Abstract
We investigated the development changes in the pattern of urinary metabolites of theophylline, a substrate for CYP1A2, to study when CYP1A2, which is absent in the perinatal period, fully develops during childhood. The urinary ratios of three metabolites (1-methyluric acid, 3-methylxanthine, and 1,3-dimethyluric acid) to theophylline in patients over 3 y of age show a much larger interindividual variation compared with those under 3 y of age, and the mean values of the ratios in patients over 3 y of age were greater than those in patients under 1 y of age. The urinary ratio of 1,3-dimethyluric acid (a metabolite generated by several cytochrome P450s) to 3-methylxanthine or 1-methyluric acid (metabolites generated by CYP1A2 exclusively) seemed to be relatively constant over 3 y of age; in patients under 3 y of age, these ratios were much higher than those in patients over 3 y of age. The urinary ratio of 1-methyluric acid to 3-methylxanthine or 3-methylxanthine to 1-methyluric acid seemed to be relatively invariable in all patients except those less than 1 y of age. These findings suggest that CYP1A2 activity may be programmed to mature by around 3 y of age and that CYP1A2 probably plays a major role in theophylline 8-hydroxylation at a therapeutic concentration after the full development of CYP1A2 activity.
Similar content being viewed by others
Main
Cytochrome P450s (CYPs) play a major role in the oxidative metabolism of a large number of endogenous and exogenous substrates(1). CYPs consist of multiple forms of structurally and functionally distinct hemoprotein isoenzymes, and the CYP subfamilies are not uniformly expressed from the perinatal period to adulthood. For example, some CYPs such as CYP2D6 and CYP2E1 are recognized in the liver from perinatal to elderly patients(2–4). CYP3A7 was considered specific in human fetal liver(5). However, Schuetz et al.(6) reported that CYP3A7 mRNA was detected in half of adult livers, whereas it was found in all fetal samples. Their findings suggest that CYP3A7 disappears during development in half of the population. In contrast, CYP1A2 protein(4,7) and its activity(8–10) are rarely observed in the neonatal period.
Theophylline, a substrate for CYP1A(11,12), is administered to patients with a wide age range because it is used in the treatment of neonatal apnea(13) and bronchial asthma(14). Theophylline undergoes extensive hepatic metabolism, and its metabolites are excreted in urine(15,16). In microsome studies, the formation rate of theophylline metabolites is a good measure of the in vitro CYP1A activity(17). Although both CYP1A1 and CYP1A2 can be responsible for theophylline metabolism, CYP1A1 is expressed at only very low levels in human liver, and the largest CYP1A subfamily in the liver is CYP1A2(1). These previous studies suggest that theophylline metabolites in urine probably reflect the in vivo activity of CYP1A2, and an increase in the CYP1A2 activity during childhood may be accompanied by an increase in the urinary elimination of theophylline metabolites. We, therefore, examined developmental changes in the pattern of urinary theophylline metabolites. This study will help in determining when CYP1A2 activity is fully developed.
SUBJECTS AND METHODS
Study patients and design. Fifty-one pediatric patients undergoing treatment for neonatal apnea (n = 7) and bronchial asthma (n = 44) were enrolled in the study. Table 1 summarizes the patient numbers in relation to age and gender. Informed consent was obtained from one or both parents of each patient. The study protocol was approved by the Institutional Review Board at St. Marianna University School of Medicine. During the study, blood chemistry data including liver and kidney function tests were within normal limits in all children. No child exhibited any signs or symptoms suggesting congestive heart failure. No other medications that affect theophylline metabolism such as anticonvulsants, rifampicin, macrolide antibiotics, or quinolone antibiotics(18) were administered within the week before and during the study. Two to 4 mg/kg/day or 15 to 20 mg/kg/day aminophylline was given i.v. at a constant infusion rate for the patients under 1 y of age or over 1 y of age, respectively. After 48 h of beginning infusion, 10 mL of a spot urine sample was collected on three different days between the third day and the seventh day of treatment, and a 2-mL blood sample was also drawn once. Plasma and urine samples were stored at -20°C until assayed.
