Abstract
Chronic lung disease in neonates results from both lung injury and inadequate repair processes. Little is known about the growth factors involved in lung injury and repair, but vascular endothelial growth factor (VEGF) has recently been reported in several animal models of lung injury. VEGF is an endothelial cell-specific mitogen, which is also known as vascular permeability factor because of its ability to induce vascular leak in some tissues. Chronic lung disease is complicated by increased vascular permeability, which can be improved by avoidance of hypoxia and in some cases by dexamethasone therapy. In many cells, hypoxia stimulates VEGF expression. Also, in some cases, dexamethasone blocks VEGF expression. This study examined the role of hypoxia and dexamethasone in regulating the expression of VEGF in pulmonary artery smooth muscle cells. An ovine VEGF cDNA fragment (453 bp) was cloned and found to be highly homologous to known human sequences for VEGF165. Sheep pulmonary artery smooth muscle cells were cultured and exposed to room air, hypoxia, and dexamethasone, alone or in combination for 6 h. At baseline these cells expressed VEGF mRNA at approximately 3.9 kb. The half-life of VEGF mRNA in the smooth muscle cells was 171 min, more than 3-fold longer than previous reports for epithelial cells. Exposure to hypoxia caused a 3-fold increase in mRNA abundance, primarily through transcriptional up-regulation. Dexamethasone blocked the hypoxia-induced increase in VEGF mRNA. The results demonstrate that hypoxia and dexamethasone are regulators of VEGF expression in ovine pulmonary artery smooth muscle cells. It is not known whether VEGF derived from these cells is involved in lung injury and/or normal homeostatsis.
Similar content being viewed by others
Main
Improvements in care have dramatically improved survival from respiratory diseases in the newborn period. Unfortunately CLD continues to be a major problem resulting in significant morbidity. The pathophysiologic mechanisms underlying the development of CLD are multifactorial including the severity of acute lung disease plus barotrauma, oxygen therapy, and inflammation(1). Inadequate lung repair may also contribute, but little is known about growth factors involved in the healing process(2). Infants with CLD have abnormalities of both airways and vasculature, with evidence of increased vascular permeability. Treatment is primarily supportive with supplemental oxygen, fluid restriction, and diuretics. In some infants, dramatic improvement is seen with dexamethasone, but the mechanism(s) for this response is not known(3). In a recent report of recovery from oxygen-induced lung injury in rabbits, Maniscalco et al.(4) reported increased abundance of VEGF mRNA in alveolar epithelial cells.
VEGF, also known as vascular permeability factor and vasculotropin, is a specific endothelial cell mitogen(5–7). VEGF activities are mediated through two tyrosine kinase receptors (KDR and flt), which are expressed on endothelial cells(8–10). VEGF is expressed in a variety of tissues and cell types and is abundantly present in lung tissue(11,12). There are four alternatively spliced forms of VEGF that appear to have similar activity, but strikingly different affinities for heparin(7, 13, 14). Hypoxia induces VEGF production in a number of cell types(15–22), and multiple studies have suggested a role for VEGF in tumor angiogenesis(7, 23). In malignant glioblastomas increased expression of VEGF is found surrounding necrotic foci of tumor, presumbaly in hypoxic regions(24). VEGF activity is markedly up-regulated in ocular fluid after experimental induction of hypoxia in a primate model(25) and is proposed to be an angiogenic factor under similar circumstances in neovascularization in diabetic retinopathy and other ischemic retinal diseases(26). VEGF has also been studied in the setting of osteogenesis, a process dependent on angiogenesis. Prostaglandins E1 and E2, which are potent stimulators of new bone formation, were shown to markedly increase levels of VEGF in osteoblastic cell lines, and further, dexamethasone suppressed this up-regulation(27). One of the poorly understood activities of VEGF is its ability to induce increased vascular permeability in the skin(7, 28). Direct evidence for VEGF causing increased permeability in the lung has not been reported.
