Abstract
Accurate interpretation of the results of GH stimulation tests is of pivotal importance not only in the evaluation of the etiology of growth retardation in children but also in the selection of the best candidates for GH therapy. We performed this study to test a novel immunofunctional GH ( IFGH) assay that makes use of the concept that one GH molecule dimerizes two GH receptors and compared the results with those obtained using two GH assays, the Diagnostic Systems Laboratories ELISA and a Hybritech immunoradiometric assay in 19 children with short stature undergoing routine GH stimulation testing. We also tested 13 normally statured control children to revisit the issue of what constitutes normal GH responses to stimuli, using all three assays and arginine and either L-dopa or insulin-induced hypoglycemia as secretagogues. Concentrations of IGF-I, IGF binding protein-3, and acid labile subunit were measured as well. There was a significant correlation between peak IFGH and Diagnostic Systems Laboratories ELISA GH responses to stimuli (r2 = 0.93) as well as between the Diagnostic Systems Laboratories ELISA and Hybritech immunoradiometric assay (r2 = 0.91). There were no significant differences between the short stature and normal group in peak or mean GH concentrations regardless of the assay used; however, the IGF-I, IGF binding protein-3, and acid labile subunit concentrations were substantially lower in the short stature group. There was a wide spectrum of GH concentrations in the normal group; ∼50% of the children had peak GH concentrations <7 ng/mL, ∼30% <5 ng/mL, and two pubertal normal subjects peaked to only 2 ng/mL with use of both the ELISA and IFGH assays. We conclude that 1) sensitive GH assays, ELISA and immunoradiometric assay, accurately detect a GH capable of generating a biologic signal comparable to an IFGH and 2) that normal GH stimulation test results can be substantially lower than previously accepted. GH-dependent growth factors may be more sensitive indicators of GH sufficiency than GH concentrations in response to pharmacologic stimuli.
Similar content being viewed by others
Main
The ultradian rhythm of GH release has made it difficult to precisely and accurately identify deficiency states in the human. Hence, the diagnosis of GH deficiency has become complex, requiring the assessment not only of anthropometric variables in children, height, weight, growth velocity, but also the measurement of growth factor concentrations and frequent blood sampling for the determination of GH concentrations. GH stimulation tests have become the standard of care in the assessment of the short child when deciding the GH secretory status. They are also helpful in assessing the potential therapeutic benefit of GH therapy in most children, and they are used routinely by more than 80% of practicing pediatric endocrinologists surveyed in the U.S. (1). The issue of what is a normal response to stimuli remains elusive, however, as it depends on the assay used and the normative data established for that particular assay (2).
Using first insulin-induced hypoglycemia and then arginine as stimuli, early investigators established that normal children peak to at least ∼5 ng/mL when challenged using a GH assay with a porcine MAb against human GH (3–5). Other secretagogues alone and in combination, such as propranolol and L-dopa (6), arginine and L-dopa (7), and clonidine (8), have all been used with variable results. More recently, analysis of the GH responses to many different pharmacologic stimuli in a very large group (n = 472) of normally growing short children revealed that many normal children failed to stimulate their serum GH concentrations, showing values significantly lower than conventionally assumed (9); however, when the GH releasing hormone combined with either arginine or the somatostatin inhibitor pyridostigmine is used, the minimum GH response is high (19 ng/mL). These authors, hence, claim that unless such powerful secretagogues are used, these tests cannot discriminate between sufficiency and deficiency in children (9). The cutoff peak serum GH concentration considered normal has also varied substantially in the last 20 y, ranging from 5 ng/mL (3) to 7 (10, 11) to 10 ng/mL most recently (12). It is clear that most endocrinologists in the U.S. have not adjusted their interpretation of stimulated GH results despite the lack of adequate assay-specific normative data; actually, a peak GH of <10 ng/mL is considered diagnostic of GH deficiency by more than 70% of the pediatric endocrinologists surveyed in the U.S. (1). Frequent blood sampling has been extensively used in research studies to estimate GH secretory patterns (13); however, frequent blood sampling does not appear to be more accurate than stimulated results in assessing GH sufficiency (14).
