Abstract
Studies were performed on isolated perfused kidneys (IPK) from postnatal developing rabbits to ask 1) whether the high renal vascular resistance (RVR) at birth involves intrinsic renal mechanisms, 2) whether nitric oxide (NO) release is involved in the modulation of renal vascular tone, and 3) whether NO modulates exogenous angiotensin II(AII)-induced vasoconstrictions. Kidenys isolated from 1-wk-old (during nephrogenesis), 3-wk-old (after nephrogenesis), and 6-wk-old rabbits were perfused in the presence of 10-5 M indomethacin. RVR decreased with age from 12.7 ± 0.6 at 1 wk to 10.1 ± 0.5 mm Hg min g mL-1 at 6 wk. Nω-Nitro-L-arginine methyl ester (L-NAME, 10-4 M) comparably increased RVR by about 30% at 1, 3, and 6 wk. The vasoconstrictions induced by 10-8 M AII increased basal pressure from 28% at 1 wk to 78% at 6 wk and were potentiated by L-NAME by about 100%. In contrast, the vasoconstrictions induced by 10-10 M AII decreased from 8% at 1 wk to 0% at 6 wk and were potentiated by L-NAME by about 250% at 1 and 3 wk. We conclude that during postanatal development: 1) RVR in IPK decreases in absence of AII and extrarenal influences, suggesting that high RVR at birth involves intrinsic mechanisms, 2) L-Arg/NO modulates basal tonus in developing IPK, and, 3) renal vasoconstrictor responses to exogenous AII are buffered by NO at early postnatal stages and follow an AII concentration-dependent developmental pattern. A specific neonatal high affinity AII/NO interaction disappearing after nephrogenesis completion precedes a low affinity AII/NO interaction, which progressively increases toward adult ages. These findings are in favor of a specific involvement of AII-NO interactions in the control of developing renal hemodynamics.
Similar content being viewed by others
Main
The immature kidney is characterized by a high RVR in vivo in various species including the human(1). A rapid decline of RVR has been shown to occur postnatally, resulting in an increase in RBF and GFR, which contributes to the renal adaptation to extrauterine life(2). Whether birth or the completion of nephrogenesis, which may occur several weeks after birth in some species, is the stimulus of this process is still a matter of debate(3, 4). The extent and the rapidity of these changes, however, suggest that a shift in the humoral and/or nervous control of renal hemodynamics is involved.
AII(5) and NO(6, 7) have been shown to be involved in the control of renal hemodynamics in both newborn and adult mammals. However, the interactions of NO and endogenous AII in regulating RBF, have been studied mainly in the adult. Thus, the role of NO in blunting the action of various vasoconstrictors(8–11), including AII in renal vessels(11–15), has been demonstrated by experiments of endothelium removal or NOS inhibition. Moreover, in anesthetized animals, both AII receptor antagonists and angiotensin-converting enzyme inhibitors have been shown to attenuate the renal vasoconstrictor response to L-NAME, a NOS inhibitor, without changing its systemic pressor effect(16–19). In turn, a number of these studies suggest that the renal but not the systemic response to NOS inhibitors is predominantly mediated by AII.
Although the renin-angiotensin system has been shown to be highly activated both systemically and intrarenally at birth, maneuvers that alter this system have not been able to identify conclusively AII as a causative agent of the high RVR in the developing kidney(20, 21). Recent studies performed on the anesthetized pig and piglet indicate that intrarenal inhibition of either NOS or AT1 AII receptor produced greater changes in RVR in developing piglets than in adult pigs. Moreover, RVR increases induced by the inhibition of NOS were virtually abolished by AT1 receptor blockade in adult and only attenuated in developing piglet, suggesting that other systemic or local renal vasoconstrictors may participate in the piglet's renal hemodynamic responses to intrarenal NO inhibition(22).
The present experiments were designed to ask 1) whether the high RVR at birth involves mechanisms intrinsic to the kidney, 2) whether NO release is involved in the modulation of basal renal vascular tone, and 3) whether NO modulates exogenous AII-induced vasoconstrictions during postnatal development. To achieve these goals, we used an in vitro neonatal model of rabbit IPK, which lacks circulating angiotensinogen and AII production and which allows the exclusion of the effects of any other, extrarenal regulating factor.