The expression of VEGF by cultured systemic vascular smooth muscle cells has been examined(18, 29, 30), but pulmonary derived cells have not been studied in vitro. Tuder et al.(31) found that VEGF was present in pulmonary vascular smooth muscle cells after lung injury secondary to chronic hypoxia. CLD results in marked increases in the cellularity of the lung, including increased numbers of smooth muscle cells. Whether VEGF derived from smooth muscle cells is important in CLD is not known. The purpose of this study was to better understand the regulation of VEGF in pulmonary vascular smooth cells by examining factors that are important regulators of clinical aspects of CLD. Specifically the effects of hypoxia and dexamethasone on the expression of VEGF mRNA in pulmonary vascular smooth muscle cells were studied.
METHODS
Cloning of ovine VEGF cDNA. Primers were constructed for use in RT-PCR using homologous regions of known human (GenBank™ accession no. X62568) and rat (GenBank™ accession no. M32167) VEGF sequences(32, 33). Primers common to all four splice variants of VEGF were chosen (the primers flank the regions of insertions and deletions). Upper primer 5′-GAAGTGGTGAAGTTCATGGA-3′; lower primer 5′-TCGGCTTGTCACATCTGCAA-3′. RT-PCR was performed using sheep lung RNA as a template at 94°C for 4 min, then 45 cycles of 94°C, 60°C, 72°C, followed by 72°C for 10 min (Life Technologies, Inc., Grand Island, NY). The amplified fragment was cloned into pGEM-T vector (Promega, Madison, WI), and sequenced using cycle sequencing (Circumvent, New England Biolabs, Beverly, MA), with multiple primers. Sequencing results were compared with known human sequences using PC/GENE (Intelligenetics; Geneva, Switzerland).
Probes. The isolated ovine VEGF cDNA was used as a template to prepare riboprobes for analysis of VEGF mRNA expression. Riboprobes were synthesized using T7 RNA polymerase (Promega) and 32P-labeled UTP to a specific activity of 2 × 106 cpm/μg ([32P]UTP, Ci/mM; DuPont NEN)(34). For normalization, antisense riboprobes or cDNA probes were made to cyclophilin(35).
Cell culture. Sheep pulmonary artery smooth muscle cells were cultured in RPMI (Life Technologies, Inc.) supplemented with 10% fetal bovine serum (Hyclone Labs, Logan, UT) by explant outgrowth technique(36). Cells were identified as smooth muscle cells by their hill and valley growth pattern and positive staining for smooth muscle cell α-actin. Early passage cells (less than 6) were seeded into P-100s plates, grown to confluence, and made quiescent in serum-free medium for 24-48 h before use. Cells were exposed to room air or hypoxia, with and without dexamethasone (Sigma Chemical Co., St. Louis, MO). Dexamethasone was studied at concentrations of 1.3, 4.0, 13, 25, and 40 mg/L. Hypoxia was achieved by infusion of a gas mixture of 95% N2, 5% CO2 into a modular incubator chamber (Billups-Rothenberg, Del Mar, CA). In seven experiments, pH, Po2, and PCo2 were measured in media. Additional plates were treated with PMA (Sigma Chemical Co.), a known inducer of VEGF expression(37). Exposure time for all experimental conditions was 6 h, except for the hypoxia time course and the actinomycin D studies where exposure times varied and are noted in the results.
Actinomycin D transcriptional inhibition. Confluent cells were made quiescent in serum-free medium for 48 h and then pretreated for 60 min with actinomycin D (Sigma Chemical Co.) 10 mg/L followed by continued actinomycin D exposure ± hypoxia. RNA was isolated for northern analysis before addition of actinomycin D, and at 30, 60, 90, 120, and 240 min after exposure to actinomycin D ± hypoxia. Preliminary studies determined that actinomycin D at 10 mg/L during the time course of this experiment was not toxic to the cells in culture.
