Abstract
The main objective of the present study was to determine whether a structured, laboratory-based exercise task would modify the energy expenditure (EE) and the pattern of spontaneous physical activity (PA) of obese boys on the day of an exercise laboratory visit and on the following day. Fourteen 10- to 15-y-old moderately obese (36.6 ± 3.3% fat) boys volunteered. They each had three laboratory visits, 1 wk apart. In one visit, they performed a strenuous 50-min cycling task; in another, a 30-min medium-intensity cycling task; and in another (which served as placebo), they did not exercise. PA was monitored the day before (d 1), during (d 2), and after (d 3) each laboratory visit by use of a heart rate monitor and a 12-h recall interview. EE was calculated from minute-by-minute heart rate and each child's predetermined relationship between oxygen uptake and heart rate. EE and PA were analyzed from 1300 to 1900 h each day using 15-min intervals. EE tended to decrease (p < 0.087) in the afternoon of all d 2 compared with d 1, and it increased on d 3 after the medium-intensity exercise (p < 0.0005). EE during d 2 and 3 combined, compared with d 1, decreased after the high-intensity exercise (534.2 versus 564.3 kJ/h, p < 0.05). It increased after the medium-intensity exercise (561.8 versus 526.7 kJ/h, p = 0.052) and was not affected after the placebo visit (589.4 versus 574.3 kJ/h). Time spent outdoors was consistently reduced on the day of laboratory visit compared with the day before and after the visit, regardless of the contents of intervention In conclusion, a single laboratory visit is followed by a reduction in EE and PA on the day of intervention. However, its effect on EE the following day may be dose dependent: medium-intensity exercise induces an increase in EE, but high-intensity exercise causes a decrease in EE. One implication is that intervention by physical training should employ medium-intensity exercise to enhance the EE of obese boys.
Similar content being viewed by others
Main
Numerous studies(1–11), but not all(12–18), suggest that obese children and adolescents are habitually less active than their nonobese peers, particularly during nonstructured activities. There are various possible explanations for the sedentary behavior of obese children, such as a low physical fitness; high rating of perceived physical effort, possibly due to a greater mechanical work per ask(19); low self-esteem with the feeling of being awkward and physically limited; discrimination by peers(20,21); or the presence of other obese and sedentary family members(3).
Regardless of the possible causes of sedentariness in obese people, enhanced PA has become part and parcel of most comprehensive intervention programs. Regimented exercise delivered several times per week for 4 wk can increase daily EE in obese adolescents by 12%(22). Similarly, a loss of 1.4% body fat in obese girls has been reported after a 10-wk exercise program(23). However, training-induced changes in EE, body mass, or percent fat often do not tally with the caloric value of the prescribed exercise(22,24). Blaak et al.(22) could explain only 50% of the increase in EE by the exercise intervention per se. It was hypothesized in that study that the exercise sessions "invigorated" the obese adolescents, who chose to increase activities during the nontraining hours. However, using HR monitoring, the authors showed only a mild increased in habitual PA outside the laboratory. An opposite scenario was seen in obese women: when given a 12-wk training program, they showed an increase in spontaneous daily activities during the non-training hours of the day(25).
The main objective of the present study, therefore, was to find out whether EE and habitual activity patterns as assessed by HR monitoring and interviews are modified on a day when obese boys are engaged in supervised, structured exercise and on the following day. Such information may yield further insight into the possible physiologic and behavioral causes for the overall increase in total EE as reported by Blaak et al.(22). For the purpose of the present study, the doubly labeled water technique is not suitable because it provides information only about total EE for 7-14 d but cannot monitor changes in EE during discrete days.
METHODS
Subjects. Fourteen boys participated in the study. Inclusion criteria were age 10 to 15 y and body fat of 30% or more. Exclusion criteria were existence of any disease other than obesity and participation in a weight-reduction program or in organized sports during the period of the study. Physical characteristics of the subjects are described in Table 1.
Design and structure of the study. The project was conducted using a repeated measurement design in which each boy served as his own control. There were three laboratory sessions, 1 wk apart, and 9 d of monitoring of PA and EE. Each week included three consecutive monitoring days (termed d 1, 2, and 3). Day 1 was used for monitoring EE and spontaneous PA pattern. Day 2 included a laboratory visit in the morning, followed by monitoring EE and spontaneous PA. Day 3 was used for monitoring EE and PA.