METHODS
Drugs. AII and indomethacin were obtained from Sigma Chemical Co. (St. Louis, MO). AII was dissolved in water at a final concentration of 10-3 M and stored at -70 °C in aliquots of 100 μL. L-NAME and L-Arg were purchased from Sigma and were freshly prepared each day before use in isotonic NaCl (L-NAME) or perfusate (L-Arg). Tiletamine-zolazepam and heparin were obtained from Reading Laboratories (Paris, France).
Preparation of rabbit IPKs. The kidneys of New Zealand rabbits at various postnatal ages (1, 3, and 6 wk) were isolated and then single-pass perfused in vitro, at constant flow and stabilized pressure, under filtering conditions. The method of artificial insemination allowed the obtention of rabbits of precise ages. The animals were anesthetized with tiletamine-zolazepam (1 mg of tiletamine and 1 mg zolazepam, per 100 g of body weight, i.m.), followed by local anesthesia of the abdominal wall with lidocaine 1%. The left kidney was exposed through a median abdominal wall incision. The dissections were performed under the microscope. The left ureter and renal vessels were dissected and cleaned, and the renal vein and artery were separated. Next, the vena cava inferior and the abdominal aorta were dissected, including the confluences (renal vein/inferior vena cava and aorta/renal artery). The perirenal tissue was removed before tying the left suprarenal artery and the lumbar arteries. The site for catheterization of the aorta was prepared, and 50 IU of heparin were injected into the inferior vena cava. The abdominal aorta was ligated up-stream to the left renal artery. From this moment on, the duration of renal ischemia was measured. The infrarenal aorta was catheterized with a double lumen, 22-G catheter moved up to the origin of the left renal artery. The catheter was kept temporally in place with a clamp, so that perfusion could be started in situ, allowing a time of ischemia of less than 60 s in all experiments. Threads around the catheter were then tied, and the aorta-renal artery combination was excised, separating it from all surrounding connective, neural, and vascular tissues, and transferred onto a thermostatically controlled holder. The ureter was kept open, to maintain kidney under filtering conditions.
Perfusion of the kidney. The isolated kidneys were perfused in a single pass open circuit by means of a computer-assisted pump. The whole circuit, including the kidney holder and the reservoir containing the perfusate, was kept at 37 °C through a parallel heating circuit. All kidney preparations were perfused at a constant flow (Q) of 4 mL min-1 g kidney weight-1. The perfusion pressure resulting from this flow was considered to reflect the total RVR and was continuously recorded through the double lumen catheter using a Statham pressure transducer(model P23Db, Gould Inc., Cleveland, OH). The left kidney was used as a weight basis for calculation. A computerized data acquisition system continuously collected pressure and flow values at 1 Hz throughout the experiment. AII was administered through automatically pushed syringes, which drained in close proximity to the renal artery with an infusion rate (q) of 0.5 mL min-1. AII was dissolved in the perfusion medium. The concentration of infused AII (C) was adjusted to obtain the required final concentration in the renal artery perfusate (Cperf = 10-10 or 10-8 M) whereby Cperf = C× q/Q. The basic perfusion solution was a Krebs-Henseleit bicarbonate buffer, pH 7.4, composed of a synthetic perfusion fluid(Plasmion®; Rhône-Poulenc Rörer Laboratories, Paris, France) containing 30 g/L modified gelatin as oncotic agent, and (in 10-3 M): Na+ 150, K+ 5, Mg2+ 1.5, and lactate 30 and supplemented with Ca2+ 1.5, glucose 11, and NaCO3- 24. Indomethacin(10-5 M) was added to the perfusate medium to rule out the mediating effects of cyclooxygenase products in the vasodilations. The perfusate was thermostated at 37 °C, continuously filtered through a 1.2-μm sieve, and gassed with 95% O2-5% CO2.
Experimental protocols. Eighty-four kidney preparations were randomly used to perform 12 different groups of experiments. The 12 groups of kidney preparations differed by the age of the animals (1, 3, and 6 wk), the absence or presence of 10-4 M L-NAME in the perfusion medium throughout the experiment and the concentration of AII infused (10-10, 10-9, or 10-8 M). The numbers of preparations performed for each group are shown in Table 1 as well as in Figs. 1 and 2. Whatever the groups, RVR was measured after an initial 30-min equilibration period before a single concentration (10-10, 10-9, or 10-8 M) of AII was infused. The AII-induced perfusion pressure increase generally reached maximum values within 5 min. Therefore, AII was infused over a period of 6 min. As a general rule, perfusion pressure returned to a stable baseline within 20 min after turning off AII infusion. Therefore, perfusion pressure changes induced by AII were recorded over a period of 30 min after starting peptide infusion.