The development of GH therapy as replacement in adults with GH deficiency for purposes other than linear growth has given renewed relevance to the diagnostic quandary of what constitutes normal and abnormal GH secretory status. To the clinicians caring for adult GH-deficient patients, this is particularly critical because they don't have the advantage of measuring height and growth velocity in their patients as normally done in children. Hoffman et al. (15) have shown that in adults with evidence of extensive pituitary disease, peak GH responses to insulin-induced hypoglycemia are clearly lower than age, sex, and body mass index (BMI) matched normal subjects, with all normal subjects having a peak GH >5 ng/mL and all GH-deficient subjects having <3 ng/mL. Testing with insulin-induced hypoglycemia also had the greatest discriminative capacity for GH deficiency compared with 24-h GH concentration profiles or measurement of IGF-I or IGFBP-3 concentrations (15). These and other data led to the recommendation of a peak GH response to insulin-induced hypoglycemia of <3 ng/mL using a Hybritech monoclonal IRMA as the ultimate test of GH insufficiency in the adult (16).
A highly sensitive IFGH assay was developed recently that makes use of the concept that one GH molecule binds with two different GH receptors at two binding sites (17). It uses a recombinant GH binding protein (GHBP) specific against one binding site of GH and a MAb against the other binding site, measuring a GH molecule capable of dimerizing two receptors and, hence, capable of generating a biologic signal. We performed the present study to investigate the correlation between this new IFGH assay and two sensitive commercially available assays for GH, a DSL ELISA and the Hybritech IRMA from Nichols/Quest Diagnostics. We also revisited the issue of what constitutes normal levels of GH by using conventional GH stimulation tests in normally statured children as well as measuring IGF-I, IGFBP-3, and ALS concentrations. Short children undergoing clinical workup for GH sufficiency were studied and their data compared with those of a group of normally statured children.
METHODS
The present study was approved by the Nemours Children's Clinic Clinical Research Review Committee and the Institutional Review Committee at Wolfson Children's Hospital and at the University of Virginia.
Study subjects.
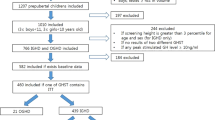
As part of the evaluation for SS and poor growth, a group of 19 children (11 males, 8 females) was recruited from our clinics after informed written consent from them (SS group) and their parents. Whether they had GH deficiency was not known before testing. One of the subjects had been treated for GH deficiency and had completed his linear growth and was undergoing retesting; hence, his height SD score (SDS) at the time of testing was no longer short (height SDS, 0.7). For comparison, a group of 13 healthy children (five males, eight females) was also recruited from the children of our medical center staff; by design, they were all of normal height (normal controls). Their clinical characteristics are summarized in Table 1.
Study design.
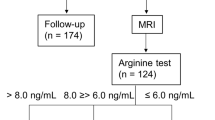
As part of their evaluation, the short children underwent a GH stimulation test using either arginine/L-dopa or arginine/insulin-induced hypoglycemia as pharmacologic stimuli. Permission was obtained for an extra milliliter of blood to be withdrawn at each time point for additional assays as detailed below. After an overnight fast, the subjects came either to the Wolfson Children's Hospital Clinical Research Center or to the University of Virginia Clinical Research Center in the early morning. After the skin was numbed with the anesthetic cream Emla (AstraZeneca, Wilmington, DE, U.S.A.), blood was withdrawn for several hormonal assays. Immediately afterward, L-dopa was given orally (either 250 or 500 mg, depending on weight), and an infusion of 10% arginine hydrochloride was begun at 0.5 g/kg infused over 30 min. Blood was withdrawn at times 0, 20, 40, 60, 90, and 120 min for determination of the GH concentrations. Plasma IGF-I, IGFBP-3, and ALS were measured at the same time points. The patients who underwent the arginine/insulin-induced hypoglycemia test (n = 6) received 0.075 U/kg of regular insulin (Humulin R, Eli Lilly, Indianapolis, IN, U.S.A.) after 60 min of sampling, and blood was withdrawn frequently during the 120 min of the test. Hypoglycemia was considered when plasma glucose was <40 mg%. One subject underwent insulin-induced hypoglycemia only. The normal controls all underwent an arginine L-dopa test.