RNA isolation and analysis. At the end of the experimental period, the cells were examined by phase contrast microscopy for evidence of cell damage or death. Total RNA was isolated from the cells using standard techniques, and poly(A)+ RNA was isolated with an oligo(dT)(Collaborative Research; Bedford, MA) cellulose affinity column and quantified by measuring absorbance at 260 and 280 nm(34, 38). Poly(A)+ RNA was loaded at 2 or 3 μg/lane, total RNA loaded at 10μg/lane, and run overnight into a 1% agarose/2.2 M formaldehyde gel at 20 V. RNA was then transferred to nitrocellulose filter (Nitro-Plus, Micron Separations, Inc.; Westboro, MA) in 10 × SSC (1 × SSC = 150 mM NaCl, 15 mM sodium citrate) and immobilized on the filter with UV cross-linking at 1200 J (UV Stratalinker, Stratagene, La Jolla, CA). The blots were prehybridized for a minimum of 2 h at 42°C in 50% formamide, 250 ng/mL sheared salmon sperm DNA, 1 × Denhardt's solution, 50 ng/mL poly(A), 0.1% SDS, and 5 × SSC. Labeled riboprobe was added to blots at a concentration of 2 × 106 cpm/mL of hybridization solution, and hybridized for 18 h at 63°C. Blots were washed in 0.1 × SSC + 0.1% SDS, and then exposed to PhosphorImager plates for 24-48 h. Results were quantified using a Bio-Rad PhosphorImager with ImageQuant software. To normalize for loading, blots were also probed for cyclophilin expression(34,35).
RT-PCR. RT-PCR was performed to specifically detect the presence of splice variants using the primers described above in the cloning experiments. These primers flank the regions containing all the exons and should identify all splice variants of VEGF. RNA isolated from cell culture experiments was used as the template at 94°C for 4 min, then 45 cycles of 94°C, 60°C, 72°C, followed by 72°C for 10 min. The amplified product was run on a 1% agarose gel and the number and sizes of fragment(s) were identified using standard size markers. Using these primers, the VEGF splice variants would yield PCR products of 332, 444, 516, and 570 bp(VEGF121, VEGF165, VEGF189, and VEGF201, respectively).
Data analysis. Results for each experiment were corrected for loading and normalized to control for each experiment. Mean and SEM were calculated for each experimental group. Data from experimental groups were compared using nonparametric statistics (Mann-Whitney) with a p value of less than 0.05 considered significant.
RESULTS
Cloning of ovine VEGF cDNA fragment. A 453-bp fragment was isolated and sequencing revealed that it corresponded to VEGF165. This fragment includes 72% of the coding sequence, and is highly homologous to both human and rat sequences (94 and 88%, respectively). The predicted amino acid sequence is shown in Table 1, aligned with known human and rat sequences. The ovine cDNA fragment includes exons common to all four forms of VEGF; thus, probes made from this cDNA can detect all four species of VEGF.
Expression of VEGF mRNA by cultured pulmonary vascular smooth muscle cells. Controls. In cells exposed to room air, VEGF mRNA was expressed predominantly as a single band at approximately 3.9 kb, as seen in Figure 1. This size would be consistent with VEGF165 mRNA as reported in other cells(29). Exposure to PMA resulted in a 9-fold increase in the abundance of this band, consistent with the reported induction by PMA(37). In some experiments a second band was seen, at about 4.1 kb. Results from RT-PCR revealed the predominant band was VEGF165, and when two bands were present, the second band was VEGF189 (data not shown).
Representative Northern blot showing expression of VEGF mRNA at baseline and after PMA treatment. Three micrograms of poly(A+) RNA from pulmonary artery smooth muscle cells were loaded in each lane. The blots were hybridized to antisense riboprobes for VEGF and cyclophilin (for loading). At baseline a single band of VEGF at about 3.9 kb could be detected. After exposure to PMA, there was a marked increase in the abundance of this band. Cyclophilin expression did not change.
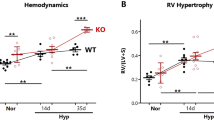
Hypoxia. Time course experiments revealed that exposure to hypoxia resulted in 2-fold increase in the abundance of VEGF mRNA by 4 h, which further increased at 6 h, and remained elevated at 16 h (data not shown). Subsequent data are reported for the 6-h time point. InFigure 2, the first lane shows control expression with a single predominant band about 3.9 kb. After exposure to 6 h of hypoxia, there was a striking increase in the abundance of the 3.9-kb band, as well as the appearance of bands at 3.7 and 4.1 kb. Not all experiments showed multiple bands after exposure to hypoxia, but all had increases in VEGF mRNA. The data for all experiments are summarized in Figure 3, where results were corrected for loading (cyclophilin expression) and normalized to control expression in each experiment. Exposure to hypoxia resulted in a significant increase over control expression (3.2 ± 0.4-fold increase; M ± SEM; n = 7). When multiple bands were present only the abundance of the 3.9-kb band was used in summarizing the data; however, inclusion of other bands gave similar results (data not shown). There was no visible evidence of cell damage from exposure to hypoxia.