Informed consent was obtained from a parent after verbal assent by the child. The study was approved by the Research Ethics Board of the McMaster University Faculty of Health Sciences.
The three laboratory visits differed in their respective protocols, designated as protocol A, B, and C. To avoid ordering effect, the protocols were assigned using the Latin square principle. Protocol A included a high-dose exercise routine, protocol B had a medium-dose exercise routine, and protocol C was used as a placebo with no exercise. The summer break period was chosen to prevent the structured routine of the school year.
Laboratory protocols. Laboratory visits took place in the morning of d 2 each week on the same weekdays and lasted 1 to 2 h. The boys were blinded to the content of the expected visit. When the child arrived at the laboratory, we first removed the HR monitor for retrieval of the collected data. Height (Harpenden stadiometer), weight (Mott scale), and percent body fat (bioimpedance analysis, RJL model BIA-101A) were measured at each visit. The HR monitor was mounted and started within 10-15 min after the end of exercise.
Exercise was performed on a cycle ergometer (Fleisch Metabo, Lausanne, Switzerland). In protocol A, the child exercised 4 times for 10 min with short breaks of 5 min in between at an intensity equivalent to a HR of 150 to 160 bpm. After the last bout, a break of at least 10 min was given to ascertain a decrease of HR to resting values. This was followed by an all-out multistage (2 min per stage) task on the same stationary cycle to establish each child's maximal O2 uptake (V˙O2; see Table 1) as well as the submaximal V˙O2-HR relationship during exercise. In protocol B, the boys performed two cycling bouts of 15 min at a HR of 130 to 140 bpm with a 5-min break in between. The exercise intensity and total work performed in the different protocols are summarized in Table 2. Protocol C was structured as a placebo session and was used to determine metabolic rate at rest in various body positions.
Calculating EE from HR monitoring. A HR monitor (Sport Tester VL4000, Polar Electro, Kempele, Finland) was installed at the child's home on the first morning of each 3-d period. HR was sampled and stored every minute of the day and the night until the start of the laboratory visit on d 2. Then the monitor was removed, stored information was retrieved, and the receiver was reprogrammed for further storage of data from d 2 and 3. The monitor was finally removed during a home visit in the evening of d 3. Thus, the total time planned for monitoring HR was 3 d and 2 nights. However, because of missing data (due to malfunction of the system) and artifacts (treated as missing data), the total yield of monitoring was <100%. An artifact was defined as a HR <40 bpm, >220 bpm, or a sudden change of >60 bpm that lasted only 1 min.
To estimate EE from the minute-by-minute HR recordings, we employed the HR flex method described by Livingstone et al.(26). Each child went through a V˙O2-on-HR calibration protocol. For that purpose, V˙O2 and HR were determined for each of several metabolic levels at rest and during exercise.
Resting EE was measured by indirect calorimetry in a thermoneutral room (temperature 22-23°C). Resting V˙O2 and HR were obtained in a supine, sitting, and standing position. An average of the three was taken to represent resting EE. Each position lasted at least 15 min, sufficient to reach a steady state. For the supine measurement, we used a ventilated hood. A mouthpiece, nose clip, and nonrebreathing valve system were used for gas collection during sitting and standing. Expired gases were analyzed and recorded every 30 s by a Beckman metabolic cart (Beckman MMC Horizon, Anaheim, CA). HR was recorded simultaneously by ECG (1500B electrocardiograph, Hewlett Packard). The most stable 2 min of each stage, regarding V˙O2 and HR, were taken for the V˙O2-HR relationship.
HR flex, used as a dividing point between HR at rest and HR during exercise, was defined(26) as the mean of the HR for the resting activities (supine, sitting, and standing) and the lowest HR during pedaling (40 rpm) at zero resistance.
To determine the individual V˙O2-HR regression line above the HR flex point, we used the simultaneously registered HR and V˙O2 data for four to five exercise intensities, as obtained during the multistage phase of protocol A. The last 30 s of each 2-min submaximal stage were taken to represent the respective data points.
Daytime periods when HR was below HR flex were considered to reflect resting metabolism. When HR exceeded HR flex, V˙O2 was derived from the subject's V˙O2-HR regression line. EE was then calculated for each minute of HR recording, assuming 20.4 kJ per each liter of O2 consumed.