Determination of theophylline in plasma and urine and its metabolites in urine. Plasma theophylline concentration was measured with a fluorescence polarization immunoassay (TDX, Abbott Laboratories, Chicago). The variation coefficients were less than 3.0% and 2.6% for 38.9 and 144.4 µmol/L of theophylline in plasma, respectively. Urinary concentrations of theophylline and its metabolites, 1-methyluric acid (1MU), 3-methylxanthine (3MX), and 1,3-dimethyluric acid (DMU), were measured by HPLC consisting of a gradient unit (LG-980-02, JASCO, Tokyo), a pump (PU-980, JASCO), an automatic sampler (AS-950, JASCO), a Wakosil ODS column (4.6 mm × 150 mm, Wako, Osaka, Japan), a variable wavelength UV detector set at 254 nm (UV-975, JASCO), and a recorder (Chromatocorder 21J, SIC, Tokyo). The mobile phase involved a combination of two phases: "A," consisting of 10 mmol/L monobasic potassium phosphate and methanol (97:3) and 5 mmol/L tetrabutylammonium, and "B," consisting of 10 mmol/L monobasic potassium phosphate and methanol (80:20) and 5 mmol/L tetrabutylammonium, and delivered at a constant flow of 1.0 mL/min. The gradient of phase A was 100% to 50% linearly from 0 to 30 min, 50% at 30 to 40 min, and 100% from 40 to 60 min. One mL of urine was mixed with 200 µL of 17% phosphoric acid and β-hydroxyethyltheophylline (Internal standard, 25 µg/sample; Sigma) and extracted with 6 mL of dichlormethane/ethylacetate/isopropanol (9:9:2). The organic layer was evaporated and reconstituted in the mobile phase "A." The quantitation of theophylline and its metabolites in urine was made by comparison with the standard curves by using the peak-height ratio method. The variation coefficients were less than 12% and 8% for 25 and 200 µmol/L of theophylline and its metabolites, respectively. The mean value derived from the three samples from each patient was used as the urinary concentration of theophylline and its metabolites.
Statistical analysis. Data are presented as mean ± SD. Statistical significance was determined by using one-way analysis of variance with Fisher's protected least significant difference test for post hoc comparisons. A p value less than 0.05 was considered statistically significant.
RESULTS
Table 2 shows the urinary ratio of each metabolite to theophylline at three sampling points and their average. There is no significant difference in each ratio between the sampling points. The ratio of DMU to theophylline was approximately 3-fold and 7-fold greater than the ratios of 3MX to theophylline and of 1MU to theophylline, respectively. The urinary ratio of the sum of three metabolites to theophylline correlated with the ratio of theophylline dose to plasma theophylline concentration (r = 0.517, p < 0.001; Fig. 1).
The urinary ratio of each metabolite to theophylline is shown as a function of age in Figure 2. In any metabolite, the ratios in patients over 3 y of age show a much larger interindividual variation than those of patients under 3 y of age. The mean ratio of 3MX or 1MU to theophylline in patients over 3 y of age was significantly higher than that in those under 3 y of age.
The urinary ratio of each metabolite, 3MX (A), 1MU (B), and DMU (C), to theophylline as a function of age. Solid squares and bars represent mean and SD, respectively, in each age group shown in Table 1. *, p < 0.05; **, p < 0.01.
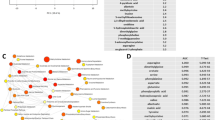
Figure 3 shows the urinary ratio of DMU or 1MU to 3MX and the urinary ratio of DMU or 3MX to 1MU as a function of age. In the urinary ratio of DMU to 3MX or 1MU, the ratio seemed to be relatively constant in patients over 3 y of age. The ratio of patients under 3 y of age was much higher than that of those over 3 y of age. In contrast, the urinary ratio of 1MU to 3MX or 3MX to 1MU seems to be relatively invariable except in those less than 1 y of age.
