Abstract
The present study was designed to examine the effects of inhibition of nitric oxide synthase on cerebral energy metabolism after hypoxia-ischemia in newborn piglets. Ten 1- to 3-d-old piglets received Nω-nitro-L-arginine (NNLA), an inhibitor of nitric oxide synthase (NNLA-hypoxia, n = 5), or normal saline (hypoxia, n = 5) 1 h before cerebral hypoxia-ischemia. After the infusion, hypoxia-ischemia was induced by bilateral occlusion of the carotid arteries and decreasing FiO2 to 0.07 and maintained for 60 min. Thereafter, animals were resuscitated and ventilated for another 3 h. Using 1H- and 31P-magnetic resonance spectroscopy, cerebral energy metabolism was measured in vivo at 15-min intervals throughout the experiment. Phosphocreatine to inorganic phosphate ratios decreased from 2.74 ± 0.14 to 0.74 ± 0.36 (hypoxia group) and 2.32 ± 0.17 to 0.18 ± 0.10 (NNLA-hypoxia group) during hypoxia-ischemia. Thereafter, phosphocreatine to inorganic phosphate ratios returned rapidly to baseline values in the hypoxia group, but remained below baseline values in the NNLA-hypoxia group. Intracellular pH decreased during hypoxia-ischemia and returned to baseline values on reperfusion in both groups. Intracellular pH values were lower in the NNLA-hypoxia group (p < 0.001, ANOVA). Lactate was not present during the baseline period. After hypoxia-ischemia, lactate to N-acetylaspartate ratios increased to 1.34 ± 0.28 (hypoxia group) and 2.22 ± 0.46 (NNLA-hypoxia group). Lactate had disappeared after 3 h of reperfusion in the hypoxia group, whereas lactate to N-acetylaspartate ratios were 1.37 ± 1.37 in the NNLA-hypoxia group. ANOVA demonstrated a significant effect of NNLA on lactate to N-acetylaspartate ratios (p < 0.001). Inhibition of nitric oxide synthase by NNLA tended to compromise cerebral energy status during and after cerebral hypoxia-ischemia in newborn piglets.
Similar content being viewed by others
Main
Perinatal hypoxia-ischemia is an important cause of cerebral palsy in human neonates(1). Recent studies in animal models of hypoxia-ischemia have demonstrated increased amounts of NO in cerebral tissue after hypoxia-ischemia and reperfusion(2–4). NO production after hypoxia-ischemia can result in the formation of peroxynitrite, and therefore contribute to free radical-induced damage of cerebral tissue(5–8). NOS, the enzyme producing NO, is present in the cerebrum of mammals in a constitutive form in neurons and endothelial cells(9).
The inhibition of constitutive NOS has been described as resulting in partial protection of electrocortical brain activity and in preservation of the structural integrity of the NMDA-receptor/ion channel complex, and of brain cell morphology in animal models of cerebral hypoxia-ischemia(10–17). Inhibition of neuronal isoforms of constitutive NOS was suggested to reduce production of peroxynitrite and excitotoxic amino acids, whereas inhibition of endothelial isoforms of constitutive NOS was suggested to reduce cerebral hyperperfusion after hypoxia-ischemia(18). The effects on the electrocortical brain activity seemed to be dose-dependent, as higher doses of NOS inhibitors did not show beneficial effects(13,16,19).
In contrast with the previous findings, other studies of localized brain ischemia demonstrated increased infarct volume after the inhibition of NOS(20–23). These detrimental effects were explained by a massive reduction of cerebral perfusion through inhibition of endothelial NOS. Inhibitors of constitutive NOS that have been used in most studies published so far are NNLA or its methyl ester L-NAME, inhibiting both neuronal and endothelial isoforms of constitutive NOS.
Recently, a piglet model of perinatal hypoxia-ischemia was developed that closely resembles the changes in brain energy metabolism of the human neonate(24). Using MRS, dramatic changes in cerebral energy metabolism are seen during cerebral hypoxia-ischemia(25), with a rapid normalization within hours after the hypoxia-ischemia, to be followed by a secondary energy failure from 8 to 12 h after the hypoxia-ischemia event(24).
According to many of the previous studies the inhibition of constitutive NOS might have beneficial effects on cerebral energy metabolism in perinatal hypoxia-ischemia. Alternatively, if the reduction of cerebral blood flow during hypoxia-ischemia is of major importance in the causation of hypoxia-ischemia-induced cerebral lesions, and if inhibition of NOS augmented this reduction in cerebral perfusion, NOS inhibition would worsen posthypoxia-ischemia cerebral energy metabolism.