RVR in 1-, 3-, and 6-wk-old rabbit kidneys perfused at 4 mL min-1 g-1 with control perfusate (○) or in the presence of 10-4 M L-NAME (•). Data are expressed per g of left kidney weight(gLKW). Numbers in parentheses denote the number of preparations performed in each group. *p < 0.05 compared with corresponding control perfusate.
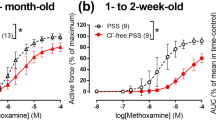
Mean tracings depicting the effect of 10-10 M(upper panels) and 10-8 M AII (lower panels) on perfusion pressure of kidneys isolated from 1-wk-old (left panels), 3-wk-old (middle panels), and 6-wk-old rabbits (right panels), perfused at constant flow (4 mL min-1 g kidney weight-1 in the absence (○) or presence of 10-4 M L-NAME(□). The number of kidney preparations performed in each group is shown in parenthesis. Net percent changes of basal perfusion pressures are shown as means ± SEM.
Expression of data. The computer-acquired data were used for further computer-assisted calculations. RVR was calculated at the end of the equilibration period by dividing the measured perfusion pressure by renal perfusion flow. RVR was expressed as mm Hg-1·(mL·min)-1 per g-1 of contralateral kidney weight. The effect of vasoactive substances is characterized not only by the maximal increase in perfusion pressure but also by the kinetic profile of these changes. To integrate these changes, we chose to represent the constrictor responses to AII by calculating the surface areas under the respective traces during the 6-min duration of AII infusion. The fact that in all experiments the maximal effect in response to AII was reached within a 6-min time allowed this mode of data expression. As basal perfusion pressures were different among the various age groups, the constrictor peak areas were expressed as net percent increases over the corresponding area under the basal pressure line. All reported data are expressed as means ± SEM. ANOVA was performed on the absolute values of RVR, and relative responses to AII and differences between means were further assessed with the Student-Newman-Keuls test. A value of p < 0.05 was considered statistically significant.
RESULTS
RVR in the isolated perfused developing kidneys. Mean values for contralateral (right) kidney weight, basal perfusion pressures and the number of kidney preparations performed in the various experimental groups are shown in Table 1. Kidney weights followed a 5-fold increase between the 1st and 6th wk of life. RVR exerted a progressive, declining developmental profile (p < 0.5 in one-way variance analysis), decreasing by 20% between the 1st and 6th wk. In the presence of L-NAME, RVR was significantly higher in each studied age group (Fig. 1). The percent increases of RVR due to L-NAME were comparable (around 30%) at 1, 3, and 6 wk.
Renal vasoconstrictor responses to AII. Fig. 2 shows the changes in mean perfusion pressure with time in the protocols used to compare the sensitivity of the kidneys isolated from 1-, 3-, and 6-wk-old rabbits with the highest (10-10 M) and the lowest (10-8 M) AII. Responses to AII, 10-9 M, displayed an intermediate profile. In the absence of 10-4 M L-NAME, AII induced a raise in perfusion pressure, which peaked within the 6-min infusion period in all experimental groups, except in 6-wk-old rabbit IPKs, where 10-10 M AII was unable to elicit any vasoconstriction. Quantification of the AII-induced vasoconstrictor effects at the various concentrations and at the various studied ages, by calculating the surface areas under the respective traces during the 6-min duration of AII infusion, are represented in Fig. 3. The developmental changes in the vasoconstrictor responses to AII followed a pattern depending upon the concentration of AII infused. At the low, 10-10 M concentration, AII significantly increased perfusion pressure by 7.5 ± 2.7% in 1-wk-old kidney preparations. This response rapidly declined with age, reaching 3.4 ± 1.5% at 3 wk and virtually disappeared at 6 wk. In marked contrast, the vasoconstrictor responses to the higher, 10-9 M and 10-8 M, AII concentrations, progressively increased with age, by 28.4 ± 4.1%, 65.4 ± 13.4%, and 77.6± 11.8% at 1, 3, and 6 wk, respectively, at the 10-8 M AII concentration (Fig. 3A). Accordingly, the dose-response curves displayed a progressive right shift in 1-, 3-, and 6-wk-old IPKs (Fig. 3B).