Activity interviews. During the laboratory visit in the morning of d 2 and in the morning and evening of d 3 at the child's home, the child was interviewed regarding activities performed on d 1, 2, and 3, respectively. Activities were grouped into two categories: indoors (including napping and watching TV) and outdoors. The amount of OUT was taken as an index of active pursuit in the subsequent analysis.
Data reduction and statistical analysis. To allow for comparisons among days when the child came in the morning to the laboratory and those without a laboratory visit, we focused in the ensuing analysis on the time interval from 1300 to 1900 h. Individual EE and OUT data were averaged over 15-min periods. We discarded those periods for which <5 min of acceptable HR or OUT data were obtained. Out of 3024 possible 15-min averages of EE (three protocols, 3 d, 24 time periods per afternoon, 14 subjects), we had a yield of 2713 (89.7%). The respective yield for OUT was 2937 (97.1%).
Data analysis was performed separately for EE and OUT using BMDP (Statistical Solutions, Cork, Ireland) program 5V (ANOVA for unbalanced repeated measures). The ANOVA were performed using all three protocols, 3 d, and 24 time intervals as repeated measures. If the factors day, protocol, or day x protocol were significant in the ANOVA, the following planned ANOVA were calculated: ANOVA 1, using only data of d 1; ANOVA 2, using data of all 3 d but only of two protocols to compare each two protocols; ANOVA 3, for each protocol separately, EE and OUT on d 2 and 3 were compared one by one to EE and OUT on d 1. To assess the overall effects of the exercise or placebo intervention compared with preintervention conditions for each protocol, related individual 15-min values of EE and OUT obtained on d 2 and 3 were averaged and compared with the respective values on d 1 using ANOVA.
Statistical significance was accepted at p < 0.05. Values are expressed as mean ± SEM unless stated otherwise.
RESULTS
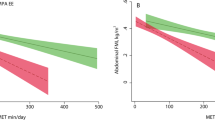
Table 3 summarizes mean EE and OUT separately for d 1 to 3 and protocols A, B, and C. EE is presented in kilojoules per hour, and OUT is presented as percentage of the total observation time.
EE. On the basis of the 3-way ANOVA (protocol, day, time of day), a significant difference in EE was observed among protocols (protocol effect, p < 0.001) and a significant protocol × day interaction was seen (p < 0.01).
ANOVA 1 revealed that baseline (d 1) EE was not different among the 3 wk. Average EE between 1300 and 1900 h on d 1 was 554.3 kJ/h, which is 2.1 ± 0.5 times the group's resting metabolic rate.
ANOVA 2 (including all days but only two protocols) showed significant effects of protocol when comparing A versus C and B versus C (both p < 0.001). A significant protocol × day interaction was observed between protocols A and B (p < 0.001) and between protocols A and C (p < 0.05).
On d 2, EE tended (p = 0.087) to be lower than in d 1 in the three protocols (ANOVA 3). On d 3, EE was reduced compared with d 1 in protocol A (p < 0.05) but increased in protocols B (p < 0.001) and, to a lesser degree, C (p < 0.05).
When EE on d 2 and 3 was averaged, it was significantly lower than on d 1 in the high-intensity protocol A (p < 0.05). In contrast, there was a tendency (p = 0.052) toward an increase in EE after the medium-intensity exercise intervention of protocol B and there was no difference between d 2 and 3 compared with d 1 for protocol C.
The resting metabolic rate measured in the present study and the calculated basal metabolic rate based on the 1985 recommendations of the World Health Organization(27) are summarized in Table 1. It is of interest that, in these obese boys, calculating basal metabolic rate according to the child's total body mass yields a major overestimate. In contrast, a calculation based on fat-free mass was very close to our direct measurements of resting metabolic rate.
OUT. The 3-way ANOVA revealed significant differences in OUT among protocols and among days but no interaction between protocols and days. OUT during d 1 did not differ among the 3 wk (ANOVA 1).
Comparing two protocols over all 3 d (ANOVA 2), OUT was significantly lower in protocols A and B than in protocol C (both comparisons, p < 0.05) but the pattern of PA changes from day to day remained constant among protocols (no significant protocol × day interaction).
OUT was significantly reduced on d 2 compared with d 1 in protocols A and B. This difference was nearly significant (p = 0.059) in protocol C. Whereas no difference was observed between d 1 and 3 in protocol A, there was a significant increase in OUT on d 3 compared with d 1 for protocol B (p < 0.01) and a trend toward an increase in OUT for protocol C (p = 0.064). There was no change in OUT from d 1 to the average of d 2 and 3 in any of the protocols.