The urinary ratio of DMU or 1MU to 3MX (left panel) and the urinary ratio of DMU or 3MX to 1MU (right panel) as a function of age. Solid squares and bars represent mean and SD, respectively, in each age group shown in Table 1. *, p < 0.05; **, p < 0.01.
DISCUSSION
We investigated the developmental changes of CYP1A2 activity by examining the urinary ratio patterns of metabolites to theophylline in the pediatric patients. Theophylline is metabolized in the liver by 8-hydroxylation to DMU, which accounts for about half the drug clearance(19). In addition, theophylline is N-demethylated to 3MX and 1-methylxanthine, which is subsequently oxidized to 1MU by xanthine oxidase(20). These metabolites, DMU, 3MX, and 1MU, as well as theophylline, are excreted in urine(15,16). As CYP1A is responsible for N-demethylation of theophylline to 3MX and 1MU(11,12) and the largest CYP1A subfamily in human liver is CYP1A2(1), the urinary ratio of 3MX or 1MU to theophylline can be considered as a measure of in vivo CYP1A2 activity.
Theophylline elimination half-life is known to vary according to age(19). Its elimination is reported to be the fastest between 1 and 4 y of age, whereas it is impaired in neonates. Therefore, 2 to 4 mg/kg/day or 15 to 20 mg/kg/day aminophylline was given for the patients under 1 y of age or over 1 y of age, respectively. In the present study, the ratio of DMU to theophylline was approximately 3-fold and 7-fold greater than the ratios of 3MX to theophylline and of 1MU to theophylline, respectively. These results are consistent with the findings of previous studies(9,15,16).
When a drug is administered at a constant rate, drug clearance is obtained as an infusion rate divided by a steady-state plasma concentration(21). Because we did not confirm that theophylline concentration reached a steady state, the ratio of theophylline dose to plasma theophylline concentration was used instead of clearance. The ratio of the sum of three metabolites to theophylline correlated with the ratio of theophylline dose to plasma theophylline concentration. Under this condition, the urinary ratios of the metabolites to theophylline would be related to the hepatic capacity for metabolizing theophylline. Dose-dependent kinetics is known in theophylline clearance. The clearance is reported to become larger at lower infusion rates(22). We gave the lower dose to a patient less than 1 y of age who had lower in vivo CYP1A2 activity. We, therefore, assume that the change in dose administered should have little influence on the results of the current study.
The urinary ratios of 3MX and 1MU to theophylline in patients under 3 y of age were smaller than those in patients over 3 y of age. These present results agree with the findings of previous in vitro(4,7,8) and in vivo(9,10) studies showing that the CYP1A2 protein and its activity are detected rarely in the neonatal period. The ratios gradually increased by approximately 3 y of age. In patients over 3 y of age, the ratios showed a marked interindividual variation and higher mean values compared with those under 3 y of age. The huge scatter of the ratios implies a wide interindividual variation of theophylline metabolism and probably in vivo CYP1A2 activity. An extensive interindividual variability is found in CYP1A2 activity in human liver microsomes(1) as well as theophylline clearance(16). Collectively, hepatic CYP1A2 protein, which is detected only minutely in the perinatal period, seems to appear gradually after birth and may be programmed to mature by approximately 3 y of age. Although the dose administered was radically different for those under 1 y and those over 1 y of age, we assume that in vivo CYP1A2 activity increases by approximately 3 y of age because the ratio of 3MX or 1MU to theophylline in patients over 1 y and less than 3 y of age is significantly smaller than that in patients over 3 y of age. These findings imply that the developmental change may take place closer to 3 y instead of 1 y of age, but they do not account for the fastest elimination being present in patients between 1 and 4 y of age. Relatively higher liver-volume to body-weight ratio in infancy(23,24) may contribute to the faster elimination of theophylline.