Effects of 10-10, 10-9, and 10-8 M AII on perfusion pressure in kidneys isolated from 1-, 3-, and 6-wk-old rabbits, perfused with control perfusate (○) or in the presence of 10-4 M L-NAME (•). Perfusion pressure changes are shown as a function of age at each AII concentration (A) or as a function of AII concentration at each age (B). *p < 0.05 compared with corresponding control perfusate as determined by two-way variance analysis. # = significant pressure changes in response to AII(p < 0.05) as determined by t test. The respective numbers of kidney preparations are shown in Table 1 or Fig. 2. Data are expressed as noted in“Methods.”
Renal vasoconstrictor responses to AII in the presence of L-NAME. As shown in Fig. 2, the vasoconstrictor responses, if any, were potentiated by NO synthesis inhibition whatever the age group or the concentration of AII infused. In addition, the relative potentiating effect of L-NAME on the vasoconstriction induced by a given concentration of AII was not significantly different between 1-, 3-, and 6-wk-old rabbits (Fig. 4). Accordingly, as in the absence of L-NAME, the developmental patterns of AII-induced vasoconstrictions in the presence of L-NAME were concentration-dependent, decreasing with age at 10-10 M and increasing with age at 10-9 M and 10-8 M (Fig. 3A). Thus, at the low, 10-10 M concentration, the perfusion in the presence of L-NAME produced a comparable 3.5-fold increase of the vasoconstrictor responses at 1 and 3 wk. At the higher, 10-9 M and 10-8 M concentrations, the perfusion in the presence of L-NAME AII produced a grossly comparable 1.7-2-fold increase of the vasoconstrictor responses at 1, 3, and 6 wk (Fig. 3A). At 6 wk, 10-10 M AII was unable to produce a significant vasoconstriction whether L-NAME was present or not (Fig. 3B). Intermediate potentiating effects of L-NAME were observed on the 10-9 M AII-induced vasoconstrictions. It should also be mentioned that, in the presence of L-NAME, a sustained 10-8 M AII-induced vasoconstriction, which persisted after the infusion of AII was stopped, was observed in the 1-wk-old group.
Relative potentiating effects of L-NAME on the vasoconstrictions induced by 10-10, 10-9, and 10-8 M AII in 1-, 3-, and 6-wk-old rabbit kidney preparations. The values represent the ratio of the AII-induced vasoconstrictions measured in the presence and in the absence of L-NAME as calculated from the data presented in Fig. 3. Age had no significant effect as determined by two-way variance analysis.
DISCUSSION
In this study, an in vitro IPK model on developing rabbits was used to edplore in the absence of any systemic influence the role of endogenous NO on intrinsic RVR and on AII vasoconstrictor action during postnatal maturation. The results obtained in the presence or in the absence of L-NAME indicate that, in the rabbit IPK, RVR follows a decreasing pattern during postnatal development, and that the role of NO in the control of renal vascular basal tone is operating during the neonatal period and during later maturational stages. Furthermore, this study shows that AII-induced vasoconstrictions and their modulation by NO in the rabbit IPK are effective during early postnatal developmental stages and later evolve according to specific, concentration-dependent maturating patterns. Especially, a high affinity, decreasing with age AII/NO interaction, is evidenced.
Development of RVR in the IPK. RVR has been shown to be higher in the immature, newborn mammal, than in its adult counterpart, and to decrease during postantal maturation. As a consequence, RBF follows an inverse developmental pattern(1). Such changes condition the postnatal development of GFR, which rapidly increases during the first weeks of life. Postnatal changes in renal hemodynamics are usually attributed to the postnatal increase in renal perfusion pressure, and overall to changes in the balance between vasoconstricting and vasodilating agents in the neonatal period, superimposed on anatomical development.