Representative Northern blot showing the expression of VEGF mRNA in pulmonary artery smooth muscle cells that have been exposed to hypoxia and/or dexamethasone for 6 h. Three micrograms of poly(A+) RNA were run in each lane. In control cells, there was a strong band of hybridization at 3.9 kb. The addition of dexamethasone did not alter the baseline expression of VEGF in this experiment. Hypoxia resulted in a striking increase in the abundance of VEGF mRNA, with several size transcripts apparent. With the addition of dexamethasone at 1.3 mg/L, there was a slight attenuation of the response to hypoxia, but at a dose of 4.0 mg/L the response was clearly attenuated. Results for all studies are summarized inFigure 3. C, room air; H, hypoxia; DEX, dose of dexamethasone, mg/L.
Data from all experiments. VEGF expression was corrected for loading and then normalized to 1 for control. After exposure to hypoxia, VEGF mRNA abundance increased over 3-fold. The response to hypoxia was attenuated in the presence of dexamethasone. *p < 0.05 when compared with control; C, room air; H, Hypoxia; Dex, dose of dexamethasone, mg/L.
pH, Po2, and Pco2 measurements of media. Media from cells exposed to room air had a mean Po2 of 139 ± 1.5 kPa. Exposure to hypoxia resulted in a gradual decrease in the Po2 which reached steady state after 4 h (2 h, Po2 = 91.5 ± 4.1; 4 h = 51.5 ± 3.5; 6 h = 61.7 ± 3.1; 16 h = 62.5 ± 3.5). pH and Pco2 did not differ with varying conditions (data not shown).
Dexamethasone and room air. Exposure of cells in room air to dexamethasone 1.3 mg/L did not alter RNA abundance. Similarly, at concentrations of 4 mg/L or greater there was no statistically significant change in VEGF mRNA abundance (48-82% of control). Dexamethasone did not result in any apparent cell damage.
Dexamethasone and hypoxia. Exposure of cells to dexamethasone concurrently with hypoxia reduced the hypoxic induction of VEGF mRNA in a dose-dependent fashion. In Figure 2, the presence of low dose dexamethasone (1.3 mg/L) combined with hypoxia resulted in decreased abundance of all bands, compared with hypoxia alone; however, the expression of VEGF was still increased over control. At 4 mg/L, the abundance of VEGF was no longer significantly increased over control. Higher doses of dexamethasone(13, 25, and 40 mg/L) did not result in further suppression (data not shown). The data are summarized in Figure 3 after normalization to control. Hypoxic exposure combined with low dose dexamethasone (1.3 mg/L) resulted in a partial attenuation of the hypoxic induction (1.8 ± 0.21;n = 3), whereas hypoxia combined with higher dose dexamethasone (4.0 mg/L) almost completely blocked the hypoxic response (1.4 ± 0.27;n = 3).
RT-PCR for splice variant evaluation. RT-PCR was performed to determine whether multiple species of VEGF mRNA were present. VEGF165 was found in all samples. When two species were seen by Northern, RT-PCR identified VEGF165 and VEGF189. In some experiments, Northern blot experiments identified multiple bands only after induction by hypoxia; however, by RT-PCR both VEGF165 and VEGF189 were present in both control samples and hypoxic samples even when Northern blot identified only one band (data not shown). There was no pattern in the appearance of VEGF189 to suggest differential regulation. VEGF121 and VEGF201 were not detected.
Actinomycin D transcriptional inhibition. The rates of decline in VEGF mRNA in the presence of actinomycin D are shown inFigure 4. In cells exposed to room air the half-life was 171 ± 12 min. After exposure to hypoxia, there was no significant change in the stability of the mRNA, with a half-life of 175 ± 22 min.
DISCUSSION
VEGF is a highly conserved growth factor whose localization to epithelial cells in normal lung places it in a strategic position to stimulate the adjacent growth of vessels which is critical for normal respiration to occur. The increased expression of VEGF in epithelial cells during recovery from hyperoxia in rabbits supports the idea that VEGF may be participating in the repair process and recovery of injured vessels(4). Although VEGF mRNA expression in smooth muscle cells is not found in normal lung, it is present in lung injury(31). VEGF has been associated with repair of other tissues and is thought to support angiogenesis and possibly to be related to increased permeability in wounds(39,40). In the lung, VEGF derived from nonepithelial cells may have a different role than epithelial derived VEGF. Additional cellular sources of VEGF could result in higher local concentrations of VEGF and function not only as a mitogen but also contribute to increased vascular permeability.