The present study was therefore designed to examine cerebral energy metabolism preceding, during, and after hypoxia-ischemia in newborn piglets using 1H- and 31P-MRS.
METHODS
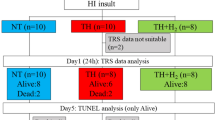
Preparation of animals. Studies were performed in 10 Yorkshire large white piglets, aged 1-3 d. Animal care protocols were approved by the Animal Care Committee of the Utrecht University. Animals were placed on a heating blanket, thereby maintaining a rectal temperature of 38.0°-39.0°C by adjusting the temperature of the blanket. Anesthesia was induced with azaperone (2 mg/kg intramuscularly). Thereafter, an i.v. line was placed in an ear vein, and metomidate (3 mg/kg) and atropine (0.01 mg/kg) were injected. Azaperone, metomidate, and atropine are compounds known to have a short half-life in piglets (L.J. Hellebrekers, personal communication). The animal was intubated. Halothane (1.5%) was added to the inhalation gas. Lidocaine (2%) was injected s.c. at incision sites, while the animals breathed spontaneously. Catheters were placed in the right femoral artery, and used for monitoring of blood pressure and arterial blood gases. Inflatable occluders were placed around the left and right common carotid arteries. After instrumentation halothane was discontinued, and the animals were transferred to the magnet. There, they were mechanically ventilated with nitrous oxide (0.79)/oxygen (0.21), using an Amsterdam Infant Ventilator. Isoflurane (0.5-1%) was added to the inhalation gas. Animals were paralyzed with pancuronium (0.3 mg/kg). Blood pressure, heart rate, end tidal CO2, and rectal temperature were recorded continuously. Arterial pH, PaO2, and PaCO2, as well as glucose, were measured at 15-min intervals throughout the initial 4 h of the study and at 60-min intervals thereafter.
Experimental protocol. Piglets were ventilated while maintaining normal blood gas values (PaO2 10.5-15.8 kPa) for a 1-h baseline period and subsequently assigned to one of two groups: hypoxia and NNLA 40 mg/kg (NNLA-hypoxia), or hypoxia and normal saline (hypoxia). After the 1-h baseline the piglets in the NNLA-hypoxia group received 40 mg/kg NNLA i.v. during 30 min. The other piglets (hypoxia) received an equal volume of normal saline. One hour after the start of the infusion of NNLA or saline, the carotid occluders were inflated and FiO2 decreased to 0.07 (t = 0 min). This resulted in PaO2 values <3.3 kPa. When a severe hypotension or a rapidly decreasing heart rate developed, FiO2 was elevated just enough to prevent further deterioration of blood pressure or heart rate. Thereafter (t = 60 min), the occluders were deflated and the FiO2 increased to obtain normoxemia (PaO2 10.5-15.8 kPa). Three hours after the reperfusion (t = 240 min) the animals were killed by an overdose of pentobarbital sodium.
Magnetic resonance studies. All experiments were performed with a Varian/SIS Co spectrometer interfaced to a 4.7-T Oxford magnet (33-cm-diameter bore size) with 32-mT/m actively shielded Oxford gradients (500-µs rise time). The head of the animal was positioned within a Helmholtz coil tuned to the proton frequency (200.057 MHz). A 3.0-cm-diameter inductively coupled surface coil tuned to the phosphorus frequency (80.984 MHz) was placed on top of the skull. Both coils were used for radiofrequency pulse transmission and signal reception.
31P-MRS experiments were performed with a 1.0-ms adiabatic half-passage excitation pulse (tan h/tan modulation functions(26)), repetition time of 10 s, and number of averages equal to 32.
1H-MRS experiments were performed with point-resolved spectroscopy localization(27) executed with 4.0-ms sinc excitation and 4.0-ms optimized sinc refocusing pulses(28). Spectra from a 12 × 12 × 12 mm3 (1.73 mL) voxel, selected in the brain as shown in Figure 1, were obtained with a repetition time of 2.5 sec, TE = 144 ms, and number of averages equal to 128.