The results of the present study indicate that, in the rabbit isolated kidney, RVR follows a decreasing postantal developmental pattern. Although lower than the reduction of RVR observed in vivo in various species including the human(1), this physiologic process is thus shown to persist in conditions excluding the influence of extrarenal regulating factors. These include local AII formation and renal sympathetic-adrenergic nerves. Local prostaglandin synthesis was ruled out, because the renal preparations have been perfused in the presence of indomethacin. These findings therefore imply that intrarenal factors are involved. As RVR is expressed per unit of kidney weight in our study, such factors are unlikely to be purely anatomical, in relation to the growth processes that affect the developing kidney including its vasculature. The local mechanisms underlying the postnatal decrease of RVR in the rabbit IPK remain to be determined.
In the present study, NO is demonstrated to be involved in the control of basal renal vacular tone in early postnatal developmental stages. Indeed, inhibition of NOS is shown to be responsible for an approximately 30% increase of RVR in the developing 1-, 3-, and 6-wk-old IPKs. In the anesthetized neonatal piglet, inhibition of NOS by intrarenal infusion of L-NAME has been shown to result in a comparable increase of RVR and a concomitant decrease in RBF and GFR; however, in this study these changes were higher in newborn piglets than in adult pigs(6). NO has been shown to intervene in an ongoing vasodilation of the renal vascular bed as early as during the third trimester of gestation in the chronically catheterized fetal sheep(7). Thus, together with the present results, it is reasonable to conclude that a functional vascular NO-L-Arg pathway is operating in the kidney as early as the prenatal period, in various species both in vivo and in vitro. Whether the NO-L-Arg pathway is fully developed at early developmental stages or whether this system is partly responsible for the high RVR observed in our study remains to be ascertained. Interestingly enough, the achievement of nephrogenesis, which is considered to state at about 2 wk of life in the rabbit(23), does not influence the slope of the decline of RVR in this study (Fig. 1). This is not in favor of the hypothesis that the achievement of nephrogenesis, and not birth itself, is responsible for the marked development of RBF and GFR observed in various species. In support of this, it has been shown that, in human premature infants, the GFR markedly increases after birth even in very low gestational age patients, in whom nephrogenesis is expected to continue(4).
AII vascular reactivity. The renin angiotensin system has been shown to intervene in the control of renal hemodynamics during fetal and postnatal development. Plasma renin is high in newborns and gradually falls with age(24). In newborn lambs, AII reduces RBF, whereas GFR is preserved, suggesting that AII acts mainly at efferent arterioles(25). The tonic effect of AII on the renal vasculature is minimal early in gestation and increases as the fetus matures(25). The angiotensin-converting enzyme inhibitor captopril does not influence hemorrhageinduced changes in RBF in young fetuses, but blocks RBF reduction in near term fetuses(26). β-Adrenergic fibers and renin-containing cells are spatially associated along the renal vasculature from fetal and newborn rats(27), and the stimulation ofβ-adrenergic system in fetal and newborn animals causes renin release and renal hemodynamic alteration(28).
In the present study performed on rabbit IPK, vascular responses to AII followed a developmental profile depending on the concentration. The vasoconstrictor responses to nanomolar concentrations of AII (10-9 M and 10-8 M) progressively increased with age. Similar findings have been reported in other studies(29), especially in the developing sheep(30). The mechanisms of the progressive increase of renal vascular responses to AII during postnatal maturation are unknown. On the other hand, a specific pattern of the renal vasoconstrictor responses to a subnanomolar concentration of AII (10-10 M) was evidenced with higher responses in renal preparations from 1-wk-old, newborn rabbits, decreasing thereafter and finally disappearing during further development. Therefore, in this in vitro model of rabbit IPK, a specific neonatal high affinity AII vasoconstricting effect disappearing after nephrogenesis completion, precedes a low affinity AII effect progressively increasing toward adult ages. Previous studies have shown that AII AT2 receptors are the dominant subtype expressed early during renal development, whereas AT1 receptors are the dominant subtype in the adult kidney(31). Although further studies are needed to determine the exact role of the AII receptor subtypes in the present findings, it is tempting to speculate that AT2 receptors might be responsible for the neonatal high affinity AII responses. Also, sustained AII 10-8 M-induced vasoconstrictions were observed only in the younger age groups of animals (Fig. 2). These findings argue for the existence of developmental specifics of the renal vasoconstrictor effect of AII. The mechanisms underlying these characteristics deserve further investigation.