In this study we show that cultured pulmonary vascular smooth muscle cells produce VEGF mRNA and thus are potential sources for VEGF production in the lung in vivo. The induction of VEGF mRNA in smooth muscle cells by decreased oxygen tension, suggests that these cells could be important producers of VEGF during hypoxia associated with lung injury. One of the proposed mechanisms for sensing oxygen tension is through heme-containing proteins, acting in a fashion similar to the regulation of erythropoietin(16). In human retinal epithelial cells and rat astrocytoma cells, the increase in VEGF mRNA after hypoxia was found to be secondary to a dramatic increase in mRNA stability(15). However, in human umbilical vein endothelial cells, expression of VEGF mRNA was not present at baseline, but a significant increase occurred after hypoxia, presumably through transcriptional up-regulation(21). In rat aortic smooth muscle cells, IL-1β increases VEGF abundance, through both an increase in mRNA stability and increased transcription(30). The mechanism(s) of hypoxic induction of VEGF has not previously been reported in vascular smooth muscle cells. In the presence of actinomycin D, we found no evidence of increased mRNA stability in cells exposed to hypoxia, suggesting that increased abundance of VEGF mRNA seen after hypoxic exposure was via a transcriptional mechanism. We cannot exclude the possibility that actinomycin D was inhibiting a factor mediating stability; however, we think this is unlikely because in the presence of actinomycin, hypoxia has been shown to increase stability in other cells, e.g. retinal epithelial cells(15). Interestingly, the half-life of VEGF mRNA in the pulmonary vascular smooth muscle cells was 3-fold longer than the half-life reported for VEGF mRNA from other types of cells(15, 22). The mechanism for the increased stability of the mRNA in smooth muscle cells is not known but such cell specific regulation of VEGF mRNA could allow for cell specific effects of exogenous agents to block VEGF expression.
The decrease in VEGF mRNA abundance found when dexamethasone was present during hypoxic exposure of the smooth muscle cells is likely through blocking transcription. Dexamethasone is known to block AP-1 mediated transcription, and the VEGF promoter has potential binding sites for AP-1 transcription factors(13). In National Institutes of Health 3T3 cells, dexamethasone has no effect on either baseline or hypoxia-induced VEGF expression but dexamethasone did block phorbol ester induction of VEGF(19). Similar results have also been reported in human mesangial cells with dexamethasone blocking induction by phorbol esters, but not altering baseline or hypoxia effects(41). In contrast, dexamethasone did suppress baseline expression of VEGF in osteoblasts(27). In our study, dexamethasone blocked the increase in VEGF mRNA during exposure of the pulmonary vascular smooth muscle cells to hypoxia, suggesting that transcription was via the AP-1 site. Recent studies have implicated hypoxia-inducible factor 1 in transcriptional activation of VEGF in Hep3B cells(42). The role of hypoxia-inducible factor 1 in the hypoxic induction of VEGF in pulmonary vascular smooth muscle cells has not been examined.
In the pulmonary vascular smooth muscle cells VEGF165 was the predominant splice variant, although VEGF189 was also detected in some samples. Because the isoforms have varying affinities for heparin, differential expression could result in alterations in the bioavailability of VEGF(43, 44). However, although we could identify multiple isoforms by RT-PCR, there was no evidence that hypoxia resulted in differential induction. This is similar to the results of Levy et al.(45), who examined hypoxic induction of VEGF in rat cardiac myocytes, including RT-PCR to determine the specific isoforms expressed and found that the isoforms were coordinately regulated. The significance of the expression of the alternative forms needs further study.