DISCUSSION
The general pattern that emerges from these results is a decrease in habitual PA and, to a lesser extent, in EE during the day of the laboratory visit and an increase on the following day. This pattern occurred regardless of whether we used HR monitoring or an interview. The HR data also suggest that the exercise sessions had a more pronounced effect on EE than did the placebo nonexercise laboratory visit. However, whereas high-intensity exercise was followed by a decrease in EE on the day of the visit and the subsequent day, medium-intensity exercise induced an increase of EE on the subsequent day.
Inconclusive data have been reported previously regarding the effect of training or of an acute exercise bout on the spontaneous PA and EE of obese people. Blaak et al.(22) described little or no increase in PA and a 12% increase in 24-h EE in ten 10- to 12-y-old obese boys who took part in a laboratory-based, 4-wk training program. This increase was well above and beyond that expected from the program itself. Epstein et al.(28) reported a decrease in spontaneous PA in obese children over a 6-mo intervention (combined diet and life-style exercise). Van Dale et al.(25) found that obese women increased their PA during a medium-intensity 12-wk training program. This pattern is in line with the OUT data in the present study. Our study, however, is the first to assess spontaneous activity of obese children, both on the day of a regimented activity and on the following day. It suggests that the direction of change in activity and EE differs between the 2 d.
Unlike our original assumption, exercise in the laboratory decreased outdoor activity on the same day. There is no clear mechanism to explain this response. Possibly, the boys were tired and reluctant to spend their reduced spare time that day in physical pursuits, especially because they had exercised that morning. The lack of change in EE and activity after the placebo visit is in line with this explanation. On the basis of clinical experience with obese children, we expected that the perception of exercise as fun and the fact that the child could successfully perform a demanding exercise task in the laboratory would serve as reinforcers for subsequent activities. Although this mechanism was not apparent on the day of the laboratory visit, it may have affected behavior on the day after the medium-intensity session. The mild increases that occurred on the day after the placebo session may reflect a "halo" effect of a visit to an exercise laboratory.
The effects of structured exercise on spontaneous activity behavior of obese people are important not only from a theoretical point of view but also have clinical implications, because changes in spontaneous activity may affect the overall 24-h EE, with implications for energy balance and the success of weight-control programs. Studies that used exercise intervention for weight control of obese children have varied in their efficacy. Whereas some(19,22,29,30) report no effect on body mass or adiposity, others(23,25,31) suggest a beneficial effect. All but one(23) of these studies focused on the exercise dosage of the program itself while ignoring the children's activity and EE outside the exercise sessions. We propose that such an omission may have contributed to our lack of understanding of why some intervention programs are effective whereas others are not.
The present study was not designed to identify an optimal training intensity that would induce an increase in spontaneous PA and EE. However, the increase on the day after a medium-intensity exercise (protocol B) compared with a decrease after an intense exercise (protocol A) suggests a dose-response relationship. Interestingly, the medium intensity in this study (30 min at 70% of maximal V˙O2) is almost identical to the one used by Blaak et al.(22) who reported an increase in 24-h EE beyond the training dose itself. Until further information is available, we suggest that training programs for obese children be of a light-to-moderate intensity (e.g. at HR that do not exceed 140-150 bpm).
The gold standard method for the measurement of EE in free-living humans is the doubly labeled water clearance analysis(32). This method, however, yields information about the total EE over 7-14 days. As such, it would be unsuitable for the present study in which we needed to compare EE at much shorter time segments. Several physiologic and mechanical variables have been tried as surrogate estimates of EE. Among these, HR monitoring is the simplest and most commonly used approach for assessing EE during free-living conditions. Even though HR is also affected by factors other than metabolic level, it has been validated against the doubly labeled methods in adults(33,34) and in children(35). Although there are no studies that have validated the use of HR monitoring in obese children, this method has been used successfully with such subjects(22). There is no reason to assume a priori differences in the utility of the HR-monitoring method in nonobese and moderately obese children, as long as precautions are being made to ascertain a stable contact of the transmitter electrodes with the skin. In this regard, the yield of some 90% of usable HR data in the present study is encouraging. One may wonder whether the 10% missing values may have skewed our findings. This, in our opinion, is unlikely. First, the BMDP statistical program is able to handle missing data unless the loss of values is nonrandom. We have no reason to suspect any pattern in the lost data, which were equally lost at any time of the day. Second, we reanalyzed the data using only six subjects who had complete HR sets plus two subjects in whom only few missing data were interpolated. Using this approach, the pattern of responses was similar to that described above. The results for these eight subjects, thus, are compatible with those derived for all 14 subjects.
