytes. J Immunol 151: 1280–1289.
Wu YC, Brinkmann V, Cox D, Heusser C, Delespess G 1992 Modulation of human IgE synthesis by transforming growth factor-β. Clin Immunol Immunopathol 62: 277–284.
Renz H, Vestner R, Petzoldt S, Brehler C, Prinz H, Rieger CHL 1990 Elevated concentrations of salivary secretory immunoglobulin A anti-cow's milk protein in newborns at risk of allergy. Int Arch Allergy Appl Immunol 92: 247–253.
Srivastava MD, Srivastava A, Brouhard B, Saneto R, Groh-Wargo S, Kubit J 1996 Cytokines in human milk. Res Commun Mol Pathol Pharmacol 93: 263–287.
Kropf J, Schurek JO, Wollner A, Gressner AM 1997 Immunological measurement of transforming growth factor-beta I (TGF-βI) in blood; assay development and comparison. Clin Chem 43: 1965–1974.
Kulkarni AB, Karlsson S 1993 Transforming growth factor-β1 knockout mice: a mutation in one cytokine gene causes a dramatic inflammatory disease. Am J Pathol 143: 3–9.
Koletzko S, Sherman P, Corey M, Griffiths A, Smith C 1989 Role of infant feeding practices in development of Crohn's disease in childhood. BMJ 298: 1617–1618.
Mayer EJ, Hamman RF, Gay EC, Lezotte DC, Savitz DA, Klingensmith GJ 1988 Reduced risk of IDDM among breast fed children. Diabetes 37: 1625–1632.
Björkstén B 1983 Does breast feeding prevent the development of allergy?. Immunol Today 4: 215–217.
Tilg H, Dinarello CA, Mier JW 1997 IL-6 and APPs: anti-inflammatory and immunosuppressive mediators. Immunol Today 18: 428–432.
Fujihashi K, McGhee JR, Lue C, Beagley KW, Taga T, Hirano T, Kishimoto T, Mestecky J, Kiyono H 1991 Human appendix B cells naturally express receptors for and respond to interleukin 6 with selective IgA1 and IgA2 synthesis. J Clin Invest 88: 248–252.
Defrance T, Vanbervliet B, Brière F, Durand I, Rousset F, Banchereau J 1992 Interleukin 10 and transforming growth factor β cooperate to induce anti-CD40-activated naive human B cells to secrete immunoglobulin A. J Exp Med 175: 671–682.
Meillet D, Labrousse F, Benoit MO, Hernvann A, Musset L, Van Amerongen G 1997 Increased serum concentration of IgA2 subclass and IgA2/IgA1 ratio: specific markers of chronic alcoholic abuse?. Eur J Clin Chem Clin Biochem 35: 275–279.
Avanzini MA, Plebani A, Monafo V, Pasinetti G, Teani M, Colombo A, Mellander L, Carlsson B, Hanson LÅ, Ugazio AG, Burgio GR 1992 A comparison of secretory antibodies in breast-fed and formula-fed infants over the first six months of life. Acta Paediatr 81: 296–301.
Fitszimmons SP, Evans MK, Pearce CL, Sheridan MJ, Wientzen R, Cole MF 1994 Immunoglobulin A subclasses in infants' saliva and in saliva and milk from their mothers. J Pediatr 124: 566–573.
Garofalo R, Chheda S, Mei F, Palkowetz KH, Rudloff HE, Schmalstieg FC, Rassin DK, Goldman AS 1995 Interleukin-10 in human milk. Pediatr Res 37: 444–449.
Sone S, Tsutsumi H, Takeuchi R, Matsuda K, Imai S, Ogra PL, Chiba S 1997 Enhanced cytokine production by milk macrophages following infection with respiratory syncytial virus. J Leukoc Biol 61: 630–636.
Rudloff S, Niehues T, Rutsch M, Kunz C, Schroten H 1999 Inflammation markers and cytokines in breast milk of atopic and non-atopic women. Allergy 54: 206–211.
Basolo F, Conaldi PG, Fiore L, Calvo S, Toniolo A 1993 Normal breast epithelial cells produce interleukins 6 and 8 together with tumor-necrosis factor: defective IL6 expression in mammary carcinoma. Int J Cancer 55: 926–930.
Bocci V, von Bremen K, Corradeschi F, Franchi F, Luzzi E, Paulesu L 1993 Presence of interferon-γ and interleukin-6 in colostrum of normal women. Lymphokine Cytokine Res 12: 21–24.
Eglinton BA, Roberton DM, Cummins AG 1994 Phenotype of T cells, their soluble receptor levels, and cytokine profile of human breast milk. Immunol Cell Biol 72: 306–313.
Allardyce RA, Wilson A 1984 Breast milk supernatants from atopic donors stimulate cord blood IgE secretion in vitro. Clin Allergy 1984: 259–267.
Ehlers S, Smith KA 1991 Differentiation of T cell lymphokine gene expression: the in vitro acquisition of T cell memory. J Exp Med 173: 25–36.
Rudloff HE, Schmalstieg FC, Palkowetz KH, Paskiewicz EJ, Goldman AS 1993 Interleukin-6 in human milk. J Reprod Immunol 23: 13–20.
Acknowledgements
The authors thank Dr. Armond Goldman for kindly providing colostrum samples and for helpful discussions and Ulrika Leek and Lena Lindell for excellent technical assistance.
Author information
Authors and Affiliations
Additional information
Supported by the Swedish Medical Research Council (grant 7510), the Vårdal Foundation, the Foundation for Strategic Research, the National Swedish Association against Allergic disease, the National Heart and Lung association, and Glaxo-Wellcome.
Rights and permissions
About this article
Cite this article
Böttcher, M., Jenmalm, M., Garofalo, R. et al. Cytokines in Breast Milk from Allergic and Nonallergic Mothers. Pediatr Res 47, 157 (2000). https://doi.org/10.1203/00006450-200001000-00026
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/00006450-200001000-00026
This article is cited by
-
Effectiveness of immunization with multi-component bacterial immunomodulator in foals at 35th day of life
Scientific Reports (2022)
-
Active free secretory component and secretory IgA in human milk: do maternal vaccination, allergy, infection, mode of delivery, nutrition and active lifestyle change their concentrations?
Pediatric Research (2021)
-
Polymeric nanoassemblies for enrichment and detection of peptides and proteins in human breast milk
Analytical and Bioanalytical Chemistry (2020)
-
Effect of Multi-Microbial Probiotic Formulation Bokashi on Pro- and Anti-Inflammatory Cytokines Profile in the Serum, Colostrum and Milk of Sows, and in a Culture of Polymorphonuclear Cells Isolated from Colostrum
Probiotics and Antimicrobial Proteins (2019)
-
Contribution of early nutrition on the development of malnutrition and allergic diseases in the first year of life: a study protocol for the Mother and Infant Cohort Study (MICOS)
BMC Pediatrics (2018)