Water suppression for 1H-MRS was achieved with chemical shift-selective spectroscopy [three 12-ms Gaussian pulses interleaved with 5.0-ms gradient crushers(29)] and a water suppression technique developed by Mescher et al.(30). These refocusing pulses (optimized sinc pulses of 16 ms) were incorporated around the second point-resolved spectroscopy 180° pulse, thereby making the double spin-echo asymmetrical [TE = TE1 + TE2 = (44 + 100) ms]. The technique of Mescher et al.(30) refocuses the J evolution of Lac during TE2, such that Lac appears positive at TE = 144 ms.
1H- and 31P-MR spectra were analyzed with frequency domain fitting software from NMRi (New Methods Research, Inc., New York, NY). In 31P-MRS the baseline was corrected. All resonances were fitted as a sum of Lorentzian- and Gaussian-shaped lines. 1H-MR spectra were analyzed on Cho, Cr, NAA, and Lac resonances. 31P-MR spectra were analyzed on PME, Pi, PDE, PCr, and ATP resonances. The pHi was determined from the chemical shift difference between Pi and PCr(31).
Data analysis. At each time, data of both groups were examined for normality and equality of variances. Statistical analysis was performed through a parametric test (two-way ANOVA with the Student-Newman-Keuls correction), or nonparametric test (ANOVA with the Kruskal-Wallis test and Dunn's multiple comparison correction) as appropriate, using a p value of 0.05 as the level of significance. Analysis within each group was performed by one-way ANOVA.
SPSS for Windows software was used for analysis. With expected group differences of 20%, power analysis revealed that groups of five animals each would be sufficient to demonstrate these differences with a β value of 0.10 and α of 0.05.
RESULTS
Physiological data. NNLA increased arterial blood pressure during normoxia and at the end of the 3-h reperfusion period (Table 1). Heart rate was lower after NNLA infusion and also during hypoxia-ischemia in the NNLA-hypoxia group. NNLA did not affect blood gas values significantly during infusion. Although arterial pH and base excess were slightly lower and PaCO2 higher in the NNLA-hypoxia group during NNLA infusion, these differences were not significant. After 1 h of hypoxia-ischemia (t = 60 min) arterial pH was significantly lower in the NNLA-hypoxia group.
Temperature was lower at the beginning of the experiment (t = -60 min), than during the remainder of the experiment. This was caused by the transfer of the animals from the operating room to the magnet, during which temperature dropped approximately 1°C. All animals regained normothermia rapidly after placement in the magnet and were normothermic from t = 0 onward.
Blood glucose values did not differ between the two groups, nor did Hb levels.
Two piglets in the NNLA-hypoxia group died between 2 and 3 h after the hypoxic-ischemic insult because of cardiac failure. Data from these two piglets are included in the t = 120 min point.
31P-MRS. Figure 2 shows an example of 31P-MR spectra of the piglets, showing resonances of PME, Pi, PDE, and ATP. 31P-MRS showed a rapid decrease in PCr/Pi ratios during hypoxia-ischemia compared with baseline values in both groups (Fig. 3, ANOVA, p < 0.001). ANOVA demonstrated a significantly lower PCr/Pi ratio in the NNLA-hypoxia group (p < 0.001). However, only at 30 and 120 min did the PCr/Pi ratio differ significantly between the two groups (p < 0.05). After hypoxia-ischemia, PCr/Pi was not significantly different from baseline values in the hypoxia group within 60 min of reperfusion, whereas PCr/Pi remained below baseline in the NNLA-hypoxia group until 3 h of reperfusion (p < 0.05).
pHi values were lower during and after hypoxia-ischemia in the NNLA group than in the hypoxia group (ANOVA, p < 0.001). Analysis at the individual points did not reach statistical significance between the two groups. pHi tended to return to baseline values faster in the hypoxia group than in the NNLA-hypoxia group, in which pHi showed a tendency to remain below baseline values.
PCr/Pi and pHi values (Fig. 4) were unchanged during the administration of NNLA (t = -60 to t = 0).
1H-MRS. 1H-MR spectra are presented in Figure 5. Cho, Cr, NAA, and-when present-Lac resonances could be clearly identified.
1H-MR spectra of a piglet before hypoxia-ischemia (hypoxia group, left top), immediately after 1 h of hypoxia-ischemia (hypoxia group, right top), and at 3 h of reperfusion in the hypoxia group (left bottom) or the NNLA-hypoxia group (right bottom). Identified peaks are Cho, total Cr (tCr), Glx, NAA, and Lac.