In conclusion, when moderately obese 10- to 15-y-old boys perform regimented exercise in the laboratory, their spontaneous PA and EE on the same day and the subsequent day may change. On the day of all visits, activity decreased significantly and EE tended to decrease. The change on the subsequent day depended on the intensity of the regimented exercise: activity was enhanced when exercise was of medium intensity and it was suppressed when exercise was intense. More insight into these phenomena may have implications for the use of training as a tool in weight management.
Abbreviations
- bpm:
-
heart beats per minute
- EE:
-
energy expenditure
- HR:
-
heart rate
- OUT:
-
time spent outdoors
- PA:
-
physical activity
- V˙:
-
oxygen uptake
References
Bloom WL, Eidex MF 1967 Inactivity as a major factor in adult obesity. Metabolism 8: 679–684
Bronstein IP 1953 Obesity in childhood: childhood studies. Am J Dis Child 63: 130–136
Bruch H 1940 Obesity in childhood. Am J Dis Child 60: 1082–1109
Cohen CJ 1992 Physical activity and dietary patterns of lean versus obese middle-school children. Ped Exerc Sci 4: 187–188
Corbin CB, Pletcher P 1968 Diet and physical activity patterns of obese and nonobese elementary school children. Res Q Exerc Sports 39: 922–928
Johnson ML, Burke BS, Mayer J 1956 Relative importance of inactivity and overeating in the energy balance of obese high school girls. Am J Clin Nutr 4: 37–44
Montoye HJ 1985 Risk indicators for cardiovascular disease in relation to physical activity in youth. In: Binkhorst RA, Kemper HCG, Saris WA (eds) Children and Exercise XI. Human Kinetics, Champaign, IL, pp 3–25
Pate R, Ross JG 1987 The national children and youth fitness study II: factors associated with health-related fitness. J Phys Ed Rec Dance 58: 93–95
Stefanik PA, Heald FP, Mayer J 1959 Caloric intake in relation to energy output of obese and non-obese adolescent boys. Am J Clin Nutr 7: 55–62
Thomson ME, Cruickshank FM 1979 Survey into the eating and exercise habits of New Zealand pre-adolescents in relation to overweight and obesity. N Z Med J 89: 7–9
Waxman M, Stunkard AJ 1980 Caloric intake and expenditure of obese boys. J Pediatr 96: 187–193
Klesges RC, Eck LH, Hanson CL, Haddock CK, Klesges LM 1990 Effects of obesity, social interactions, and physical environment on physical activity in preschoolers. Health Psychol 9: 435–449
Klesges RC, Haddock CK, Eck LH 1990 A multimethod approach to the measurement of childhood physical activity and its relationship to blood pressure and body weight. J Pediatr 116: 888–893
Marti B, Vartianen E 1989 Relations between leisure time exercise and cardiovascular risk factors among 15-year-olds in Finland. J Epidemiol Community Health 43: 228–233
Stunkard A, Pestka Y 1962 The physical activity of obese girls. Am J Dis Child 103: 116–121
Vara L, Argas S 1989 Caloric intake and activity levels are related in young children. Int J Obesity 13: 613–617
Watson AWS, O'Donovan DJ 1977 The relationship of level of habitual activity to measures of leanness-fatness, physical working capacity, strength, and motor ability in 17- and 18-year-old males. Eur J Appl Physiol 37: 93–100
Wilkinson PW, Parkin JM, Pearlson G, Strong H, Sykes P 1977 Energy intake and physical activity in obese boys. BMJ 1: 750–756
Ward DS, Blimkie CJR, Bar-Or O 1986 Rating of perceived exertion in obese adolescents. Med Sci Sports Exerc 18:S72
Allon N 1979 Self-perception of the stigma of overweight in relationship to weight-losing pattern. Am J Clin Nutr 32: 470–480
Monello LF, Mayer J 1963 Obese adolescent girls: an unrecognized "minority" group?. Am J Clin Nutr 13: 35–39
Blaak EE, Westerterp KR, Bar-Or O, Wouters LJM, Saris WHM 1992 Total energy expenditure and spontaneous activity in relation to training in obese boys. Am J Clin Nutr 55: 777–782
Gutin B, Cucuzzo N, Islam S, Smith C, Moffatt R, Pargman D 1995 Physical training improves body composition in black obese 7- to 11-year-old girls. Obes Res 3: 305–312