AII/NO interactions. In the adult kidney, a number of studies have provided support for a role of AII in mediating the effect of NOS inhibition both in vivo(16–19) and in vitro(15). This effect depends on the level of activation of the reninangiotensin system(32–34), as indicated by results obtained in conscious animals with normal renin activity(35) or under modified salt diet(35, 36), and in animals with different renal perfusion pressures(37, 38). On the other hand, a blunting effect of NO on renal AII-induced vasoconstriction has been evidenced in vivo in conscious animals treated with NOS inhibitors(9–13). In vitro, a comparable effect of endogenous NO on AII-induced renal vasoconstriction has been documented in afferent(11, 39, 40) but not in efferent arterioles(14). The mechanism of the AII-induced NO-dependent vasodilatory component is not clear but presumably might involve a shear stress-dependent mechanism, triggered by vasoconstriction and associated with an increase in endothelial cytosolic calcium(41).
The present study in the neonatal and developing rabbit kidney also evidences a blunting effect of NO on renal AII vasoconstricting actions, as early as at the postnatal period in the rabbit IPK. Indeed, L-NAME potentiated AII-induced vasoconstrictions whatever the AII concentration and the age. As the relative potentiating effect of L-NAME on each concentration of AII did not change with age, the developmental patterns of AII-induced vasoconstrictions in the absence and the presence of L-NAME were qualitatively similar. The specific AII/NO interaction observed at subnanomolar concentration of AII in newborn animals has not yet been reported to our knowledge and may characterize a specific physiologic role of AII and NO in the control of renal hemodynamics in early postnatal developmental stages. However, the mechanism underlying this observation remains unknown. A recent study comparing the effects of endogenous and exogenous NO on AII-elicited vasoconstrictions in the rat kidney in vivo suggests that NO-induced attenuation of AII vasoconstricting effects is not due to a constrictor-induced production of NO(42). On the other hand, as already discussed above, our results may support the hypothesis that this early specific AII/NO interaction might involves AT2 receptors which are abundantly expressed at this developmental period. Clearly, further experiments using specific AII receptor subtype antagonists are needed to assess this hypothesis. Also, bearing in mind that AII also functions as a growth factor, the assessment of a possible relation between nephrogenesis, which is achieved around 2 wk after birth in the rabbit(23), and the involvement of AT1 or AT2 receptors requires further investigation.
The relative potentiating effect of L-NAME on AII-induced vasoconstrictions was not dependent upon postnatal maturation in our study. This observation suggests that the mechanism underlying the NO-mediated modulation of AII renal vasoconstricting effects is developed as soon as in the neonatal rabbit and does presumably not undergo further maturation at the ages of 3 and 6 wk in the rabbit IPK.
In conclusion, NO modulates both RVR and the renal vasoconstrictor effect of AII in the in vitro, developing rabbit IPK. In this model, RVR follows a decreasing developmental pattern. The postnatal development profile of AII-NO interactions depends on AII concentration. At nanomolar concentration vascular responses to AII, as well as the unmasking effect of NOS inhibitors on these responses, increase during postnatal development. Inversely at a low, 10-10 M AII concentration, unique vascular responses at the earliest stage of postnatal renal development are unmasked by inhibition of NO synthesis. Taken together, the present results, obtained on an isolated kidney model, further demonstrate the role of NO in the control of basal renal hemodynamics and in the modulation of the effects of vasoconstricting agents such as AII. They also evidence a specific, maturational profile of AII/NO interactions in the developing kidney and are in support of a combined role of AII and NO in the control of renal hemodynamics during postnatal development.
Abbreviations
- AII:
-
angiotensin II
- IPK:
-
isolated perfused kidney
- L-NAME:
-
Nω-nitro-L-arginine methyl ester
- NO:
-
nitric oxide
- NOS:
-
nitric oxide synthase
- RVR:
-
renal vascular resistance
- RBF:
-
renal blood flow
- AT1, AT2:
-
angiotensin receptor subtypes 1, 2
References
Gruskin AB, Edelmann CM Jr, Yan S 1970 Maturational changes in renal blood flow in piglets. Pediatr Res 4: 7–13.