1H-MRS demonstrated increased Lac/NAA (Fig. 6) and Lac/Cho (data not shown) ratios in both groups during hypoxia-ischemia (ANOVA, p < 0.001), whereas NAA/Cho ratios remained unchanged in the untreated group and tended to decrease in the NNLA group. Analysis of individual points did not demonstrate significant differences (Fig. 6).
Lac was demonstrated as early as 15 min of hypoxia-ischemia, but was elevated significantly from 30 min onward. After hypoxia-ischemia, Lac disappeared within 2 h in three of five piglets of the control group, and disappeared in the other two piglets in the subsequent 2 h. Lac could be demonstrated in all animals of the NNLA group throughout the remainder of the experiment. Lac did not appear in the brain during the administration of NNLA before hypoxia-ischemia.
DISCUSSION
The present study examined the effects of inhibition of constitutive NOS on cerebral energy metabolism in a piglet model of perinatal hypoxia-ischemia. The time course of 1H-and 31P-MRS changes in brain tissue during and after hypoxia-ischemia was similar to that published by others in the same model, demonstrating the reproducibility of the model(24).
In our study short-term outcome was worse in animals with simultaneous inhibition of neuronal and endothelial NOS before cerebral hypoxia-ischemia: PCr/Pi and pHi values were lower, and Lac tended to be higher in the NNLA-hypoxia group. Conflicting results have been described previously after inhibition of neuronal and endothelial NOS and cerebral hypoxia-ischemia. Studies in adult animal models of stroke have demonstrated an increase of neuronal damage after simultaneous inhibition of neuronal and endothelial NOS(20–23). In contrast to these findings, others have demonstrated partial protection of cerebral damage after hypoxia or ischemia by inhibition of NOS(10–17). Because in the present study the administration of NNLA tended to deteriorate cerebral energy metabolism during and after cerebral hypoxia-ischemia, these results resemble the effects of simultaneous neuronal and endothelial NOS inhibition in stroke models of hypoxia-ischemia. Preservation of brain cell membrane function(32), and in particular the NMDA receptor/ion channel complex, during hypoxic hypoxia has been demonstrated after inhibition of NOS by NNLA in newborn piglets(17). Lipton et al.(33) postulated that a specific redox state of NO, i.e. the nitrosonium ion, may be neuroprotective through binding to the NMDA receptor. Because ischemia and hypoxia were applied simultaneously in the present study, our study cannot be compared with studies in which hypoxic hypoxia without ischemia has been used.
In the present study the animals received NNLA before hypoxia-ischemia, so the effects of NNLA during normoxia could be studied. NNLA under normoxic conditions did not affect the cerebral energy status, because PCr/Pi and pHi were unchanged and Lac was not formed, confirming findings of biochemical analysis of brain tissue(32). Previously it has been shown that the function of enzymes such as Na+,K+-ATPase in brain cell membranes was not affected by the administration of NNLA(17,32,34). Although blood pressure increases and heart rate decreases after administration of NNLA, cardiac output does not appear to be affected during normoxia nor during hypoxia in newborn sheep(35). In contrast to these findings studies in 1- to 2-wk-old piglets did show a decreased cardiac output after NNLA administration, but cerebral blood flow was unchanged during normoxia at doses of NNLA <80 mg/kg(36). However, we cannot entirely exclude that hemodynamic changes by NNLA administration before hypoxia-ischemia account, at least in part, for the observed differences between the two groups.
During hypoxia-ischemia limited cerebral blood flow was established through the vascular circle of Willis. Patency of the vascular circle of Willis in newborn piglets is suggested by the fact that occlusion of both carotid arteries without decreasing FiO2 did not show any changes in PCr/Pi during 10 min of occlusion (personal observation).
Recently, neuroprotective effects of NNLA immediately after cerebral hypoxia-ischemia in lambs have been shown only to be present at a dose of 10 mg/kg, whereas no protection could be demonstrated at a dose of NNLA of 40 mg/kg(16). In a previous study we have measured NOS activity in brain tissue after administration of NNLA, both in normoxia and hypoxia(17). In the present study the dose of NNLA, 40 mg/kg i.v., was chosen because it has been shown both by enzyme assays and electron spin trapping techniques to be sufficient to completely inhibit cerebral production of NO during hypoxia(17,32,37). The dose of 40 mg/kg NNLA might be too high a dose for neuroprotection in the present model, although it cannot be excluded that lower doses are effective.