Assays.
The DSL ELISA test was used to determine GH concentrations in these timed series. This is an enzymatically amplified 2-step sandwich-type immunoassay using a monoclonal anti-human GH antibody with a sensitivity of 0.03 ng/mL and an intra- and interassay coefficient of variation (CV) of 4 and 6%, respectively. The standards of this assay are calibrated against the World Health Organization standard code 88/624.
In addition, a DSL IFGH assay developed previously (17) was used to determine the GH concentration of GH molecules capable of binding at two different binding sites. This assay makes use of a MAb against binding site 2 of the GH molecule and a biotinylated recombinant GHBP that in turn binds to binding site 1 of GH. After incubation and washing, the wells are incubated with the biotinylated recombinant human GHBP and its binding to the GH molecule captured by adding streptavidin-labeled horseradish peroxidase. The absorbance measured is, hence, directly proportional to the concentration of biologically active intact GH that possesses both GH receptor binding sites. The sensitivity is 0.06 ng/mL with an intra- and interassay CV of 3 to 5% and 4 to 9%, respectively. The standards are also calibrated against World Health Organization code 88/624.
All patients in the SS group also had their GH concentrations measured by the Hybritech Tandem-R IRMA at Quest Diagnostic Laboratories (San Juan Capistrano, CA, U.S.A.). The assay uses two MAb against two sites of the GH molecule. The sensitivity is 0.2 ng/mL, and an intra- and interassay CV is 3 to 4% and 3 to 5%, respectively. A limited time series in the normal controls group was also analyzed with this assay at the DSL. The standards use the GH reference preparation HS 2243E from the National Institutes of Health. This assay was run only for some of the samples of the normal controls (n = 9).
Plasma IGF-I, IGFBP-3, and ALS concentrations were measured at DSL by using the DSL commercially available ELISA.
Statistical analysis.
Parametric t tests were used to analyze differences between the two study groups for all the growth factors measured. Multiple stepwise regression analysis was used to estimate the relative associations between GH assays and other circulating growth factors and anthropometric measures. Significance was established at p < 0.05.
RESULTS
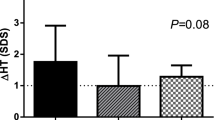
Table 2 summarizes the concentrations of growth factors and GH by three different assays in the present cohort and compares those with normal controls. The serum GH concentrations in the SS group were comparable whether the immunofunctional or DSL ELISA assay was used, yet the Hybritech assay was consistently higher in this cohort. There was a high correlation between the peak GH concentrations regardless of the assay used within groups (Fig. 1). There were no statistically significant differences between GH concentrations (peak or mean) between the SS versus normal controls group regardless of the GH assay used. The slope of the IFGH versus DSL ELISA GH curve was, however, substantially higher (0.98) than that of the DSL ELISA GH versus Hybritech IRMA GH (0.68) or the IFGH and Hybritech GH (0.65), indicating that the Hybritech IRMA is not measuring the exact same molecules as the DSL ELISA and IFGH. Interestingly, there was a wide array of GH concentration in all assays in the normal controls with 11 out of 13 subjects having peaks <7 ng/mL in the IFGH assay, six out of 13 using the DSL ELISA, and four out of nine using the conventional Hybritech IRMA. Actually, of the normally statured children, 46% or six out of 13 subjects had levels <5 ng/mL using the conventional DSL ELISA and three out of nine (33%) using the Hybritech IRMA (Fig. 2). These ranges were observed in both prepubertal and pubertal youngsters. The lower GH peaks were also observed comparably in those who were stimulated by insulin-induced hypoglycemia versus arginine/L-dopa.