VEGF has been shown to cause increased permeability in the skin after s.c. injection in rabbits(28). Many studies have implicated VEGF as a permeability enhancing factor primarily because of its co-localization in regions of edema, e.g. tumors and delayed hypersensitivity(7, 46). An early study of malignant human astroglial tumor cells described a factor present in conditioned media (likely VEGF) that induced a marked increase in capillary vascular permeability which could be blocked with dexamethasone pretreatment(47). The high levels of expression in normal lung, where there is no evidence of vascular leak suggests that VEGF does not always induce increased permeability. The factors that determine the ability of VEGF to induce vascular leak are not known but possibly higher concentrations (as might be present in injured lung) or receptor expression are involved.
We speculate that expression of VEGF mRNA by pulmonary vascular smooth muscle cells is involved in the pathophysiology of chronic lung disease. In chronic lung disease, hypoxia may induce VEGF expression and dexamethasone therapy may block this augmented VEGF expression. Further study of the role and regulation of VEGF in lung diseases is needed, especially to pinpoint factors that may modulate the permeability enhancing effects of this growth factor.
Abbreviations
- VEGF:
-
vascular endothelial growth factor
- CLD:
-
chronic lung disease
- RT:
-
reverse transcriptase
- PCR:
-
polymerase chain reaction
- PMA:
-
phorbol 12-myristate 13-acetate
References
Abman SH, Groothius JR 1994; Pathophysiology and treatment of bronchopulmonary dysplasia. Pediatr Clin North Am 41: 277–315.
Perkett EA 1995; Role of growth factors in lung repair and diseases. Curr Opin Pediatr 7: 242–249.
Yoder MC, Chua R, Tepper R 1991; Effect of dexamethasone on pulmonary inflammation and pulmonary function of ventilator dependent infants with BPD. Am Rev Respir Dis 143: 1044–1048.
Maniscalco WM, Watkins RH, Finkelstein JN, Campbell MH 1995; Vascular endothelial growth factor mRNA increases in alveolar epithelial cells during recovery from oxygen injury. Am J Respir Cell Mol Biol 13: 377–386.
Leung DW, Cachianes G, Kuang W-J, Goeddel DV, Ferrara N 1989; Vascular endothelial growth factor is a secreted angiogenic mitogen. Science 246: 1306–1312.
Connolly DT 1991; Vascular permeability factor: a unique regulator of blood vessel function. J Cell Biochem 47: 219–223.
Dvorak HF, Brown LF, Detmar M, Dvorak AM 1995; Vascular permeability factor/vascular endothelial growth factor, microvascular hyperpermeability, and angiogenesis. Am J Pathol 146: 1029–1039.
Neufeld G. Tessler S, Gitay-Goren H, Cohen T, Levi B-Z 1994; Vascular endothelial growth factor and its receptors. Prog Growth Factor Res 5: 89–97.
Barleon B, Hauser S, Schöllmann C, Weindel K, Marmé D, Yayon A, Weich HA 1994; Differential expression of the two VEGF receptor flt and KDR in placenta and vascular endothelial cells. J Cell Biochem 54: 56–66.
Jakeman LB, Winer J, Bennett GL, Altar CA, Ferrara N 1992; Binding sites for vascular endothelial growth factor are localized on endothelial cells in adult rat tissues. J Clin Invest 89: 244–253.
Monacci WT, Merrill MJ, Oldfield EH 1993; Expression of vascular permeability factor/vascular endothelial growth factor in normal rat tissues. Am J Physiol 264:C995–C1002.
Bacic M, Edwards NA, Merrill MJ 1995; Differential expression of vascular endothelial growth factor (vascular permeability factor) forms in rat tissues. Growth Factors 12: 11–15.
Tischer E, Mitchell R, Hartman T, Silva M, Gospodarowicz D, Fiddes JC, Abraham JA 1991; The human gene for vascular endothelial growth factor. J Biol Chem 266: 11947–11954.
Ferrara N, Houck K, Jakeman L, Leung DW 1992; Molecular and biological properties of the vascular endothelial growth factor family of proteins. Endocr Rev 13: 18–32.
Shima DT, Deutsch U, D'Amore PA 1995; Hypoxic induction of vascular endothelial growth factor (VEGF) in human epithelial cells is mediated by increase in mRNA stability. FEBS Lett 370: 203–208.
Goldberg MA, Schneider TJ 1994; Similarities between the oxygen-sensing mechanisms regulating the expression of vascular endothelial growth factor and erythropoietin. J Biol Chem 269: 4355–4359.