From studies in knockout mice it is known that NO produced by neuronal NOS is neurodestructive, whereas NO from endothelial NOS is neuroprotective after cerebral hypoxia-ischemia(18,38). Inasmuch as effects of NNLA on arterial blood pressure are dose-dependent(36), we speculate that higher doses of NNLA inhibit endothelial NOS, whereas lower doses of NNLA inhibit neuronal NOS.
Recently, specific inhibitors of neuronal as well as endothelial NOS have become available. Using a specific inhibitor of neuronal NOS, 7-nitroindazole, neuroprotective effects have been shown in rats(39). Future studies must show its effectiveness in the present model.
In the present study the rectal temperature was carefully monitored and kept within a range of 38.0° to 39.0°C. Neuroprotective effects of moderate hypothermia have been demonstrated after cerebral hypoxia in newborn piglets(40). Cerebral temperature was not monitored in this experiment, but others using the same model have shown that tympanic temperature is unaltered after 1 h of hypoxia-ischemia(24). As both the NNLA and the untreated group underwent the same exposure to hypoxia-ischemia, it is unlikely that the brain temperature differed between the groups during and after the hypoxic-ischemic insult.
The adverse effects of NNLA on cerebral energy metabolism in the present study are most likely to be explained by inhibition of vasodilation through inhibition of endothelial NOS during and after hypoxia-ischemia as is the case in the aforementioned stroke models of cerebral hypoxia-ischemia. Although the role of NO in hypoxia-induced cerebral vasodilation is controversial and may be species-dependent, studies in adult sheep(41), rats(42), and newborn pigs(43) have demonstrated that NO is in part responsible for hypoxia-induced cerebral vasodilation. The differences between the two groups in our study also suggest NO production during cerebral hypoxia-ischemia in newborn piglets.
In the present study the volume of interest of the piglet brain (Fig. 1) did not include forebrain, cortical gray matter, or cerebellum, areas reported to show major NO-dependent hypoxia-induced vasodilation(44). Inasmuch as both carotid arteries were occluded during the hypoxia-ischemia insult in the present animal model(24) and brain perfusion was only possible through the vertebral artery, a decreased perfusion of the brain through vasoconstriction of the vertebral artery might be responsible for the observed changes during hypoxia-ischemia. After hypoxia-ischemia, a decreased perfusion of the brain by inhibition of NOS may have played a role in the delayed recovery in the NNLA group, as has been demonstrated in newborn lambs(16,45), rats(46), and pigs(47). Because NO did not seem to be the sole mediator for postischemic hyperemia in newborn piglets beyond 8 min of reperfusion(47), other factors such as cell membrane changes may be responsible for our observations.
Decreases in brain energy metabolism induce brain cell membrane injury. The effects are dependent on the severity of the energy depletion(48). In addition, a disturbance of brain energy metabolism results in long-term adverse effects on brain cell membrane function(49). From these publications it is unlikely that the piglets in the present study that received NNLA and showed a very poor cerebral energy status would eventually show an improved long-term outcome.
In conclusion, inhibition of NOS by NNLA compromised cerebral energy status during and after cerebral hypoxia-ischemia in newborn piglets. Decreased cerebral perfusion through the vertebral artery during hypoxia-ischemia and through all cerebral arteries in the reperfusion phase may be responsible for observed differences in pHi, PCr/Pi, and Lac/NAA between the two groups. The present study does not support the hypothesis that prehypoxic administration of high doses of a nonspecific NOS inhibitor is neuroprotective during hypoxia-ischemia.
Abbreviations
- Cho:
-
total choline
- Cr:
-
total (phospho)creatine
- Glx:
-
glutamate, glutamine, and GABA
- 1H-MRS:
-
proton magnetic resonance spectroscopy
- Lac:
-
lactate
- MR:
-
magnetic resonance
- NAA:
-
N-acetylaspartate
- L-NAME:
-
Nω-nitro-L-arginine methyl ester
- NMDA:
-
N-methyl-D-aspartate
- NNLA:
-
Nω-nitro-L-arginine
- NO:
-
nitric oxide
- NOS:
-
nitric oxide synthase (EC 1.14.13.39)
- PaO2:
-
arterial partial pressure of oxygen
- PaCO2:
-
arterial partial pressure of carbon dioxide
- PCr:
-
phosphocreatine
- PDE:
-
phosphodiesters
- pHi:
-
intracellular pH
- Pi:
-
inorganic phosphate
- PME:
-
phosphomonoesters
- 31P-MRS:
-
phosphorous magnetic resonance spectroscopy
- TE:
-
echo time
References
Levene MI, Kornberg J, Williams THC 1985 The incidence and severity of postasphyxial encephalopathy in full-term infants. Early Hum Dev 11: 21–28.