Guignard JP, Torrado A, Da Cunha O, Gautier E 1975 Glomerular filtration rate in the first three weeks of life. J Pediatr 87: 268–272.
Arant BS Jr 1978 Developmental patterns of renal function maturation compared in the human neonate. J Pediatr 92: 705–712.
Bueva A, Guignard JP 1994 Renal function in preterm neonates. Pediatr Res 36: 572–577.
Tufro-McReddie A, Gomez RA 1993 Ontogeny of the renin-angiotensin system. Semin Nephrol 13: 519–530.
Solhaug MJ, Wallace MR, Granger JP 1993 Endothelium-derived nitric oxide modulates renal hemodynamics in the developing piglet. Pediatr Res 34: 750–754.
Bogaert GA, Kogan BA, Mevorach RA 1993 Effects of endothelium-derived nitric oxide on renal hemodynamics and function in the sheep fetus. Pediatr Res 34: 755–761.
Cocks TM, Angus JA 1983 Endothelium-dependent relaxation of coronary arteries by noradrenaline and serotonin. Nature 305: 627–630.
Conrad KP, Whittemore SL 1992 NG-Monomethy1-L-arginine and nitroarginine potentiate pressor responsiveness of vasoconstrictors in conscious rats. Am J Physiol 262:R1137–R1144.
Ito S, Juncos LA, Nushiro N, Jonhson CS, Carretero OA 1991 Endothelium-derived relaxing factor modulates endothelin action in afferent arterioles. Hypertension 17: 1052–1056.
Ito S, Johnson CS, Carretero OA 1991 Modulation of angiotensin II-induced vasoconstriction by endothelium-derived relaxing factor in the isolated microperfused rabbit afferent arteriole. J Clin Invest 87: 1656–1663.
Baylis C, Harvey J, Engels K 1994 Acute nitric oxide blockade amplifies the renal vasoconstrictor actions of angiotensin II. J Am Soc Nephrol 5: 211–214.
Alberola AM, Salazar FJ, Nakamura T, Granger JP 1994 Interaction between angiotensin II and nitric oxide in control of renal hemodynamics in conscious dogs. Am J Physiol 267:R1472–R1478.
Ito S, Arima S, Ren YL, Juncos LA, Carretero OA 1993 Endothelium-derived relaxing factor/nitric oxide modulates angiotensin II action in the isolated microperfused rabbit afferent but not efferent arteriole. J Clin Invest 91: 2012–2019.
Ohishi K, Carmines PK, Inscho EW, Navar LG 1992 EDRF-angiotensin II interactions in rat juxtamedullary afferent and efferent arterioles. Am J Physiol 263:F900–F906.
Sigmon DH, Carretero OA, Beierwaltes WH 1992 Angiotensin dependence of endothelium-mediated renal hemodynamics. Hypertension 20: 643–650.
Sigmon DH, Carretero OA, Beierwaltes WH 1992 Plasma renin activity and the renal response to nitric oxide synthesis inhibition. J Am Soc Nephrol 3: 1288–1294.
Hajj-ali AF, Zimmerman BG 1992 Nitric oxide participation in renal hemodynamic effect of angiotensin converting enzyme inhibitor lisinopril. Eur J Pharmacol 212: 279–281.
Sigmon DH, Beierwaltes WH 1993 Renal nitric oxide and angiotensin II interaction in renovascular hypertension. Hypertension 22: 237–242.
Robillard JE, Weismann DN, Gomez A, Ayres NA, Lawton WJ, Van Orden DE 1983 Renal and adrenal responses to converting-enzyme inhibition in fetal and newborn life. Am J Physiol 244:R249–R256.
Osborn JL, Hook JB, Bailie MD 1980 Effects of saralasin and indomethacin on renal function in developing piglets. Am J Physiol 238:R438–R442.
Solhaug MJ, Wallace MR, Granger JP 1996 Nitric oxide and angiotensin II regulation of renal hemodynamics in the developing piglet. Pediatr Res 39: 527–533.
Kazimierczak J 1963 Histochemical study of oxidative enzymes in rabbit kidney before and after birth. Acta Anat 55: 352–369.
Godard C, Gaillard R, Vallotton MB 1976 The renin-angiotensin-aldosterone system in mother and fetus at term. Nephron 17: 353–360.