Minchenko A, Bauer T, Salceda S, Caro J 1994; Hypoxic stimulation of vascular endothelial growth factor expression in vitro and in vivo. Lab Invest 71: 374–379.
Brogi E, Wu T, Namiki A, Isner JM 1994; Indirect angiogenic cytokines upregulate VEGF and bFGF gene expression in vascular smooth muscle cell, whereas hypoxia upregulates VEGF expression only. Circulation 90: 649–652.
Finkenzeller G, Technau A, Marmé D 1995; Hypoxia-induced transcription of the vascular endothelial growth factor gene is independent of functional AP-1 transcription factor. Biochem Biophys Res Commun 208: 432–439.
Iizuka M, Yamauchi M, Ando K, Hori N, Furusawa Y, Itsukaichi H, Fukutsu K, Moriya H 1994; Quantitative RT-PCR assay detecting the transcriptional induction of vascular endothelial growth factor under hypoxia. Biochem Biophys Res Commun 205: 1474–1480.
Namiki A, Brogi E, Kearney M, Kim EA, Wu T, Couffinhal T, Varticovski L, Isner JM 1995; Hypoxia induces vascular endothelial growth factor in cultured human endothelial cells. J Biol Chem 270: 31189–31195.
Levy AP, Levy NS, Goldberg MA 1996; Post-transcriptional regulation of vascular endothelial growth factor by hypoxia. J Biol Chem 271: 2746–2753.
Warren RS, Yuan H, Matli MR, Gillett NA, Ferrara N 1995; Regulation by vascular endothelial growth factor of human colon cancer tumorigenesis in mouse model of experimental liver metastasis. J Clin Invest 95: 1789–1797.
Shweiki D, Itin A, Soffer D, Keshet E 1992; Vascular endothelial growth factor induced by hypoxia may mediate hypoxia-initiated angiogenesis. Nature 359: 843–845.
Miller JW, Adamis AP, Shima DT. D'Amore PA, Moulton RS, O'Reilly MS, Folkman J, Dvorak HF, Brown LF, Berse B, Yeo T-K, Yeo K-T 1994; Vascular endothelial growth factor/vascular permeability factor is temporally and spatially correlated with ocular angiogenesis in a primate model. Am J Pathol 145: 574–584
Aiello LP, Avery RL, Arrigg PG, Keyt BA, Jampel HD, Shah ST, Pasquale LR, Thieme H, Iwamoto MA, Park JE, Nguyen HV, Aiello LM, Ferrara N, King GL 1994; Vascular endothelial growth factor in ocular fluid of patients with diabetic retinopathy and other retinal disorders. N Engl J Med 331: 1480–1487.
Harada S, Nagy JA, Sullivan KA, Thomas KA. Endo N, Rodan GA, Rodan SB 1994; Induction of vascular endothelial growth factor expression by prostaglandin E2 and E1 in osteoblasts. J Clin Invest 93: 2490–2496.
Collins PD, Connolly DT, Williams TJ 1993; Characterization of the increase in vascular permeability induced by vascular permeability factor in vivo. Br J Pharmacol 109: 195–199.
Ferrara N, Winer J, Burton T 1991; Aortic smooth muscle cells express and secrete vascular endothelial growth factor. Growth Factors 5: 141–148.
Li J, Perrella MA, Tsai J-C, Yet S-F, Hsieh C-M, Yoshizumi M, Patterson C, Endege WO, Zhou F, Lee M-E 1995; Induction of vascular endothelial growth factor gene expression by interleukin-1β in rat aortic smooth muscle cells. J Biol Chem 270: 308–312.
Tuder RM, Flook BE, Voelkel NF 1995; Increased gene expression for VEGF and the VEGF receptors KDR/Flk and Flt in lungs exposed to acute or to chronic hypoxia. J Clin Invest 95: 1798–1807.
Conn G, Bayne ML, Soderman DD, Kwok PW, Sullivan KA, Palisi TM, Hope DA, Thomas KA 1990; Amino acid and cDNA sequences of a vascular endothelial cell mitogen that is homologous to platelet-derived growth factor. Proc Natl Acad Sci USA 87: 2628–2632.
Weindel K, Marmé D, Weich HA 1992; AIDS-associated Kaposi's sarcoma cells in culture express vascular endothelial growth factor. Biochem Biophys Res Commun 183: 1167–1174.