Sato T, Tominaga T, Ohnishi T, Ohnishi ST 1994 Electron paramagnetic resonance study on nitric oxide production during focal ischemia and reperfusion in the rat. Brain Res 647: 91–96.
Iadecola C, Xu X, Zhang F, el Fakahany EE, Ross ME 1995 Marked induction of calcium-independent nitric oxide synthase activity after focal cerebral ischemia. J Cereb Blood Flow Metab 15: 52–59.
Yoshida T, Waeber C, Huang Z, Moskowitz MA 1995 Induction of nitric oxide synthase activity in rodent brain following middle cerebral artery occlusion. Neurosci Lett 194: 214–218.
Radi R, Beckman JS, Bush KM, Freeman BA 1991 Peroxynitrite-induced membrane lipid peroxidation: the cytotoxic potential of superoxide and nitric oxide. Arch Biochem Biophys 288: 481–487.
Malinski T, Bailey F, Zhang ZG, Chopp M 1993 Nitric oxide measured by a porphyrinic microsensor in rat brain after transient middle cerebral artery occlusion. J Cereb Blood Flow Metab 13: 355–358.
Kader A, Frazzini VI, Solomon RA, Trifiletti RR 1993 Nitric oxide production during focal cerebral ischemia in rats. Stroke 24: 1709–1716.
Rubbo H, Radi R, Trujillo M, Telleri R, Kalyanaraman B, Barnes S, Kirk M, Freeman B 1994 Nitric oxide regulation of superoxide and peroxynitrite-dependent lipid peroxidation. J Biol Chem 269: 26066–26075.
Bredt DS, Glatt CE, Hwang PM, Fotuhi M, Dawson TM, Snyder SH 1991 Nitric oxide synthase protein and mRNA are discretely localized in neuronal populations of the mammalian CNS together with NADPH diaphorase. Neuron 7: 615–624.
Trifiletti RR 1992 Neuroprotective effects of NG-nitro-L-arginine in focal stroke in the 7-day old rat. Eur J Pharmacol 218: 197–198.
Buisson A, Margaill I, Callebert J, Plotkine M, Boulu RG 1993 Mechanisms involved in the neuroprotective activity of a nitric oxide synthase inhibitor during focal cerebral ischemia. J Neurochem 61: 690–696.
Nishikawa T, Kirsch JR, Koehler RC, Bredt DS, Snyder SH, Traystman RJ 1993 Effect of nitric oxide synthase inhibition on cerebral blood flow and injury volume during focal ischemia in cats. Stroke 24: 1717–1724.
Carreau A, Duval D, Poignet H, Scaton B, Vigé X, Nowicki JP 1994 Neuroprotective efficacy of NG-nitro-L-arginine after focal cerebral ischemia in the mouse and inhibition of cortical nitric oxide synthase. Eur J Pharmacol 256: 241–249.
Hamada Y, Hayakawa T, Hattori H, Mikawa H 1994 Inhibitor of nitric oxide synthesis reduces hypoxic-ischemic brain damage in the neonatal rat. Pediatr Res 35: 10–14.
Maiese K, Wagner J, Boccone L 1994 Nitric oxide: a downstream mediator of calcium toxicity in the ischemic cascade. Neurosci Lett 166: 43–47.
Dorrepaal CA, Shadid M, Steendijk P, van der Velde ET, Van de Bor M, Baan J, Van Bel F 1997 Effect of post-hypoxic-ischemic inhibition of nitric oxide synthesis on cerebral blood flow, metabolism and electrocortical brain activity in newborn lambs. Biol Neonate 72: 216–226.
Groenedaal F, Mishra OP, McGowan JE, Hoffman DJ, Delivoria-Papadopoulos M 1997 Function of cell membranes in cerebral cortical tissue of newborn piglets after hypoxia and inhibition of nitric oxide synthase. Pediatr Res 42: 174–179.
Huang Z, Huang PL, Panahian N, Dalkara T, Fishman MC, Moskowitz MA 1994 Effects of cerebral ischemia in mice deficient in neuronal nitric oxide synthase. Science 265: 1883–1885.