The urinary ratio of 1MU to 3MX or 3MX to 1MU seems to be relatively invariable except for patients less than 1 y of age. These findings can be attributed to the fact that the same enzyme, CYP1A2, is responsible for the formation of 3MX and 1MU from theophylline(11,12). In contrast, the urinary ratio of DMU to 3MX or 1MU in patients under 3 y of age was greater than that in patients over 3 y of age, and the ratios were approximately constant in patients over 3 y of age. Previous studies reported that theophylline is metabolized to DMU by several CYP subfamilies besides CYP1A2, mainly CYP2E1 and CYP3A4(12,17,25). Because the activity and the expression of both CYP2E1 and CYP3A are recognized from perinatal period(3,4,26,27), the contribution of several CYP subfamilies in the perinatal liver to 8-hydroxylation of theophylline may result in a higher mean value for the urinary ratio of DMU to theophylline during infancy, compared with the urinary ratio of 3MX or 1MU to theophylline. Similarly, a higher mean value in the urinary ratio of DMU to 3MX or 1MU during infancy, compared with those in patients over 3 y of age, may be related to a deficiency in CYP1A2 activity and to the existence of other CYP subfamilies responsible for theophylline 8-hydroxylation.
Although several CYP subfamilies are reported to be responsible for 8-hydroxylation of theophylline to DMU in vitro(12,17,25), CYP1A2 presumably plays a main role in catabolizing theophylline to DMU in patients over 3 y of age. The urinary ratio of DMU to 3MX or 1MU in patients over 3 y of age was approximately constant, as was the ratio of 3MX to 1MU or 1MU to 3MX in patients over 1 y of age. If CYP2E1 and CYP3A, both of which show a wide interindividual variation in their in vivo activities(28,29), play a major role in generating DMU, the urinary ratio of DMU to 3MX or 1MU should be different from patient to patient over 3 y of age because CYP1A2 is exclusively responsible for generating 3MX and 1MU(11,12). In addition, the urinary ratio of DMU to theophylline shows a large interindividual variation in patients over 3 y of age, as do those of 3MX to theophylline and 1MU to theophylline. If CYP2E1 or CYP3A4 plays a major role in generating DMU, a wide interindividual variation can be seen in patients younger than 3 y of age because CYP2E1 and CYP3A4 exist in patients under 3 y of age(3,4,26,27). We, therefore, assume that CYP1A2 metabolizes theophylline to DMU after its full development. Before full development of CYP1A2, CYP2E1 and CYP3A4 besides CYP1A2 may convert theophylline to DMU.
There are some limitations to the current study. First, all patients in the study had neonatal apnea or asthma. Some diseases are known to affect theophylline clearance. A case report suggested that theophylline clearance was decreased in some patients with influenza B infection(30). A previous study implies that theophylline clearance decreases in Gram-negative bacterial sepsis(31). No patient enrolled in the present study was suspected to have these conditions. Although we found no evidence that neonatal apnea or bronchial asthma affects in vivo CYP1A2 activity, further work comparing patients and healthy subjects will be required to address the question of the influence of these diseases on in vivo CYP1A2 activity. Second, theophylline might be able to induce its own metabolism. Most of the subjects with asthma received theophylline treatment before the current study. To see whether aminophylline induces its own metabolism, we compared the urinary ratios of metabolites with theophylline in three urine samples. Because there was no significant difference in each ratio between the sampling points, aminophylline therapy up to 7 d did not affect theophylline metabolism. We also compared the ratios between patients with and without theophylline before the present study in patients over 3 y of age whose CYP1A2 was considered to be fully developed. Although we cannot draw a conclusion from the small sample of four patients without theophylline before the study, all of them had a lower than average urinary ratio (Table 3). The possibility of theophylline inducing its own metabolism remains to be studied.