Perkett EA, Pelton RW, Meyrick B, Gold L, Expression of transforming growth factor β mRNAs and proteins in vascular remodelling in the sheep air embolization model of pulmonary hypertension. Am J Respir Cell Mol Biol 11: 16–24.
Danielson PE, Forss-Petter S, Brow MA. Calavetta L, Douglass J, Milner RS, Sutcliffe JG 1988; p1B15: a cDNA clone of the rat mRNA encoding cyclophilin. DNA 7: 261–267
Hoover RL, Rosenberg R, Haering W, Karnovsky MJ 1980; Inhibition of rat arterial smooth muscle cell proliferation by heparin. Circ Res 47: 578–583.
Dolecki GJ, Connolly DT 1991; Effects of a variety of cytokines and inducing agents on vascular permeability factor mRNA levels in U937 cells. Biochem Biophys Res Commun 180: 572–578.
Chomczynski P, Sacchi H 1987; Single-step method of RNA isolation by acid guanidium thiocyanate-phenol-chloroform extraction. Anal Biochem 162: 156–159.
Brown LF, Yeo K-T, Berse B, Yeo T-K, Senger DR, Dvorak HF, Van De Water L 1992; Expression of vascular permeability factor (vascular endothelial growth factor) by epidermal keratinocytes during wound healing. J Exp Med 176: 1375–1379.
Peters KG, DeVries C, Williams LT 1993; Vascular endothelial growth factor receptor expression during embryogenesis and tissue repair suggests a role in endothelial differentiation and blood vessel growth. Proc Natl Acad Sci USA 90: 8915–8919.
Iijima K, Yoshikawa N, Connolly DT, Nakamura H 1993; Human mesangial cells and peripheral blood mononuclear cells produce vascular permeability factor. Kidney Int 44: 959–966.
Forsythe JA, Jiang BH, Iyer NV, Agani F, Leung SW, Koos RD, Semenza GL 1996; Activation of vascular endothelial growth factor gene transcription by hypoxiainducible factor 1. Mol Cell Biol 16: 4604–4613.
Houck KA, Leung DW, Rowland AM, Winer J, Ferrara N 1991; Dual regulation of vascular endothelial growth factor bioavailability by genetic and proteolytic mechanisms. J Biol Chem 267: 26031–26037.
Park JE, Keller GA, Ferrara N 1993; The vascular endothelial growth factor (VEGF) isoforms: differential deposition into the subepithelial extracellular matrix and bioactivity of extracellular matrix-bound VEGF. Mol Biol Cell 4: 1317–1326.
Levy AP, Levy NS, Loscalzo J, Calderone A, Takahashi N, Yeo K-T, Koren G, Colucci WS, Goldberg MA 1995; Regulation of vascular endothelial growth factor in cardiac myocytes. Circ Res 76: 758–766.
Brown LF, Olbricht SM, Berse B, Jackman RW, Matsueda G, Tognazzi KA, Manseau EJ, Dvorak HF, VanDeWater L 1995; Overexpression of vascular permeability factor (VPF/VEGF) and its endothelial receptors in delayed hypersensitivity skin reactions. J Immunol 154: 2801–2807.
Bruce JN, Criscuolo GR, Merrill MJ, Moquin RR, Blacklock JB, Oldfield EH 1987; Vascular permeability induced by protein product of malignant brain tumors: inhibition by dexamethasone. J Neurosurg 67: 880–884.
Acknowledgements
The authors thank Rhoda Jones and Lynn Hall for their technical assistance.
Author information
Authors and Affiliations
Additional information
Supported in part by Turner Scholars Program, T35 HL07717, HL36526. J.G.K. is a recipient of a Resident's Research Award.
Presented in part at The Society for Pediatric Research, San Diego, May 1995.
Rights and permissions
About this article
Cite this article
Klekamp, J., Jarzecka, K., Hoover, R. et al. Vascular Endothelial Growth Factor Is Expressed in Ovine Pulmonary Vascular Smooth Muscle Cells in Vitro and Regulated by Hypoxia and Dexamethasone . Pediatr Res 42, 744–749 (1997). https://doi.org/10.1203/00006450-199712000-00005
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/00006450-199712000-00005