Nagafuji T, Sugiyama M, Matsiu T, Koide T 1993 A narrow therapeutical window of a nitric oxide synthase inhibitor against transient ischemic brain injury. Eur J Pharmacol 248: 325–328.
Yamamoto S, Golanov EV, Berger SB, Reis DJ 1992 Inhibition of nitric oxide synthesis increases focal ischemic infarction in rat. J Cereb Blood Flow Metab 12: 717–726.
Buchan AM, Gertler SZ, Huang ZG, Li H, Chaundy KE, Xue D 1994 Failure to prevent selective CA1 neuronal death and reduce cortical infarction following cerebral ischemia with inhibition of nitric oxide synthase. Neuroscience 61: 1–11.
Morikawa E, Moskowitz MA, Huang Z, Yoshida T, Irikura K, Dalkara T 1994 L-Arginine infusion promotes nitric oxide-dependent vasodilation, increases regional cerebral blood flow, and reduces infarct volume in rat stroke. Stroke 25: 429–435.
Sancesario G, Iannone M, Morello M, Bernardi G 1994 Nitric oxide inhibition aggravates ischemic damage of hippocampal but not of NADPH neurons in gerbils. Stroke 25: 436–444.
Penrice J, Lorek A, Cady EB, Amess PN, Wylezinska M, Cooper CE, D'Souza PD, Brown GC, Kirkbride V, Edwards AD, Wyatt JS, Reynolds EOR 1997 Proton magnetic resonance spectroscopy of the brain during acute hypoxia-ischemia and delayed cerebral energy failure in the newborn piglet. Pediatr Res 41: 795–802.
Roth SC, Edwards AD, Cady EB, Delpy DT, Wyatt JS, Azzopardi D, Baudin J, Townsend J, Stewart AL, Reynolds EO 1992 Relation between cerebral oxidative metabolism following birth asphyxia, and neurodevelopmental outcome and brain growth at one year. Dev Med Child Neurol 34: 285–295.
Garwood M, Ke Y 1991 Symmetric pulses to induce arbitrary flip angles with compensation for RF inhomogeneity and resonance offsets. J Magn Reson 94: 511–525.
Bottomley PA 1987 Spatial localization in NMR spectroscopy in vivo. Ann N Y Acad Sci 508: 333–348.
Mao J, Mareci TH, Andrew ER 1988 Experimental study of optimal selective 180 radiofrequency pulses. J Magn Reson 79: 1–10.
Haase A, Frahm J, Hanicke W, Matthaei D 1985 1H NMR chemical shift selective (CHESS) imaging. Phys Med Biol 30: 341–344.
Mescher M, Tannus A, O'Neil Johnson M, Garwood M 1996 Solvent suppression using selective echo dephasing. J Magn Reson 123: 226–229.
Petroff OAC, Prichard JW, Behar KL, Alger JR, den Hollander JA, Shulamn RG 1985 Cerebral intracellular pH by 31P nuclear magnetic resonance spectroscopy. Neurology 35: 781–788.
Numagami Y, Zubrow AB, Mishra OP, Delivoria-Papadopoulos M 1997 Lipid free radical generation and brain cell membrane alteration following nitric oxide synthase inhibition during cerebral hypoxia in the newborn piglet. J Neurochem 69: 1542–1547.
Lipton SA, Choi YB, Pan ZH, Lei SZ, Chen HSV, Sucher NJ, Loscalzo J, Singel DJ, Stamler JS 1993 A redox-based mechanism for the neuroprotective and neurodestructive effects of nitric oxide and related nitroso-compounds. Nature 364: 626–632.
Groenendaal F, Mishra OP, McGowan JE, Delivoria-Papadopoulos M 1995 Brain cell membrane Na+,K+-ATPase activity after inhibition of cerebral nitric oxide synthase by intravenous NG-nitro-L-arginine in newborn piglets. Biol Neonate 68: 419–425.
Dorrepaal CA 1997 Post Hypoxic-Ischemic Brain Injury of the Newborn and the Role of Nitric Oxide Inhibition. Ridderprint, Ridderkerk, Netherlands, 129–146.
Rudinsky B, Bell A, Hipps R, Meadow W 1993 Relative contribution of endothelium-derived relaxation factor to vascular tone in the systemic, pulmonary, and cerebral circulations of piglets. Dev Pharmacol Ther 20: 152–161.