Robillard JE, Nakamura KT, Matherne GP, Jose PA 1988 Renal hemodynamics and functional adjustments to postnatal life. Semin Perinatol 12: 143–150.
Gomez RA, Robillard JE 1984 Developmental aspects of the renal responses to angiotensin II in fetal lambs and adult sheep. Circ Res 54: 301–312.
Pupilli C, Gomez RA, Tuttle JB 1991 Spatial association of renin-containing cells and nerve fibers in developing rat kidney. Pediatr Nephrol 5: 690–695.
Robillard JE, Nakamura KT 1988 Neurohormonal regulation of renal function during development. Am J Physiol 254:F850–F858.
Gleason CA 1987 Prostaglandins and the developing kidney. Semin Perinatol 11: 12
Robillard JE, Gomez RA, Van Orden DE 1982 Comparison of the adrenal and renal responses to angiotensin II in fetal lambs and adult sheep. Circ Res 50: 140–147.
Aguilera G, Kapur S, Feuillan P, Sunar-Akbasak B, Bathia AJ 1994 Developmental changes in angiotensin II receptor subtypes and AT1 receptor mRNA in rat kidney. Kidney Int 46: 973–979.
Baylis C, Engels K, Samsell L, Harton P 1993 Renal effects of acute endothelium-derived relaxing factor blockade are not mediated by angiotensin II. Am J Physiol 264: F74–F78.
Pucci ML, Lin L, Nasjletti A 1992 Pressor and renal vasoconstrictor effects of NG-nitro-L-arginine as affected by blockade of pressor mechanisms mediated by the sympathetic nervous system, angiotensin, prostanoids and vasopressin. J Pharmacol Exp Ther 261: 240–245.
Sigmon DH, Newman JM, Beierwaltes WH 1994 Angiotensin II-endothelium-derived nitric oxide interaction in conscious rats. J Am Soc Nephrol 4: 1675–1682.
Sigmon DH, Beierwaltes WH 1993 Angiotensin II-nitric oxide interaction and the distribution of blood flow. Am J Physiol 265:R1276–R1283.
Deng X, Welch WJ, Wilcox CS 1994 Renal vasoconstriction during inhibition of NO-synthase: effects of dietary salt. Kidney Int 46: 639–646.
Takenaka T, Mitchell KD, Navar LG 1993 Contribution of angiotensin II to renal hemodynamic and excretory responses to nitric oxide synthesis inhibition in the rat. J Am Soc Nephrol 4: 1046–1053.
Sigmon DH, Carretero OA, Beierwaltes WH 1992 Endothelium-derived relaxing factor regulates renin release in vivo. Am J Physiol 256:F256–F261.
Imig JD, Roman RJ 1992 Nitric oxide modulates vascular tone in preglomerular arterioles. Hypertension 19: 770–774.
Tamaki T, Hasui K, Aki Y, Kimura S, Abe Y 1993 Effects of N(G)-nitro-L-Arginine on isolated rabbit afferent arterioles. Jpn J Pharmacol 62: 231–237.
Busse R, Mulsch A, Fleming I, Hecker M 1993 Mechanisms of nitric oxide release from the vascular endothelium. Circulation 87: 18–25.
Parekh N, Dobrowolski L, Zou A-P, Steinhausen M 1996 Nitric oxide modulates angiotensin II- and norepinephrine-dependent vasoconstriction in rat kidney. Am J Physiol 270: R630–R635.
Acknowledgements
The authors thank Drs. N. Parekh and K.-H. Endlich for kindly reviewing the manuscript.
Author information
Authors and Affiliations
Additional information
Supported by the French National Institute of Health and Medical Research(INSERM), grant CJF 9409, the French Ministry of Higher Education (MENESR), EA 1314 and the French Medical Foundation.
Rights and permissions
About this article
Cite this article
Simeoni, U., Zhu, B., Muller, C. et al. Postnatal Development of Vascular Resistance of the Rabbit Isolated Perfused Kidney: Modulation by Nitric Oxide and Angiotensin II. Pediatr Res 42, 550–555 (1997). https://doi.org/10.1203/00006450-199710000-00022
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/00006450-199710000-00022
This article is cited by
-
Neuronal nitric oxide synthase, nNOS, regulates renal hemodynamics in the postnatal developing piglet
Pediatric Research (2012)