Plasma IGF-I, IGFBP-3, and ALS concentrations, however, were consistently lower in the SS group compared with controls whether the data are expressed as actual concentrations or SDS. These differences persisted even when all data of the four children younger than 6 y of age were eliminated in the analysis.
Multiple regression analysis was performed in the SS group to assess the relations between peak GH responses to stimuli (using both the IFGH and ELISA DSL assays), and the data are shown in Table 3. There were no significant correlations between peak IFGH or ELISA GH concentrations and plasma IGF-I, IGFBP-3, or ALS concentrations nor between IFGH or ELISA GH concentrations and height SDS, BMI, chronologic age, or linear growth velocity.
DISCUSSION
These studies show a very tight correlation between the IFGH assay and conventional commercially available assays for GH in SS and normal children. Both the ELISA by DSL and the Hybritech IRMA correlated well with the IFGH assay and with one another, even though the Hybritech assay gave consistently higher values for GH concentrations than the IFGH and ELISA methods in the short children studied. These data suggest that the IFGH assay may not offer any substantial advantage over the ELISA method in the majority of patients studied, which speaks well for the accuracy of the commercial assays tested (the standard DSL ELISA or Hybritech IRMA) to detect biologically active molecules.
SS caused by biologically inactive forms of GH has been previously reported, and it is characterized by high circulating GH concentrations, lack of GH action, and marked catch-up growth to exogenous GH administration (18). Mutations in the GH-1 gene have been found associated with this condition, and the mutant GH not only failed to stimulate tyrosine phosphorylation but could also exert an antagonistic effect (18, 19). Determining whether there are patients with idiopathic SS who have an abnormal ratio of immunofunctional to immunoassay concentrations, suggestive of biologically inactive forms of GH, would require both assays to be run in a large cohort of otherwise normal children with idiopathic SS.
In a substantial number of the normally statured children studied here, using either arginine and L-dopa or arginine and insulin-induced hypoglycemia as the pharmacologic stimuli for GH secretion, the peak GH responses to stimuli were below the critical cutoffs conventionally accepted. Approximately 50% of the cohort of normal children had peaks <7 ng/mL using either the DSL ELISA or Hybritech IRMA, and 33 to 46% (Hybritech IRMA or DSL ELISA) had levels below 5 ng/mL. Actually, two fully pubertal normal subjects had peak GH concentrations in the 2 ng/mL range using the IFGH and DSL ELISA GH assay. Taken in aggregate, these and other data support the concept that GH stimulation tests in children cannot accurately determine deficiency unless the levels are very low (<2 ng/mL), making the arbitrary cutoffs of <10, 7, or even 5 ng/mL useless in the assessment of the short child when contemporary sensitive assays and common secretagogues are used. It is possible, however, that better separation between deficiency and sufficiency states would be found if the more potent stimuli [like GH releasing hormone and pyridostigmine (9)] were used.
The measurement of circulating growth factors, on the other hand, showed interesting trends. IGF-I, IGFBP-3, and ALS concentrations were all in aggregate lower in the SS group than in the normal controls even when the youngest children in the SS group were excluded from analysis. Because all these peptides are GH dependent, the fact that normal children had substantially higher concentrations than the SS group suggests that the measurement of these growth factors may be a more discriminating measure of GH sufficiency in children than GH stimulation tests, a principle supported by others (20).
There were no correlations between the peak GH response to stimuli measured with any of the three assays used and commonly used anthropometric measures such as height, BMI, chronologic age, growth velocity, IGF-I, IGFBP-3, or ALS concentrations, making predictions of the potential linear growth with GH therapy difficult at best.