Andersen CB, Ohnishi T, Groenendaal F, Mishra OP, Delivoria-Papadopoulos M 1995 The in vivo identification of free radicals in newborn piglet cerebral cortex during hypoxia. Pediatr Res 37: 41A
Huang PL, Fishman MC 1996 Genetic analysis of nitric oxide synthase isoforms: targeted mutation in mice. J Mol Med 74: 415–421.
Yoshida T, Limmroth V, Irikura K, Moskowitz MA 1994 The NOS inhibitor, 7-nitroindazole, decreases focal infarct volume but not the response to topical acetylcholine in pial vessels. J Cereb Blood Flow Metab 14: 924–929.
Amess PN, Penrice J, Cady EB, Lorek A, Wylezinska M, Cooper CE, D'Souza PD, Tyszczuk L, Thoresen M, Edwards AD, Wyatt JS, Reynolds EOR 1997 Mild hypothermia after severe transient hypoxia-ischemia reduces the delayed rise in cerebral lactate in the newborn piglet. Pediatr Res 41: 803–808.
Iwamoto J, Yang SP, Yoshinaga M, Krasney E, Krasney J 1992 Nω-nitro-L-arginine influences cerebral metabolism in awake sheep. J Appl Physiol 73: 2233–2240.
Pelligrino DA, Wang Q, Koenig HM, Albrecht RF 1995 Role of nitric oxide, adenosine, N-methyl-D-aspartate receptors, and neuronal activation in hypoxia-induced pial arteriolar dilation in rats. Brain Res 704: 61–70.
Wilderman MJ, Armstead WM 1997 Role of PACAP in the relationship between cAMP and opioids in hypoxia-induced pial artery vasodilation. Am J Physiol 272:H1350–H1358.
Ichord RN, Helfaer MA, Kirsch JR, Wilson D, Traystman RJ 1994 Nitric oxide synthase inhibition attenuates hypoglycemic cerebral hyperemia in piglets. Am J Physiol 266:H1062–H1068.
Marks KA, Mallard CE, Roberts I, Williams CE, Gluckman PD, Edwards AD 1996 Nitric oxide synthase inhibition attenuates delayed vasodilation and increases injury after cerebral ischemia in fetal sheep. Pediatr Res 40: 185–191.
Wei HM, Chi OZ, Liu X, Sinha AK, Weiss HR 1994 Nitric oxide synthase inhibition alters cerebral blood flow and oxygen balance in focal cerebral ischemia in rats. Stroke 25: 445–450.
Greenberg RS, Helfaer MA, Kirsch JR, Traystman RJ 1995 Effect of nitric oxide synthase inhibition on postischemic cerebral hyperemia. Am J Physiol 269:H341–H347.
DiGiacomo JE, Pane CR, Gwiazdowski S, Mishra OP, Delivoria-Papadopoulos M 1992 Effect of graded hypoxia on brain cell membrane injury in newborn piglets. Biol Neonate 61: 25–32.
Rosenkrantz TS, Kubin J, Mishra OP, Smith D, Delivoria-Papadopoulos M 1996 Brain cell membrane Na+, K+-ATPase activity following severe hypoxic injury in the newborn piglet. Brain Res 730: 52–57.
Author information
Authors and Affiliations
Additional information
Supported by a grant from the Wilhelmina Children's Hospital Research Fund (WKZ # 96-04).
Rights and permissions
About this article
Cite this article
Groenendaal, F., De Graaf, R., Van Vliet, G. et al. Effects of Hypoxia-Ischemia and Inhibition of Nitric Oxide Synthase on Cerebral Energy Metabolism in Newborn Piglets. Pediatr Res 45, 827–833 (1999). https://doi.org/10.1203/00006450-199906000-00008
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/00006450-199906000-00008
This article is cited by
-
Effect of Src Kinase inhibition on Cytochrome c, Smac/DIABLO and Apoptosis Inducing Factor (AIF) Following Cerebral Hypoxia-Ischemia in Newborn Piglets
Scientific Reports (2017)
-
Patterns of neonatal hypoxic–ischaemic brain injury
Neuroradiology (2010)
-
Long-Term Neuroprotection with 2-Iminobiotin, An Inhibitor of Neuronal and Inducible Nitric Oxide Synthase, after Cerebral Hypoxia-Ischemia in Neonatal Rats
Journal of Cerebral Blood Flow & Metabolism (2005)