In summary, we have shown the developmental changes in the metabolic capacity measured by the urinary ratios of three metabolites to theophylline, a substrate for CYP1A2. The findings of the present study suggest that CYP1A2 activity may be programmed to mature by around 3 y of age and that CYP1A2 probably plays a major role in 8-hydroxylation of theophylline at a therapeutic concentration after full development of CYP1A2. To confirm the maturation of CYP1A2 activity during childhood, additional studies in healthy subjects are desirable to evaluate the activity by other in vivo CYP1A2 probes and/or to measure directly the CYP1A2 protein and activity in the liver.
Abbreviations
- CYP:
-
cytochrome P450
- 1MU:
-
1-methyluric acid
- 3MX:
-
3-methylxanthine
- DMU:
-
1,3-dimethyluric acid
References
Guengerich FP 1995 Human cytochrome P450 enzymes. In: Oritiz de Montellano PR (ed) Cytochrome P450. Plenum Press, New York, 473–535.
Treluyer J-M, Jacqz-Aigrain E, Alvarez F, Cresteil T 1991 Expression of CYP2D6 in developing human liver. Eur J Biochem 202: 583–588.
Carpenter SP, Lasker JM, Raucy JL 1996 Expression, induction, and catalytic activity of the ethanol-inducible cytochrome P450 (CYP2E1) in human fetal liver and hepatocytes. Mol Pharmacol 49: 260–268.
Tateishi T, Nakura H, Asoh M, Watanabe M, Tanaka M, Kumai T, Takashima S, Imaoka S, Funae Y, Yabusaki Y, Kamataki T, Kobayashi S 1997 A comparison of hepatic cytochrome P450 protein expression between infancy and postinfancy. Life Sci 61: 2567–2574.
Kitada M, Kamataki T, Itahashi K, Rikihisa T, Kato R, Kanakubo Y 1985 Purification and properties of cytochrome P-450 from homogenates of human fetal liver. Arch Biochem Biophys 241: 275–280.
Schuetz JD, Beach DL, Guzelian PS 1994 Selective expression of cytochrome P450 CYP3A mRNAs in embryonic and adult human liver. Pharmacogenetics 4: 11–20.
Cazeneuve C, Pons G, Rey E, Treluyer J-M, Cresteil T, Thiroux G, d'Athis P, Olive G 1994 Biotransformation of caffeine in human liver microsomes from foetuses, neonates, infants and adults. Br J Clin Pharmacol 37: 405–412.
Berthou F, Ratanasavanh D, Alix D, Carlhant D, Riche C, Guillouzo A 1988 Caffeine and theophylline metabolism in newborn and adult human hepatocytes: Comparison with adult hepatocytes. Biochem Pharmacol 37: 3691–3700.
Grygiel JJ, Birkett DJ 1980 Effect of age on patterns of theophylline metabolism. Clin Pharmacol Ther 28: 456–462.
Carrier O, Pons G, Rey E, Richard M-O, Moran C, Badoual J, Olive G 1988 Maturation of caffeine metabolic pathways in infancy. Clin Pharmacol Ther 25: 447–453.
Sarkar MA, Jackson BJ 1994 Theophylline N-demethylations as probes for P4501A1 and P4501A2. Drug Metab Dispos 22: 827–834.
Zhang Z-Y, Kaminsky LS 1995 Characterization of human cytochromes P450 involved in theophylline 8-hydroxylation. Biochem Pharmacol 50: 205–211.
Aranda JV, Sitar DS, Parsons WD, Loughnan PM, Neims AH 1976 Pharmacokinetic aspects of theophylline in premature newborns. N Engl J Med 295: 413–416.
Weinberger M, Hendeles L 1996 Theophylline in asthma. N Engl J Med 334: 1380–1388.
Jenne JW, Nagasawa HT, Thompson RD 1976 Relationship of urinary metabolites of theophylline to serum theophylline levels. Clin Pharmacol Ther 19: 375–381.