It is estimated that approximately 42% of all children treated with GH in the U.S. do not have classic GH deficiency (21); however, the efficacy of GH in increasing linear growth and ultimate height in those youngsters, many of whom have idiopathic SS, is indeed modest (22). Hence, the financial savings of establishing the proper diagnosis of GH deficiency in childhood are substantial. SS children who are otherwise normal and are growing along the 5% with normal IGF-I, IGFBP-3, and ALS concentrations may not need to undergo GH stimulation testing and subsequent brain magnetic resonance imaging in the absence of CNS symptoms. GH stimulation tests should be reserved for those with low circulating growth factors and poor growth (23).
In summary, a novel IFGH assay used during GH stimulation tests of short children showed strong correlation with standard GH DSL ELISA and Hybritech IRMA, suggesting that these contemporary GH immunoassays detect mostly GH capable of generating a biologic signal. We also showed that normally statured children can fail to increase their GH concentrations above 2 ng/mL yet have normal levels of circulating GH-dependent growth factors. These data also indicate that the criteria of peak GH responses to common stimuli considered abnormal if <10, 7, or even 5 ng/mL need to be revisited. We conclude that normal GH stimulation test results can be substantially lower than previously accepted. GH-dependent growth factors may be more sensitive indicators of GH sufficiency than stimulated GH concentrations.
Abbreviations
- IFGH:
-
immunofunctional GH
- SS:
-
short stature
- IRMA:
-
immunoradiometric assay
- IGFBP-3:
-
IGF binding protein-3
- ALS:
-
acid labile subunit
- DSL:
-
Diagnostic Systems Laboratories
References
Wyatt DT, Mark D, Slyper A 1995 Survey of growth hormone treatment practices by 251 pediatric endocrinologists. J Clin Endocrinol Metab 80: 3292–3297.
Celniker AC, Chen AB, Wert RM Jr Sherman BM 1989 Variability in the quantitation of circulating growth hormone using commercial immunoassays. J Clin Endocrinol Metab 68: 469–476.
Root AW, Rosenfield RL, Bongiovanni AM, Eberlein WR 1967 The plasma growth hormone response to insulin-induced hypoglycemia in children with retardation of growth. Pediatrics 39: 844–852.
Root AW, Saenz-Rodriguez C, Bongiovanni AM, Eberlein WR 1969 The effect of arginine infusion on plasma growth hormone and insulin in children. J Pediatr 74: 187–197.
Youlton R, Kaplan SL, Grumbach MM 1969 Growth and growth hormone. IV. Limitations of the growth hormone response to insulin and arginine and of the immunoreactive insulin response to arginine in the assessment of growth hormone deficiency in children. Pediatrics 43: 989–1004.
Collu R, Leboeuf G, Letarte J, Ducharme JR 1975 Stimulation of growth hormone secretion by levodopa-propranolol in children and adolescents. Pediatrics 56: 262–266.
Weldon VV, Gupta SK, Klingensmith G, Clarke WL, Duck SC, Haymond MW, Pagliara AS 1975 Evaluation of growth hormone release in children using arginine and L- dopa in combination. J Pediatr 87: 540–544.
Lanes R, Hurtado E 1982 Oral clonidine—an effective growth hormone-releasing agent in prepubertal subjects. J Pediatr 100: 710–714.
Ghigo E, Bellone J, Aimaretti G, Bellone S, Loche S, Cappa M, Bartolotta E, Dammacco F, Camanni F 1996 Reliability of provocative tests to assess growth hormone secretory status. Study in 472 normally growing children. J Clin Endocrinol Metab 81: 3323–3327.
Fass B, Lippe BM, Kaplan SA 1979 Relative usefulness of three growth hormone stimulation screening tests. Am J Dis Child 133: 931–933.
Frasier SD 1974 A preview of growth hormone stimulation tests in children. Pediatrics 53: 929–937.