Moody DL, Wilmore JH, Girandola RN, Royce JP 1972 The effect of jogging program on the body composition of normal and obese high school girls. Med Sci Sports Exerc 4: 210–213
Van Dale D, Schoffelen PFM, Ten Hoor F, Saris WHM 1989 Effects of addition of exercise to energy restriction on 24-hour energy expenditure, sleeping metabolic rate, and daily physical activity. Eur J Clin Nutr 43: 441–451
Livingstone MB, Coward WA, Prentice AM, Davies PS, Strain JJ 1992 Daily energy expenditure in free-living children: comparison of heart-rate monitoring with the doubly labeled water (2H2(18)O) method. Am J Clin Nutr 56: 343–352
Schofield WN, Schofield C, James WPT 1985 Basal metabolic rate-review and prediction, together with an annotated bibliography of source material. Hum Nutr Clin Nutr 39C( suppl): 5–96
Epstein LH, Wing RR, Penner BC, Kress MJ 1985 Effect of diet and controlled exercise on weight loss in obese children. Pediatrics 107: 358–361
Jette M, Barry W, Pearlman L 1977 The effects of an extracurricular physical activity program on obese adolescents. Can J Public Health 68: 39–42
Parizkova J, Vaneckova M, Vamberova M 1962 A study of changes in some functional indicators following reduction of excessive fat in obese children. Physiol Bohemoslov 11: 351–357
Sasaki J, Shindo M, Tanaka H, Ando M, Arakawa K 1987 A long-term aerobic exercise program decreases the obesity index and increases the high density lipoprotein cholesterol concentrations. Int J Obesity 11: 339–345
Schoeller DA, Ravussin E, Schutz Y, Acheson KJ, Baetsch P, Jaquier E 1986 Energy expenditure by doubly labeled water validation in humans and proposed calculation. Am J Physiol 250:R823–R830
Livingstone MBE, Prentice AM, Coward AW, Cessay SM, Strain JJ, McKenna PG, Nevin GB, Barker ME, Hickey RJ 1990 Simultaneous measurement of free-living energy expenditure by the doubly labeled water method and heart-rate monitoring. Am J Clin Nutr 52: 59–65
Schulz S, Westerterp KR, Brueck K 1989 Comparison of energy expenditure by the doubly labeled water technique with energy intake, heart rate, and activity recording in man. Am J Clin Nutr 49: 1146–1154
Emons HJ, Groenenboom DC, Westerterp KR, Saris WH 1992 Comparison of heart rate monitoring combined with indirect colorimetry and the doubly labelled water (2H218O) method for the measurement of energy expenditure in children. Eur J Appl Physiol 65: 99–103
Acknowledgements
The authors thank Eric Duku, Mike Riddell, and Randy Calvert for their valuable comments and suggestions.
Author information
Authors and Affiliations
Additional information
Supported by a grant from the Canadian Fitness and Lifestyle Research Institute.urrent address [S.K.]: Klinik für Kinder & Jugendliche, Stadtspital Triemli, Zürich, Switzerland.urrent address [H.H.]: Univ.-Kinderklinik, 97080 Würzburg, Germany.
Rights and permissions
About this article
Cite this article
Kriemler, S., Hebestreit, H., Mikami, S. et al. Impact of a Single Exercise Bout on Energy Expenditure and Spontaneous Physical Activity of Obese Boys. Pediatr Res 46, 40–44 (1999). https://doi.org/10.1203/00006450-199907000-00007
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/00006450-199907000-00007
This article is cited by
-
Effects of High-Intensity Interval Training in School on the Physical Performance and Health of Children and Adolescents: A Systematic Review with Meta-Analysis
Sports Medicine - Open (2022)
-
Ambulatory blood pressure response to a bout of HIIT in metabolic syndrome patients
European Journal of Applied Physiology (2017)
-
Impact of imposed exercise on energy intake in children at risk for overweight
Nutrition Journal (2016)
-
The ActivityStat Hypothesis
Sports Medicine (2013)
-
Potential causes, mechanisms, and implications of post exercise hypotension
Journal of Human Hypertension (2002)