Miller M, Opheim KE, Raisys VA, Motulsky AG 1984 Theophylline metabolism: Variation and genetics. Clin Pharmacol Ther 35: 170–182.
Sarkar MA, Hunt C, Guzelian PS, Karnes HT 1994 Characterization of human liver cytochromes P-450 involved in theophylline metabolism. Drug Metab Dispos 20: 31–37.
Boobis AR, Burley D, Davies DM, Davies DS, Harrison PI, Orme ML'E, Park BK, Goldberg LI 1991 Theophylline. In: Dollery CT (ed) Therapeutic Drugs. Churchill Livingstone Inc., New York, pp T32–T41.
Ogilvie RI 1978 Clinical pharmacokinetics of theophylline. Clin Pharmacokinet 3: 267–293.
Birkett DJ, Miners JO, Attwood J 1983 Secondary metabolism of theophylline biotransformation products in man-route of formation of 1-methyluric acid. Br J Clin Pharmacol 15: 117–119.
Rowland M, Tozer TN 1989 Constant-rate regimens. In: Rowland M, Tozer TN (eds) Clinical Pharmacokinetics: Concepts and Applications, 2nd Ed. Lea & Febiger, Philadelphia, 63–77.
Weinberger MM, Ginchansky E 1977 Dose-dependent kinetics of theophylline disposition in asthmatic children. J Pediatr 91: 820–824.
Aimi S, Yasoshima S, Sugai M, Sato B, Sakai T, Nakajima Y 1952 Studies on the weight and size of internal organs of normal Japanese. Acta Pathol Jpn 2: 173–200.
Grygiel JJ, Ward H, Ogborne M, Goldin A, Birkett DJ 1983 Relationships between plasma theophylline clearance, liver volume and body weight in children and adults. Eur J Clin Pharmacol 24: 529–532.
Fuhr U, Doehmer J, Battula N, Wolfel C, Kudla C, Keita Y, Staid AH 1992 Biotransformation of caffeine and theophylline in mammalian cell lines genetically engineered for expression of single cytochrome P450 isoforms. Biochem Pharmacol 43: 225–235.
Mathews HM, Carson LIW, Lyons SM 1988 A pharmacokinetic study of midazolam in paediatric patients undergoing cardiac surgery. Br J Anaesth 61: 302–307.
Payne K, Mattheyse FJ, Liedenberg D, Dawes T 1989 The pharmacokinetics of midazolam in paediatric patients. Eur J Clin Pharmacol 37: 267–272.
Schellens JHM, Soons PA, Breimer DD 1988 Lack of bimodality in nifedipine plasma kinetics in a large population of healthy subjects. Biochem Pharmacol 37: 2507–2510.
Kim RB, O'Shea D, Wilkinson GR 1995 Interindividual variability of chlorzoxazone 6-hydroxylation in men and women and its relationship to CYP2E1 genetic polymorphism. Clin Pharmacol Ther 57: 645–655.
Kraemer MJ, Furukawa CT, Koup JR, Shapiro GG, Pierson WE, Bierman CW 1982 Altered theophylline clearance during an influenza B outbreak. Pediatrics 69: 476–480.
Shedlofsky SI, Israel BC, McClain CJ, Hill DB, Blouin RA 1994 Endotoxin administration to humans inhibits hepatic cytochrome P450-mediated drug metabolism. 94: 2209–2214.
Acknowledgements
The authors gratefully acknowledge the contributions of the medical staff in the pediatric ward of St. Marianna University Hospital.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Tateishi, T., Asoh, M., Yamaguchi, A. et al. Developmental Changes in Urinary Elimination of Theophylline and Its Metabolites in Pediatric Patients. Pediatr Res 45, 66–70 (1999). https://doi.org/10.1203/00006450-199901000-00011
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/00006450-199901000-00011