Tillmann V, Buckler JM, Kibirige MS, Price DA, Shalet SM, Wales JK, Addison MG, Gill MS, Whatmore AJ, Clayton PE 1997 Biochemical tests in the diagnosis of childhood growth hormone deficiency. J Clin Endocrinol Metab 82: 531–535.
Giustina A, Veldhuis JD 1998 Pathophysiology of the neuroregulation of growth hormone secretion in experimental animals and the human. Endocr Rev 19: 717–797.
Rose SR, Ross JL, Uriarte M, Barnes KM, Cassorla FG, Cutler GB Jr 1988 The advantage of measuring stimulated as compared with spontaneous growth hormone levels in the diagnosis of growth hormone deficiency. N Engl J Med 319: 201–207.
Hoffman DM, O'Sullivan AJ, Baxter RC, Ho KK 1994 Diagnosis of growth-hormone deficiency in adults. Lancet 343: 1064
Carroll PV, Christ ER, Bengtsson BA, Carlsson L, Christiansen JS, Clemmons D, Hintz R, Ho K, Laron Z, Sizonenko P, Sonksen PH, Tanaka T, Thorn M 1998 Growth hormone deficiency in adulthood and the effects of growth hormone replacement: a review. Growth Hormone Research Society Scientific Committee. J Clin Endocrinol Metab 83: 382–395.
Strasburger CJ, Wu Z, Pflaum CD, Dressendorfer RA 1996 Immunofunctional assay of human growth hormone (hGH) in serum: a possible consensus for quantitative hGH measurement. J Clin Endocrinol Metab 81: 2613–2620.
Takahashi Y, Shirono H, Arisaka O, Takahashi K, Yagi T, Koga J, Kaji H, Okimur Y, Abe H, Tanaka T, Chihara K 1997 Biologically inactive growth hormone caused by an amino acid substitution. J Clin Invest 100: 1159–1165.
Takahashi Y, Chihara K 1998 Clinical significance and molecular mechanisms of bioinactive growth hormone. Int J Mol Med 2: 287–291.
Rosenfeld RG, Albertsson-Wikland K, Cassorla F, Frasier SD, Hasegawa Y, Hintz RL, Lafranchi S, Lippe B, Loriaux L, Melmed S 1995 Diagnostic controversy: the diagnosis of childhood growth hormone deficiency revisited. J Clin Endocrinol Metab 80: 1532–1540.
Cuttler L, Silver JB, Singh J, Marrero U, Finkelstein B, Tannin G 1996 Short stature and growth hormone therapy: a national study of physician recommendation patterns. JAMA 276: 531–537.
Hintz RL, Attie KM, Baptista J, Roche A 1999 Effect of growth hormone treatment on adult height of children with idiopathic short stature. Genentech Collaborative Group. N Engl J Med 340: 502–507.
Vance ML, Mauras N 1999 Growth hormone therapy in adults and children. N Eng J Med 341: 1216
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Mauras, N., Walton, P., Nicar, M. et al. Growth Hormone Stimulation Testing in Both Short and Normal Statured Children: Use of an Immunofunctional Assay. Pediatr Res 48, 614–618 (2000). https://doi.org/10.1203/00006450-200011000-00010
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/00006450-200011000-00010
This article is cited by
-
Pegvisomant-primed growth hormone (GH) stimulation test is useful in identifying true GH deficient children
Hormones (2017)
-
The role of insulin like growth factor (IGF) — 1 and IGF — binding protein-3 in diagnosis of Growth Hormone Deficiency in short stature children
The Indian Journal of Pediatrics (2009)
-
Growth hormone deficiency in children
Pituitary (2008)
-
Assessment of serum IGF-I concentrations in the diagnosis of isolated childhood-onset GH deficiency: A proposal of the Italian Society for Pediatric Endocrinology and Diabetes (SIEDP/ISPED)
Journal of Endocrinological Investigation (2006)